Abstract
The objective of this study was to compare the one-week bonding effectiveness of nine contemporary composite cements used to lute ceramic to dentin and to determine an appropriate processing method for pretesting failures. The microtensile bond strengths (µTBS) of different luting agents including five self-adhesive cements (Unicem, 3 M ESPE; Maxcem, Kerr; Monocem, Shofu; G-Cem, GC; and Multilink Sprint, Ivoclar-Vivadent), two self-etch cements (Panavia F2.0 and Clearfil Esthetic Cement, Kuraray), and two etch-and-rinse cements (Calibra, Dentsply, and Variolink II, Ivoclar-Vivadent) were measured using a standardized protocol. As control, a two-step self-etch adhesive combined with a restorative composite (Clearfil SE+Clearfil APX, Kuraray) were included as luting material. Depending on the processing of the pretesting failures, two groups of cements could be distinguished: (1) those with low bond strength and many pretesting failures and (2) those with relatively high bond strength and few pretesting failures. Nevertheless, the control luting procedure involving a self-etch adhesive combined with a restorative composite presented with a significantly higher µTBS. The µTBS was clearly product-dependent rather than being dependent on the actual adhesive approach. Fracture analysis indicated that failure usually occurred at the dentin–cement interface especially for the cements with low bond strength and many pretesting failures. Depending on the cement system, an adequate immediate ceramic-to-dentin bond strength can be obtained, even with self-adhesive cements that do not use a separate dental adhesive. Yet, the self-etch adhesive Clearfil SE combined with the restorative composite revealed a superior bonding performance and should therefore be preferred in clinical situations where the restoration transmits light sufficiently.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Indirect restorations in metal, ceramic, or composite need cementation by a luting agent.
Compared with other classes of cements, composite cements are renowned for their low solubility, superior physicomechanical strength, and good adhesion to tooth tissue, the latter because their multistep application procedure commonly involves the application of a separate dental adhesive [1]. Recently, so-called “self-adhesive” composite cements that do not use a separate adhesive have been marketed. Restorations, especially those that cannot rely on much mechanical retention such as inlays and overlays, will benefit from the use of composite cement.
With respect to their chemical formulation, composite cements resemble very much composite restoratives; however, they usually contain a lower concentration of filler particles, which imparts the composite cement its fluid properties. Similar to restorative composites, composite cements can be bonded to teeth by an adhesive. Depending upon the use of a separate adhesive and on the actual adhesive approach, composite cements can be subdivided into three classes: (1) “etch-and-rinse” composite cements, which utilize an etch-and-rinse adhesive (including a phosphoric acid etching step); (2) “self-etch” composite cements, which utilize a self-etch adhesive, and (3) self-adhesive composite cements that do not use a dental adhesive but are applied directly on the prepared tooth's dentin and enamel.
Like dental adhesives, composite cements have undergone a similar evolution toward a more simplified application procedure [2]. RelyX Unicem (3 M ESPE) was the first self-adhesive composite cement that no longer required a dental adhesive according to its application instructions [3]. The newest cements introduced to the market all belong to this class of self-adhesive composite cements whose application procedure is much simplified compared with the rather complex and laborious procedure of multistep composite cements.
The clinical longevity of indirect restorations greatly depends on the physicomechanical properties of the restoration and also on the bonding effectiveness of the luting agent to both the tooth and the indirect restoration substrate, generating a two-fold tooth cement and cement restoration interface complex. In addition, various clinical parameters, such as kind of surface treatment, type of restorative material, and cavity, design are aspects that need to be considered prior to the selection of a luting material.
The objective of this study was to evaluate the immediate bonding effectiveness of several contemporary composite cements used to lute hydrofluoric acid-etched and silane-treated ceramic to dentin. As control, a microhybrid composite along with a two-step self-etch adhesive was used. The microtensile bond strength was determined to test the null hypothesis that self-adhesive composite cements are equally effective as composite cements that utilize a separate dental adhesive. Different processing methods for pretesting failures were evaluated.
