Abstract
Introduction
Risk factors associated with subchondral insufficiency fracture (SIF) of the femoral head have not been established. The aim of the present study was to determine the incidence and risk factors for SIF of the femoral head following renal transplantation (RT).
Materials and methods
We analyzed the cases of 681 RT patients (mean age at surgery: 49.5 ± 13.6 years, 249 women, 432 men) to determine the incidence of SIF. Hip magnetic resonance imaging (MRI) was performed 6 months post-RT. The following potential predictors of SIF were evaluated: (1) patient’s condition at RT: bone mineral density (BMD), pre-RT laboratory values including calcium (Ca), phosphorus (P), calcium-phosphorus product (Ca × P), and intact parathyroid hormone; the patient and donor’s blood relationship; and mismatching number of human leukocyte antigens (HLAs), and (2) post-RT dosage(s) of steroid(s), the immunosuppressive regimen, and the incidence of acute rejection.
Results
SIF was observed in 15 hips (13 patients, 1.9%). We successfully matched 39 patients without SIF. A multivariate logistic regression analysis adjusted for cumulative dosages of steroids, revealed the following were risk factors for SIF: osteoporosis (OR: 11.4, p = 0.046), lumbar BMD (OR: 0.003, p = 0.038), pre-RT serum P (OR 2.68, p = 0.004), and pre-RT serum Ca × P (OR: 1.11, p = 0.005).
Conclusion
Since osteoporosis, the lumbar BMD, serum P, and serum Ca × P were identified as risk factors for a post-RT SIF, these factors should be evaluated before RT for the prediction of the SIF risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
A subchondral insufficiency fracture (SIF) of the femoral head is a serious complication and a potential cause of the femoral head collapse, which leads to considerable restriction in the patient's function and eventual disability, ultimately causing a femoral collapse that requires a total hip arthroplasty [1]. A SIF of the femoral head is recognized as a musculoskeletal complication that is similar in some respects to osteonecrosis of the hip after renal transplantation (RT) [2,3,4,5]. The precise prevalence of SIF is unknown. A recent histopathological re-evaluation noted that SIF was observed in 6.3% of patients with a preoperative diagnosis of osteoarthritis, and in 11.1% of patients with osteonecrosis of the femoral head [6]. Among 300 consecutive RT patients for whom magnetic resonance imaging (MRI) of the hip was conducted, a SIF of the femoral head was observed in 1.0% (five hips, three patients) [2]. There have been few investigations of the incidence of SIF in a large sample of RT patients.
Several risk factors for the development of SIF have been reported. In several populations that did not include RT patients, these factors included older age, osteoporosis, military recruit status, transplant patient status, chronic steroid use, and tumor osteomalacia [7,8,9]. No studies have statistically established the risk factors associated with SIF. Our institution performs the greatest number of RTs according to the uniform immunosuppressive regimen in Japan, and our RT protocol includes a routine MRI examination of the hip 6 months post-RT. We conducted this study to determine the precise prevalence of SIF among our RT patients, and we performed a complementary case–control study to evaluate the risk factors for post-RT SIF.
Chronic renal failure involves a failure to metabolize vitamin, failure to excrete phosphorus, and failure to absorb calcium, which together cause hyperphosphoremia and hypocalcemia, resulting in osteoporosis [4]. The use of steroids and immunosuppressive agents after RT has also been reported to cause secondary osteoporosis [4]. We focused herein on the roles of osteoporosis, serum parathyroid hormone, calcium, and phosphorus in relation to SIF. This prospective study of > 600 patients who underwent RT investigated (1) the incidence of SIF and (2) factors that could be used to predict the occurrence of a SIF after RT, examining osteoporosis, serum parathyroid hormone, calcium, and phosphorus in particular.
Materials and methods
Patient
Between January 2015 and October 2018, 737 patients underwent a living-donor RT at our institution. Patients aged ≤ 19 years (n = 13), patients in whom osteonecrosis of the femoral head was confirmed before their RT (n = 4), those who had not undergone an MRI examination 6 months after their RT (n = 36), and others (n = 3) were excluded from the present analyses. The reasons that MRI could not be performed after some of the patients' RT included claustrophobia and the presence of a heart pacemaker.
