Abstract
Introduction
Studies have shown that an impaired bone condition, represented by osteoporosis and increased fracture risk, may potentially aggravate periodontal disease and, consequently, the risk of tooth loss. This 5-year prospective study aimed to investigate whether systemic bone condition represents risk factor for tooth loss due to periodontal disease amongst elderly women.
Material and methods
Seventy-four participants, aged ≥ 65 years, who attended the 5-years recall for periodontal evaluation were involved. Baseline exposures were osteoporosis and fracture risk probabilities (FRAX). Women were grouped according to bone mineral density (BMD) and years of bone treatment for osteoporosis. The primary outcome at a 5-year follow-up was the number of tooth loss due to periodontal disease. Periodontitis staging and grading, and causes of tooth loss were recorded.
Results
The multivariate Poisson regression models showed that women with untreated/shortly treated osteoporosis were 4 times more likely to present higher number of tooth loss due to periodontal disease than those with normal BMD or treated for ≥ 3 years (risk ratio (RR) = 4.00, 95% CI 1.40–11.27). Higher FRAX was also linked to tooth loss (RR = 1.25, 95% CI 1.02–1.53). Receiver-operating characteristic (ROC) curve suggested that women with history of ≥ 1 tooth losses have higher chances of worse major FRAX (sensitivity = 72.2%; specificity = 72.2%).
Conclusion
In this 5-year study, higher FRAX and untreated osteoporosis were risk factors for tooth loss. Women with normal BMD or treated for osteoporosis for ≥ 3 years did not show increased risk. Management of skeletal conditions should be emphasized with periodontal care for the prevention of tooth loss in elderly women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Global awareness of developing strategies for improving quality of life and reducing health costs among elderly people has increased attention due to the association between systemic bone mass and oral health [1]. Low bone mineral density (BMD) and higher fracture risk probability in ten years (FRAX) have been associated with periodontal disease, which is one of the main causes of tooth loss among adults [2,3,4]. Prospective studies investigating whether low BMD and higher FRAX scores could contribute to the reduction of periodontal apparatus and thus be considered risk factors for tooth loss are important. Despite the importance of the topic, there is a scarcity of studies specifically designed to provide a clear consensus on this issue so far.
Osteoporosis is a systemic skeletal disease characterized by low bone mass and increased risk of fragility fracture. The condition is one of the most common and impactful metabolic diseases in older adults [5, 6]. Fractures are recognized as the hallmark of bone fragility and a major cause of morbidity in elderly people, which are associated with increased mortality and a huge economic burden [7, 8].
In the last years, some evidences suggested that antiresorptive drugs used in the management of osteoporosis may be effective in improving clinical outcomes to periodontal treatment [9,10,11]. A recent meta-analysis on the use of bisphosphonates (BP) associated to nonsurgical mechanical periodontal therapy has shown significant improvements regarding probing depth reduction, clinical attachment level gain and radiographic assessment, favoring the group that used BP [10]. There is a lack of long-term studies on the influence of these medications on tooth loss due to periodontitis in individuals with osteoporosis.
Based on the hypothesis that an impaired systemic bone condition may lead to tooth loss over the years, this 5-year prospective study aimed to investigate whether osteoporosis and increased fracture risk are risk factors for tooth loss due to periodontal disease amongst elderly women. Additionally, the influence of bone medication on this outcome was investigated.