Materials and methods
Nine composite cements were used (Tables 1 and 2), including, respectively, two etch-and-rinse composite cements (Calibra, Dentsply and Variolink II, Ivoclar-Vivadent), two self-etch composite cements (Panavia F2.0, Kuraray and Clearfil Esthetic Cement, Kuraray), and five self-adhesive composite cements (RelyX Unicem, 3 M ESPE; Maxcem, Kerr; Monocem, Shofu; G-Cem, GC; and Multilink sprint, Ivoclar-Vivadent). As control, ceramic was luted to dentin using the two-step self-etch “gold standard” Clearfil SE (Kuraray) in combination with the microhybrid composite Clearfil APX (Kuraray).
Tooth preparation
Noncarious human molars gathered following informed consent approved by the Commission for Medical Ethics of the KULeuven were stored in 0.5% chloramine/water at 4°C and were used within 3 months after extraction. Flat dentin surfaces were obtained by removing coronal enamel with an Isomet low-speed diamond saw (Isomet 1000, Buehler, Lake Bluff, IL, USA). A standardized smear layer was produced first by grinding with a regular-grit (100 µm) diamond bur (842, Komet, Lemgo, Germany) mounted in the Microspecimen Former (University of Iowa, Iowa City, IA, USA), and second, by use of a SiC paper (600-grit). Dentin surfaces were verified for absence of enamel and/or pulp tissue using a stereo-microscope (Wild M5A, Heerbrugg, Switzerland). Subsequently, they were cleaned with pumice paste, rinsed with water, and air-dried without desiccating dentin, unless mentioned differently in Table 2 with regard to the respective manufacturers' instructions (Monocem, Shofu).
Ceramic preparation
The ceramic blocs (VITA blocks Mark II for Cerec/inlab, Vita, Bad Sächingen, Germany) were sectioned in three smaller blocs of approximately 4.15 mm thickness each (width 8 × 8 mm). Hydrofluoric acid (IPS Ceramic etching gel, Ivoclar-Vivadent) was then applied for 60 s, after which the ceramic surface was thoroughly rinsed with water and air-dried. Next, silane (Monobond S, Ivoclar-Vivadent) was applied and left undisturbed for 60 s, after which the surface was again air-dried. Finally, in order to improve resin infiltration into the etch pits in the ceramic block, a fluid, unfilled bonding resin, Heliobond (Ivoclar-Vivadent) was applied but not light-cured.
Bonding procedures
The ceramic blocks were next luted to dentin using the different cements, each strictly following the respective manufacturer's recommendations (Table 2).
Each block was luted under a fixed pressure of 1 kg and light-cured for 20 s from each side (Demetron Optilux 500, Kerr, Orange, USA) with a light output of not less than 550 mW/cm2 (100 seconds of light emission in total).
Microtensile bond strength (µTBS) testing
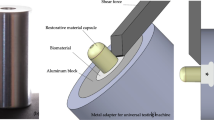
After one week of water storage at 37°C, the specimens were sectioned with a water-cooled diamond saw (Isomet 1000) in both x and y directions, perpendicular to the adhesive interface to obtain about 16 sticks with a cross-sectional area of approximately 1 mm2. The dimensions of the sticks were measured by means of a digital caliper (Mitutoyo, Kanagawa, Japan). The peripheral sticks where the ceramic block was bonded to enamel were excluded. After examination under a light microscope for absence of enamel, the sticks were fixed by their ends to the microtensile bond testing device (modified Cuicchi's device) with cyanocrylate glue (Model Repair II Blue, Dentsply-Sankin, Tokyo, Japan). This jig was then fixed in a LRX testing machine (Lloyd, Hampshire, UK) with a load cell of 100 N after which the specimens were stressed in tension at a crosshead speed of 1.0 mm/min. The bond strength values were calculated in MPa (derived from dividing the imposed force (in N) at the time of fracture by the bond area (in squaremeters). Depending on the inclusion of the so-called pretesting failures (ptfs, i.e., samples that failed before the bond strength could be determined), three groups of µTBS results were calculated: (1) µTBS with the ptfs counted in as 0 MPa, (2) µTBS with the ptfs counted in as the lowest value measured, and (3) µTBS with the ptfs not counted in.