We evaluated a final total of 681 RT patients (249 women, 432 men) to determine the incidence of SIF. None of the patients had a confirmed SIF before their RT. Informed consent was obtained from all patients for the publication of their data, and the study was approved by our hospital's ethics committee.
Five immunosuppressive drugs (cyclosporin, tacrolimus taken 1 × /day, tacrolimus taken 2 × /day, mycophenolate mofetil, and everolimus) were administered to the patients after the RT. In all patients, prednisolone (PSL: 60 mg intravenously) was administered 1 h before the RT, and methylprednisolone 500 mg was administered during the RT. Oral PSL administration was started on a postoperative day (POD) 1 using the following protocol: 60 mg on POD1, 50 mg on POD2, 40 mg on POD3, 30 mg on POD4, 20 mg on POD5, 15 mg on POD6, and 10 mg on POD7 to POD14. If the blood types of the donor and recipient were different, PSL 10 mg/day was administered for 2 weeks before the RT. In a case of acute rejection (AR) after RT, methylprednisolone 500 mg/day was administered for 3 days. To calculate the cumulative glucocorticoid dose, the methylprednisolone dosage was converted to prednisolone equivalents by multiplying it by 1.25 [10].
MRI of the hip using a 1.5 T superconducting magnet (Ingenia 1.5; Philips Healthcare, Amsterdam, Netherlands) was performed 6 months after each patient’s RT. An irregular and serpiginous shape with a low-intensity band parallel to the articular surface on T1-weighted images was defined as a SIF [11]. A bone mineral density (BMD) (Discovery; Hologic, Tokyo) examination of the left forearm and lumbar spine (Philips Healthcare) was performed 1 month before each patient’s RT, and laboratory tests were performed 1 month before and 8 weeks and 6 months after the RT. Blood collection in hemodialysis patients was performed on a non-dialysis day before the RT.
We prospectively performed the examinations and retrospectively collected and analyzed the data. For the evaluation of potential predictors of SIF, we assigned the patients to one of two groups based on whether they developed a SIF, i.e., the SIF and non-SIF groups. The non-SIF patients were matched to SIF patients by age (± 2 years), sex, and BMI (± 2 kg/m2). The following potential predictors of SIF were evaluated: (1) the patient's condition at the time of transplantation: age at surgery; sex; BMI; alcohol consumption and smoking habit; osteoporosis; osteopenia; BMDs (left forearm, lumbar spine); steroid treatment before renal transplantation; pre-RT dialysis duration; secondary hyperparathyroidism; laboratory test results including creatinine, blood urea nitrogen (BUN), calcium (Ca), phosphorus (P), calcium-phosphorus product (Ca × P), alkaline phosphatase (ALP), intact parathyroid hormone (PTH), and uric acid (UA) before RT; the relationship between the patient and donor blood types; ABO mismatch; mismatching number of human leukocyte antigens (HLAs), especially HLA class I and class II; and (2) post-RT parameters: dosages of steroids at 4 and 8 weeks and 6 months after transplantation; laboratory test results including creatinine, BUN, and UA 8 weeks post-RT; immunosuppressive regimen; incidence of AR; and delayed graft function (DGF).
AR was diagnosed based on a biopsy. DGF was defined as the need for hemodialysis in the early post-RT phase. Based on the left forearm or lumbar spine BMD, a BMD value > 70% but < 80% of the young adult mean (YAM) was diagnosed as osteopenia, and a BMD ≤ 70% of the YAM was diagnosed as osteoporosis [12].
Statistical analyses
The statistical analyses included Fisher’s exact test, Student’s t-test, and uni- and multivariate logistic regression analyses. A multivariate logistic regression analysis was performed with adjustment for the cumulative dosages of steroids at 6 months. We performed a receiver-operating characteristic (ROC) curve analysis to identify volume thresholds at which significant changes in the risk probability of SIF occurred. All analyses were performed using SPSS ver. 22 (IBM, Armonk, NY). A p-value < 0.05 was considered significant.
