Abstract
Introduction
This study established normative references for total body less head (TBLH) BMD, lumbar spine (L1–L4) BMD, and both total and appendicular lean mass (LM) in Thai children and adolescents (aged 5–18 years) using DXA. This work expands upon 2014 normative data for Thai children, which included L2–L4 BMD, total body BMD (head included), and total LM.
Materials and methods
We reanalyzed total body and lumbar spine DXA scans (Lunar Prodigy Pro, GE Healthcare; enCORE version 7.53) from 174 boys and 193 girls, using upgraded software (enCORE version 17SP2) for TBLH BMD, L1–L4 BMD, and LM analysis. The “enhanced” mode was applied for TBLH BMD and LM. Adjustments for total and appendicular LM were made relative to squared height (m2) to account for body size variability.
Results
Normative data stratified by sex and Tanner stage were generated for TBLH BMD, L1–L4 BMD, and LM indices. Weight and Tanner stage significantly determined BMD and LM. Adolescent girls exhibited higher LSBMD values due to earlier pubertal onset. Boys showed higher LM indices with more rapid gains during growth spurts.
Conclusion
This study provides updated normative reference values for BMD (TBLH and L1–L4) and LM (total and appendicular) in Thai children and adolescents, measured via DXA. These references will enhance the assessment of low bone mass and LM deficits in Thai pediatric populations, particularly in those with chronic illnesses.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Childhood osteoporosis, arising from congenital or acquired conditions, heightens fracture risk throughout life [1]. Optimal bone mineral accretion during childhood and adolescence is crucial, as peak bone mass is a primary determinant of future osteoporosis risk [2]. Therefore, assessing bone health is essential for early detection and intervention in children with low bone mineral density (BMD), especially those with chronic conditions known to negatively impact bone health.
Dual-energy X-ray absorptiometry (DXA) is the preferred technique for evaluating pediatric bone mass due to its accessibility, speed, and minimal radiation exposure [3]. Beyond its established role in assessing BMD, DXA is also a valid and reliable tool for pediatric body composition analysis [3], accurately measuring bone mineral content, lean mass (LM), and fat mass. The latest densitometers allow for comprehensive assessment via a single whole-body scan.
DXA’s utility in evaluating low LM in children has gained prominence [4]. While excess fat in children remains a public health concern, low LM also poses significant health risks. Children with low LM are at greater risk of metabolic syndrome [5, 6] Additionally, low LM, indicative of protein-energy wasting, has been documented in childhood cancer survivors [7] and in children with chronic inflammatory diseases [8], chronic kidney disease [9], and cerebral palsy [10]. Sarcopenia (low LM and poor muscle strength) in children with chronic diseases is associated with adverse clinical outcomes [11].
Despite DXA’s status as a reference technique for BMD and body composition assessment, its interpretation is hindered by the lack of universal reference values. Accurate analysis requires reference data specific to the population, considering factors such as race, sex, and age.
In 2014, our group published normative references for Thai children and adolescents, including total body BMD with the head region (TBBMD), L2–L4 BMD, and total LM [12]. This was extended in 2022 to include proximal femur BMD [13]. However, the International Society for Clinical Densitometry (ISCD) currently recommends total body less head (TBLH) and L1–L4 as the preferred skeletal sites for pediatric areal BMD assessment in most pediatric subjects [3, 14].
TBLH BMD is preferred over TBBMD because the skull constitutes a large, disproportionate skeletal component that is minimally influenced by activity or environmental factors [15]. Our initial 2014 reference did not include TBLH BMD due to limitations in the software used at that time (enCORE version 7.53, GE Healthcare, Madison, WI, USA).
A 2018 upgrade to our DXA system (Prodigy software, enCORE version 17SP2) enabled TBLH analysis and “enhanced” total body (TB) analysis, which offers improved skeletal edge detection and better local estimation of tissue composition over bones. This enhanced analysis, available since enCORE version 14.10, leverages algorithmic improvements from the higher resolution iDXA system. These improvements enhance the detection of low-density bone and reduce the impact of soft tissue thickness on BMD, making the analysis particularly beneficial for younger and smaller subjects [16, 17]. Consequently, we established a new reference for TBBMD as TBLH BMD using this enhanced mode.
Additionally, this study introduces more detailed normative references for LM parameters, including total LM, appendicular LM (ALM), total LM index (total LMI), and ALM index (ALMI), all analyzed with enhanced TB analysis. Lean mass primarily consists of skeletal muscle, excluding fat and bone mass, with total LM including organ tissue, while ALM is largely muscle tissue. ALM is increasingly recognized as a measure of skeletal muscle deficit in children [18]. Adjustments for body size (total LMI and ALMI) may better represent LM status in growing children.
Regarding lumbar spine BMD (LSBMD) assessment, L1 misidentification occurs in up to 13% of adult DXA scans. Analyzing L2–L4 minimizes this impact [19], making L2–L4 BMD common in pediatric clinical and research settings [20,21,22]. However, the 2013 ISCD Pediatric Official Position recommends L1–L4 BMD [3]. Therefore, we established a new LSBMD reference as L1–L4 BMD to complement our earlier L2–L4 BMD reference [12].
To generate these references, we reanalyzed existing lumbar spine and TB scans (obtained 2008–2011) using upgraded software to derive TBLH BMD, L1–L4 BMD, total LM, and ALM.
This study aimed to establish age- and sex-specific reference values for TBLH BMD, L1–L4 BMD, total LM, total LMI, ALM, and ALMI as measured by DXA in Thai children and adolescents (aged 5–18 years).