The mode of failure was determined with a stereomicroscope (Wild M5A, Heerbrugg, Switzerland) at magnification of ×50 and recorded as “adhesive” (between dentin–cement or cement–ceramic), “cohesive” (in dentin, in cement or in ceramic), or “mixed” (Fig. 1).
Statistical analysis
The bond strength values were subjected to Kruskal–Wallis' test at a level of significance of 5%.
Results
The microtensile bond strengths of the tested cements together with the statistical analysis are shown in Fig. 2 and Table 1. The statistical outcome clearly varied according to the inclusion of the ptfs. Nevertheless, the two-step self-etch adhesive, Clearfil SE, and the restorative composite, Clearfil APX, always had a µTBS significantly superior to the other cements. Among the cements, the highest µTBS were obtained with the etch-and-rinse composite cements Calibra and Variolink, the self-etch composite cement Panavia F2.0, and with the self-adhesive cement G-Cem and RelyX Unicem. No significant differences in bond strengths to dentin were noticed between these cements when the ptfs were included as 0 MPa or as the lowest measured value. Only G-Cem exhibited some pretesting failures (three out of 37, Fig. 2). The bond strength of Clearfil Esthetic Cement was slightly lower, resulting in a statistical difference with Calibra, Panavia F2.0, and RelyX Unicem (Fig. 2 and Table 3).
µTBS of different luting materials bonded to dentin. Bars with different color indicate another way of processing the pretesting failures. Overlapping bars indicate that there is no statistical difference between the cement systems and asterisks indicate cements with a µTBS that is statistically significantly different from the µTBS of the other cements (Kruskal Wallis, p < 0.05). Abbreviation: ptf pretesting failure
The bond strengths of the self-adhesive composite cements Maxcem, Monocem, and Multilink Sprint were significantly lower compared with that of the other cements and the control. Their lower bond strength can partially be explained by the large number of pretesting failures (Table 3).
Failure analysis showed a “mixed” failure pattern for most composite cements involving failure both at the dentin–cement and/or cement–ceramic interface combined with a cohesive failure of the cement, the ceramic, and/or dentin substrate (Fig. 1). There was, however, a trend towards more “adhesive” dentin–cement failures for the composite cements that exhibited relatively low bond strength. The higher the bond strength, the more “adhesive” cement–ceramic failures were recorded. The control Clearfil SE, combined with Clearfil APX, failed predominantly at the cement–ceramic interface (Fig. 1).
Discussion
In this study, the bonding effectiveness of nine contemporary luting agents to bond ceramic to dentin was compared. As control, the “gold-standard” two-step self-etch adhesive Clearfil SE in combination with the microhybrid restorative composite Clearfil APX was chosen. Since the composition of composite cement resembles very much the composition of a restorative composite, the latter can also be used as luting agent on the condition that it is sufficiently fluid and that it can be adequately light-cured. In this study, the ceramic blocks were made of feldspatic ceramic (Vita Mark II), which transmits light relatively well especially considering the small dimensions of the blocks. In contrast, the cement systems tested in this study were all dual curing [4]. Their polymerization can be initiated by activation of light and chemical initiators due to which they remain the materials of choice to lute indirect tooth-colored restorations with a thickness of 4 mm or more [5]. To ensure a maximal mechanical strength, all composite cements were light-cured in this study, meaning that their actual polymerization was initiated both chemically and by light.
Nonetheless, the solely light-cured restorative composite (control) obtained a bond strength that was superior to that of all the cements. This must most likely be attributed to (1) the excellent bonding performance of the two-step self-etch adhesive Clearfil SE, as was repeatedly reported in several in-vitro [6–9] and in-vivo [10] studies; and (2) to the superior mechanical properties of the highly-loaded restorative composite Clearfil APX compared to the lower-filled composite cements. In addition, this outcome indicates that the ceramic blocks of 4.15 mm in thickness still transmit light sufficiently to initiate polymerization.