Materials and Methods
Study design, participants and setting
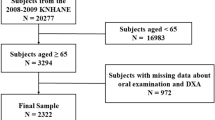
The baseline data of this study was described previously as a cross-sectional involving 134 elderly women aged 65 years or more, which showed that women with osteoporosis, particularly those not treated with antiresorptive drugs, had a greater chance to present severe periodontitis than those with normal BMD [12]. At baseline, all participants received periodontal therapy and were advised to attend periodontal supportive maintenance. BMD was measured by dual-energy x-ray absorptiometry (DXA) at the lumbar spine (L1–L4), femoral neck and total femur. All the assessments were performed in a standardized way, by trained technologists, using a GE Lunar DPX-NP (GE Health Care Clinical Systems Medical Equipment). Women who presented associated diseases or drugs that affected bone (osteopenia, Paget, diabetes mellitus, malignancies, corticosteroids, immunosuppressive drugs or chemotherapy) and those who were smoking were excluded from the study. Eligibility for the 5-year prospective study was to have been treated for periodontitis at baseline and the attendance of a periodontal recall visit at the dental center for a periodontal evaluation. Of the 134 elderly women with baseline data, 60 were unable to participate in the 5-year follow-up. Therefore, data concerning 74 participants were analyzed (follow-up response rate 55.2%) (Fig. 1).
This study was carried out in accordance with the Declaration of Helsinki, informed consents were obtained and received ethical approval by the local Research Ethics Committee, protocol 3.469.969.
Data collection
Fracture risk assessment
FRAX was calculated for each participant at baseline, by filling in the online form of the FRAX calculation tool, adjusted for Brazilian population, with data on age, sex, body mass index, prior fragility fracture, parental history of hip fracture, current tobacco smoking, long-term use of oral glucocorticoids, rheumatoid arthritis, other causes of secondary osteoporosis, and alcohol beverage consumption. FRAX was calculated in two ways: with the inclusion and non-inclusion of femoral neck BMD (www.shef.ac.uk/frax) [13, 14].
Osteoporosis diagnosis
The lowest T-score was considered to classify each participant as normal BMD (T-score ≥ -1 standard deviation (SD) from peak BMD of the lumbar spine, femoral neck and total hip), or as osteoporosis (T-score ≤ − 2.5 SD at any of these sites) [6].
All participants responded a structured questionnaire about low impact fractures occurring after 40 years. Skull, hands and feet fractures were not considered as fragility fractures. Morphometric vertebral fractures were searched using lateral x-rays of thoracic and lumbar spine, according to Genant’s scale.
Description of the primary outcome: tooth loss
The primary outcome variable, modeled as count data, was the number of lost teeth due to periodontal disease, at 5-years follow-up.
This variable was based on the difference between the number of teeth from baseline to follow-up. Tooth loss due to periodontal disease was considered when: the women received such information from their dentists; they were informed that the tooth was affected by “a gingival or periodontal problem”, or that there was tooth mobility related to this problem; they stated that the tooth became loose on its own, without a proper injury; or they were informed by the dentist that the tooth did not present enough support to be maintained in the mouth [15]. The information was double checked for consistency using the electronic patient records of the dental center.
Description of the exposure variables
The exposure variables, for systemic bone condition, were:
- osteoporosis
- baseline FRAX major fracture risk (with and without BMD).
Secondary outcomes: periodontal conditions
One calibrated clinician, blinded for BMD status, performed the full-mouth periodontal examinations in each subject, at baseline and follow-up.
Probing depth (PD) and clinical attachment level (CAL) were measured at six sites (mesial, distal, and middle sites of the buccal and lingual sides) on each tooth, using a North Caroline periodontal probe (Hu-Friedy®, USA). Dental biofilm was recorded using the plaque index (PI) according to absence (score 0 = non-visible) or presence (score 1 = visible). Bleeding on probing (BOP) was also determined in a dichotomous way. Intra-examiner reliability for PD and CAL measurements was calculated at baseline through intra-class correlation (ICC) coefficients. ICC for PD and CAL were 0.80 and 0.88, respectively.
