Abstract
Interferon-induced transmembrane protein 5 (IFITM5) is an osteoblast-specific membrane protein that has been shown to be a positive regulatory factor for mineralization in vitro. However, Ifitm5 knockout mice do not exhibit serious bone abnormalities, and thus the function of IFITM5 in vivo remains unclear. Recently, a single point mutation (c.-14C>T) in the 5′ untranslated region of IFITM5 was identified in patients with osteogenesis imperfecta type V (OI-V). Furthermore, a single point mutation (c.119C>T) in the coding region of IFITM5 was identified in OI patients with more severe symptoms than patients with OI-V. Although IFITM5 is not directly involved in the formation of bone in vivo, the reason why IFITM5 mutations cause OI remains a major mystery. In this review, the current state of knowledge of OI pathological mechanisms due to IFITM5 mutations will be reviewed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
IFITM5 (also known as BRIL) is a member of the interferon-induced transmembrane (IFITM) protein family. There are 5 family members in humans (IFITM1, 2, 3, 5, and 10) and 7 in mice (IFITM1, 2, 3, 5, 6, 7, and 10). IFITM1, 2, and 3 are induced by interferon and participate in a protective mechanism against viral infections [1, 2]. IFITM5 is not induced by interferon and thus does not participate in a protection mechanism against viruses [3, 4]. IFITM5’s function has been investigated primarily by Moffatt’s group and our group. IFITM5 was identified by high-throughput screening for cDNA encoding secretory and membrane proteins in osteoblasts [5]. Subsequently, global gene expression analysis of cultured murine osteoblasts suggested that Ifitm5 (murine IFITM5 gene) was expressed during mineralization [6]. Other IFITM members localize to the endosome compartment [4, 7, 8], but IFITM5 localizes to the cell membrane [9]. IFITM5 was thought to have two transmembrane regions and a type III (N-out/C-out) topology [9], but recently it was shown to have one transmembrane region and a type II (N-in/C-out) topology, and to localize to the endoplasmic reticulum and cell membrane (Fig. 1) [10]. Conserved cysteine at residues 52, 53, and 86 of murine IFITM5 (C50, C51, and C84 in human IFITM5) is palmitoylated and functions as intramembrane anchors (Fig. 1) [10]. Furthermore, palmitoylation of C52 and C53 is important for targeting IFITM5 to the cell membrane and for its stability [10].
Topology and localization of murine IFITM5. IFITM5 is localized to the endoplasmic reticulum and then transported to the Golgi apparatus. S-Palmitoylation at C52, C53, and C86 occurs either in the endoplasmic reticulum and/or the Golgi apparatus. The palmitoylated IFITM5 is finally targeted to the plasma membrane. Reproduced with permission [10]
Distinct from the other IFITM members, which show ubiquitous expression, IFITM5 is expressed specifically in the initial stage of osteoblast mineralization [9, 11]. In in vitro studies, Ifitm5 overexpression in osteoblasts promotes mineralization and, conversely, Ifitm5 knockdown by short hairpin RNA suppresses mineralization. Thus, IFITM5 was suggested as a positive mineralization regulatory factor [9]. However, Ifitm5 knockout mice (Ifitm5 −/−) did not show any major abnormalities in osteogenesis (Fig. 2a) [11]. Rarely, long bones in Ifitm5 knockout mice exhibited bending (Fig. 2b). However, most IFITM5 knockout mice did not show these abnormalities [11]. These results collectively suggested that IFITM5 does not function as a positive regulator of mineralization in vivo.
Skeletal phenotype of heterozygous and homozygous Ifitm5-deficient newborn mice. a No significant change in skeletal phenotype is observed between heterozygous and homozygous Ifitm5-deficient newborn mice. b Bending of long bones is rarely observed in homozygous Ifitm5-deficient mice. Reproduced with permission [11]
In 2012, one year after our group published a study on Ifitm5 knockout mice bone phenotype, it was reported that patients with osteogenesis imperfecta type V (OI-V) presented mutations in IFITM5 (the human IFITM5 gene) [12, 13]. Furthermore, in 2014, different mutations in IFITM5 were found in OI patients with more severe symptoms than patients with OI-V [14–16]. From these findings arose the question of how mutations in IFITM5, previously thought to have no function in mineralization in vivo, can induce OI.