With respect to the cement systems, their bond strengths and the ensuing statistical analysis varied depending upon the processing of the pretesting failures. In literature, the correct handling of samples that failed before they could be tested is still up to debate. However, it is generally accepted that pretesting failures cannot just be omitted as this will cause a bias to higher bond-strength results (Fig. 2 and Table 3) [11, 12]. To avoid bias, pretesting failures can be counted in as 0 MPa even though it is accepted that this may induce a bias to a lower bond strength [6, 13, 14]. Doing so, two groups could be distinguished in this study: (1) Cements with low bond strengths (<4 MPa) and many pretesting failures and (2) cements with significantly higher bond strengths (>13 MPa) and no (or only a few in case of G-Cem) pretesting failures (Fig. 2 and Table 3). One could also include pretesting failures as the lowest measured µTBS value. In this study, this resulted in statistically significant differences between Maxcem, Monocem, and Multilink Sprint. An explanation for these statistical differences is the decrease in standard deviation since the many pre-testing failures were counted in with the same value. There are some other disadvantages to the use of the lowest measured µTBS value, such as the fact that the lowest measured µTBS values are probably more test-specific than adhesive-specific and that they depend much on the accuracy of the testing device. All in all, it is best to avoid pretesting failures as much as possible, as they will always bias the bond strength to a certain extent. Development of new atraumatic preparation techniques to avoid excessive stresses during the preparation of µTBS-sticks is much recommended, such as, for example, the use of an impression material to envelop the ceramic block and to prevent eccentric forces during the cutting of the sticks [C. Kleverlaan (ACTA Amsterdam), unpublished research].
The bond strength did not appear to depend on the actual adhesive approach (etch-and-rinse versus self-etch versus self-adhesive). However, composite cements that use a separate dental adhesive tended towards higher bond strength (Fig. 2). Nevertheless, the self-adhesive composite cements G-Cem and RelyX Unicem performed equally well. This newest and most simplified class of self-adhesive cements were conceived to self-adhere to tooth tissue. In contrast to multistep luting cements that employ a separate adhesive, the luting material itself also contains acidic monomers to enhance wetting and to actually bond to dentin [15]. In addition, they may contain solvents, such as water (G-Cem) or they may require wet bonding (Monocem, Shofu; Table 3) to allow ionization of the functional monomers. Similar to dental adhesives, they should exhibit a high flowability to ensure good wetting of the tooth surface.
Interestingly, in spite of their common use of ED primer II (Kuraray), the bond strength of Clearfil Esthetic Cement was significantly lower than that of Panavia F2.0, both products from Kuraray. The lower bond strength of Clearfil Esthetic Cement must thus be attributed to the chemical composition and/or physical properties of the composite cement. In contrast to Panavia F2.0, the composite cement of Clearfil Esthetic Cement does not contain the monomer 10-MDP, known for its good adhesive capacity [16]. A plausible explanation may then be a lower conversion rate of Clearfil Esthetic Cement as 10-MDP in Panavia F2.0 can act as a diluent, increasing the conversion. On the other hand, Panavia F2.0 is manually mixed with a spatula in contrast to the automix syringe provided with Clearfil Esthetic Cement. Even though reduction of the number of air inclusions seems favorable at first sight, they can also act as stress reducers, which may be a second hypothesis for the higher bond strength of Panavia F2.0.
Failure analysis revealed that adhesion, especially to dentin remains the weak link in the indirect restoration/tooth complex. In particular, the self-adhesive composite cements that exhibited many pretesting failures failed predominantly adhesively at the dentin–cement interface (Fig. 1). The higher the bond strength, however, the more failures occurred at the cement–ceramic interface, which indicates that the adhesion to ceramic was relatively good. A good adhesion to the feldspatic ceramic blocks was obtained by hydrofluoric acid etching to produce a microretentive surface, and, subsequently, by silane treatment to promote an additional chemical bond to the ceramic. In addition, a bonding resin (Heliobond, consisting of 60 wt% Bis-GMA, and 40 wt% TEGDMA) was applied to ensure good covalent bonding to the resin cement/composite. This ceramic bonding technique is well established [17–20] and was used for all samples so that the bond to the ceramic substrate was no variable in this study.
