Abstract
The aim of the study was to evaluate the influence of fatigue and cementation mode on the fracture behavior of endodontically treated bovine incisors restored with zirconium dioxide posts and crowns. Forty-eight endodontically treated bovine primary incisors were restored with zirconium dioxide posts (Cerapost, Brasseler), composite build-ups, and crowns cast from a chromium cobalt alloy. In 16 teeth, each of the posts was cemented conventionally with KetacCem (3M ESPE) or adhesively with Panavia F (Kuraray) or RelyX UniCem (3M ESPE). One-half of the specimens in each group were subjected to thermocycling with 10,000 cycles at 5–55°C and mechanical aging, loading the specimens at an angle of 45° in 1,200,000 cycles with 50 N. Fracture resistance was determined by loading the specimens until fracture at an angle of 45° to the long axis of the teeth. The loading test showed that neither cementation mode nor fatigue testing had an influence on the load bearing capability. Most specimens fractured in a favorable way, independent from the type of cementation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Metal post-and-core foundations may negatively affect the esthetic outcome of all-ceramic restorations of endodontically treated teeth, e.g., by altering light transmission [11, 47].
In addition to post systems based on the classical materials (e.g., precious gold alloys or titanium), tooth-like colored materials (e.g., ceramics and composites) have been introduced [10, 24]. Zirconium dioxide and glass (or quartz) fiber-reinforced composites (FRC), in particular, are the foundation of many modern post-and-core concepts [27].
Zirconium dioxide posts can be fixed conventionally, as well as adhesively [33, 36]; the dentin-like Young’s modulus of FRC posts and its postulated protective effect on root fractures due to force peaks, as transmitted by rigid materials, makes an adhesive cementation necessary [14, 25].
It has been reported that the formation of resin tags, adhesive lateral branches, and a resin dentin interdiffusion zone is possible to achieve with available adhesive systems applied on root dentin [2]; some studies have demonstrated improved retention of posts [31] and decreased microleakage [1] and higher fracture resistance [28] of teeth when posts are cemented with a resin cement than with other cements.
However, the bond strength to root dentin may be influenced by a variety of factors [14], e.g., sclerotic processes and the deposition of secondary and tertiary dentin [37], structural differences between radicular dentin and coronal dentin [12, 46] or the presence of provisional cements, endodontic sealers, and rinsing solutions [40, 41].
In general, conventional cements offer some advantages over resin cements, including lower costs and less complicated procedures with less opportunities for procedural errors [7, 29, 37].
This in vitro study investigated the influence of thermomechanical fatigue testing and cementation mode on the fracture behavior of severely damaged bovine incisors restored with zirconia posts covered by a full metal crown.
The hypotheses were as follows: (1) Irrespective of fatigue testing, severely damaged bovine incisors restored with crowns and conventionally cemented zirconium oxide posts do not show a lower fracture resistance than do incisors with crowns and adhesively luted posts, and (2) no difference exists between the use of conventional cementation compared to adhesive luting of zirconia posts concerning the failure mode.
Materials and methods
Forty-eight bovine primary incisors with mature root development, a straight root with a minimum length of 16 mm and a similar diameter, were decapitated at a distance of 16 mm from the apex and randomly divided into six groups (n = 8); the specimens were stored in a solution of water and 0.1% thymol at room temperature. Teeth were removed from the thymol solution only for the purpose of processing them as specimens in the study.
The root canals were instrumented in a crown-down technique to an apical size of ISO 40 and obturated with gutta-percha (Coltene/Whaledent, Langenau, Germany) and sealer (AH plus, Dentsply DeTrey, Konstanz, Germany) using cold lateral condensation.
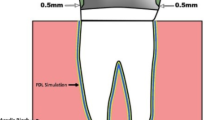
All teeth were embedded in an acrylic resin (Palapress Vario; Heraeus Kulzer GmbH, Hanau, Germany) cube. The acrylic level was adjusted 3 mm below the coronal plateau.
Table 1 shows the materials used for the restorative procedures in the test groups. The cylindro-conically shaped zirconium dioxide post Cerapost (Brasseler, Lemgo, Germany) with 1.75 mm in diameter was inserted in all specimens.
Thirteen-millimeter deep post spaces were prepared as measured from the coronal plateau using the system-specific preparation instruments, according to the manufacturer’s recommendations.