Materials and methods
Subjects
A total of 381 healthy Thai children and adolescents (aged 5.5–18.8 years) were initially recruited from Bangkok schools between 2008 and 2011. Children exceeding the 97th percentile or falling below the third percentile on standard Thai growth curves were excluded [23]. Additional exclusion criteria were as follows:
-
Use of medications affecting bone health (eg, glucocorticoids, anticonvulsants, vitamin D, and calcium).
-
Presence of chronic illnesses known to impact bone health.
-
A fracture history exceeding age-based thresholds (≥ 2 if ≤ 10 years; ≥ 3 if > 10 years).
After applying these criteria, 367 subjects remained (174 boys, 193 girls).
Anthropometric measurement and pubertal assessment
Each subject’s weight and height were measured using a standard weight scale (Tanita Corp, Arlington Heights, IL, USA) and a Harpenden Stadiometer (Holtain Limited, Crymych, UK). Height and weight Z-scores were derived using Thai national standards [24], and body mass index (BMI) was calculated. A single physician (P.N.) assessed pubertal status using the Tanner classification.
Measurement of TBBMD, LSBMD, and LM by DXA
Lumbar spine and TB scans were acquired from 174 boys and 193 girls between 2008 and 2011 using a DXA scanner (Lunar Prodigy Pro, GE Healthcare, Madison, WI, USA) and analyzed with enCORE software (version 7.53). All measurements were performed by a trained technician (P.W.) following daily quality assurance protocols.
Prior to scanning, subjects were given instructions to minimize the potential effects of time of day, diet, bladder status, and clothing on LM values. All DXA scans were conducted in the morning between 8:00 and 9:00 AM. Subjects were asked to refrain from eating breakfast before the scan, although young children were allowed light snacks to ensure comfort and cooperation. Subjects wore light hospital gowns and were instructed to empty their bladders before scanning, although it was understood that very young children might not always be able to do so. Any external metal objects were removed to minimize artifacts.
During whole-body scans, subjects were positioned according to ISCD recommendations: lying face-up with a neutral chin, with palms facing down, arms straight and slightly away from the body, feet in a neutral position, and ankles strapped [25, 26]. For LSBMD measurements, subjects were placed in a supine position with their lumbar lordosis flattened using a foam leg block [16].
Duplicate measurements from 30 randomly selected study participants were used to determine precision errors and least significant changes. Each of these 30 participants or their parents/guardians provided consent for these measurements. The precision errors calculated from the duplicate measurements ensured consistency in the proper positioning of pediatric subjects and the accurate analysis of pediatric scans. The errors were as follows: 0.61% for LSBMD, 0.7% for TBBMD, and 1.05% for total LM. The least significant changes at the 95% confidence interval were 1.7% for LSBMD, 1.9% for TBBMD, and 2.9% for total LM.
The minimum acceptable precision errors for a technician measuring BMD and body composition were previously established as 1.9% for LSBMD, 1% for TBBMD, and 2% for total LM. The acceptable least significant change thresholds were also previously determined to be 5.3% for LSBMD, 2.8% for TBBMD, and 5.5% for total LM [16, 26].
Reanalysis of TB and lumbar spine scans
A trained technician (T.M.) reanalyzed existing DXA scans (Lunar Prodigy Pro, enCORE version 7.53) using upgraded software (enCORE version 17SP2) as previously described [17]. The upgraded enCORE software not only enhances functionality and precision but also maintains the same algorithms and compatibility across different generations of Lunar DXA systems. Consequently, reanalyzing previously scanned images with the newer software has minimal to no impact on BMD values, provided the same analysis mode is applied [17].
Specific measurements included areal BMD for the lumbar spine (L1–L4) and TBLH. Additionally, total LM (which includes LM across the entire body) and ALM (the sum of LM specifically in the arms and legs) were assessed. Total LM and ALM (in kg) were adjusted for squared height (meters2), resulting in total LMI and ALMI, respectively, to account for differences in body size.
Each TB image reanalysis employed the enhanced mode, which improves soft tissue and bone differentiation algorithms compared to basic-mode analysis [16, 17]. The software automatically placed the region of interest for each image, which was then reviewed to ensure correct positioning for both lumbar spine and TB scans, in accordance with manufacturer guidelines [16]. If necessary, adjustments were made to isolate arm regions from the hips and thighs during body composition analysis. For the lumbar spine (L1–L4), correct placement of the analysis box and intervertebral line positioning were verified.
Lumbar spine bone mineral apparent density
DXA-derived BMD is calculated as bone mineral content per bone area. However, because DXA cannot measure bone depth, BMD values are influenced by bone size. To address this, we calculated the bone mineral apparent density of the lumbar spine (LSBMAD) using the following formula:
where “width” represents the mean width across the first to fourth lumbar vertebral bodies, which are assumed to be cylindrical [27].
Ethics and consent
This study was approved by the Ethics Committee of the Faculty of Medicine Siriraj Hospital, Mahidol University (reference numbers: 183/2007 and 060/2022). The study adhered to the Declaration of Helsinki and Good Clinical Practice Guidelines. Written informed consent was obtained from subjects aged 18 years or older. For subjects younger than 18, both parental/guardian consent and subject assent were obtained. The informed consent process included information on the low DXA radiation exposure, which is less than daily natural background radiation.
Statistical analysis
The sample size was calculated using the formula: n = (Z2δ2)/d2, where Z = 1.96, δ is the estimated standard deviation, and d is the distance from the mean to the limit. A two-sided 95% confidence interval was used to estimate the mean BMD values. The standard deviation and the distance from the mean to the limit were derived from a previously published normal BMD reference [28]. The calculation resulted in a minimum required sample size of 355 participants.
