Abstract
Background
In reconstruction by vascularized fibular graft (VFG) after wide resection of musculoskeletal tumors, there are problems such as the method of fixing the fibular graft, the period of achieving bone union, and the avoidance of postoperative fractures. We have performed VFG on 19 cases over a 30-year period. We have investigated these problems and now report the results.
Methods
From 1980 to 2009, we performed VFG on 19 cases to reconstruct the bone defect after resection of a musculoskeletal tumor. The mean age was 19.5 years. Reconstructed bone defects were located in the femur in 10 cases (1 of inlay graft, 1 of individual intercalary graft, 7 of intercalary graft into treated bone, 1 of curettaged bone marrow), the tibia in 3 cases (1 of individual intercalary graft, 2 of intercalary graft into treated bone), the humerus in 3 cases (2 of sling procedure, 1 of individual intercalary graft), the foot in 2 cases individual intercalary graft, and the sacroiliac joint in 1 case of individual intercalary graft. The mean follow-up period after surgery was 7.25 years. We evaluated the success of primary bone union, the period required to achieve bone union, complications, clinical outcome, and the Musculoskeletal Tumor Society (MSTS) score.
Results
Successful bone union was achieved for 79% of cases (15/19 patients). The average period required to achieve bone union was 7.8 months. There were 4 cases of non-union and 2 other complications. Clinical outcome status was continuous disease-free in 12 cases and died of disease in 7. The mean MSTS score was 98% (93–100%).
Conclusion
Vascularized fibular graft is a useful reconstructive procedure for long-bone defects after wide excision of musculoskeletal tumors. The method of fixation can be selected according to the situation; although times required for bone union are long, it is possible to prevent postoperative fractures by a combined approach with treated bone and/or double barrel fibular grafts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Because 5-year survival improves dramatically after resection of malignant musculoskeletal tumors, long-lasting durability is required in limb-salvage procedures. Reconstruction of bone defects after extensive resection of musculoskeletal tumors is one of the most difficult reconstruction procedures because of poor vascular beds and the negative effect of chemotherapy and/or radiation. A free vascularized fibular graft (FVFG), developed by Taylor et al. [1] in 1975, is a living bone graft which can be used for limb salvage and which is now widely used. Because the vascularized fibular graft (VFG) is a living bone graft it can be performed even for bone-receiving parts which have widespread bone loss and are in poor vascular condition as a result of preoperative chemotherapy and/or radiation, and because it is a tubular bone the shape is straight. We performed FVFG or pedicle vascularized fibular graft (PVFG) to reconstruct extensive bone defects after resection of bone tumors in 19 patients over the past 30 years. In reconstruction by VFG after wide resection of musculoskeletal tumors, there are problems such as the method of fixing the fibular graft, the period of achieving bone union, and the avoidance of postoperative fractures. Our results were investigated and are reported here.
Materials and methods
Institutional review board approval was obtained before publication of this report, and the cases gave their consent to be involved in this study and for publication of their data, but we could not obtain consent for some cases who passed away or who could not be contacted because their whereabouts were unknown.