The posts in groups 1 and 2 were cemented in a conventional way using automatically mixed (Cap-Mix; 3M ESPE, Seefeld, Germany) glass ionomer cement (KetacCem, 3M ESPE, Seefeld, Germany).
In groups 3 and 4, the dentinal and post surfaces were conditioned by applying a self-etching primer (ED primer, Kuraray, Osaka, Japan). Panavia F 2.0 (Kuraray) was mixed for 30 s and applied to the total post surface. Following seating, excess cement was removed and light curing took place for 40 s.
In groups 5 and 6, RelyX UniCem (3M ESPE) was mixed automatically (Cap-Mix; 3M ESPE). The post was seated without further conditioning of the dentinal surfaces. Light curing took place after removing excess cement for 40 s.
The cores were built up in increments using a micro-hybrid composite (Herculite XRV, Kerr Hawe, Bioggio, Switzerland) after etching the dentin (15 s) with 37.5% phosphoric acid (Kerr Etchant, KerrHawe) and application of an adhesive system (Optibond FL, Kerr Hawe).
A 0.6-mm chamfer preparation for a crown was prepared with a tapered diamond bur (8878KP 018, Brasseler) with the finishing line ending 1.5 mm apical to the composite build-up. The palatal surface was prepared with an oval-shaped diamond bur (8899.314 031, Brasseler). The resulting total height of the prepared abutments was 6 mm on the vestibular face and 3 mm on the oral face. Crowns were cast from a chromium cobalt alloy (Remanium GM 800+, Dentaurum, Pforzheim, Germany) and cemented with glass ionomer cement (KetacCem).
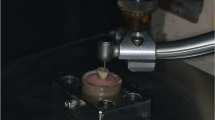
The samples in groups 2, 4, and 6 were subjected to thermocycling (Willytec, Gräfelfing, Germany) with 10,000 cycles at 5–55°C, and mechanical aging was performed in a chewing simulator (Willytec), loading the specimens at an angle of 45° in 1,200,000 cycles with 50 N.
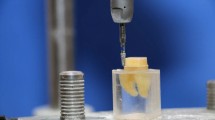
All samples were loaded until failure in a universal testing device (Zwick/Roell, Ulm, Germany) at an angle of 45° to the long axis of the roots using a stainless steel spherical antagonist (diameter: 4 mm) at a crosshead speed of 0.5 mm min−1, with the force transferred to the palatal surface 2 mm below the incisal edge. A sudden decrease in force of more than 30 N was regarded as an indication of failure, and the maximum force up to this point was recorded as the force at fracture.
Due to the chosen sample size (n = 8), the mean fracture loads were analyzed applying the non-parametric Kruskal–Wallis test. The level of significance was set at p < 0.05.
All samples were assessed for failure modes by visual inspection in combination with ink staining (Parker, Baden-Baden, Germany). “Favorable failures” were defined as repairable failures as fractures of the root on or above the level of bone simulation. “Unfavorable failures” were defined as unrepairable failures as root fractures below the level of bone simulation [15]. The results were reported using descriptive statistics.
Results
Table 2 and Fig. 1 show the results of load-bearing capacity testing. Specimens fractured at failure loads of 480 N (RelyX UniCem, fatigue testing) to 580 N (KetacCem, no fatigue testing). Comparing the different modes of cementation similar values for fracture load could be found, before fatigue testing as well as afterwards. The roots restored with conventionally cemented posts revealed the highest decrease in fracture resistance after fatigue loading. Nevertheless, the difference between fracture loads before and after artificial aging was not statistically significant.
Most specimens fractured in a favorable way, independent from the cementation variant (Table 3). Predominantly, post fractures together with root fractures on or above the simulated root level were observed.
Discussion
Bovine teeth were used in this study to provide a more uniform root anatomy and standardized sample length. Studies have reported little difference between human and bovine dentin as a bonding substrate [30, 39].
The specimens were stored in 0.1% thymol solution at room temperature. Thymol has an anti-fungal action, less influence on the adhesive mechanisms in comparison to alternative storage media (e.g., saline or formalin), and has been repeatedly described in other studies [17, 19].
In this study, the crowns were cast from a cobalt chrome alloy. This is not reflective of clinical practice, but is a technically and financially less expensive method to simulate a full coverage restoration in an in vitro setting.
