Abstract
Background
Night pain is a particularly vexing symptom in patients with rotator cuff tear. It disturbs sleep and decreases quality of life, and there is no consensus regarding its etiology. Based on arthroscopic surgical observations of synovitis around the rotator interval or capsule surface in rotator cuff tear, we hypothesized that blood flow from the artery feeding the capsule increases blood supply to the synovium. This study aimed to investigate the relationship between blood flow and night pain using pulse Doppler ultrasonography.
Methods
A series of 47 consecutive patients with rotator cuff tear was evaluated. The peak systolic velocity and resistance index of blood flow in the ascending branch of the anterior humeral circumflex artery were evaluated using pulse Doppler ultrasonography. We also investigated 20 normal shoulders in healthy volunteers. The peak systolic velocity and resistance index were compared between affected and unaffected sides in patients and between dominant and nondominant sides in controls.
Results
Anterior humeral circumflex artery peak systolic velocity and resistance index did not differ between sides in control subjects or in patients with rotator cuff tear without night pain. However, anterior humeral circumflex artery peak systolic velocity and resistance index did differ significantly between sides in patients with rotator cuff tear with night pain.
Conclusions
This study revealed anterior humeral circumflex artery hemodynamics in patients with rotator cuff tear and normal subjects using Doppler ultrasonography. Night pain, particularly involving aching, appears to be related to the hemodynamics. These findings suggest that investigating the hemodynamics of patients with rotator cuff tear with night pain may lead to greater understanding of the etiology of this symptom.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Night pain is frequently encountered among patients with shoulder problems. In 1934, Codman wrote in “The Shoulder” [1] that “Severe night pain is typical in a patient with rotator cuff pathology.” Rotator cuff pathology with night pain has been reported to arise from impingement [2], increasing subacromial pressure [3, 4], changing skin temperature [5] or synovitis [6, 7]. However, no consensus concerning the underlying cause of night pain in patients with shoulder problems has been reached.
During arthroscopic surgery, hyperemic synovitis is often observed around the rotator interval or joint capsule in patients with rotator cuff tear (RCT). Therefore, we hypothesized that synovitis may cause the severe night pain, with increased synovial blood flow possibly leading to increased blood flow of the artery feeding the capsule.
Previous studies have investigated the vascular anatomy around the shoulder, including the humeral head [8, 9], rotator cuff [10–12], glenoid labrum [13] and capsule. Andary et al. [14] reported the vascular anatomy of the glenohumeral capsule, a well-vascularized structure with direct predictable contributions from four arteries [anterior humeral circumflex (AHCA), posterior humeral circumflex, suprascapular and circumflex scapular]. The AHCA provides the major blood supply to the lateral portion of the capsule. Vessels from the AHCA ascend along the anterior humeral insertion and arborize medially to supply the anterior part of the lateral aspect of the capsule [14]. Previous studies have directly evaluated whole blood flow of the shoulder joint using power Doppler ultrasonography or dynamic magnetic resonance imaging (MRI) [15–18] in the inflammatory condition of the shoulder. Power Doppler ultrasonography results were semiquantitative because synovium vessels were nonspecific and data measuring blood flow were not reproducible. Dynamic MRI results, on the other hand, were quantitative, but this examination is inconvenient and invasive. No previous report has evaluated the relationship between shoulder night pain and blood flow in specific arteries. Therefore, in the present study, we assessed a specific artery, the AHCA—which is easily identifiable and reproducible because of clear bony landmarks, such as the bicipital groove—in relation to shoulder night pain.
Materials and methods
Study subjects
From August 2010 to July 2011, the shoulder morphology of 106 consecutive patients who visited the outpatient clinic of our hospital for the first time reporting shoulder pain was examined using ultrasonography and radiography. Of these patients, 47 showed RCT and were selected as candidates for this prospective study. Twenty normal shoulders in healthy volunteers who had no history of shoulder pain were chosen to serve as the control group. Patient demographics are shown in Table 1. There were no significant differences in age among the three groups (P > 0.05).
Definition of night pain
Night pain associated with shoulder problems is likely to have several pathologies: Some patients report awakening to aching pain that is relieved by sitting or heating, whereas others are awakened by a piercing pain while rolling over or by a pressing pain while in the lateral decubitus position, which is relieved by changing position. Among these presentations, the most confusing problem is aching pain that disturbs sleep [1]. Therefore, in this study, night pain was defined as an aching pain that disturbs sleep, causing the patient to want to sit. Given this definition, we carefully interviewed patients for these characteristics of night pain. Movement-related pain, such as when rolling over, and compression pain on the affected side in the lateral position were excluded.