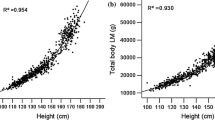
Regression analysis was performed to identify the best-fitting models for the relationships between age and the following parameters: TBLH BMD, LSBMD, LSBMAD, total LM, total LMI, ALM, and ALMI. Coefficients of determination (R2) were calculated. A quadratic model, incorporating age and age2, provided the best fit for both boys and girls.
The means and standard deviations (SDs) for TBLH BMD, LSBMD, LSBMAD, total LM, total LMI, ALM, and ALMI were computed separately for boys and girls across each age group and Tanner stage. Unpaired t tests were used to assess differences between boys and girls within corresponding age groups and Tanner stages.
One-way analysis of variance (ANOVA) with Bonferroni correction was used to compare TBLH BMD, LSBMD, LSBMAD, total LM, total LMI, ALM, and ALMI across age groups and Tanner stages within each sex. Significant differences were identified through post hoc testing.
Multiple linear regression was conducted to evaluate the relationships between age, Tanner stage, weight, height, and the following parameters: TBLH BMD, LSBMD, LSBMAD, total LM, total LMI, ALM, and ALMI. Variance inflation factors (VIF) were calculated to assess multicollinearity among the independent variables. Independent variables with VIF values exceeding 10 were removed from the model if deemed necessary, based on the specific context and potential impact on the analysis.
Data analysis was performed using IBM SPSS Statistics, version 29 (IBM Corp, Armonk, NY, USA). A P value < 0.05 was considered statistically significant.
Results
Anthropometric data
DXA scans were analyzed for 367 subjects (174 boys and 193 girls) aged 5–18 years. The anthropometric data (height, height Z-score, weight, weight Z-score, and BMI) are presented in Table 1. The mean height Z-scores were 0.2 ± 0.9 for boys and 0.2 ± 1.0 for girls. The mean weight Z-scores were 0.2 ± 0.8 for both sexes. The mean BMIs were 17.8 ± 2.6 kg/m2 for boys and 17.8 ± 2.8 kg/m2 for girls.
TBLH BMD, LSBMD, and LSBMAD by age group
Table 2 provides the means (SDs) for age- and sex-specific TBLH BMD, LSBMD, and LSBMAD.
All parameters (TBLH BMD, LSBMD, and LSBMAD) increased with age in both sexes (Fig. 1A, B, and C). Boys reached peak annual increases in TBLH BMD and LSBMD at age 16, with continued increases until age 18. Girls showed peak annual increases in TBLH BMD and LSBMD at ages 10 and 12, respectively, with values plateauing around age 16 (Fig. 1A and B).
Relationships in boys and girls between A age and bone mineral density of the total body less head (TBLH BMD; g/cm2), B age and BMD of the lumbar spine (LSBMD; g/cm2), C age and bone mineral apparent density of the lumbar spine (LSBMAD; g/cm3), and D age and BMD of each individual lumbar spine (L1, L2, L3 and L4; g/cm2). The lines show the best-fitting function with the factors age and age2 (quadratic function) for boys and girls
TBLH BMD was greater in boys than girls in the 5–9 and 16–19 age groups, with statistical significance (P < 0.005) observed only in the 16–19 age group. In contrast, girls had higher LSBMD values than boys between ages 9 and 17, with significant differences at ages 10 and 12 (each P < 0.05) and 13–15 (P < 0.01). Although boys exhibited greater LSBMD in the 18–19 age group, this difference was not statistically significant (Fig. 1A and B).
The LSBMAD showed the greatest annual increase at age 18 in boys and at age 12 in girls, continuing to increase in both sexes thereafter. After age 8, girls demonstrated significantly greater LSBMAD than boys (P < 0.05) (Fig. 1C).
Among the lumbar vertebrae (L1 to L4), BMD was observed in descending order from L3, L4, L2, to L1. Notably, L3 had the highest BMD in 64% of subjects, while L1 had the lowest BMD in 69.5% of subjects. BMD at L1 was significantly lower than at L2 (P < 0.05), L3, and L4 (P < 0.01). Additionally, L2 BMD was significantly lower than L3 BMD (P = 0.049), but no significant difference was observed between L3 and L4 BMD (Fig. 1D). The L1-L4 BMD reference values presented in this study are significantly lower than the L2–L4 BMD values previously reported by our group [12] across nearly all age groups (P < 0.05; data not shown). However, the variance was minimal (1.6% ± 1.3%).
TBLH BMD, LSBMD, and LSBMAD for each Tanner stage
Table 3 presents the Tanner stage- and sex-specific means (SDs) for TBLH BMD, LSBMD, and LSBMAD.
TBLH BMD, LSBMD, and LSBMAD increased with pubertal progression in both sexes (Fig. 2A–C). Significant increases in BMD and LSBMAD were observed between adjacent Tanner stages during late puberty in both sexes (TBLH BMD: Tanner IV vs V; LSBMD and LSBMAD: Tanner III vs IV and Tanner IV vs V [all P < 0.001]). Notably, only TBLH BMD showed a significant increase from Tanner I to Tanner II in both sexes (P < 0.001).
At different Tanner stages in boys and girls, A bone mineral density of the total body less head (TBLH BMD; g/cm2), B BMD of the lumbar spine (LSBMD; g/cm2), and C bone mineral apparent density of the lumbar spine (LSBMAD; g/cm3). P values between Tanner stages of the same sex are shown only for consecutive Tanner stages
At each Tanner stage, boys exhibited significantly higher TBLH BMD than girls (P < 0.05; Fig. 2A) but significantly lower LSBMAD at Tanner stages I, IV, and V (P < 0.01; Fig. 2C). No significant differences in LSBMD were observed between boys and girls (Fig. 2B).