Women were considered to have severe periodontitis at baseline and follow-up if they presented ≥ 2 interproximal sites with CAL ≥ 6 mm (not on the same tooth) and at least and ≥ 1 interproximal site with PD ≥ 5 mm, according to the American Academy of Periodontology and the Center for Disease Control (AAP/CDC) [16]. Based on the World Workshop on the New Classification of Periodontal and Peri‐Implant Diseases and Conditions, periodontitis staging I–IV were attributed according to the severity of periodontitis at follow-up. Grading A, B or C was used as an indicator of the rate of periodontitis progression, based on direct evidence, by CAL change in the worst site of the remaining teeth at 5-years follow-up [17, 18]. Concerning the periodontal approach, the first step at baseline was aimed at guiding behavior change by motivating the patient to undertake successful removal of supragingival dental biofilm and risk factor control, as well as possible plaque-retentive factors that impaired oral hygiene practices. Irrespective of the presence of periodontitis, all of the study participants received oral hygiene instructions, and mechanical therapy, including oral prophylaxis. The cause-related therapy was aimed at controlling periodontitis through subgingival instrumentation. If the treatment has been successful (no PD > 4 mm with BOP or no PD ≥ 6 mm), patients were placed in a supportive periodontal care program, including recommended recall visits at a 4 to 6-month intervals. If not successful, patient was submitted to surgical therapy, whenever appropriated. A tooth was extracted only if it presented a hopeless prognosis. Teeth with mobility grades 1 and 2, including those with furcation involvement, remained in the mouth if they did not cause oral dysfunction. Intervals between periodontal maintenance visits and causes of tooth loss in the last five years were recorded for each participant through a questionnaire during dental appointment.
Statistical analysis
Descriptive statistics were performed for baseline data according to BMD status at baseline (normal BMD/osteoporosis) and also between groups with or without history of tooth loss as a result of periodontal disease at follow-up. Continuous and categorical variables were compared using Mann–Whitney test and chi-square test, respectively. The analyses were also conducted according to subgroups of ‘BMD and bone medication’ during follow-up: G1-Normal BMD, G2-Untreated osteoporosis, G3-Osteoporosis with treatment < 3 years, and G4-Osteoporosis with treatment ≥ 3 years. Wilcoxon test was used to compare periodontal parameters between follow-up and baseline examinations, including PD, CAL, BOP, PI, number of natural teeth, frequencies of severe periodontitis, staging and grading of periodontitis. The association of grades A, B and C of periodontitis with means of FRAX was also explored by means, using Kruskal–Wallis test.
Crude and multivariate Poisson regression analyses with robust covariance were used to estimate risk ratio (RR) and 95% confidence intervals (CIs) on the association of the exposure variables with the main outcome. Multivariate Poisson regression models were adjusted for sociodemographic and clinical factors, specifically: ‘BMD and bone medication’ (G1–G4); ethnicity; age; family income; educational level; plaque index; number of remaining teeth and number of dental maintenance visits.
Receiver operating characteristic (ROC) curve analysis explored the cut-off points of major FRAX related to tooth loss due to periodontal disease among the participants.
Statistical significance was set at 5%. All data processing and analyses were performed using the software SPSS version 21.0 (“Statistical Package for the Social Sciences”, SPSS Inc., Chicago, USA).
Results
Participants: baseline characteristics
Sociodemographic and clinical data of study participants who completed the follow-up were relatively homogeneous regarding most of the sociodemographic features: ethnicity, education, family income, number of dependents, age at menopause, type of menopause (physiological or surgical), except for age at baseline (mean of 68.5 vs. 70.5 years old, for normal BMD and osteoporosis, respectively, p = 0.04). Characteristics related to bone status, and oral health information, are also shown in Table 1. Data related do bone status and FRAX were always significantly worse in the group of women with osteoporosis.
Primary outcome: tooth loss
Table 1 shows patients divided in two groups, according to tooth loss. There were no significant differences in the sociodemographic data of patients presenting or not tooth losses. FRAX probabilities were higher in women with tooth loss during follow-up. Tooth loss was also associated with osteoporosis, specifically when untreated or treated for less than 3 years.