The clinical phenotype of OI-V is distinct from other OI
OI is a hereditary connective tissue disorder characterized by bone fragility, and can be categorized into at least 12 subtypes [17]. In autosomal dominant OI, most cases are caused by defects in the COLIA1 or COLIA2 genes [18–20]. These mutations affect the basic structure or the synthesis levels of type I collagen [21–26]. On the other hand, autosomal recessive OI is caused by defects in genes that affect the stability of the structure of type I collagen (CRTAP, LEPREI1, PPIB, SERPINH1, FKBP10, and BMP1) [27–34]. In addition to these causative genes, it has been shown that mutations of SERPINF1, SP7, TMEM38B, and WNT1, whose productions are not involved in the stability of collagen structure, also cause autosomal recessive OI [35–42]. OI caused by mutations of SP7, TMEM38B, and WNT1 are as yet unclassified [17].
OI-V is an autosomal dominant OI as defined by Glorieux et al. [43]. Less than 5 % of patients with OI are diagnosed with OI-V [44]. The OI-V clinical phenotype differs from other OI, and is characterized by forearm interosseous membrane calcification and hyperplastic callus formation (Fig. 3). However, OI-V exhibits a broad inter-patient disease severity. Forearm interosseous membrane calcification is observed in essentially all patients and it is associated with a limitation in forearm supination/pronation [12, 15, 43, 45–49]. Hyperplastic callus formation occurs during the healing period of bone fractures, but is not observed in all patients [12, 15, 43, 45–49]. Radial head dislocation is observed in many patients and is a cause of elbow deformity [12, 37, 43, 48, 49]. Furthermore, features such as a radiographically dense band of forearm metaphyses [43, 50] and mesh-like lamellation patterns on bone histology [43, 45, 49] are also OI-V characteristics. A hyper-dense metaphyseal band is first observed in infancy, interosseous membrane calcification before the age of two, radial head dislocation around age 3.5, and hyperplastic callus formation appears before 10 years of age [47, 51]. Type I collagen N-telopeptide secretion into urine is observed only during the callus formation period [43]. Blue sclera [46], short stature [45], and bone fractures at birth may be observed as rare manifestations [46]. Furthermore, OI-VI features such as vertebra compression and scoliosis have been reported to occur in OI-V [45]. Dentinogenesis imperfecta is not observed. There is a marked diversity in the frequency of bone fractures due to bone fragility.
Radiographs from an OI-V patient. a Forearm interosseous membrane calcification. b Hyperplastic callus in femur. Reproduced with permission [15]
Mutation in the UTR of IFITM5 causes OI-V
In 2012, two groups reported the presence of a single recurrent heterozygous mutation (c.-14C>T) in the 5′ untranslated region (5′-UTR) of IFITM5 of patients with OI-V [12, 13]. Subsequently, many groups reported IFITM5 c.-14C>T mutation in patients with OI-V [15, 45, 46, 49, 52–57] and this mutation is now considered to be the cause of autosomal dominant OI-V. The IFITM5 c.-14C>T mutation shifts the IFITM5 upstream and creates a new start codon, resulting in the addition of 5 amino acids (MALEP) at the N-terminus of IFITM5 (Fig. 4a, b). The longer transcript due to this 5′-UTR mutation of IFITM5 can be detected in bone samples from patients with OI-V [58]. To date, the mutant protein IFITM5 with 5 additional amino acids (MALEP-IFITM5) has not been directly detected in bone samples from patients with OI-V [58]. However, when IFITM5 harboring the c.-14C>T mutation is expressed in HEK293 cells, a protein longer than the wild-type IFITM5 is synthesized [13].
Mutants of human IFITM5. a Wild-type IFITM5. C50, C51, and C84 are palmitoylated. b IFITM5 mutant produced by c.-14C>T mutation. Five amino acid residues (MALEP) are added at the N-terminus. Palmitoylation at C50, C51, and C84 normally occurs. c IFITM5 mutant produced by c.119C>T mutation. The 40th serine residue is substituted by a leucine residue (S40L). C50 and C51 are predicted not to be palmitoylated, resulting in localization in the endoplasmic reticulum but not the plasma membrane
The IFITM5 c.-14C>T mutation has been found in all patients with OI-V. However, the mechanism by which this mutation causes OI-V remains unclear. Ifitm5 knockout mice did not exhibit major defects in bone [11]. Furthermore, while IfitmDel −/− mice, lacking the whole Ifitm locus, did exhibit a decrease in protection against viral infections [1, 59], no gross abnormalities were observed. Two individuals with a 320- and 440-kb heterozygous genomic deletion containing IFITM5 exhibited short stature, short phalanges, microcephaly, and clinodactyly, but did not show any bone fragility or the characteristic hyperplastic callus formation observed in OI-V [13]. These facts indicate that the cause of OI-V is related to neither the loss of function nor the haploinsufficiency of IFITM5.