Relationships between BMD and LSBMAD vs age, Tanner stage, weight, and height
Supplementary Table 1 presents the multiple linear regression analysis assessing the relationships between age, Tanner stage, weight, and height versus both BMD and LSBMAD. For boys, height was excluded from the regression model due to a high variance inflation factor (> 10).
In boys, age and weight were significant determinants of TBLH BMD (R2 = 90.0%) and LSBMD (R2 = 78.1%). Tanner stage was significantly associated only with LSBMD (R2 = 78.1%). Weight alone served as a weak determinant of LSBMAD (R2 = 31.3%).
For girls, age, Tanner stage, and weight were significant determinants of TBLH BMD (R2 = 89.6%), LSBMD (R2 = 82.9%), and LSBMAD (R2 = 55.4%). Height significantly influenced LSBMD and LSBMAD, but not TBLH BMD.
Total LM, total LMI, ALM, and ALMI for each age group
Table 2 presents age- and sex-specific means (SDs) for total LM, total LMI, ALM, and ALMI.
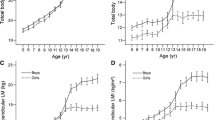
All LM parameters increased with age in both sexes. In boys, total LM and ALM showed rapid increases starting at age 8, peaking near the end of the studied age range (just before 19 years). In girls, total LM and ALM increased gradually from age 5 and plateaued at age 16 (Fig. 3A and C). Height-adjusted measures (total LMI and ALMI) mirrored the age-related patterns of total LM and ALM in both sexes, though the magnitude of increases across age groups was attenuated (Fig. 3B and D).
Relationships in boys and girls between A age and total lean mass (total LM; kg), B age and total lean mass index (total LMI; kg/m2), C age and appendicular lean mass (ALM; kg), and D age and appendicular lean mass index (ALMI; kg/m2). The lines show the best-fitting function with the factors age and age2 (quadratic function) for boys and girls
Boys exhibited steeper increases and higher values across all LM indices than girls. Significant sex differences in total LM, total LMI, ALM, and ALMI emerged from age 12 onward (P < 0.05; Fig. 3A–D).
Our new LM reference values obtained via the enhanced mode were lower (6.5% ± 4.1%) than the previously published total LM values derived with the basic mode [12].
Total LM, total LMI, ALM, and ALMI for each Tanner stage
Table 3 provides the Tanner stage- and sex-specific means (SDs) for total LM, total LMI, ALM, and ALMI.
Both total LM and ALM increased with pubertal progression in both sexes (Supplementary Fig. A and C). However, when adjusted for height (as total LMI and ALMI), the magnitude of these increases across pubertal stages was attenuated (Supplementary Fig. B and D).
Significant increases in total LM and ALM were observed between several adjacent Tanner stages in both sexes (Supplementary Fig. A and C). In contrast, increases between adjacent Tanner stages were less common for total LMI and ALMI (Supplementary Fig. B and D).
Across all Tanner stages, boys exhibited significantly greater values for all LM indices than girls (P < 0.01).
Relationships between total LM, total LMI, ALM, and ALMI vs age, Tanner stage, weight, and height
Multiple linear regression analysis was used to assess the relationships between total LM, total LMI, ALM, and ALMI with age, Tanner stage, weight, and height (Supplementary Table 2). For boys, height was excluded from the regression model due to a high variance inflation factor (> 10).
In boys, age, Tanner stage, and weight were significant determinants of total LM (R2 = 96.6%), total LMI (R2 = 81.3%), and ALM (R2 = 96.1%). Weight was the sole significant determinant of ALMI (R2 = 87.8%).
In girls, weight and height were significant determinants of all LM indices: total LM (R2 = 96.8%), total LMI (R2 = 78.9%), ALM (R2 = 96.0%), and ALMI (R2 = 81.8%). Tanner stage significantly influenced only total LM (R2 = 96.8%). Despite the progressive increase in LM indices from childhood through adolescence, age did not independently determine LM indices in girls.
Discussion
Population- and ethnicity-specific normative references are crucial for accurate BMD and body composition assessments. This study established normative references for lumbar spine (L1-L4) and TBLH BMD, along with total LM and ALM, in Thai children and adolescents (aged 5–18 years) using DXA (Lunar Prodigy Pro; GE Healthcare). This work expands upon the normative data for Thai children reported in 2014, which included L2-L4 BMD and TBBMD.
The ISCD Pediatric Official Position designates L1–L4 as the preferred site for LSBMD assessment [3]. Published normative LSBMD references across pediatric populations typically include either L1–L4 or L2–L4 BMD values. Our study revealed that L1–L4 BMD values are significantly lower than the previously reported L2–L4 BMD values. However, the difference is minimal and may not significantly impact clinical practice. Both L1–L4 and L2–L4 BMD can be used to assess LSBMD, with L2–L4 recommended when L1 morphology is abnormal or a metallic implant is present in L1.
To our knowledge, the pattern of LSBMD distribution across the L1–L4 vertebrae in children has not been previously reported. Ryan et al. demonstrated a stepwise increase in L1–L4 BMD, with L1 exhibiting the lowest BMD in adults [29]. Our findings indicate that the distribution of LSBMD across L1 to L4 in children does not follow a strict stepwise pattern, aligning more closely with the data from Peel et al. in adults, where L3 exhibited the highest BMD values [19].