Clinical failures of dental restorations most commonly result from fatigue [42]. Therefore, all specimens were artificially aged, applying dynamic thermal and mechanical loading with similar parameters as found in the scientific literature to simulate about 5 years of clinical function [20, 23]. Dynamic and static loading were performed at an angle of 45° to the long axis of the roots to simulate a clinical situation, which represents a biomechanical “worst case scenario”. This is also in accordance with published reports about post-and-core fracture and fatigue testing of endodontically treated teeth [22, 34].
Regarding the fracture behavior, the use of zirconium dioxide posts showed no differences compared with titanium or cast gold posts when restoring endodontically treated teeth with substantial horizontal loss of the clinical crown [20, 32]. Fatigue studies have shown the influence of post properties on the restoration behavior and indicated that posts, which exhibit physical properties close to the dentin, allow minimization of the incidence of adhesive failures or specimen fractures [21, 22, 26].
However, the superiority of posts with a dentin-like modulus of elasticity, which is reported in a number of publications and is attributed to more advantageous stress distribution to the residual tooth structure [13, 18], could not be confirmed in all studies on this topic. The rigidity of post-and-core systems seems to have no influence on the fracture behavior of severely damaged endodontically treated teeth with limited ferrule [16].
In current scientific literature, failures of the ceramic post-tooth complex were predominantly described as fractures of the posts, without root fractures. The fracture of the ceramic post seems to absorb most of the energy, thereby saving the remaining root from fracture [15]. In the present study, we observed predominantly post fractures together with root fractures on or above the simulated root level. A reason for this finding may be found in the chosen test set-up. A sudden decrease in force of more than 30 N was regarded as an indication of failure; it may be that the decrease in force after post fracture did not reach 30 N and load was transferred on the specimen until fracture of the dental hard tissue.
Although hydrofluoric acid etching and the application of a silane-coupling agent to silica-based ceramics increase the bond strength between all-ceramic restorations and composite resins [35], these techniques do not improve the bond strength of zirconium and alumina ceramics, as their high crystalline content renders them resistant to acid etching [8]. Studies on the shear bond strength to zirconia ceramic have shown that a composite resin cement containing an adhesive phosphate monomer provides significant bond strength values [5].
Nevertheless, in an in vitro evaluation of push-out bond strength of various luting agents to tooth-colored posts, fiber-reinforced composite posts demonstrated significantly higher bond strength values compared to the zirconium oxide posts [4].
In the present study, we compared two adhesive phosphate monomer containing resin cements, which showed a strong bond to zirconium oxide ceramic in previous in vitro investigations and one glass iomomer cement [4, 45]. In a study on the effects of luting agent and thermocycling on bond strength to root canal dentine, the self-adhesive resin cement RelyX UniCem revealed higher bond strength values compared to Panavia F used together with its corresponding bonding agent [3]. Despite this findings, varying the luting agents did not affect the failure mode of the specimens in our study.
Furthermore, applying a glass ionomer cement did not result in a lower fracture resistance nor a less advantageous fracture mode, though other authors did not recommend conventional cementation of zirconium dioxide posts, due to low bond strength values to post and root dentin [4, 9].
Despite a presumed negative effect on the bonding of zirconia posts to root dentin [6, 9], fatigue loading showed no effect on the fracture resistance of endodontically treated and severely decayed bovine incisors restored with adhesively luted zirconia posts. Furthermore, there was no significant difference in the fracture behavior of specimens with conventionally and adhesively cemented posts. Therefore, hypotheses 1 and 2 of this study are confirmed.
Due to the high rigidity of the posts, the load-bearing capability of the restored tooth may be primarily dependent on the fracture resistance of the post and not on the post/hard tissue bonding.
The less technique-sensitive conventional cementation of zirconium dioxide posts seems to be further on a reliable alternative to luting procedures. Increased microleakage may be a problem of endodontically treated teeth restored with rigid, conventionally cemented posts [38, 43]; but uncertainty remains when predicting the clinical effect of microleakage. Valderhaug et al. [44] showed that root filled teeth with a high quality endodontic treatment and an optimal morphology of the conventionally cemented cast post and core have a similar survival rate as crowned teeth with a vital pulp over an observation period of 25 years. The incidence of periapical lesions on radiographs was low for both groups.
Conclusion
With respect to fracture behavior, adhesive fixation of zirconium dioxide posts bears no advantage over conventional cementation.