Recently, a mouse model of OI-V harboring the Ifitm5 c.-14C>T mutation was generated [60]. This OI-V mouse model showed a slow rate of mineralization in utero, and exhibited abnormal rib cage formation and long bone deformities and fractures (Fig. 5). Furthermore, growth plate expansion was also observed, as seen in infant patients with OI-V. Using cell culture of osteoblasts isolated from the calvaria of E18.5 OI-V mouse model embryos, Sp7, Col1a1, Bsp, and Ocn (also known as Bglap) gene expression levels were shown to be reduced compared to that of osteoblasts from wild-type mice. Moreover, the degree of mineralization was reduced. These results clearly demonstrate that the Ifitm5 c.-14C>T mutation does indeed have an effect on bone formation. On the other hand, the type I collagen of the OI-V mouse model did not show the post-translational modifications observed in other types of OI and was normal. Therefore, the decrease in mineralization rate and bone deformities observed in the OI-V mouse model is thought to be unrelated to changes in type I collagen structure. Surprisingly, the OI-V mouse model with the Ifitm5 c.-14C>T mutation exhibited perinatal lethality. This is thought to be due to respiratory failure caused by abnormal rib cage formation in neonatal mice [60]. To date, abnormal rib cage formation has not been reported in patients with OI-V. Since the OI-V mouse model exhibits perinatal lethality, whether the characteristics of OI-V such as hyperplastic callus formation and interosseous membrane calcification occur in the post-natal phase remains unknown.
Skeletal phenotype of mice with c.-14C>T mutation in Ifitm5. a Delayed bone formation in E.15.5 mutant mouse. b Bone fracture in E18.5 mutant mouse. c Abnormalities of the forelimbs, hindlimbs, and ribs. Reproduced with permission [60]
In contrast, transgenic mice overexpressing wild-type Ifitm5 showed normal growth and pre- and post-natal development, and no skeletal defects were observed (Fig. 6) [60]. Moreover, the bone morphological parameters of these transgenic mice, obtained by micro-computed tomography, did not differ from those of wild-type mice. Therefore, it is thought that the Ifitm5 c.-14C>T mutation does not cause a gain of normal function [60].
Skeletal phenotype of Ifitm5-transgenic mice. No change in skeletal phenotype is observed between wild-type and Ifitm5 transgenic mice at E15.5 (a) and E18.5 (b). Reproduced with permission [60]
Mutation of IFITM5 coding region causes OI that is similar to OI-VI, but not OI-V
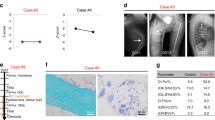
In 2014, mutations in the coding region of IFITM5 were newly identified in OI patients with more severe symptoms than patients with OI-V [14–16]. The mutation is an autosomal dominant de novo mutation (c.119C>T) and causes a serine to leucine substitution on the 40th residue (p.S40L) (Fig. 4c). Patients with this IFITM5 heterozygous mutation (IFITM5-S40L) exhibit bending of long bones [15], short stature [14, 16], bowing of extremities [14, 16], vertebral compression [14, 15], and scoliosis [16] (Fig. 7). Furthermore, patients exhibit blue sclera [15, 16], and dentinogenesis imperfecta is also observed [16]. Regarding bone histology, broad bands of unmineralized osteoid and fish-scale patterns are seen [16]. These bone histological characteristics are similar to those observed in autosomal recessive OI-VI. However, these patients do not have mutations in SERPINF1, the causative gene of OI-VI [16].