Results
Of the 681 patients, the average patient age at the time of RT surgery was 49.5 ± 13.6 years (range 20–78 years), and the mean body mass index (BMI) was 22.8 ± 4.0 kg/m2 (range 10.1–38.4 kg/m2). Of the 681 patients, 297 (43.6%) had received dialysis before their RT. The average pre-RT dialysis duration was 2.0 ± 4.0 years (range 1 month to 28 years). The causes of the patients’ end-stage renal disease included diabetes mellitus (n = 152), immunoglobulin A nephropathy (n = 99), chronic glomerular nephritis (n = 94), nephrosclerosis (n = 50), polycystic kidney disease (n = 50), focal glomerulosclerosis (n = 28), unknown causes (n = 113), and other causes (n = 95).
A SIF occurred in 15 hips (13 patients, 1.9%). The patients with a SIF did not have severe symptoms such as pain. Of the 668 patients (244 women, 424 men) without a SIF, the average patient age at the time of RT surgery was 49.2 ± 13.6 years (range 20–78 years), and the mean BMI was 22.9 ± 4.0 kg/m2 (range 10.1–38.4 kg/m2). Compared to the non-SIF patients, the SIF group was older and had lower body weights; it also included more women.
We successfully matched the SIF group with 39 patients without SIF. All 13 of the patients with a SIF achieved symptom resolution with non-operative treatment. The mean cumulative corticosteroid doses from surgery to 2, 3, 4, 6, and 8 weeks and 6 months after RT are shown in Supplementary Table S1; there were no significant differences in any of the values between the SIF and non-SIF groups.
As shown in Tables 1 and 2, the results of the univariate analysis revealed that the factors predictive of the development of a SIF were as follows for the SIF and non-SIF groups, respectively: the prevalence of osteoporosis (23.1% and 2.6%, p = 0.044), the lumbar BMD (0.81 and 0.94 g/cm2, p = 0.025), a mismatching number of class II HLAs (1.3 and 0.9, p = 0.044), serum P before RT (6.3 and 4.9 mg/dL, p = 0.001), and serum Ca × P before RT (56.1 and 44.1 mg2/dL2, p = 0.001). However, according to the multivariate logistic regression analysis adjusted for the cumulative dosages of steroids at 6 months, a mismatching number of class II HLA was not significantly associated with SIF. As shown in Table 3, the following were potential risk factors for the occurrence of a SIF after RT: osteoporosis (odds ratio [OR]: 11.4, 95% confidence interval [CI]: 1.04–2118.7, p = 0.046), the lumbar BMD (OR: 0.003, 95%CI: 0.01–0.72, p = 0.038), the pre-RT serum P (OR 2.68, 95%CI: 1.36–5.29, p = 0.004), and the pre-RT serum Ca × P (OR: 1.11, 95%CI: 1.03–1.21, p = 0.005).
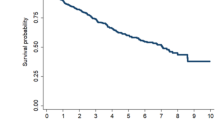
The ROC curve analysis revealed that a pre-RT serum P value of 5.6 mg/dL and a pre-RT Ca × P value of 51.7 mg2/dL2 were the cut-off points for the occurrence of a SIF. As illustrated in Fig. 1, for serum P, the area under the curve (AUC) was 0.78 with 0.692 sensitivity and 0.744 specificity. For the Ca × P value, the AUC was 0.77 with 0.846 sensitivity and 0.769 specificity. The lumbar BMD did not have a defined significant cut-off point.
The results of the ROC curve analysis to identify volume thresholds at which significant changes of the risk probability of the occurrence of a subchondral insufficiency fracture (SIF) of the femoral head. No significant cut-off point for the lumbar bone mineral density (BMD) before renal transplantation (RT) was revealed. The pre-RT serum phosphorus (P) value 5.6 mg/dL (0.692 sensitivity, 0.744 specificity) and the pre-RT calcium-phosphorus product (Ca × P) value 51.7 mg2/dL2 (0.846 sensitivity, 0.729 specificity) were revealed to be the cut-off points for the occurrence of a SIF of the femoral head, with respective areas under the curve (AUCs) of 0.78 and 0.77 and 95%CIs at 0.639–0.929 and 0.624–0.910
Discussion
This study is the first to estimate the prevalence of SIF and potential risk factors for the development of a SIF, based on the largest number of RT patients to date (n = 681). SIF of the femoral head has been most commonly observed in patients with osteoporosis among both RT patients and non-RT patients [2, 13], but no reports have statistically established that osteoporosis or other factors are risk factors associated with a SIF of the femoral head. Our present findings demonstrated that osteoporosis is one of the potential risk factors for SIF. We were unable to determine cut-off values for the BMD at several body sites. The average lumbar BMD of our patients with a SIF was 0.81 g/cm2, which was considered possible osteopenia. Additional studies are necessary to detect significant cut-off values for other factors that may be related to the occurrence of a SIF.