Ultrasonographic evaluation
Sonographic examinations were performed independently by two experienced sonographers, each with at least 10 years of ultrasound experience and extensive experience in musculoskeletal ultrasonography, using a 5–13-MHz linear array transducer (ProSound Alpha 7; Hitachi-Aloka Medical, Ltd., Tokyo, Japan). The same Doppler settings were used for all examinations, with no adjustment of Doppler parameters. The gain setting for color Doppler was just below noise level, and the system was adjusted to detect flow with higher sensitivity. During Doppler ultrasonography, patients remained in a sitting position with 90° elbow joint flexion and the hand resting palm up on the thigh during examination of the AHCA, and 90° elbow joint flexion and 45° shoulder joint abduction during examination of the brachial artery (BA). Before the color Doppler ultrasonographic examination, patients rested for 5 min.
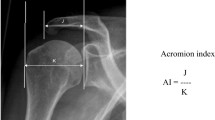
Measurement of artery velocity
AHCA and BA blood flow were assessed using color Doppler ultrasonography and pulse Doppler ultrasonography to determine the peak systolic velocity (PSV) and resistance index (RI = PSV − end diastolic velocity/PSV). Fundamental color Doppler mode was used first to identify an adequate scanning plane that clearly depicted the bicipital groove and laterally adjacent AHCA on the transverse scan (Fig. 1a). Pulse Doppler mode then was used to measure the velocity of the AHCA on the longitudinal scan (Fig. 1b). The sample volume was set within the AHCA, and the incident angle between the AHCA, and Doppler beam was kept at 60° or less (Fig. 1c). To assess the BA, the transducer was placed on the medial humerus. The sample volume was set within the BA, and the incident angle between the BA and Doppler beam was kept at 60° or less. Each shoulder was evaluated three times, and mean values were calculated.
a Short axis color Doppler US images of the bicipital groove. The ascending branch of the anterior humeral circumflex artery (arrow) is located on the lateral side of the biceps tendon. b Long axis color Doppler US images of the ascending branch of the anterior humeral circumflex artery (arrow). c Pulse Doppler US images peak systolic velocity (arrow) and end diastolic velocity (arrowhead)
Reproducibility of measured AHCA velocity
In a pilot study, intra- and interobserver reliabilities were assessed by examining five healthy subjects. AHCA velocity was measured five times for each subject by two experienced sonographers. Intra- and interobserver reliabilities were estimated using calculations of intraclass correlation coefficients (ICCs; one-way analysis of variance and two-way analysis of variance, respectively). Intraobserver reproducibility was high for both observers (observer A, ICC = 0.983; observer B, ICC = 0.969), as was interobserver reproducibility (ICC = 0.949). The statistical program used for the calculations was IBM SPSS staistics 19.0 (IBM, SPSS, Chicago IL).
Ethics
The Ethics Committee of Gifu University School of Medicine approved the study, and all patients provided written informed consent before participating.
Statistical analyses
Statistical analysis was performed using GraphPad Prism version 5.01 (GraphPad Software, La Jolla, CA). Outcomes between affected and unaffected sides in patients and between dominant and nondominant sides in controls were compared using the Mann–Whitney U test. For comparison of more than two groups, analysis of was variance (ANOVA) was used.
Results
Comparison of PSV between affected and unaffected sides
PSV of the BA did not differ between affected and unaffected sides in any group (Table 2). However, patients with RCT with night pain showed significantly higher PSV of the AHCA on the affected side than on the unaffected side (affected side, 34.9 ± 16.5 cm/s; unaffected side, 15.8 ± 6.5 cm/s; P < 0.001). Patients with RCT without night pain and control subjects showed no significant difference in PSV of the AHCA between sides (Table 3).
Comparison of RI between affected and unaffected sides
Patients with RCT with night pain showed significantly lower RI of the AHCA on the affected side than on the unaffected side (affected side, 0.70 ± 0.090; unaffected side, 078 ± 0.11; P < 0.01). On the other hand, patients with RCT without night pain and control subjects showed no significant difference in RI of the AHCA between sides (Table 4).
Discussion
In our study, although BA blood flow showed no change between all pathologic conditions, AHCA blood flow was altered in patients with RCT with night pain. In particular, these patients showed significantly higher PSV and significantly lower RI of the AHCA on the affected side than on the unaffected side. We conclude that these hemodynamic differences reflect a selective and pathognomonic change.