FVFG and PVFG were performed in 20 cases out of 86 cases involving reconstruction of bone defects after wide resection of musculoskeletal tumors performed over a period of 30 years, from 1980 to 2009, at our institution. Of these cases we investigated 19 cases, excluding one case in which amputation was performed immediately after the operation because of tumor cell positivity of the resection stump. Fundamentally, VFG was used for reconstruction of bone defects in which the joint was not reconstructed; prostheses were used in reconstruction of joint surfaces. Table 1 shows the age, gender, diagnosis, location, length of the bone defect, preoperative chemotherapy, preoperative radiation therapy, surgery, resected margin, type of vascular anastomosis, and length of fibula graft. We performed FVFG in 16 cases and PVFG in 3. There were 9 males and 10 females, with an age range of 5–49 years (average 19.5 years). The location of the tumor was the femur in 10 cases (1 case of arthrodesis for knee joint inlay graft with a intramedullary rod and 1 case of intercalary graft, 7 cases of intercalary graft into treated bone, 1 case present in curettaged bone marrow); the tibia in 3 cases (1 case of individual intercalary graft, 2 cases of intercalary graft into treated bone); the humerus in 3 cases (2 cases of sling procedure (replacement of the proximal humerus by use of free vascularized fibula including the fibula head; the tendons of biceps femoris and palmaris longus together with a transient stainless-steel wire were used to suspend the head of the fibula from the remaining part of the scapula, usually the acromion; the peroneal artery was anastomosed to the deep brachial artery [2]), 1 case of individual intercalary graft); the foot in 2 cases (2 cases of individual intercalary graft), and the sacroiliac joint in 1 case (1 case of individual intercalary graft). The pathological diagnosis was osteosarcoma in 11 cases, Ewing’s sarcoma in 2, adamantinoma in 2, and chondrosarcoma, synovial sarcoma, malignant fibrous histiocytoma (MFH), and desmoid tumor in 1 case each. The preoperative treatment consisted of chemotherapy alone in 13 cases and a combination of chemotherapy and radiotherapy in 3. As an intraoperative bone treatment, radiation was performed in 4 cases and pasteurization in 5. A VFG was used together with the treated bone in 9 cases (the treated bone was hollowed out conforming to the shape of the fibula graft, with the central part removed, and the graft was transplanted into the central part of the treated bone), with double barrel graft in 3 cases. The method of fixation was an intramedullary rod in 1 case (Case 1), Kirschner wires in 5 cases (Cases 2, 3, 4, 10, and 18), plates in 9 cases (Cases 5, 6, 7, 8, 9, 13, 15, 16, and 17), Kirschner wires + plates in 1 case (Case 19), an extrafixation-added Kirschner wire in 1 case (Case 14), screws in 1 case (Case 12), and without fixation in 1 case (Case 11). When the graft was taken out including the head of the bone, the lateral collateral ligaments fixed the tibio-fibular joint side of the tibia. To prevent instability of the foot joints after the graft was harvested, a 7 cm length from the distal end of the graft was retained. The length of the bone defect was 8–24 cm (average 15.4 cm), and the length of the harvested bone was 10–28 cm (average 19.3 cm). The postoperative follow-up period ranged from 1 to 20.7 years (average 7.25 years). The type of vascular anastomosis was end-to-end in 13 cases and end-to-side in 2 (in principle, in the superior limbs, a branch of the brachial artery was made the recipient, in the femurs, a branch of the femoral artery, a branch of the popliteal artery was made the recipient, whereas the peroneal arteries and veins were used in the blood vessels of the donors). For postoperative after-treatment, early pendulum exercise was started in the superior limbs. In the inferior limbs, a partial load was started, using an ischium-supporting non-weight-bearing brace, while union of the bone was observed, and the load was gradually increased. We evaluated the period required to achieve bone union (by verifying callus formation in simple X-ray photographs), postoperative complications, local recurrence, additional operations, clinical outcome, and MSTS score (we could evaluate, retrospectively, Cases 2, 8, 12, 16, 17, 18); the lateral-diameter hypertrophy of the transplanted graft bone was evaluated for Cases 1, 4, 10, 12, and 18, the cases in which there were postoperative complications and the cases in which intercalary grafts were performed in the centers of the treated bones, excluding three cases which could not be evaluated (Figs. 1, 2).
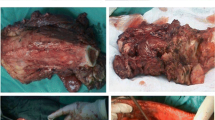
Case 17. A 15-year-old female with parosteal osteosarcoma of the right distal femur. A Periosteal reaction at the posterior aspect of the right femur is seen by X-ray at the time of the first visit (arrow) (a). Gadolinium-enhanced MRI shows high accumulation (b coronal view, c axial view). B Specimen after wide resection (a). Resected bone after tumor removal and pasteurization (b). C Postoperative X-ray after reconstruction, an FVFG and a pasteurized bone were fixed with an A-O Tube plate® (a). X-ray shows bone union 7 months after surgery (b). X-ray taken 10 years after surgery (c)
Case 18. A 17-year-old male with Ewing sarcoma of the right foot. Preoperative gadolinium-enhanced MRI reveals a tumor involving the 1st, 2nd, and 3rd metatarsals (A coronal view, B sagittal view). Preoperative X-rays show periosteal reaction at the base of the 2nd and 3rd metatarsals (arrows) (C, D). Reconstruction was carried out by double barrel FVFG that was fixed with transverse Kirschner wires, and the skin defect was covered with a cutaneous flap (E). 6 years after surgery, X-ray shows bone union (F)
Results
Successful bone union was achieved for 79% of cases (15/19 patients). We performed 9 VFG from 1980 to 1989 and 10 VFG from 1990 to 2009. Since 1990, successful bone union has been achieved in 100% of cases (10/10 patients). Time to achievement of bone union ranged from 5 to 12 months (average 7.8 months). The resection margin involved a wide margin in 18 cases and an intralesional margin in 1 case that was followed by amputation. The clinical outcome status was continuous disease free (CDF) for 12 cases and dead of disease (DOD) for 7. Postoperative complications occurred in 6 patients. There were 4 non-union cases. Of these, 3 infectious non-unions were salvaged with knee rotation plasty (Cases 5, 7, and 9), and 1 non-union was salvaged with arthrodesis (Case 3). There were 2 other complications. A postoperative stress fracture was noted in 1 patient with adamantinoma of the tibia that had been reconstructed by ipsilateral PVFG; this was successfully treated with contralateral FVFG (Case 2).
