Abstract
Objectives
The aim of this study was to compare two different thermoplastic techniques—a core-carrier technique (Thermafil) and warm vertical compaction—in terms of overextension of root canal filling in vivo.
Materials and methods
Flaring of 88 teeth was conducted using Pro Files .04 as finishing files, and the teeth were obturated using Thermafil. Flaring of 74 teeth was performed using Pro Files .06 as finishing files, and the teeth were obturated using warm vertical compaction.
Results
Seventy (80 %) of the teeth obturated using Thermafil and 31 (42 %) teeth obturated using warm vertical compaction show extruded root canal filling. In contrast to Thermafil, there is a higher rate of extruded root canal filling of teeth with more than one root canal using warm vertical compaction.
Conclusion
Thermafil demonstrated a higher rate of extruded root canal filling compared to warm vertical compaction. Warm vertical compaction is a more predictable method of filling compared to Thermafil.
Clinical relevance
Root canal filling extrusion will cause irritation of the surrounding tissue and impair repair processes. In the present in vivo study, there was a higher rate of root canal filling extrusion using Thermafil compared to warm vertical compaction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The objectives of root canal treatment are adequate cleaning and shaping of the root canal system and complete filling using a biologically inert and dimensionally stable material [1]. The goal of root canal obturation is to fill the root canal system and eliminate all portals of entry between the root canal and the periodontium. This is critical for the long-term prognosis of the root canal treatment [2]. An ideal filling seals all foramina, is well condensed and adapted to the canal walls, and ends at the apical constriction [3, 4]. Due to resorption of the foramen associated with apical periodontitis, the apical constriction is often not present. In these cases, the root canal filling has its apical terminus as close as possible to the apical foramen. Most methods of root canal filling use different formulations of gutta-percha in combination with a sealer. Endodontic sealers are capable of filling imperfections, patent accessory canals, and multiple foramina [5]. The sealer component should be kept to a minimum due to their dimensional instability and solubility over time [6, 7]. There are different techniques for placing gutta-percha into the root canal. Cold lateral compaction is a technique that is taught most frequently. This technique has the advantage of controlling the length of the root canal filling during obturation [8]. However, the shape of most root canals can complicate its application. Techniques using thermoplasticized gutta-percha have gained popularity over time [9, 10]. Among these, coated carrier systems (Thermafil) consisting of a plastic central carrier with a layer of so-called α-phase gutta-percha, which is softened by heat before being inserted into the root canal, have become popular. Previous reports suggest a homogenous mass in the root canal with a better core/sealer ratio compared to lateral compaction [11]. Warm vertical compaction requires a well-tapered and shaped canal along with a proper-fitting master gutta-percha point [12]. Hydraulic forces exerted during the compaction of the softened, warm gutta-percha and sealer move the filling material throughout the canal space and into accessory, lateral canals, fins, and loops [13]. Using thermoplasticized gutta-percha obturation techniques, the risk of extrusion of the root canal filling increases compared to cold lateral compaction [14–16]. Previous in vitro studies indicate a rate of extruded root canal filling from 25 to 100 % using Thermafil [16–18] and a range from 3 to 83 % of extruded root canal filling using warm vertical compaction [17, 18]. Overextension of root canal filling will decrease the long-term prognosis of the root canal treatment [19, 20]. To date, there are only few information about the rate of overextension of root canal filling using thermoplasticized gutta-percha in vivo. The objective of the present retrospective in vivo study was to evaluate and compare two different thermoplastic techniques—a core-carrier technique (Thermafil) and warm vertical compaction—in terms of overextension of root canal filling.
Materials and methods
Selecting patients
For this study, 162 root canal fillings of single- and multiple-rooted teeth were analyzed. The root canal fillings were performed by one endodontist over a period of 3 years. This is a retrospective study. Root canal treatments of vital and nonvital pulps were examined. Eighty-eight teeth were filled using Thermafil; 74 teeth were filled using warm vertical compaction.
Flaring of root canals and determination of working length
Root canals were flared using a hybrid technique depending on the root canal anatomy. Gates-Glidden drills, Pro File OS, and System GT Accessory files (Dentsply, Konstanz, Germany) were used for preflaring. Then, hand files ISO 6 till ISO 15 were used to access the apical third of the root canal in combination with Raypex 5 (VDW, Munich, Germany), an electronic apex locator. To determine working length, an ISO 10 K-file was inserted into the root canal until all three green bars were reached. The stopper was positioned at the reference point, and the insertion length was measured and recorded [21]. Now the root canal was shaped till ISO 15 with K-files at working length. Working length was verified with a radiographic cone shot or a radiographic file shot. For working length, it was considered that the cone or file ends 1 mm shorter than the radiographic apex. During shaping, an ISO 10 K-file was repeatedly inserted at working length to maintain patency. The coronal and middle third of the root canals were flared using Pro Files .06 and ProTaper S instruments. After gauging, apical shaping was performed till ISO 30 or larger and a taper of 4 % according to the manufacturer's recommendation for Thermafil and a taper of 6 % for warm vertical compaction according to the manufacturer's recommendation till an apical stop was present. Root canals that were filled with Thermafil were flared using Pro Files .04 as finishing files. Root canals that were filled using warm vertical compaction technique were flared using Pro Files .06 as finishing file. Per root canal, 5 ml of 5.25 % NaOCl and 17 % EDTA were used for irrigation. The irrigation was applied using 30-gauge NaviTips (Ultradent Products, Inc., South Jordan, UT, USA).