Among the 74 patients, 48 had osteoporosis and 35 had good adherence to osteoporosis medication: bisphosphonates (BP)- alendronate 70 mg/weekly (n = 25), risedronate 35 mg/weekly (n = 5), ibandronate 150 mg/monthly (n = 2); and strontium ranelate 60 mg/daily (n = 3). Of them, 5 women changed to denosumab 60 mg/ml subcutaneously/6 months, 3 to intravenous BP (zoledronic acid 4%, annually), and one to teriparatide 20 mcg/daily. Two more women only used denosumab. The information on adherence to bone treatment was carefully checked by self-reported data and by digital medical records at the hospital. Among the 13 women non-adherent to bone treatment, 6 presented tooth loss at follow-up, whereas only 12 of the 35 women treated for osteoporosis lost teeth. Out of the whole sample, 34 women (45.9%) attended the periodontal appointments at least once a year after baseline; 18 (24.4%) attended between 2 and 3 years, and the last 22 women (29.7%) had just come for the study recall.
In total, 37 teeth were lost by the 18 women who lost teeth due to periodontal causes at follow-up. About their position of them, we observed the following: 5.6% upper incisors, 33.3% lower incisors, 50.0% upper pre-molars/molars, and 11.1% lower pre-molars/molars.
Multivariate analysis for tooth loss
The results of the crude and multivariate Poisson regression analysis, according to the outcomes variables at follow-up, are shown in Table 2.
The number of teeth lost in a 5-year period as a result of periodontal disease was significantly associated with FRAX (with or without femoral neck BMD) and with osteoporosis in crude analysis. However, after adjustments, the association remained significant only for FRAX calculated with BMD (RR = 1.25, 95% CI 1.02–1.53). Neither FRAX without BMD, nor osteoporosis were predictors for tooth loss after adjustments. Multivariate regression showed that ‘BMD and bone medication’ was linked with tooth loss: women with untreated osteoporotic BMD, or with a short period of treatment, were 4 times or more, more likely to present higher number of teeth lost than those with normal BMD (G2; RR = 4.00, 95% CI 1.40–11.27; and G3, RR = 4.58, 95% CI 1.04–20.19; RR = 6.89, 95% CI 1.67–28.36; RR = 7.80, 95% CI 1.67–36.35). Osteoporosis treated ≥ 3 years was not linked to tooth loss.
Secondary outcomes: periodontal parameters
Periodontal evaluation
The periodontal clinical measures according to BMD status are presented in Table 3. The analysis included only teeth which were present at baseline and follow-up exams. There was a significant reduction in the mean of PD, PI, percentage of sites with CAL ≥ 6 mm and number of teeth between baseline and 5-years follow up, as well as a significant increase in worsening interdental CAL.
Comparisons between groups of women with or without osteoporosis did not show differences in periodontal parameters neither at baseline, nor at follow-up.
Association of grade of periodontitis and fracture risk
The associations of grading of periodontitis with mean FRAX scores (with or without BMD) are shown in Table 4. The lower the FRAX probabilities, the lower the grade of periodontitis, that is: the worse systemic bone condition, represented by a higher fracture risk, is associated to the progression of periodontitis over time.
ROC curve, sensitivity and specificity
ROC curve (Fig. 2) showed an area under the curve (AUC) of 0.73 (p = 0.004). A sensitivity of 72.2% and specificity of 72.2% were observed. Women with at least 1 tooth lost due to periodontal disease during follow-up had a 72% likelihood of having major FRAX ≥ 5.15 at baseline, and those with no tooth loss had a 72% chance of having lower FRAX than that.
Discussion
The findings of this 5-year prospective study suggest that untreated/shortly treated osteoporosis and higher FRAX were risk factors for tooth loss. To the best of our knowledge, this was the first study conducted specifically to reach these goals.