References
Bachicha WS, DiFiore PM, Miller DA, Lautenschlager EP, Pashley DH (1998) Microleakage of endodontically treated teeth restored with posts. J Endod 24:703–708
Bitter K, Paris S, Martus P, Schartner R, Kielbassa AM (2004) A confocal laser scanning microscope investigation of different dental adhesives bonded to root canal dentine. Int Endod J 37:840–848
Bitter K, Meyer-Lueckel H, Priehn K, Kanjuparambil JP, Neumann K, Kielbassa AM (2006) Effects of luting agent and thermocycling on bond strengths to root canal dentine. Int Endod J 39:809–818
Bitter K, Priehn K, Martus P, Kielbassa AM (2006) In vitro evaluation of push-out bond strengths of various luting agents to tooth-colored posts. J Prosthet Dent 95:302–310
Blatz MB, Chiche G, Holst S, Sadan A (2007) Influence of surface treatment and simulated aging on bond strengths of luting agents to zirconia. Quintessence Int 38:745–753
Bottino MA, Baldissara P, Valandro LF, Galhano GA, Scotti R (2007) Effects of mechanical cycling on the bonding of zirconia and fiber posts to human root dentin. J Adhes Dent 9:327–331
de la Macorra JC, Pradies G (2002) Conventional and adhesive luting cements. Clin Oral Investig 6:198–204
Derand P, Derand T (2000) Bond strength of luting cements to zirconium oxide ceramics. Int J Prosthodont 13:131–135
Dietschi D, Ardu S, Rossier-Gerber A, Krejci I (2006) Adaptation of adhesive post and cores to dentin after in vitro occlusal loading: evaluation of post material influence. J Adhes Dent 8:409–419
Duret B, Duret F, Reynaud M (1996) Long-life physical property preservation and postendodontic rehabilitation with the Composipost. Compend Contin Educ Dent 20(Suppl):S50–S56
Fernandes AS, Shetty S, Coutinho I (2003) Factors determining post selection: a literature review. J Prosthet Dent 90:556–562
Ferrari M, Mannocci F, Vichi A, Cagidiaco MC, Mjor IA (2000) Bonding to root canal: structural characteristics of the substrate. Am J Dent 13:255–260
Ferrari M, Vichi A, Garcia-Godoy F (2000) Clinical evaluation of fiber-reinforced epoxy resin posts and cast post and cores. Am J Dent 13:15B–18B
Ferrari M, Vichi A, Grandini S (2001) Efficacy of different adhesive techniques on bonding to root canal walls: an SEM investigation. Dent Mater 17:422–429
Fokkinga WA, Kreulen CM, Vallittu PK, Creugers NH (2004) A structured analysis of in vitro failure loads and failure modes of fiber, metal, and ceramic post-and-core systems. Int J Prosthodont 17:476–482
Fokkinga WA, Kreulen CM, Le Bell-Ronnlof AM, Lassila LV, Vallittu PK, Creugers NH (2006) In vitro fracture behavior of maxillary premolars with metal crowns and several post-and-core systems. Eur J Oral Sci 114:250–256
Goodis HE, Marshall GW Jr., White JM, Gee L, Hornberger B, Marshall SJ (1993) Storage effects on dentin permeability and shear bond strengths. Dent Mater 9:79–84
Grandini S, Goracci C, Tay FR, Grandini R, Ferrari M (2005) Clinical evaluation of the use of fiber posts and direct resin restorations for endodontically treated teeth. Int J Prosthodont 18:399–404
Haller B, Hofmann N, Klaiber B, Bloching U (1993) Effect of storage media on microleakage of five dentin bonding agents. Dent Mater 9:191–197
Heydecke G, Butz F, Hussein A, Strub JR (2002) Fracture strength after dynamic loading of endodontically treated teeth restored with different post-and-core systems. J Prosthet Dent 87:438–445
Isidor F, Brondum K (1992) Intermittent loading of teeth with tapered, individually cast or prefabricated, parallel-sided posts. Int J Prosthodont 5:257–261
Isidor F, Odman P, Brondum K (1996) Intermittent loading of teeth restored using prefabricated carbon fiber posts. Int J Prosthodont 9:131–136
Krejci I, Reich T, Lutz F, Albertoni M (1990) An in vitro test procedure for evaluating dental restoration systems. 1. A computer-controlled mastication simulator. Schweiz Monatsschr Zahnmed 100:953–960
Kwiatkowski S, Geller W (1989) A preliminary consideration of the glass-ceramic dowel post and core. Int J Prosthodont 2:51–55