The ISCD Pediatric Official Positions recommend TBLH as the preferred skeletal site for TBBMD assessment in children [14]. TBLH BMD is favored because it avoids the potential distortion caused by the relatively large size of the skull, which is less responsive to activity and environmental factors [15]. In this study, we re-established the TBBMD reference as TBLH BMD using the enhanced mode. The newer generation of enCORE software (GE Healthcare) for enhanced TB analysis provides improved soft tissue composition modeling and point typing, resulting in superior image resolution compared to that obtainable with the basic analysis mode [16, 17].
Moreover, this study established updated total LM reference values and additional LM parameters, including ALM, total LMI, and ALMI, for Thai children and adolescents. The new total LM reference values are 6.5% ± 4.1% lower than our previously published values derived from basic mode analysis [12]. This reduction in total LM values reflects the general trend observed when switching from basic to enhanced TB analysis [17]. Our findings underscore the importance of considering the analysis mode when interpreting TBBMD or LM using enCORE 14.10 or later software (GE Healthcare). Consistency between the analysis mode of the TB measurement and that of the normative reference data is crucial.
There is a high and inverse association between LM and the prevalence of adverse risk factors for cardiovascular disease and diabetes mellitus in children [6]. Furthermore, low LM has been linked to the severity of various pediatric chronic illnesses [7,8,9,10]. The use of ALM rather than total LM has been suggested as a more accurate method for quantifying skeletal muscle. In children with cerebral palsy, low skeletal muscle mass was significantly underestimated when assessed by total LMI (16.2%) compared to ALMI (42.2%) [30].
Differences in body size among children should be considered when interpreting BMD or LM parameters. In children with short stature or growth delay, the ISCD recommends adjusting spine and TBLH areal BMD values for height Z-score [14]. For total LM and ALM, a more appropriate approach is to correct these values for height, resulting in total LMI and ALMI, respectively.
The criterion for diagnosing low bone mass in children is well established as a BMD Z-score of less than or equal to -2 standard deviations below the population mean [14]. However, a specific criterion for diagnosing low LM in children is currently lacking. In adults, sarcopenia (low muscle mass and strength) is defined as an ALMI two standard deviations below the mean [31]. Nevertheless, assessments of total LM, total LMI, ALM, and ALMI may prove valuable in monitoring LM deficits associated with disease progression and treatment response in chronic pediatric illnesses.
The positive correlations between weight, BMD, and all LM indices in both sexes suggest that increased mechanical loading on bones and muscles due to greater weight promotes BMD [32] and LM development [33]. Notably, adolescent girls tend to have higher LSBMD values than boys of the same age, which is related to girls entering puberty earlier. Additionally, there are positive correlations between Tanner stage, BMD, and LM indices from pre-puberty (Tanner I) through all stages of puberty, with rapid gains in BMD and LM indices occurring specifically during the pubertal growth spurt. These factors collectively highlight the significant influence of sex steroids on BMD and LM acquisition [34]. In addition to weight and puberty, age independently affects most BMD and LM indices. However, LM indices in girls are more dependent on growth and puberty than on age.
A progressive increase in the estimated volumetric BMD of the lumbar spine (LSBMAD) indicates an actual rise in lumbar spine mineralization rather than an increase in bone size during growth. In contrast to areal BMD findings, LSBMAD, which represents actual mineralization, was not considerably influenced by age, puberty, or growth. The increase in LSBMD associated with age and pubertal progression is likely due to increased bone size. These findings underscore the utility of bone mineral apparent density as a method to correct for bone size [27].
A recognized limitation of DXA is the variability in results among densitometers from different manufacturers. Significant differences in BMD and body composition values exist between systems from GE Healthcare Lunar (Madison, WI, USA) and Hologic (Bedford, MA, USA), precluding direct comparisons with Hologic-derived reference data [35, 36]. However, reference data obtained from pencil-beam GE Lunar DPXL densitometers remain applicable for fan-beam GE Lunar Prodigy systems, as no significant differences in TBBMD and LSBMD values have been observed between these platforms [37]. Accordingly, we compared our new BMD and LM reference values with published normative data from DXA devices from the same manufacturer using the enhanced TB analysis mode.
Compared to children in the UK [38] and Mexico [39], Thai children exhibit lower TBLH and LSBMD. They also have lower total LM than Austrian children [40]. Within Asia, Thai children exhibit greater LSBMD (6.8% ± 3.1%) than Indian children [41]. These disparities underscore the importance of population-specific normative data, even when comparing Asian children from different subcontinents.
Our observations regarding the dynamic changes in BMD and LM across age and pubertal progression align with published references [38,39,40,41,42,43,44]. These changes include age- and puberty-dependent increases in BMD and LM, rapid gains during growth spurts, and positive correlations between BMD, weight, and LM. Additionally, we confirmed earlier maximal BMD increases with total LM plateaus in girls and higher LM indices with more rapid gains during growth spurts in boys.
The timing of peak BMD and LM gains and the onset of their respective plateaus varies significantly across different populations. For instance, Korean [42] and Indian [41] children experience rapid BMD gains earlier than their Thai counterparts, while Thai children exhibit their most notable BMD gains earlier than Dutch children [43]. Moreover, peak total LM and ALM in our study were attained later than those observed in Chinese children [44]. These findings underscore the influence of genetic factors, nutritional status, and pubertal timing on BMD and LM across various demographic groups.
Our study has several limitations that warrant acknowledgment. First, the sample included only six boys in the 10-year-old category. Despite this small sample size, the standard deviations for bone and LM parameters in this cohort were moderate and consistent with those in other age cohorts, suggesting that the reference data for boys in this age group are reliable. Second, the BMD and LM measurements were derived from schoolchildren in Bangkok, limiting geographic diversity. However, improvements in living standards and healthcare accessibility in Thailand over the past two decades have likely reduced the disparity in baseline nutritional status and physical growth between urban and rural Thai children. Thus, our normative references are expected to be broadly applicable in clinical practice throughout Thailand.