Primary outcome
Since the endpoint of periodontal disease is tooth loss, this was the main outcome addressed in this prospective study. Osteoporosis, itself, has not predicted tooth loss due to periodontal disease at follow-up. The focus on risk factors concerning tooth loss should rely on groups of BMD and bone treatment instead, since women with untreated/short treated osteoporosis were more than 4 times more likely to present higher number of teeth losses compared to women with normal BMD or with osteoporosis treated for 3 years or more. Untreated osteoporosis may negatively impact periodontal condition by mechanisms related to disruption of the homeostasis concerning bone remodeling, hormonal balance, and resolution of inflammation [19]. Regression models showed that FRAX major remained associated with tooth loss after adjustments. For grade of periodontitis, statistical significance was lost. Irrespective of this, it was observed that the higher the FRAX, the worse the grading (Table 4). Some authors reported that major FRAX was significantly higher in patients with moderate and severe periodontitis than in those with mild periodontitis [20]. Postmenopausal women with FRAX absolute risk for major fractures higher than 20% had more severe PD, CAL and tooth loss due to periodontal disease than those with lower FRAX scores [21]. In Brazil, relative risk is used for FRAX, instead. The absolute values obtained using FRAX for both major and hip fractures are informed into National Osteoporosis Guideline Group (NOGG for estimation of patients at fracture risk for whom osteoporosis treatment is recommended (www.abrasso.org.br).
The FRAX tool is easily accessed over the internet and may be calculated without BMD when this value is not available, which makes its use very practical [6]. Combining FRAX score with clinical and radiographic evaluations of the periodontium should be recommended in the routine of the dental practice, not only to screen women potentially prone to osteoporotic fractures, but also to support the planning of supportive periodontal therapy and enroll patients in a strict maintenance program to control risk factors for tooth loss as a result of periodontitis progression.
Secondary outcomes
The significant reduction of PD over 5-years may reflect a sound control on the progression of the periodontal disease. Significant differences comparing the periodontal parameters between the groups of women with or without osteoporosis may not have reached significant differences because data were computed only for the remaining teeth at follow-up; also because the sample size was not too large. Thus, these participants presented healthier periodontal conditions, since the teeth affected by severe and progressive periodontal disease were extracted over the 5-year period.
In a 5-year study that explored changes in periodontal disease among postmenopausal females, mean of tooth loss due to periodontal disease was 0.10 [22]. Although that study was not designed to investigate the association between systemic bone condition and tooth loss, the authors reported lower frequency of tooth loss due to periodontal disease (13%) than our findings (24%). A systematic review focusing on the progression of periodontitis in terms of clinical attachment loss, radiographic bone loss and tooth loss revealed an annual mean of tooth loss of 0.20, increasing with advancing age (> 50 years 0.23), and an annual mean of attachment loss of 0.1 mm [23]. These values are higher than our findings. This may be explained by the lower severity of periodontal disease, low exposure to major risk factors for periodontitis (like smoking and diabetes), and adequate oral hygiene, represented by low plaque indexes in the studied sample. If they had not reached autonomy on self-maintained oral health, the amount of biofilm would be higher and periodontal disease might have been more severe after the 5-year period, with more participants with periodontitis grades B or C, and more tooth loss.
Potential clinical relevance
Encouraging adherence to osteoporosis treatment
This study showed that the evaluated outcome was influenced by bone medication use. These drugs have also been related to other oral health improvements [24, 25]. Two recent meta-analyses showed the benefits of systemic BP on CAL when administered along with conventional periodontal treatment [9, 10]. Comparing the effects of the different types of antiosteoporosis drugs on periodontal condition should be explored in future studies.
The goal of bone-targeted drug therapy in patients with osteoporosis is to increase bone strength to decrease the risk of fractures [6]. Improving adherence to osteoporosis therapy requires effective patient/professional communication. Oral health professionals should encourage adherence to osteoporosis treatment, explaining that the risk of medication-related osteonecrosis of the jaw seems to be low in patients with osteoporosis, comparing to the risk of bone fractures in the absence of treatment [26,27,28].
Effects on patient care and health policies
The burden of osteoporosis, fragility fractures and, consequently, the increasing demand for treatment are expected because of the aging process of the population in most countries. It reflects the importance of placing research into aging individuals at the forefront of health research [29, 30].