Lanza A, Aversa R, Rengo S, Apicella D, Apicella A (2005) 3D FEA of cemented steel, glass and carbon posts in a maxillary incisor. Dent Mater 21:709–715
Mannocci F, Ferrari M, Watson TF (1999) Intermittent loading of teeth restored using quartz fiber, carbon-quartz fiber, and zirconium dioxide ceramic root canal posts. J Adhes Dent 1:153–158
Meyenberg H, Lüthy H, Schärer P (1995) Zirconia posts: a new all-ceramic concept for nonvital abutment teeth. J Esthet Dent 7(2):73–80
Mezzomo E, Massa F, Libera SD (2003) Fracture resistance of teeth restored with two different post-and-core designs cemented with two different cements: an in vitro study. Part I. Quintessence Int 34:301–306
Morgano SM, Brackett SE (1999) Foundation restorations in fixed prosthodontics: current knowledge and future needs. J Prosthet Dent 82:643–657
Nakamichi I, Iwaku M, Fusayama T (1983) Bovine teeth as possible substitutes in the adhesion test. J Dent Res 62:1076–1081
Nissan J, Dmitry Y, Assif D (2001) The use of reinforced composite resin cement as compensation for reduced post length. J Prosthet Dent 86:304–308
Nissan J, Parson A, Barnea E, Shifman A, Assif D (2007) Resistance to fracture of crowned endodontically treated premolars restored with ceramic and metal post systems. Quintessence Int 38:e120–e123
Nothdurft FP, Pospiech PR (2006) Clinical evaluation of pulpless teeth restored with conventionally cemented zirconia posts: a pilot study. J Prosthet Dent 95:311–314
Nothdurft FP, Seidel E, Gebhart F, Naumann M, Motter PJ, Pospiech PR (2008) Influence of endodontic posts on the fracture behavior of crowned premolars with class II cavities. J Dent 36:287–293
Ozcan M, Vallittu PK (2003) Effect of surface conditioning methods on the bond strength of luting cement to ceramics. Dent Mater 19:725–731
Paul SJ, Werder P (2004) Clinical success of zirconium oxide posts with resin composite or glass-ceramic cores in endodontically treated teeth: a 4-year retrospective study. Int J Prosthodont 17:524–528
Pospiech P (2002) All-ceramic crowns: bonding or cementing? Clin Oral Investig 6:189–197
Reid LC, Kazemi RB, Meiers JC (2003) Effect of fatigue testing on core integrity and post microleakage of teeth restored with different post systems. J Endod 29:125–131
Rueggeberg FA (1991) Substrate for adhesion testing to tooth structure—review of the literature. Dent Mater 7:2–10
Sung EC, Tai ET, Chen T, Caputo AA (2002) Effect of irrigation solutions on dentin bonding agents and restorative shear bond strength. J Prosthet Dent 87:628–632
Tjan AH, Nemetz H (1992) Effect of eugenol-containing endodontic sealer on retention of prefabricated posts luted with adhesive composite resin cement. Quintessence Int 23:839–844
Torbjorner A, Fransson B (2004) A literature review on the prosthetic treatment of structurally compromised teeth. Int J Prosthodont 17:369–376
Usumez A, Cobankara FK, Ozturk N, Eskitascioglu G, Belli S (2004) Microleakage of endodontically treated teeth with different dowel systems. J Prosthet Dent 92:163–169
Valderhaug J, Jokstad A, Ambjornsen E, Norheim PW (1997) Assessment of the periapical and clinical status of crowned teeth over 25 years. J Dent 25:97–105
Wegner SM, Kern M (2000) Long-term resin bond strength to zirconia ceramic. J Adhes Dent 2:139–147
Yoshiyama M, Carvalho RM, Sano H, Horner JA, Brewer PD, Pashley DH (1996) Regional bond strengths of resins to human root dentine. J Dent 24:435–442
Zalkind M, Hochman N (1998) Esthetic considerations in restoring endodontically treated teeth with posts and cores. J Prosthet Dent 79:702–705
Conflict of interest statement
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nothdurft, F.P., Schmitt, T., Motter, P.J. et al. Influence of fatigue testing and cementation mode on the load-bearing capability of bovine incisors restored with crowns and zirconium dioxide posts. Clin Oral Invest 12, 331–336 (2008). https://doi.org/10.1007/s00784-008-0205-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-008-0205-9