It is important to note that the BMD and LM reference data in our study were collected from children approximately a decade ago. To our knowledge, secular trends in BMD and LM among children have not yet been documented. Nonetheless, there has been a noteworthy trend toward increased overall growth and a reduction in the age at the onset of puberty among Thai children over the past four decades [45]. These changes in growth and puberty patterns may have an unknown impact on BMD and LM measurements.
Conclusion
Using DXA, this study established reference values for both TBLH BMD and L1-L4 BMD and determined detailed LM parameters, including total and appendicular LMIs, in Thai children and adolescents (aged 5–18 years). Given the shared geographical, genetic, healthcare, and nutritional contexts among Thai and broader Southeast Asian populations, our BMD references have the potential to be instrumental in assessing low bone mass and bone fragility risks in Southeast Asian children. Additionally, the comprehensive LM references provided may facilitate the efficient monitoring and evaluation of intervention strategies in Southeast Asian children with chronic conditions affecting LM.
Abbreviations
- ALM:
-
Appendicular lean mass
- ALMI:
-
Appendicular lean mass index
- ANOVA:
-
Analysis of variance
- BMD:
-
Bone mineral density
- BMI:
-
Body mass index
- DXA:
-
Dual-energy X-ray absorptiometry
- ISCD:
-
The International Society for Clinical Densitometry
- LM:
-
Lean mass
- LMI:
-
Lean mass index
- LSBMAD:
-
Bone mineral apparent density of the lumbar spine
- LSBMD:
-
Bone mineral density of the lumbar spine
- SD:
-
Standard deviation
- TB:
-
Total body
- TBBMD:
-
Bone mineral density of the total body (including the head)
- TBLH:
-
Total body less head
- TBLH BMD:
-
Bone mineral density of the total body less head
- VIF:
-
Variance inflation factor
References
Boyce AM, Gafni RI (2011) Approach to the child with fractures. J Clin Endocrinol Metab 96:1943–1952. https://doi.org/10.1210/jc.2010-2546
Ott SM (1990) Attainment of peak bone mass. J Clin Endocrinol Metab 71:1082A-A1182. https://doi.org/10.1210/jcem-71-5-1082
Crabtree NJ, Arabi A, Bachrach LK, Fewtrell M, El-Hajj Fuleihan G, Kecskemethy HH, Jaworski M, Gordon CM, International Society for Clinical D (2014) Dual-energy X-ray absorptiometry interpretation and reporting in children and adolescents: the revised 2013 ISCD Pediatric Official Positions. J Clin Densitom 17:225–242. https://doi.org/10.1016/j.jocd.2014.01.003
Guglielmi G, Ponti F, Agostini M, Amadori M, Battista G, Bazzocchi A (2016) The role of DXA in sarcopenia. Aging Clin Exp Res 28:1047–1060. https://doi.org/10.1007/s40520-016-0589-3
Burrows R, Correa-Burrows P, Reyes M, Blanco E, Albala C, Gahagan S (2016) High cardiometabolic risk in healthy Chilean adolescents: associations with anthropometric, biological and lifestyle factors. Public Health Nutr 19:486–493. https://doi.org/10.1017/S1368980015001585
Kim S, Valdez R (2015) Metabolic risk factors in U.S. youth with low relative muscle mass. Obes Res Clin Pract 9:125–132. https://doi.org/10.1016/j.orcp.2014.05.002
van Atteveld JE, de Winter DTC, Pluimakers VG, Fiocco M, Nievelstein RAJ et al (2023) Frailty and sarcopenia within the earliest national Dutch childhood cancer survivor cohort (DCCSS-LATER): a cross-sectional study. Lancet Healthy Longev 4:e155–e165. https://doi.org/10.1016/S2666-7568(23)00020-X
Houttu N, Kalliomaki M, Gronlund MM, Niinikoski H, Nermes M, Laitinen K (2020) Body composition in children with chronic inflammatory diseases: a systematic review. Clin Nutr 39:2647–2662. https://doi.org/10.1016/j.clnu.2019.12.027
Foster BJ, Kalkwarf HJ, Shults J, Zemel BS, Wetzsteon RJ, Thayu M, Foerster DL, Leonard MB (2011) Association of chronic kidney disease with muscle deficits in children. J Am Soc Nephrol 22:377–386. https://doi.org/10.1681/ASN.2010060603
Stallings VA, Cronk CE, Zemel BS, Charney EB (1995) Body composition in children with spastic quadriplegic cerebral palsy. J Pediatr 126:833–839. https://doi.org/10.1016/s0022-3476(95)70424-8
Mager DR, Hager A, Gilmour S (2023) Challenges and physiological implications of sarcopenia in children and youth in health and disease. Curr Opin Clin Nutr Metab Care 26:528–533. https://doi.org/10.1097/MCO.0000000000000969
Nakavachara P, Pooliam J, Weerakulwattana L, Kiattisakthavee P, Chaichanwattanakul K, Manorompatarasarn R, Chokephaibulkit K, Viprakasit V (2014) A normal reference of bone mineral density (BMD) measured by dual energy X-ray absorptiometry in healthy thai children and adolescents aged 5–18 years: a new reference for Southeast Asian Populations. PLoS One 9:e97218. https://doi.org/10.1371/journal.pone.0097218
Trakulpark C, Manpayak T, Weerakulwattana P, Pooliam J, Nakavachara P (2022) Reference values of bone mineral density of proximal femur for Southeast Asian children and adolescents. Arch Osteoporos 17:145. https://doi.org/10.1007/s11657-022-01184-9