Radiographs from a postnatal OI patient with c.119C>T mutation in Ifitm5. a Intrauterine fractures of the left humerus, rib deformities, and rib fractures. b Short and bent tibia and fibula. c Vertebral compression. Reproduced with permission [14]
SERPINF1 encodes the multifunctional secretory protein, pigment epithelium-derived factor (PEDF) [61–65]. The bones of Serpinf1 knockout mice exhibit a reduction in the trabecular bone volume, similar to bone tissue in patients with OI-VI; the unmineralized osteoid is thick and there is an increase in the mineral:matrix ratio [65]. The increase in the mineral:matrix ratio is thought to be due to the reduction in type I collagen brought about by the defect in PEDF [65]. The frailty in bone may be due to the increase in this ratio and, as a consequence, an inability to maintain mineralization of the matrix.
Molecular mechanisms involved in the effect of IFITM5 mutations on the pathology of OI
The IFITM5 c.119C>T mutation causes a severe form of OI. Its pathology differs from the OI-V caused by the IFITM5 c.-14C>T mutation. Therefore, the onset of OI caused by the proteins IFITM5-S40L and MALEP-IFITM5 is believed to be due to different molecular mechanisms. IFITM5-S40L and MALEP-IFITM5 expression levels do not differ from wild-type IFITM5 [10, 16]. Thus, it is unlikely that IFITM5 expression level is related to OI pathology.
It has been reported that osteoblasts expressing IFITM5-S40L and those expressing MALEP-IFITM5 show differences in SERPINF1 expression and, accordingly, a different level of PEDF secretion [16]. In patients with OI expressing IFITM5-S40L, PEDF serum levels were normal. However, culture of isolated osteoblasts showed a low level of SERPINF1 expression during differentiation. Consequently, the level of PEDF secretion was dramatically reduced compared to wild-type osteoblasts. OI pathology caused by IFITM5-S40L presents similarities to that of OI-VI caused by SERPINF1 mutations. Thus, the reduction in type I collagen secretion and mineralization may originate from a localized reduction in PEDF from osteoblasts, which function in an autocrine fashion. Conversely, osteoblasts isolated from OI-V patients with the IFITM5 c.-14C>T mutation show a significant increase in SERPINF1 expression compared to the wild-type. As a result, the level of PEDF secretion was also increased. Exogenous PEDF is known to promote mineralization [66, 67], and thus PEDF is likely to be involved in the hyperplastic callus formation and interosseous membrane calcification observed in OI-V. Unfortunately, the OI-V mouse model exhibits perinatal lethality. Therefore, whether PEDF is involved in hyperplastic callus formation and interosseous membrane calcification after birth cannot be investigated in this mouse model. If indeed PEDF is involved in hyperplastic callus formation and interosseous membrane calcification, it means that SERPINF1 expression is regulated, both temporally and spatially, by MALEP-IFITM5. The OI-V mouse model shows a slow rate of mineralization in utero, and osteoblasts isolated from these mice present a low expression level of Col1a1 and a low mineralization level [60]. Serpinf1 expression levels in osteoblasts isolated from the OI-V mouse model have not been investigated, and currently the correlation between MALEP-IFITM5 and PEDF in this mouse model remains unknown.
The IFITM5-S40L and MALEP-IFITM5 proteins have been shown to differ in their topology and localization [10]. The murine IFITM5 p.S42L mutation, which corresponds to the human IFITM5 p.S40L mutation, is not S-palmitoylated on C52 and C53. As a result, this mutated IFITM5 protein is not transported to the cell membrane and remains in the Golgi apparatus. On the other hand, the localization, topology, and synthesis level of MALEP-IFITM5 caused by the Ifitm5 c.-14C>T mutation did not differ from wild-type IFITM5. Therefore, a scenario in which the mis-localization of IFITM5-S40L causes pathology similar to OI-VI is possible. However, its localization cannot be considered to be a cause of OI-V induced by MALEP-IFITM5.