The development of strategies related to the prevention and treatment of periodontal disease is important for tooth maintenance and quality of life related to oral health in postmenopausal women with impaired systemic bone condition. Dentists should also advise their patients on lifestyle measures to improve bone health by increasing the level of physical activity, reducing or stopping smoking and alcohol beverage intake, reducing the risk of falls and ensuring adequate dietary calcium intake and vitamin D status [31]. In the present study, a significant association was found between grades of periodontitis and FRAX. However, previous research reported that elderly participants in the high risk group of osteoporosis fractures did not show more severe periodontal condition, according to Community Periodontal Index (CPI), than those in the low and moderate risk group. The authors acknowledged that the role of number of remaining natural teeth in the oral cavity would be more critical than the inflammatory status of the periodontium on the incidence of osteoporotic fracture in elderly women. Discrepancies between the findings of both studies possibly occurred due to methodological differences, such as the studied population, study design, and mainly due to the discrepancies in the clinical periodontal indexes used to assess participant’s periodontal status. In the present study, grade was considered an appropriate periodontal index to evaluate the possible link between periodontitis progression with osteoporosis risk fracture, since grade represents a specific measure of periodontal disease, namely impaired periodontal status over time [32].
Besides that, it is worthy to notice that ROC curve showed that the history of tooth loss due to periodontal disease in the last 5 years could be an useful tool to indicate worse major FRAX. Dentists should refer elderly women to the physician evaluation when detecting one or more losses in the dental exam.
Final considerations
There are some limitations to be addressed in this study, like the small sample size, which influences the precision of the association measurement, decreasing the statistical power. It results in loss of generalizability and, consequently, on the reliability of the findings. If the follow-up response rate was higher, or the follow-up was longer, it could have resulted in more patients enrolled in the study, and consequently, greater power. Moreover, this study was conducted in a naval-based hospital. Thus, the participants, who were relatives of military personnel, were assisted by experienced professionals at the naval dental center and hospital, which may not reflect the reality of the available healthcare assistance to the general population.
A limitation would be that most of the women with osteoporosis were treated with bone medication. However, this issue was addressed by adjusting the analyses for four groups according to BMD and bone medication (G1–G4). If osteoporosis was not properly managed in the studied sample, then periodontal tissues could have been worsened over the years, and the negative effects of systemic bone fragility on periodontal tissues would be stronger. Not offering treatment to these women would be unacceptable, unethical, for exposing them to a higher risk of fractures, thus, increasing the related morbidity and mortality.
We recognize that the goals concerning ideal intervals for periodontal maintenance were not reached. Although we recommended intervals up to six months, less than 50% of the participants with severe periodontitis at baseline adhered to these adequate recall intervals. Despite that, improved periodontal status over the 5-year period has evidenced that periodontal therapy was effective, and is worthy, as consensually recognized [33]. The prevention of periodontal diseases requires the improvement of knowledge, better health literacy, patient empowerment, motivation, and compliance [34].
In conclusion, an impaired systemic bone condition, represented by untreated osteoporosis, and higher FRAX were predictors for tooth loss due to periodontal disease over a 5-year period in the studied population of elderly women. However, when managed with bone medication for ≥ 3 years, osteoporosis was not a risk factor for tooth loss.