Corticosteroid use can lead to bone loss and an increased risk of fracture. For example, fracture risk is associated with a prednisolone dose of 2.5–7.5 mg/day [14]. A prednisolone dose ≥ 30 mg/day with a cumulative dose > 5 g was reported to pose a marked increase in the relative risk of vertebral and hip fractures [15]. The steroid doses used for our patients were low compared to those in previous reports, and we observed no significant cumulative dose difference between the SIF and non-SIF groups.
To the best of our knowledge, there is no published report on the relationship between high values of serum P and Ca × P and the occurrence of a SIF after RT. This study is the first to report that elevated serum P and Ca × P are potential risk factors for a SIF after renal transplantation, independent of corticosteroid use. Notably, serum P and Ca × P are frequently elevated in individuals with end-stage renal disease [16], and elevated serum P and Ca × P were reported to be associated with vascular calcification [15, 16].
Among our RT patients, the SIF patients’ serum P (average 6.3 mg/dL) and Ca × P (average 56.1 mg2/dL2) values were higher than those of the non-SIF patients. A relationship between osteoporosis and vascular events including arteriosclerosis has been described [17, 18], and arteriosclerosis could have a direct effect on bone tissue via an ischemic mechanism [19]. These might be one of the reasons that elevated serum P and Ca × P pose a risk for the development of a SIF.
This study has some limitations. There was a relatively small number of patients with SIFs (n = 13, 15 hips). However, most of the relevant past publications are case reports with low numbers of patients. Our findings are based on consecutive cases and a relatively large number of SIF patients. No power analysis was performed to determine whether a sufficient number of patients was included to detect clinically meaningful differences between groups.
It is possible that the patients’ SIFs occurred before their RTs, as MRI examinations were not performed immediately before the RTs and the SIF symptoms were not severe. We may thus have been unable to detect the precise number of cases.
It is also possible that some of the SIFs occurred > 6 months after the RTs; we may thus have not detected the actual number of SIF cases. Some SIFs have been first detected on MRI within 3 months after transplantation [2, 4], and the number of patients who develop a SIF > 6 months after their RT is thus likely to be small and not likely to have influenced the present results. It is difficult to distinguish SIF and osteonecrosis of the femoral head when a low-intensity band on T1-weighted images is extremely small [2].
Medications for osteoporosis (such as bisphosphonates) may have a high correlation with SIF. However, we did not include the use/nonuse of osteoporosis medications in our analyses. Additional investigations are necessary to clarify the correlation between osteoporosis medication use and SIF.
Factors other than age, sex, BMI, and the cumulative dosage of steroids were not adjusted. It is possible that factors such as the status before RTs (i.e., hemodialysis, peritoneal dialysis, or non-dialysis) and history of steroid treatment were major confounders. Further studies are needed to determine whether other factors increase the risk of the occurrence of a SIF.
Blood samples were collected from the hemodialysis patients on a non-dialysis day. Since hemodialysis patients' blood data change depending on the timing of the blood collection, it is possible that the blood collection timing in this study could have influenced the blood data.