A peptidyl-prolyl cis–trans isomerase of the FK506-binding protein (FKBP) family member, FKBP11 (also known as FKBP19), has been identified and is a partner molecule that interacts with murine IFITM5 [68]. S-Palmitoylation of IFITM5 C52 and C53 is essential for the interaction between FKBP11 and IFITM5 [69]. Moreover, the murine IFITM5-S42L does not interact with FKBP11 (unpublished data). When murine osteoblasts are cultured with 2-bromopalmitic acid, a palmitoylation inhibitor, diffused mineralization nodules, which differ from the normal mineralization nodules, are observed [69]. This strongly indicates that either the mis-localization of IFITM5, due to the failure of C52 and C53 S- palmitoylation, or the failure of interaction with FKBP11, influences OI due to IFITM5-S40L. On the other hand, murine MALEP-IFITM5 retained its interaction with FKBP11, as observed in wild-type IFITM5 (unpublished data). Mutations in FKBP65 (encoded by Fkbp10), from the same FKBP family as FKBP11, inhibit the hydroxylation of telopeptide lysyl residues, which are involved in the intermolecular cross-link formation of type I collagen and cause the autosomal recessive Bruck syndrome and OI-XI [70–73]. Autosomal recessive disorders caused by mutations in FKBP65 exhibit the following clinical phenotypes: bone fragility, congenital joint contracture, scoliosis, and osteoporosis [70]. Fkbp10 knockout mice exhibit perinatal lethality. However, the calvarial collagen from these knockout mice showed instability in their intermolecular cross-link formation of telopeptide lysines [73]. This type of inhibition of hydroxylation of type I collagen telopeptide lysyl residues is not observed in the OI-V mouse model with the Ifitm5 c.-14C>T mutation [60]. Therefore, the scenario in which MALEP-IFITM5 lowers the stability of type I collagen structure via inhibiting FKBP11 function can be excluded.
Although it appears that S-palmitoylation of IFITM5 C52 and C53 affects the function of IFITM5, S-palmitoylation is a reversible modification [74]. The peptidyl-prolyl cis–trans isomerase activity of FKBP12 has been reported to be involved in the depalmitoylation of the membrane protein H-Ras [75]. FKBP12 binds to S-palmitoylated H-Ras and depalmitoylates it by acting on proline neighboring the S-palmitoylated cysteine. The palmitoylation/depalmitoylation cycle is linked to the bidirectional trafficking of H-R between the Golgi apparatus and cell membranes [76–78]. The IFITM5 N-terminal region presents a lot of proline residues. A newly proposed topology for IFITM5 has shown that the N-terminal region is intracellular, not extracellular [10]. Since the peptidyl-prolyl cis–trans isomerase of FKBP11 is predicted to be in the extracellular region, it is unlikely that FKBP11 is involved in the depalmitoylation of IFITM5. FKBP11 also interacts with the CD81–CD9 complex, both of whose parts are S-palmitoylated [68]. CD81 and CD9 both have proline residues in their extracellular regions. Currently, it is unknown whether the interaction between IFITM5 and FKBP11 has an effect on mineralization. In contrast to Fkbp10, the causative gene of Bruck syndrome and the OI-XI, knockout mouse phenotype, Lexicon Phenotype Analysis of Fkbp11 knockout mice indicated an increase in bone mineral content and mineral density (http://www.informatics.jax.org/external/ko/lexicon/2549.html). Therefore, FKBP11 may be functioning as a negative regulator of bone function. Furthermore, osteopenia has been reported in CD81 and CD9 double knockout mice [79]. However, the mineralization capacity of bone marrow cells isolated from these double knockout mice did not exhibit any differences from those isolated from wild-type mice. Thus, it is thought that the effect of CD81 and CD9 on bone formation is only indirect [79]. Other than FKBP11, no other proteins interacting with IFITM5 have been reported. Proteins interacting with MALEP-IFITM5 have also not been reported. If proteins interacting specifically with the MALEP-IFITM5 protein can be identified, it will result in a better understanding of the function of IFITM5 and the causes of OI-V.
The complexity of OI-V molecular mechanisms
Although a clear positive correlation is observed between IFITM5 and mineralization in vitro, this relationship is not observed in vivo. Therefore, it is thought that there may be a different system for mineralization in vivo and that this is the main system. Furthermore, the fact that Ifitm5 knockout mice and Ifitm5 transgenic mice do not show major bone abnormalities indicates that, for normal bone tissue, mineralization via IFITM5 is suppressed. The hyperplastic callus formation and interosseous membrane calcification observed in OI-V may be due to removal of this suppression. Specifically, hyperplastic callus formation may be due to excess mineralization induced by the relief of IFITM5 suppression on top of the main system involved in mineralization, and interosseous membrane calcification may be due to the removal of IFITM5 suppression in locations that do not normally ossify. If this is indeed the case, in in vitro studies, where IFITM5 function is not suppressed, it will be difficult to determine whether this suppression is removed in the case of MALEP-IFITM5.