References
Friedman PK, Lamster IB (2016) Tooth loss as a predictor of shortened longevity: exploring the hypothesis. Periodontol 2000 72:142–152
Penoni DC, Fidalgo TK, Torres SR, Varela VM, Masterson D et al (2017) Bone density and clinical periodontal attachment in postmenopausal women: a systematic review and meta-analysis. J Dent Res 96:261–269
Jepsen S, Caton JG, Albandar JM, Bissada NF, Bouchard P et al (2018) Periodontal manifestations of systemic diseases and developmental and acquired conditions: consensus report of workgroup 3 of the 2017 world workshop on the classification of periodontal and peri-implant diseases and conditions. J Periodontol 89:S237–S248
Albandar JM, Susin C, Hughes FJ (2018) Manifestations of systemic diseases and conditions that affect the periodontal attachment apparatus: case definitions and diagnostic considerations. J Clin Periodontol 45:S171–S189
Almeida M, Laurent MR, Dubois V, Claessens F, O’Brien CA et al (2017) Estrogens and androgens in skeletal physiology and pathophysiology. Physiol Rev 97:135–187
Kanis JA, Cooper C, Rizzoli R, Reginster JY (2019) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int 30:3–44
Curtis EM, Moon RJ, Harvey NC, Cooper C (2017) The impact of fragility fracture and approaches to osteoporosis risk assessment worldwide. Bone 104:29–38
Binkley N, Blank RD, Leslie WD, Lewiecki EM, Eisman JA, Bilezikian JP (2017) Osteoporosis in crisis: it’s time to focus on fracture. J Bone Miner Res 32:1391–1394
Akram Z, Abduljabbar T, Kellesarian SV, Abu Hassan MI, Javed F, Vohra F (2017) Efficacy of bisphosphonate as an adjunct to nonsurgical periodontal therapy in the management of periodontal disease: a systematic review. Br J Clin Pharmacol 83:444–454
Muniz F, Silva BFD, Goulart CR, Silveira TMD, Martins TM (2021) Effect of adjuvant bisphosphonates on treatment of periodontitis: systematic review with meta-analyses. J Oral Biol Craniofac Res 11:158–168
Yu B, Wang CY (2022) Osteoporosis and periodontal diseases - an update on their association and mechanistic links. Periodontol 2000. 89:99–113
Penoni DC, Torres SR, Farias ML, Fernandes TM, Luiz RR, Leao AT (2016) Association of osteoporosis and bone medication with the periodontal condition in elderly women. Osteoporos Int 27:1887–1896
Kanis JA, Harvey NC, Cooper C, Johansson H, Oden A, McCloskey EV (2016) A systematic review of intervention thresholds based on FRAX: a report prepared for the national osteoporosis guideline group and the international osteoporosis foundation. Arch Osteoporos 11:25
Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B et al (2014) Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 25:2359–2381
Eke PI, Dye B (2009) Assessment of self-report measures for predicting population prevalence of periodontitis. J Periodontol 80:1371–1379
Eke PI, Page RC, Wei L, Thornton-Evans G, Genco RJ (2012) Update of the case definitions for population- based surveillance of periodontitis. J Periodontol 83:1449
Tonetti MS, Greenwell H, Kornman KS (2018) Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. J Clin Periodontol 45:S149-s161
Papapanou PN, Sanz M, Buduneli N, Dietrich T, Feres M et al (2018) Periodontitis: consensus report of workgroup 2 of the 2017 world workshop on the classification of periodontal and peri-implant diseases and conditions. J Clin Periodontol 45:S162–S170
Wang CJ, McCauley LK (2016) Osteoporosis and periodontitis. Curr Osteoporos Rep 14:284–291
Kalinowski P, Rozylo-Kalinowska I, Piskorz M, Bojakowska-Komsta U (2019) Correlations between periodontal disease, mandibular inferior cortex index and the osteoporotic fracture probability assessed by means of the fracture risk assessment body mass index tool. BMC Med Imaging 19:41
Alli F, Bhandal GK, Thacker HL, Palomo L (2015) Can the FRAX tool be a useful aid for clinicians in referring women for periodontal care? Menopause J North Am Menopause Soc 22:75–78