Several authors have recommended to light-cure the bonding resin applied to dentin and the ceramic substrate prior to cementation in order to increase the bond strength [21, 22] as well as to improve the marginal adaptation to both the substrates [23]. However, separately light-curing the bonding agent may affect the accuracy of fit of the restoration in the prepared cavity when the impression is taken before the resin bonding is applied [21], as the cured adhesive film will have a certain thickness. In this study, it was decided not to light-cure the resin bonding separately and to have the uncured resin bonding dilute and copolymerize with the subsequently applied composite cement to form a strong and stable bond.
As indicated by many other researchers [3, 5, 24, 25], the cements in this study were applied under a fixed pressure of 1 kg before being light-cured for 20 seconds from each side. The importance of cementation under pressure was revealed by De Munck et al. [3], especially for the first self-adhesive composite cement on the market, RelyX Unicem. The authors suggested that this cement should always be applied under pressure to ensure that the cement intimately adapts to the cavity walls [3].
The null hypothesis stating that self-adhesive composite cements are equally effective as composite cements that utilize a separate dental adhesive must be accepted for RelyX Unicem and G-Cem. However, there was an obvious trend towards inferior bonding effectiveness of self-adhesive composite cements to dentin. This all indicates that the adhesion of self-adhesive cements is highly dependent on the chemical formulation and physical properties (wetting, etc.) of the cement. In this study, the restorative composite resin obtained the highest bond strengths. This indicates that when sufficient light transmission can be assured, conventional restorative composites can also be used to cement indirect restorations. Nevertheless, the viscosity of the restorative composite must be taken into account because this may interfere with the fit of the restoration. Special techniques, such as ultrasonication, to render the composite more fluid, have already been recommended to overcome this problem [3]. Nevertheless, Clearfil APX used in this study was sufficiently fluid from itself.
In conclusion, depending on the composite cement, good immediate bond strength can be obtained when luting ceramic to dentin, even with self-adhesive composite cements that do not use a separate dental adhesive. However, the self-adhesive capacity of composite cement seems to depend on product-specific factors, such as chemical composition and viscosity. A good alternative to composite cements is the use of a dental adhesive combined with a restorative composite, at least when sufficient light-curing can be ensured.
References
Saskalauskaite E, Tam LE, McComb D (2008) Flexural strength, elastic modulus, and pH profile of self-etch resin luting cements. J Prosthodont 17:262–268
Van Meerbeek B, De Munck J, Yoshida Y, Inoue S, Vargas M, Vijay P, Van Landuyt K, Lambrechts P, Vanherle G (2003) Buonocore memorial lecture. Adhesion to enamel and dentin: current status and future challenges. Oper Dent 28:215–235
De Munck J, Vargas M, Van Landuyt K, Hikita K, Lambrechts P, Van Meerbeek B (2004) Bonding of an auto-adhesive luting material to enamel and dentin. Dent Mater 20:963–971
Paul SJ, Scharer P (1997) The dual bonding technique: a modified method to improve adhesive luting procedures. Int J Periodontics Restorative Dent 17:536–545
Hikita K, Van Meerbeek B, De Munck J, Ikeda T, Van Landuyt K, Maida T, Lambrechts P, Peumans M (2007) Bonding effectiveness of adhesive luting agents to enamel and dentin. Dent Mater 23:71–80
Van Landuyt KL, Peumans M, De Munck J, Lambrechts P, Van Meerbeek B (2006) Extension of a one-step self-etch adhesive into a multi-step adhesive. Dent Mater 22:533–544
Sidhu SK, Omata Y, Tanaka T, Koshiro K, Spreafico D, Semeraro S, Mezzanzanica D, Sano H (2007) Bonding characteristics of newly developed all-in-one adhesives. J Biomed Mater Res B Appl Biomater 80:297–303