Interestingly, ICC was high in healthy volunteers and may be related to the anatomical features of AHCA. Despite being a small artery, the AHCA passes through the lateral side of the bicipital groove and under the transverse ligament. The bicipital groove is easily detected by gray-scale ultrasound; therefore, it is possible to detect the longitudinal image of AHCA. Moreover, PSV of this artery may be insusceptible to probe compression because of its location under the transverse ligament. These anatomical properties may account for the high ICC in the healthy volunteers.
Several reports have examined the relationship between the blood flow of the synovium and shoulder pain using power Doppler ultrasonography or dynamic MRI [15–18]. Matsuzaki et al. assessed signal intensity on dynamic MRI and arthroscopic and histological findings of the subacromial bursa and found signal intensity to be positively correlated with arthroscopic findings of redness and villous formation as well as histologic findings of capillary proliferation and papillary hyperplasia in RCT [16]. In idiopathic frozen shoulder, Tamai et al. reported that the glenohumeral joint (GHJ) and subacromial bursa demonstrated contrast enhancement on dynamic MRI. Moreover, the values for the GHJ were greater than those for the subacromial bursa [15]. Several studies have investigated rheumatoid arthritis (RA) using power Doppler ultrasonography and reported increased blood flow of the synovium around the rotator cuff and bicipital groove [18, 19]. For example, Strunk et al. reported that power Doppler ultrasonography demonstrated increased vascularity in the long bicipital tendon sheath of patients with RA [15]. These results suggest that blood flow may increase because of synovitis in symptomatic shoulders. However, these studies did not investigate a specific relationship between blood flow and shoulder night pain.
In this study, RI of the AHCA on the affected side was decreased compared with that on the unaffected side in patients with RCT with night pain. Terslev et al. reported that a low RI value indicates an inflammatory condition in RA. Although peripheral diastolic blood flow is usually low, diastolic blood flow increases to supply blood to the synovium in inflammatory conditions, leading to a relative decrease in RI [20]. Accordingly, our results may suggest an inflammatory condition in patients with RCT with night pain.
Patients with night pain sometimes take a hot shower or attempt to sleep in a sitting position to relieve pain [1]. These symptoms cannot be explained only by physical stimuli, such as rolling over or the lateral decubitus position. Certainly, changing the sleep position decreases the subacromial pressure [3, 21], which can explain the pain relief, but taking a hot shower cannot. In healthy humans, circulation is influenced by postural change [22], and exposure to a hot environment increases the skin blood flow and sweat rate, thus increasing heat dissipation and resulting in a reduction of central blood flow [23]. Miyakoshi et al. reported the circadian rhythm of shoulder skin temperature, which is characterized by high temperature during the daytime and low temperature at night. However, shoulders with a clear inflammatory condition do not decrease in skin temperature during the night. The authors proposed that this difference is influenced by intraarticular inflammation and that shoulder skin temperature may reflect various pathologic conditions of the shoulder joint, which is located close to the skin surface [5]. Intraarticular blood flow is influenced by intraarticular inflammation, environmental temperature and postural change. Therefore, we believe that change in intraarticular blood flow may be able to explain the distinctive symptom of night pain in RCT.
This study has several limitations. We did not evaluate blood pressure or measure the diameter of the AHCA; therefore, these data may have differed between shoulders. Hyperplasia of the microvasculature often occurs with inflammation in the bicipital groove, and examiners may misidentify the microvessels and the AHCA. As a result, Doppler US may mistakenly identify hyperplasia of microvessels instead of AHCA in these patients. Lastly, one hypothesis of this study was that PSV of the AHCA is lower in the sitting rather than the supine position. However, we did not measure blood flow of the AHCA with patients in the supine position; as such, changes in blood flow due to posture cannot be assessed from this study.
In conclusion, patients with RCT with night pain showed significantly higher PSV of the AHCA, indicating that increased intraarticular blood flow is one factor underlying the pathogenesis of night pain in patients with RCT. Assessment of PSV of the AHCA may help in the management of night pain in such patients.
References
Codman E. Rupture of the supraspinatus tendon and other lesions in or about the subacromial bursa. Florida: Krieger; 1934.
Buss DD, Freehill MQ, Marra G. Typical and atypical shoulder impingement syndrome: diagnosis, treatment, and pitfalls. Instr Course Lect. 2009;58:447–57.
Kempf B, Kongsted A. Association between the side of unilateral shoulder pain and preferred sleeping position: a cross-sectional study of 83 Danish patients. J Manip Physiol Ther. 2012;35:407–12.