LaMonte MJ, Hovey KM, Genco RJ, Millen AE, Trevisan M, Wactawski-Wende J (2013) Five-year changes in periodontal disease measures among postmenopausal females: the buffalo osteoperio study. J Periodontol 84:572–584
Needleman I, Garcia R, Gkranias N, Kirkwood KL, Kocher T et al (2018) Mean annual attachment, bone level, and tooth loss: a systematic review. J Clin Periodontol 45:S112–S129
Shah NP, Nayee S, Pazianas M, Sproat C (2017) Beyond ONJ - a review of the potential uses of bisphosphonates in dentistry. Br Dent J 222:727–730
Sedghizadeh PP, Sun S, Jones AC, Sodagar E, Cherian P et al (2021) Bisphosphonates in dentistry: historical perspectives, adverse effects, and novel applications. Bone 147:115933
Madeira M, Rocha AC, Moreira CA, Aguiar ÁMM, Maeda SS et al (2020) Prevention and treatment of oral adverse effects of antiresorptive medications for osteoporosis - a position paper of the Brazilian Society of Endocrinology and Metabolism (SBEM), Brazilian Society of Stomatology and Oral Pathology (Sobep), and Brazilian Association for Bone Evaluation and Osteometabolism (Abrasso). Arch Endocrinol Metab. https://doi.org/10.20945/2359-3997000000301
Kim SH, Lee YK, Kim TY, Ha YC, Jang S, Kim HY (2021) Incidence of and risk for osteonecrosis of the jaw in Korean osteoporosis patients treated with bisphosphonates: a nationwide cohort-study. Bone 143:115650
Ruggiero SL, Dodson TB, Aghaloo T, Carlson ER, Ward BB, Kademani D (2022) American association of oral and maxillofacial surgeons’ position paper on medication-related osteonecrosis of the Jaws-2022 update. J Oral Maxillofac Surg 80:920–943
Briggs AM, Shiffman J, Shawar YR, Åkesson K, Ali N, Woolf AD (2020) Global health policy in the 21st century: challenges and opportunities to arrest the global disability burden from musculoskeletal health conditions. Best Pract Res Clin Rheumatol 34:101549
GBD 2017 Disease and Injury Incidence and Prevalence Collaborators (2018) Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 392:1789–1858
Compston J, Cooper A, Cooper C, Gittoes N, Gregson C et al (2017) UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos 12:43
Hong SW, Lee J, Kang JH (2023) Associations between oral health status and risk of fractures in elder adults. Sci Rep. 13:1361
Sanz M, Herrera D, Kebschull M, Chapple I, Jepsen S et al (2020) Treatment of stage I-III periodontitis-the EFP S3 level clinical practice guideline. J Clin Periodontol. 47:4–60
Cota LOM, Villar CC, Vettore MV, Campos JR, Amaral G et al (2021) Periodontal diseases: is it possible to prevent them? A populational and individual approach. Braz Oral Res 35:e098
Funding
This study was not funded.
Author information
Authors and Affiliations
Contributions
DCP, SRT and ATTL: made substantial contributions to the conception and design of the study. DCP, MLO, MVV and MLFF: contributed to acquisition, analysis, and interpretation of data. DCP: drafted the manuscript. SRT, MLO, MLFF, MVV and ATTL: contributed to revising the article critically for important intellectual content. All authors approved the final version of the article to be published.
Corresponding author
Ethics declarations
Conflict of interest
Daniela Cia Penoni, Sandra Regina Torres, Matheus Lima Oliveira, Maria Lucia Fleiuss Farias, Mario Vianna Vettore and Anna Thereza Thomé Leão declare that they have no conflict of interest.
Ethics approval
Our study was carried out in accordance with the Declaration of Helsinki and received ethical approval by Hospital Clementino Fraga Filho/Universidade Federal do Rio de Janeiro Research Ethics Committee, in Rio de Janeiro, Brazil, protocol 3.469.969.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Penoni, D.C., Torres, S.R., Oliveira, M.L. et al. Untreated osteoporosis and higher FRAX as risk factors for tooth loss: a 5-year prospective study. J Bone Miner Metab 41, 727–737 (2023). https://doi.org/10.1007/s00774-023-01451-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-023-01451-w