Proenca JP, Polido M, Osorio E, Erhardt MC, Aguilera FS, Garcia-Godoy F, Osorio R, Toledano M (2007) Dentin regional bond strength of self-etch and total-etch adhesive systems. Dent Mater 23:1542–1548
Perdigao J, Gomes G, Gondo R, Fundingsland JW (2006) In vitro bonding performance of all-in-one adhesives. Part I–microtensile bond strengths. J Adhes Dent 8:367–373
Peumans M, De Munck J, Van Landuyt K, Lambrechts P, Van Meerbeek B (2007) Five-year clinical effectiveness of a two-step self-etching adhesive. J Adhes Dent 9:7–10
Phrukkanon S, Burrow MF, Tyas MJ (1998) The influence of cross-sectional shape and surface area on the microtensile bond test. Dent Mater 14:212–221
Phrukkanon S, Burrow MF, Tyas MJ (1998) Effect of cross-sectional surface area on bond strengths between resin and dentin. Dent Mater 14:120–128
Tay FR, King NM, Suh BI, Pashley DH (2001) Effect of delayed activation of light-cured resin composites on bonding of all-in-one adhesives. J Adhes Dent 3:207–225
De Munck J, Van Meerbeek B, Yoshida Y, Inoue S, Suzuki K, Lambrechts P (2004) Four-year water degradation of a resin-modified glass-ionomer adhesive bonded to dentin. Eur J Oral Sci 112:73–83
Van Landuyt KL, Snauwaert J, De Munck J, Peumans M, Yoshida Y, Poitevin A, Coutinho E, Suzuki K, Lambrechts P, Van Meerbeek B (2007) Systematic review of the chemical composition of contemporary dental adhesives. Biomaterials 28:3757–3785
Yoshida Y, Nagakane K, Fukuda R, Nakayama Y, Okazaki M, Shintani H, Inoue S, Tagawa Y, Suzuki K, De Munck J, Van Meerbeek B (2004) Comparative study on adhesive performance of functional monomers. J Dent Res 83:454–458
Peumans M, Hikita K, De Munck J, Van Landuyt K, Poitevin A, Lambrechts P, Van Meerbeek B (2007) Effects of ceramic surface treatments on the bond strength of an adhesive luting agent to CAD-CAM ceramic. J Dent 35:282–288
Stewart GP, Jain P, Hodges J (2002) Shear bond strength of resin cements to both ceramic and dentin. J Prosthet Dent 88:277–284
Roulet JF, Soderholm KJ, Longmate J (1995) Effects of treatment and storage conditions on ceramic/composite bond strength. J Dent Res 74:381–387
Brentel AS, Ozcan M, Valandro LF, Alarca LG, Amaral R, Bottino MA (2007) Microtensile bond strength of a resin cement to feldpathic ceramic after different etching and silanization regimens in dry and aged conditions. Dent Mater 23:1323–1331
Frankenberger R, Sindel J, Kramer N, Petschelt A (1999) Dentin bond strength and marginal adaptation: direct composite resins vs ceramic inlays. Oper Dent 24:147–155
Ozturk N, Aykent F (2003) Dentin bond strengths of two ceramic inlay systems after cementation with three different techniques and one bonding system. J Prosthet Dent 89:275–281
Behr M, Rosentritt M, Regnet T, Lang R, Handel G (2004) Marginal adaptation in dentin of a self-adhesive universal resin cement compared with well-tried systems. Dent Mater 20:191–197
Chieffi N, Chersoni S, Papacchini F, Vano M, Goracci C, Davidson CL, Tay FR, Ferrari M (2006) Effect of the seating pressure on the adhesive bonding of indirect restorations. Am J Dent 19:333–336
Chieffi N, Chersoni S, Papacchini F, Vano M, Goracci C, Davidson CL, Tay FR, Ferrari M (2007) The effect of application sustained seating pressure on adhesive luting procedure. Dent Mater 23:159–164
Acknowledgments
The authors would like to thank the manufacturers for supplying materials for this study.
K. L. Van Landuyt has been granted a Postdoctoral Research Fellowship of the Research Foundation-Flanders (FWO). This study was supported in part by the FWO No. G.0206.07 and the KULeuven OT/06/55 research grants.
Conflicts of interest
There are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sarr, M., Mine, A., De Munck, J. et al. Immediate bonding effectiveness of contemporary composite cements to dentin. Clin Oral Invest 14, 569–577 (2010). https://doi.org/10.1007/s00784-009-0327-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-009-0327-8