Obturation using Thermafil
After root canal preparation, the appropriate Thermafil obturator (Dentsply, Konstanz, Germany) was chosen according to the final Pro File, and the size was checked using verifiers (Dentsply, Konstanz, Germany). Gutta-percha overlapping the core more than 0.5 mm was cut off. Obturators with a core that was not covered by gutta-percha at the tip were not used. The walls of the coronal third of the root canal were covered with sealer (AH plus, Dentsply, Konstanz, Germany) using a paper point. Obturators were heated using a Thermaprep Plus oven (Dentsply, Konstanz, Germany) according to the manufacturer's recommendation. Obturators were inserted into the root canals. The core was cut using a Thermocut drill (Dentsply, Konstanz, Germany), and the gutta-percha was compacted using a ball burnisher. The access cavity was filled with Composite (Optibond FL, KerrHawe, Bioggio, Switzerland; Filtec Z250, 3M ESPE, Neuss, Germany).
Obturation using warm vertical compaction
Warm vertical compaction was performed using an Elements Obturation Unit (Sybron Endo, Orange, USA). A 6 % tapered master gutta-percha point (Dentsply, Konstanz, Germany) was chosen according to the size of the final Pro File and checked for apical tugback. A heat plugger of the Elements Obturation Unit (Sybron Endo, Orange, USA) was selected that fits passively within 3–5 mm from the apical terminus. The master point was covered with sealer and placed into the root canal with an agitating motion. Now the heat plugger was activated and utilized to sear off the master point. Depending on the length of the root canal, the master point was seared off in multiple steps until the heat plugger could be placed within 3–5 mm from the apical terminus. The apical plug was packed using hand pluggers (Buchanan, Sybron Endo, Orange, USA). Reverse filling of the root canal was performed with thermosoftened gutta-percha using the handpiece of the Elements Obturation Unit (Sybron Endo, Orange, USA). The tip of the warm canula was positioned against the apical pack. The handpiece was activated, and a 2–3-mm segment of warm gutta-percha was dispensed into the apical region. This segment of gutta-percha was plugged using hand pluggers (Buchanan, Sybron Endo, Orange, USA). This backfilling technique was repeated till the root canal was filled completely [22].
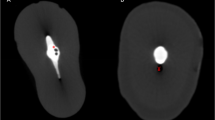
Radiograph evaluation
Conventional radiographs of obturated root canals were taken with parallel technique after root canal filling using a Heliodent DS X-ray apparatus with a voltage of 60 kV and an exposure time of 0.16 s for front teeth and premolars and 0.20 s for molars. The radiographs were photographed using a Canon EOS 20D camera. In a blind evaluation, each root canal was examined regarding overextension of root canal filling as a yes/no decision. Root canals without overextruded root canal filling were assigned as 0, root canals with overextruded root canal filling were assigned as 1. In multi-rooted teeth, teeth without overextruded root canal filling were assigned as 0, and teeth with one or more overextruded root canal filling were assigned as 1.
Statistical analysis
Data were submitted to a Fisher-Yates' chi-square test. The effect size, describing the strength of association or non-independence between data values, was determined using odds ratio. Odds ratios were verified using Mantel–Haenszel estimator.
Results
Rate of root canal filling extrusion
One hundred one (62 %) of 162 teeth had extruded root canal filling. From 88 teeth filled using Thermafil, 70 (80 %) demonstrated extruded root canal filling. From 74 teeth using vertical compaction technique, 31 (42 %) showed extruded root canal filling.
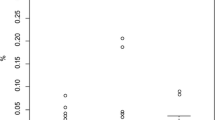
Rate of root canal filling extrusion depending on the number of root canals
From 88 teeth filled with Thermafil, 46 teeth had one root canal, and 42 teeth had more than one root canal. A total number of 70 teeth showed extruded root canal filling. Thirty seven (80 %) of 46 teeth with one root canal had extruded root canal filling. Thirty three (79 %) of 42 teeth with more than one root canal showed extruded root canal filling. There was no statistical significance between the rate of extruded root canal filling of teeth with one root canal compared to teeth with more than one root canal (p > 0.05, Fisher test).