Shuhart CR, Yeap SS, Anderson PA, Jankowski LG, Lewiecki EM, Morse LR, Rosen HN, Weber DR, Zemel BS, Shepherd JA (2019) Executive summary of the 2019 ISCD position development conference on monitoring treatment, DXA cross-calibration and least significant change, spinal cord injury, peri-prosthetic and orthopedic bone health, transgender medicine, and pediatrics. J Clin Densitom 22:453–471 https://doi.org/10.1016/j.jocd.2019.07.001
Taylor A, Konrad PT, Norman ME, Harcke HT (1997) Total body bone mineral density in young children: influence of head bone mineral density. J Bone Miner Res 12:652–655. https://doi.org/10.1359/jbmr.1997.12.4.652
GE-Healthcare (2017) X-ray bone densitometer with enCORE v17 Software – User Manual
Lundstam K, Godang K, Pretorius M, Markwardt P, Hellstrom M, Bollerslev J, Heck A (2021) The influence of Dxa Hardware, Software, reference population and Software analysis settings on the bone mineral density and T-score relationship. J Clin Densitom. https://doi.org/10.1016/j.jocd.2021.07.002
Summer SS, Wong BL, Rutter MM, Horn PS, Tian C, Rybalsky I, Shellenbarger KC, Kalkwarf HJ (2021) Age-related changes in appendicular lean mass in males with Duchenne muscular dystrophy: a retrospective review. Muscle Nerve 63:231–238. https://doi.org/10.1002/mus.27107
Peel NF, Johnson A, Barrington NA, Smith TW, Eastell R (1993) Impact of anomalous vertebral segmentation on measurements of bone mineral density. J Bone Miner Res 8:719–723. https://doi.org/10.1002/jbmr.5650080610
Boot AM, van den Heuvel-Eibrink MM, Hahlen K, Krenning EP, de Muinck Keizer-Schrama SM (1999) Bone mineral density in children with acute lymphoblastic leukaemia. Eur J Cancer 35:1693–1697. https://doi.org/10.1016/s0959-8049(99)00143-4
Boot AM, van der Sluis IM, Krenning EP, de Muinck Keizer-Schrama SM (2009) Bone mineral density and body composition in adolescents with childhood-onset growth hormone deficiency. Horm Res 71:364–371. https://doi.org/10.1159/000223422
Ma J, Siminoski K, Alos N, Halton J, Ho J et al (2015) The choice of normative pediatric reference database changes spine bone mineral density Z-scores but not the relationship between bone mineral density and prevalent vertebral fractures. J Clin Endocrinol Metab 100:1018–1027. https://doi.org/10.1210/jc.2014-3096
Department of Health MoPH, Thailand (2000) Reference for weight, height and nutritional indices in Thais aged 1 day to 19 years
Ekwattanakit S, Nakavachara P, Viprakasit V, Phil D (2018) Microsoft ® Office Excel-based Worksheet Program For Rapid Calculation Of Weight-For-AgE (WA) and height-for-age (HA) Z-scores in Thai pediatric population (THAI-Z). Southeast Asian J Tropic Med Public Health 48:183–191
GE-Healthcare (2003) enCORE Operator’s Manual Version 8
Shuhart C, Cheung A, Gill R, Gani L, Goel H, Szalat A (2024) Executive summary of the 2023 adult position development conference of the international society for clinical densitometry: DXA reporting, follow-up BMD testing and trabecular bone score application and reporting. J Clin Densitom 27:101435. https://doi.org/10.1016/j.jocd.2023.101435
Lu PW, Cowell CT, Lloyd-Jones SA, Briody JN, Howman-Giles RO (1996) Volumetric bone mineral density in normal subjects, aged 5–27 years. J Clin Endocrinol Metab 81:1586–1590. https://doi.org/10.1210/jcem.81.4.8636372
Liu J, Wang L, Sun J, Liu G, Yan W, Xi B, Xiong F, Ding W, Huang G, Heymsfield S, Mi J (2017) Bone mineral density reference standards for Chinese children aged 3–18: cross-sectional results of the 2013–2015 China Child and Adolescent Cardiovascular Health (CCACH) Study. BMJ Open 7:e014542. https://doi.org/10.1136/bmjopen-2016-014542
Ryan PJ, Blake GM, Herd R, Parker J, Fogelman I (1994) Distribution of bone mineral density in the lumbar spine in health and osteoporosis. Osteoporos Int 4:67–71. https://doi.org/10.1007/BF01623225
Duran I, Martakis K, Rehberg M, Stark C, Koy A, Schoenau E (2019) The appendicular lean mass index is a suitable surrogate for muscle mass in children with cerebral palsy. J Nutr 149:1863–1868. https://doi.org/10.1093/jn/nxz127
Baumgartner RN, Koehler KM, Gallagher D, Romero L, Heymsfield SB, Ross RR, Garry PJ, Lindeman RD (1998) Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol 147:755–763. https://doi.org/10.1093/oxfordjournals.aje.a009520
Iwaniec UT, Turner RT (2016) Influence of body weight on bone mass, architecture and turnover. J Endocrinol 230:R115–R130. https://doi.org/10.1530/JOE-16-0089
Slaughter MH, Lohman TG, Boileau RA (1978) Relationship of anthropometric dimensions to lean body mass in children. Ann Hum Biol 5:469–482. https://doi.org/10.1080/03014467800003121
Veldhuis JD, Roemmich JN, Richmond EJ, Rogol AD, Lovejoy JC, Sheffield-Moore M, Mauras N, Bowers CY (2005) Endocrine control of body composition in infancy, childhood, and puberty. Endocr Rev 26:114–146. https://doi.org/10.1210/er.2003-0038