Konishiike T, Hashizume H, Nishida K, Inoue H, Nagoshi M. Shoulder pain in long-term haemodialysis patients. A clinical study of 166 patients. J Bone Joint Surg Br. 1996;78:601–5.
Miyakoshi N, Itoi E, Sato K, Suzuki K, Matsuura H. Skin temperature of the shoulder: circadian rhythms in normal and pathologic shoulders. J Shoulder Elbow Surg. 1998;7:625–8.
Berghs BM, Sole-Molins X, Bunker TD. Arthroscopic release of adhesive capsulitis. J Shoulder Elbow Surg. 2004;13:180–5.
Yamaguchi K, Sethi N, Bauer GS. Postoperative pain control following arthroscopic release of adhesive capsulitis: a short-term retrospective review study of the use of an intra-articular pain catheter. Arthroscopy. 2002;18:359–65.
Gerber C, Schneeberger AG, Vinh TS. The arterial vascularization of the humeral head. An anatomical study. J Bone Joint Surg Am. 1990;72:1486–94.
Laing PG. The arterial supply of the adult humerus. J Bone Joint Surg Am. 1956;38:1105–16.
Moseley HF, Goldie I. The arterial pattern of the rotator cuff of the shoulder. J Bone Joint Surg Br. 1963;45:780–9.
Rothman RH, Parke WW. The vascular anatomy of the rotator cuff. Clin Orthop Relat Res. 1965;41:176–86.
Rathbun JB, Macnab I. The microvascular pattern of the rotator cuff. J Bone Joint Surg Br. 1970;52:540–53.
Cooper DE, Arnoczky SP, O’Brien SJ, Warren RF, DiCarlo E, Allen AA. Anatomy, histology, and vascularity of the glenoid labrum. An anatomical study. J Bone Joint Surg Am. 1992;74:46–52.
Andary JL, Petersen SA. The vascular anatomy of the glenohumeral capsule and ligaments: an anatomic study. J Bone Joint Surg Am. 2002;84:2258–65.
Tamai K, Mashitori H, Ohno W, Hamada J, Sakai H, Saotome K. Synovial response to intraarticular injections of hyaluronate in frozen shoulder: a quantitative assessment with dynamic magnetic resonance imaging. J Orthop Sci. 2004;9:230–4.
Matsuzaki S, Yoneda M, Kobayashi Y, Fukushima S, Wakitani S. Dynamic enhanced MRI of the subacromial bursa: correlation with arthroscopic and histological findings. Skeletal Radiol. 2003;32:510–20.
Breidahl WH, Newman JS, Taljanovic MS, Adler RS. Power Doppler sonography in the assessment of musculoskeletal fluid collections. AJR Am J Roentgenol. 1996;166:1443–6.
Stegbauer J, Rump LC, Weiner SM. Sites of inflammation in painful rheumatoid shoulder assessed by musculoskeletal ultrasound and power Doppler sonography. Rheumatol Int. 2008;28:459–65.
Strunk J, Lange U, Kurten B, Schmidt KL, Neeck G. Doppler sonographic findings in the long bicipital tendon sheath in patients with rheumatoid arthritis as compared with patients with degenerative diseases of the shoulder. Arthritis Rheum. 2003;48:1828–32.
Terslev L, Torp-Pedersen S, Qvistgaard E, Danneskiold-Samsoe B, Bliddal H. Estimation of inflammation by Doppler ultrasound: quantitative changes after intra-articular treatment in rheumatoid arthritis. Ann Rheum Dis. 2003;62:1049–53.
Werner CM, Ossendorf C, Meyer DC, Blumenthal S, Gerber C. Subacromial pressures vary with simulated sleep positions. J Shoulder Elbow Surg. 2010;19:989–93.
Schatz IJ. Orthostatic hypotension. I. Functional and neurogenic causes. Arch Intern Med. 1984;144:773–7.
Yamazaki F, Yamauchi K, Tsutsui Y, Endo Y, Sagawa S, Shiraki K. Whole body heating reduces the baroreflex response of sympathetic nerve activity during Valsalva straining. Auton Neurosci. 2003;103:93–9.
Acknowledgments
There was no external source of funding for this study.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Terabayashi, N., Watanabe, T., Matsumoto, K. et al. Increased blood flow in the anterior humeral circumflex artery correlates with night pain in patients with rotator cuff tear. J Orthop Sci 19, 744–749 (2014). https://doi.org/10.1007/s00776-014-0604-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00776-014-0604-5