From 74 teeth filled using vertical compaction technique, 35 (47 %) teeth had one root canal, and 39 (53 %) teeth had more than one root canal. Nine (29 %) of 35 teeth with one root canal had extruded root canal filling. Twenty two (71 %) of 39 teeth with more than one root canal had extruded root canal filling. There is a higher rate of root canal filling extrusion of teeth with more than one root canal compared to teeth with one root canal (p < 0.01, Fisher test) (Table 1, Fig. 1).
Discussion
Previous in vitro studies have shown that there is a higher gutta-percha/sealer ratio using obturation techniques with thermoplasticized gutta-percha compared to cold lateral compaction, but the risk of root canal filling extrusion increases [15–17, 23]. A meta-analysis demonstrated a greater incidence of overextension using warm gutta-percha obturation techniques compared to cold lateral compaction. The obturation quality, long-term prognosis, periapical healing, and postoperative pain prevalence were similar [2, 24]. Previous in vitro studies demonstrated that the rate of extruded root canal filling varies from 25 to 100 % using Thermafil and from 3 to 83 % using warm vertical compaction [8, 15–17]. In the present retrospective in vivo study, 80 % of teeth obturated using Thermafil and 42 % of teeth obturated using warm vertical compaction had extruded root canal filling. Analyzing the radiographs, it was impossible to differentiate between gutta-percha and sealer when evaluating the overextended root canal filling. Regarding the facts, a yes/no decision in terms of overextension of root canal filling was made. The variance of the rates of extruded root canal filling found in previous studies may be due to modifications in the experimental design: different flaring techniques with different tapers, manual or rotary flaring technique, different surfaces (dentin, plastic material when using artificial canals), and using different sealers or different amounts of sealer.
When obturating a root canal using warm vertical compaction technique, the length at which the heat plugger is inserted influences the rate of root canal filling extrusion. The deeper the heat plugger is inserted in the root canal, the higher the risk of overextension of root canal filling [5]. In the present study, heat pluggers were inserted 3–5 mm shorter than the working length [25]. According to previous findings, the gutta-percha master cone will only be plasticized if the heat plugger is inserted 2 mm shorter than the working length. The technique used in the present study should be considered as a compromise because the gutta-percha will not completely plasticize when inserting the heat plugger 3–5 mm shorter than the working length [22, 23].
Multiple factors influence the outcome of a root canal filling, e.g., the complexity of the anatomy of the root canal system or hydrostatic pressure. In the present study, there is a higher rate of overextended root canal filling of teeth with more than one root canal (71 %) compared to teeth with one root canal (29 %) using warm vertical compaction technique. A yes/no decision will statistically lead to an increasing rate of teeth with overextended root canal filling with increasing number of root canals when each root canal has an apical foramen. However, the rate of teeth with root canal filling extrusion was not dependent on the number of root canals using Thermafil. When obturating root canals using Thermafil, the spreading of gutta-percha is uncontrollable. Molars are more difficult to access, and their root canals have curvatures more frequently than premolars and front teeth. The insertion of Thermafil points is more difficult and takes more time filling premolars and molars and might lead to a decreasing rate of root canal filling extrusion per root due to the cooling of gutta-percha in these cases. Another explanation might be that in Thermafil cases, the extrusion of root canal filling was so frequent that no differences can be seen in teeth with more than one root canal compared to teeth with one root canal.
There are multiple factors that influence the outcome of a root canal treatment, namely the presence or absence of preoperative apical periodontitis, density and apical extent of root filling, and quality of coronal restoration [26]. For vital cases, extrusion of root canal filling will not limit their long-term prognosis. Several studies have shown that gutta-percha is well tolerated by tissue [27]. There is an adverse effect in teeth with preoperative apical periodontitis due to overinstrumentation which normally precedes overextension of root canal filling. Dentin and cementum chips and root canal filling material forced into the periapical region are associated with active inflammation, intensify inflammatory processes, and impair their repair process [27, 28].
Conclusion
Modern thermoplastic root canal obturation techniques are associated with a considerable rate of extrusion of root canal filling depending on the specific technique. In the present study, the rate of extruded root canal filling is higher using Thermafil (80 %) compared to warm vertical compaction (42 %). Warm vertical compaction is a more predictable method in terms of avoidance of root canal filling extrusion.