Delayed union, in which bone union took longer than 6 months, occurred in 93.3% (14/15) of the cases. Volkmann contracture was found in 1 patient with osteosarcoma of the humerus (the cause was believed to be injury of the brachial artery and median nerve during the operation), and disarticulation of the shoulder joint was performed at 7 years after surgery at the patient’s request (Case 19).
Two of the 4 patients who underwent intraoperative radiation during surgery developed postoperative infections (Cases 5, 7). No postoperative infections were found in cases in which pasteurized bone was used (Cases 13, 14, 15, 16, and 17).
The mean MSTS Score was 98% (93–100%). The mean amount of hypertrophy fibular graft was 42% (0–80%).
Discussion
There have been many articles on the use of vascularized fibular grafts to reconstruct the extremity after resection of a malignant tumor. Most have reported good results [2, 4–14, 16]. Malizos et al. [4] stated that such a graft seems to be indicated when there is a bone defect of at least 5 cm and the blood supply from the surrounding soft tissues is deficient. Enneking et al. [5] reported very low success of bone union in non-vascularized bone grafts involving bone defects of longer than 7 cm. VFG therefore seems to be indicated for defects longer than 7 cm. FVFG and PVFG are widely recognized as a means of reconstructing bone defects, but the surgical technique is demanding.
Overall success of VFG union for our patients was 79% (15/19 patients). Several articles have reported the success of bone union by VFG. Yajima et al. [6] reported achieving bone union in 19 of 20 (95%) patients who underwent FVFG for reconstruction of the femur. Usui et al. [7] reported bone union in 88% (36/41), and Shimose et al. [8] reported 94% (16/17). Minami et al. [9] reported primary bone union in 84% of cases and eventual successful bone union of 95%. The success of VFG bone union in our cases was 79% (15/19). Calculated by year, our success in bone union was 56% (5/9) in the first 10 years, and it improved to 100% (10/10) in the last 20 years. Several factors might have affected this improvement—the learning curve, reduced post-operative infection because of a change of bone treatment from radiation to pasteurization, use of double barrel graft, and use of end to side vessel anastomosis.
The incidence of postoperative bone fractures after single VFG was reported to be 33.3% (14/42) by de Boer et al. [10] and 11.1% (3/27) by Hsu et al. [11]. Postoperative fractures after use of several procedures of single, and double barrel fibula graft were reported to be 15.9% (36/41 patients) by Usui [7], 17.6% (3/17) by Shimose et al. [8], and 14.4% (15/104) by Minami et al. [9].
Jones et al. [12] and Hou and Liu [13] reported no postoperative fracture after use of double barrel fibula grafts.
Okubo et al. [14] reported that 2 fibular grafts are needed for extensive defects of the femur, even though a long operation time may be required. Jupiter et al. [15] reported a successful case using FVFG that was cut and folded into 2 for 11-centimeter segments on a single vascular pedicle. Jones et al. [12] reported a “double barrel” graft that achieved folded grafts with one pedicle vessel. Toh et al. [16] reported that double barrel FVFG on a single vascular pedicle can be used to fill the defect up to 14 cm. Hou and Liu [13] reported that 2 fibular grafts provide adequate strength for reconstruction of the femur with no postoperative bone fracture. The only patient suffering a postoperative fracture in our series was the patient who underwent a intercalary graft without treated bone on the tibia (6.6%; 1/15). The incidence seemed lower than that reported by others. Less postoperative fractures might be achieved by the use of treated bone and double barrel fibular grafts.