Shepherd JA, Fan B, Lu Y, Wu XP, Wacker WK, Ergun DL, Levine MA (2012) A multinational study to develop universal standardization of whole-body bone density and composition using GE Healthcare Lunar and Hologic DXA systems. J Bone Miner Res 27:2208–2216. https://doi.org/10.1002/jbmr.1654
Genton L, Karsegard VL, Zawadynski S, Kyle UG, Pichard C, Golay A, Hans DB (2006) Comparison of body weight and composition measured by two different dual energy X-ray absorptiometry devices and three acquisition modes in obese women. Clin Nutr 25:428–437. https://doi.org/10.1016/j.clnu.2005.11.002
Oldroyd B, Smith AH, Truscott JG (2003) Cross-calibration of GE/Lunar pencil and fan-beam dual energy densitometers–bone mineral density and body composition studies. Eur J Clin Nutr 57:977–987. https://doi.org/10.1038/sj.ejcn.1601633
Crabtree NJ, Shaw NJ, Bishop NJ, Adams JE, Mughal MZ, Arundel P, Fewtrell MS, Ahmed SF, Treadgold LA, Hogler W, Bebbington NA, Ward KA, Team AS (2017) Amalgamated reference data for size-adjusted bone densitometry measurements in 3598 children and young adults-the ALPHABET study. J Bone Miner Res 32:172–180. https://doi.org/10.1002/jbmr.2935
Lopez-Gonzalez D, Wells JC, Cortina-Borja M, Fewtrell M, Partida-Gaytán A, Clark P (2021) Reference values for bone mineral density in healthy Mexican children and adolescents (in eng). Bone 142:115734. https://doi.org/10.1016/j.bone.2020.115734
Ofenheimer A, Breyer-Kohansal R, Hartl S, Burghuber OC, Krach F, Schrott A, Franssen FME, Wouters EFM, Breyer MK (2021) Reference charts for body composition parameters by dual-energy X-ray absorptiometry in European children and adolescents aged 6 to 18 years-Results from the Austrian LEAD (Lung, hEart, sociAl, boDy) cohort. Pediatr Obes 16:e12695. https://doi.org/10.1111/ijpo.12695
Khadilkar AV, Sanwalka NJ, Chiplonkar SA, Khadilkar VV, Mughal MZ (2011) Normative data and percentile curves for dual energy X-ray absorptiometry in healthy Indian girls and boys aged 5–17 years. Bone 48:810–819. https://doi.org/10.1016/j.bone.2010.12.013
Lim JS, Hwang JS, Lee JA, Kim DH, Park KD, Cheon GJ, Shin CH, Yang SW (2010) Bone mineral density according to age, bone age, and pubertal stages in Korean children and adolescents. J Clin Densitom 13:68–76. https://doi.org/10.1016/j.jocd.2009.09.006
van der Sluis IM, de Ridder MA, Boot AM, Krenning EP, de Muinck Keizer-Schrama SM (2002) Reference data for bone density and body composition measured with dual energy x ray absorptiometry in white children and young adults. Arch Dis Child 87:341–347; discussion 41–47 https://doi.org/10.1136/adc.87.4.341
Guo B, Wu Q, Gong J, Xiao Z, Tang Y, Shang J, Cheng Y, Xu H (2016) Relationships between the lean mass index and bone mass and reference values of muscular status in healthy Chinese children and adolescents. J Bone Miner Metab 34:703–713. https://doi.org/10.1007/s00774-015-0725-8
Jaruratanasirikul S, Sriplung H (2015) Secular trends of growth and pubertal maturation of school children in Southern Thailand. Ann Hum Biol 42:447–454. https://doi.org/10.3109/03014460.2014.955057
Acknowledgements
We sincerely thank Paul Markwardt, Senior Engineering Manager at GE Healthcare, Madison, WI, USA, for his technical guidance in the reanalysis of the scans. We also thank Praewvarin Weerakulwattana for conducting the initial BMD and lean mass assessments using DXA. Additionally, we appreciate David Park’s contribution to the English language editing of this manuscript.
Funding
Financial support for this research was provided by a Routine-to-Research grant (R2R086/08) conferred on PN by the Faculty of Medicine Siriraj Hospital, Mahidol University.
Author information
Authors and Affiliations
Contributions
PN conceptualized the study design and sought expertise from GE professionals. TM was responsible for the reanalysis of all DXA scans. KP and JP carried out the statistical evaluations. KP was instrumental in the data collection and initial drafting of the manuscript. PN undertook the data analysis and was pivotal in writing and finalizing the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Kaewpanpat Prajantawanich, Teerarat Manpayak, Julaporn Pooliam, and Pairunyar Nakavachara declare that there is no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
774_2024_1550_MOESM3_ESM.jpg
Supplementary file3 (JPG 108 KB) At different Tanner stages in boys and girls, (A) total lean mass (total LM; kg), (B) total lean mass index (total LMI; kg/cm2), (C) appendicular lean mass (ALM; kg), and (D) appendicular lean mass index (ALMI; kg/cm2). P values between Tanner stages of the same sex are shown only for consecutive Tanner stages.
About this article
Cite this article
Prajantawanich, K., Manpayak, T., Pooliam, J. et al. Updated reference values for BMD and lean mass measured by DXA in Thai children. J Bone Miner Metab (2024). https://doi.org/10.1007/s00774-024-01550-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00774-024-01550-2