Availability of data and materials
The datasets during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Bangil M, Soubrier M, Dubost JJ, Rami S, Carcanagues Y et al (1996) Subchondral insufficiency fracture of the femoral head. Rev Rhum Engl Ed 63:859–861
Ohtsuru T, Yamamoto T, Murata Y, Morita Y, Munakata Y et al (2019) Incidence of osteonecrosis and insufficiency fracture of the hip and knee joints based on MRI in 300 renal transplant patients. Hip Int 29:316–321
Ohtsuru T, Yamamoto T, Murata Y, Morita Y, Munakata Y et al (2017) Bilateral subchondral insufficiency fractures of the femoral head in patients with living renal transplantation: a report of two cases. J Orthop Sci 22:972–975
Ikemura S, Yamamoto T, Nakashima Y, Shuto T, Jingushi S et al (2005) Bilateral subchondral insufficiency fracture of the femoral head after renal transplantation: a case report. Arthritis Rheum 52:1293–1296
Higuchi Y, Tomosugi T, Futamura K, Okada M, Narumi S et al (2020) Incidence and risk factors for osteonecrosis of the hip in renal transplant patients: a prospective single-centre study. Int Orthop 44:1927–1933
Yamamoto T, Iwamoto Y, Schneider R, Bullough PG (2008) Histopathological prevalence of subchondral insufficiency fracture of the femoral head. Ann Rheum Dis 67:150–153
Kim S-M, Oh S-M, Cho C-H, Lim S-J, Moon Y-W et al (2016) Fate of subchondral fatigue fractures of femoral head in young adults differs from general outcome of fracture healing. Injury 47:2789–2794
Hackney LA, Lee MH, Joseph GB, Vail TP, Link TM (2016) Subchondral insufficiency fractures of the femoral head: associated imaging findings and predictors of clinical progression. Eur Radiol 26:1929–1941
Kobayashi H, Ito N, Akiyama T, Okuma T, Kinoshita Y et al (2017) Prevalence and clinical outcomes of hip fractures and subchondral insufficiency fractures of the femoral head in patients with tumour-induced osteomalacia. Int Orthop 41:2597–2603
Lopez-Ben R, Mikuls TR, Moore DS, Julian BA, Bernreuter WK et al (2004) Incidence of hip osteonecrosis among renal transplantation recipients: a prospective study. Clin Radiol 59:431–438
Yamamoto T, Schneider R, Bullough PG (2001) Subchondral insufficiency fracture of the femoral head: histopathologic correlation with MRI. Skeletal Radiol 30:247–254
Soen S, Fukunaga M, Sugimoto T, Sone T, Fujiwara S et al (2013) Diagnostic criteria for primary osteoporosis: year 2012 revision. J Bone Miner Metab 31:247–257
Gaudiani MA, Samuel LT, Mahmood B, Sultan AA, Kamath AF (2020) Subchondral insufficiency fractures of the femoral head: systematic review of diagnosis, treatment and outcomes. J Hip Preserv Surg 7:85–94
Buckley L, Guyatt G, Fink HA, Cannon M, Grossman J et al (2017) 2017 American College of Rheumatology guideline for the prevention and treatment of glucocorticoid-induced osteoporosis. Arthritis Rheumatol 69:1521–1537 ((Hoboken, NJ))
van Staa T-P, Geusens P, Pols HAP, Laet C-D, Leufkens H-G-M et al (2005) A simple score for estimating the long-term risk of fracture in patients using oral glucocorticoids. QJM 98:191–198
Boaz M, Weinstein T, Matas Z, Green SS (2005) Peripheral vascular disease and serum phosphorus in hemodialysis: a nested case-control study. Clin Nephrol 63:98–105
Laroche M (1996) [Arteriosclerosis and osteoporosis]. Presse Med 25(2):52–4
Szulc P, Kiel DP, Delmas PD (2008) Calcifications in the abdominal aorta predict fractures in men: MINOS study. J Bone Miner Res 23:95–102
Campos-Obando N, Koek WNH, Hooker ER, Eerden BCVD, Pols HA et al (2017) Serum phosphate is associated with fracture risk: the rotterdam study and MrOS. J Bone Miner Res 32:1182–1193
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Material preparation, data collection and analysis were performed by KF, MO, TK, HS, KK, SN, YW, NG, TA and KS. The first draft of the manuscript was written by TT and YH and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.”
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the ethics committee of our hospital.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Higuchi, Y., Tomosugi, T., Futamura, K. et al. Risk factors for subchondral insufficiency fracture of the femoral head in renal transplant patients. J Bone Miner Metab 40, 968–973 (2022). https://doi.org/10.1007/s00774-022-01360-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-022-01360-4