Vascularized fibular graft is a useful procedure for reconstruction of long bone defect. Regarding treatment of the resected bone, pasteurization proved safer and better than irradiation according to our results. Double barrel fibular grafts improved the success of bone union and prevented postoperative fractures.
References
Taylor GI, Miller GD, Ham FJ. The free vascularized bone graft: a clinical extension of microvascular techniques. Plast Reconstr Surg. 1975;55:533–44.
Wada T, Usui M, Isu K, Yamawakii S, Ishii S. Reconstruction and limb salvage after resection for malignant bone tumor of the proximal humerus. J Bone Joint Surg. 1999;81-B(5):808–13.
Boer HH, Wood MB. Bone changes in the vascularized fibular graft. J Bone Joint Surg. 1989;71-B(3):374–8.
Malizos KN, Zalavras CG, Soucacos PN, Beris AE, Urbaniak JR. Free vascularized fibular grafts for reconstruction of skeletal defects. J Am Acad Orthop Surg. 2004;12(5):360–9.
Enneking WF, Eady JL, Burchardt H. Autogenous cortical bone graft in the reconstruction of segmental defects. J Bone Joint Surg. 1980;62-A(7):1039–58.
Yajima H, Tamai S, Mizumoto S, Ono H. Vascularized fibular grafts for reconstruction of the femur. J Bone Joint Surg. 1993;75-B(1):123–8.
Usui M. Free vascularized fibular grafting for reconstruction after tumor resection. Rinshou Seikeigeka. 1998;33(3):267–76 (in Japanese).
Shimose S, Sugita T, Ishida O, Kubo T, Hirao K, Matsuo T, Tanaka K, Ochi M. Reconstruction using vascularized fibular grafts in malignant bone and soft tissue tumors. Kansetu Geka. 2005;24:846–50 (in Japanese).
Minami A, Kasashima T, Iwasaki N, Kato N, Kaneda K. Vascularized fibular grafts: an experience of 102 patients. J Bone Joint Surg. 2000;82-B(7):1022–5.
De Boer HH, Wood MB, Hermans J. Reconstruction of large skeletal defects by vascularized fibula transfer: factors that influenced the outcome of union in 62 cases. Int Orthop. 1990;14:121–8.
Hsu RWW, Wood MB, Sim FH, Chao EYS. Free vascularized fibular grafting for reconstruction after resection. J Bone Joint Surg. 1997;79-B(1):36–42.
Jones NF, Swartz WM, Mears DC, Jupiter JB, Grossman A. The ‘double barrel’ free vascularized fibular bone graft. Plast Reconstr Surg. 1988;81:379–85.
Hou SM, Liu TK. Reconstruction of skeletal defects in the femur with ‘two strut’ free vascularized fibular grafts. J Trauma. 1992;33:840–5.
Okubo K, Murota K, Tomita Y, Beppu M, Takahashi F, Moriyama M, Watanabe K. Dual free vascularized fibular grafts for treatment of large bone defects of tumors. Seikeigeka. 1985;36:917–26 (in Japanese).
Jupiter JB, Bour CJ, May JWJ. The reconstruction of defects in the femoral shaft with vascularized transfers of fibular bone. J Bone Joint Surg. 1987;69-A(3):365–74.
Toh S, Harata S, Ohmi Y, Nakahara K, Satoh F, Tsubo K, Nakamura R, Nishikawa S. Dual vascularized fibula transfer on a single vascular pedicle: a useful technique in long bone reconstruction. J Reconstr Microsurg. 1988;4:217–21.
Conflict of interest
The authors did not receive and will not receive any benefits or funding from any commercial party or parties related directly or indirectly to the subject of this article.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Tanaka, K., Maehara, H. & Kanaya, F. Vascularized fibular graft for bone defects after wide resection of musculoskeletal tumors. J Orthop Sci 17, 156–162 (2012). https://doi.org/10.1007/s00776-011-0194-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00776-011-0194-4