References
Hulsmann M, Peters OA, Dummer PMH (2005) Mechanical preparation of root canals: shaping goals, techniques and means. Endod Top 10:30–76
Peng L, Ye L, Tan H, Zhou X (2007) Outcome of root canal obturation by warm gutta-percha versus cold lateral condensation: a meta-analysis. J Endod 33:106–109
Michanowicz AE, Michanowicz JP, Michanowicz AM, Czonstkowsky M, Zullo TP (1989) Clinical evaluation of low-temperature thermoplasticized injectable gutta-percha: a preliminary report. J Endod 15:602–607
Leduc J, Fishelberg G (2003) Endodontic obturation: a review. Gen Dent 51:232–233
Wu MK, Fan B, Wesselink PR (2000) Diminished leakage along root canals filled with gutta-percha without sealer over time: a laboratory study. Int Endod J 33:121–125
Gilhooly RM, Hayes SJ, Bryant ST, Dummer PM (2000) Comparison of cold lateral condensation and a warm multiphase gutta-percha technique for obturating curved root canals. Int Endod J 33:415–420
Gilhooly RM, Hayes SJ, Bryant ST, Dummer PM (2001) Comparison of lateral condensation and thermomechanically compacted warm alpha-phase gutta-percha with a single cone for obturating curved root canals. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 91:89–94
Schafer E, Olthoff G (2002) Effect of three different sealers on the sealing ability of both thermafil obturators and cold laterally compacted gutta-percha. J Endod 28:638–642
Silver GK, Love RM, Purton DG (1999) Comparison of two vertical condensation obturation techniques: touch ‘n heat modified and system b. Int Endod J 32:287–295
Johnson WB (1978) A new gutta-percha technique. J Endod 4:184–188
Gencoglu N, Orucoglu H, Helvacioglu D (2007) Apical leakage of different gutta-percha techniques: thermafil, js quick-fill, soft core, microseal, system b and lateral condensation with a computerized fluid filtration meter. Eur J Dent 1:97–103
Schilder H (1967) Filling root canals in three dimensions. Dent Clin North Am 723–44
Venturi M, Breschi L (2004) Evaluation of apical filling after warm vertical gutta-percha compaction using different procedures. J Endod 30:436–440
Gencoglu N, Garip Y, Bas M, Samani S (2002) Comparison of different gutta-percha root filling techniques: thermafil, quick-fill, system b, and lateral condensation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 93:333–336
Clinton K, Van Himel T (2001) Comparison of a warm gutta-percha obturation technique and lateral condensation. J Endod 27:692–695
Da Silva D, Endal U, Reynaud A, Portenier I, Orstavik D, Haapasalo M (2002) A comparative study of lateral condensation, heat-softened gutta-percha, and a modified master cone heat-softened backfilling technique. Int Endod J 35:1005–1011
Kececi AD, Unal GC, Sen BH (2005) Comparison of cold lateral compaction and continuous wave of obturation techniques following manual or rotary instrumentation. Int Endod J 38:381–388
Robinson MJ, McDonald NJ, Mullally PJ (2004) Apical extrusion of thermoplasticized obturating material in canals instrumented with Profile 0.06 or Profile GT. J Endod 30:418–421
Schaeffer MA, White RR, Walton RE (2005) Determining the optimal obturation length: a meta-analysis of literature. J Endod 31:271–274
Kojima K, Inamoto K, Nagamatsu K, Hara A, Nakata K, Morita I, Nakagaki H, Nakamura H (2004) Success rate of endodontic treatment of teeth with vital and nonvital pulps. A meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 97:95–99
Vieyra JP, Acosta J (2011) Comparison of working length determination with radiographs and four electronic apex locators. Int Endod J 44:510–518
Ruddle CJ (2010) Filling root canal systems: the Calamus 3-D obturation technique. Dent Today 29(76):78–81
Wu MK, van der Sluis LW, Wesselink PR (2002) A preliminary study of the percentage of gutta-percha-filled area in the apical canal filled with vertically compacted warm gutta-percha. Int Endod J 35:527–535
Sari S, Duruturk L (2007) Radiographic evaluation of periapical healing of permanent teeth with periapical lesions after extrusion of AH plus sealer. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 104:e54–e59
Guess GM, Edwards KR, Yang ML, Iqbal MK, Kim S (2003) Analysis of continuous-wave obturation using a single-cone and hybrid technique. J Endod 29:509–512
Liang YH, Li G, Wesselink PR, Wu MK (2011) Endodontic outcome predictors identified with periapical radiographs and cone-beam computed tomography scans. J Endod 37:326–331
Sjogren U, Hagglund B, Sundqvist G, Wing K (1990) Factors affecting the long-term results of endodontic treatment. J Endod 16:498–504
Bergenholtz G, Lekholm U, Milthon R, Engstrom B (1979) Influence of apical overinstrumentation and overfilling on re-treated root canals. J Endod 5:310–314
Conflict of interest
The authors deny any conflicts of interest related to this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tennert, C., Jungbäck, I.L. & Wrbas, KT. Comparison between two thermoplastic root canal obturation techniques regarding extrusion of root canal filling—a retrospective in vivo study. Clin Oral Invest 17, 449–454 (2013). https://doi.org/10.1007/s00784-012-0726-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-012-0726-0