On another note, OI-V shows symptoms of bone loss and subsequent bone fragility, which contradict the other symptoms of hyperplastic callus formation and ectopic bone formation. Regarding bone fragility, major differences can be observed between patients with OI-V. Recently, in a culture of primary osteoblasts isolated from OI-V patients, it was reported that the expression level of mineralization marker genes such as ALPL, IBSP, OPN, and OCN was increased, while COL1A1 expression was significantly decreased and the structure of secreted type I collagen was also abnormal [80]. The possibility that the abnormality of type I collagen production is thought to be involved in bone fragility in OI-V, but the mechanism by which MALEP-IFITM5 affects the level and the structure of secreted type I collagen remains unknown.
Regarding OI-V caused by the IFITM5 c.-14C>T mutation, the bone formation mechanism of IFITM5 and the regulatory mechanism of IFITM5 function in vivo needs to be elucidated. For this to be achieved, the way in which MALEP-IFITM5 affects these mechanisms must be unraveled.
References
Brass AL, Huang IC, Benita Y, John SP, Krishnan MN, Feeley EM, Ryan BJ, Weyer JL, van der Weyden L, Fikrig E, Adams DJ, Xavier RJ, Farzan M, Elledge SJ (2009) The IFITM proteins mediate cellular resistance to influenza A H1N1 virus, West Nile virus, and dengue virus. Cell 139:1243–1254
Everitt AR, Clare S, Pertel T, John SP, Wash RS et al (2013) IFITM3 restricts the mobidity and mortality associated with influenza. Nature 484:519–523
Bailey CC, Huang IC, Kam C, Farzan M (2012) Ifitm3 limits the severity of acute influenza in mice. PLoS Pathog 8:e1002909
Huang IC, Bailey CC, Weyer JL, Radoshitzky SR, Becker MM, Chiang JJ, Brass AL, Ahmed AA, Chi X, Dong L, Longobardi LE, Boltz D, Kuhn JH, Elledge SJ, Bavari S, Denison MR, Choe H, Farzan M (2011) Distinct patterns of IFITM-mediated restriction of filoviruses, SARS coronavirus and influenza A virus. PLoS Pathog 7:e1001258
Moffatt P, Salois P, Gaumond MH, St-Amant N, Godin E, Lanctot C (2002) Engineered viruses to select genes encoding secreted and membrane-bound proteins in mammalian cells. Nucleic Acids Res 30:4285–4294
Hanagata N, Takemura T, Monkawa A, Ikoma T, Tanaka J (2007) Phenotype and gene expression pattern of osteoblast-like cells cultured on polystyrene and hydroxyapatite with pre-adsorbed type-I collagen. J Biomed Mater Res Part A 83A:362–371
Li K, Markosyan RM, Zheng YM, Golfetto O, Bungart B, Li M, Ding S, He Y, Liang C, Lee JC, Gratton E, Cohen FS, Liu SL (2013) IFITM proteins restrict viral membrane hemifusion. PLoS Pathog 9:e1003124
Feeley EM, Sims JS, John SP, Chin CR, Pertel T, Chen LM, Gaiha GD, Ryan BJ, Donis RO, Elledge SJ, Brass AL (2011) IFITM3 inhibits influenza A virus infection by preventing cytosolic entry. PLoS Pathog 7:e1002337
Moffatt P, Gaumond MH, Salois P, Sellin K, Beestte MC, Godin E, de Oliveira PT, Atkins GJ, Nanci A, Thomas G (2008) Bril: a novel bone-specific modulator of mineralization. J Bone Miner Res 23:1497–1508
Patoine A, Gaumond MH, Jaiswal PK, Fassier F, Rauch F, Moffatt P (2014) Topological mapping of BRIL reveals a type II orientation and effects of osteogenesis imperfect mutations on its cellular destination. J Bone Miner Res 29:2004–2016
Hanagata N, Li X, Morita H, Takemura T, Li J, Minowa T (2011) Characterization of the osteoblast-specific transmembrane protein IFITM5 and analysis of IFITM5-deficient mice. J Bone Miner Metab 29:279–290
Cho TJ, Lee KE, Lee SK, Song SJ, Kim KJ, Jeon D, Lee G, Kim HN, Lee HR, Eom HH, Lee ZH, Kim OH, Park WY, Park SS, Ikegawa S, Yoo WJ, Choi IH, Kim JW (2012) A single recurrent mutation in the 5′-UTR of IFITM5 causes osteogenesis imperfecta type V. Am J Hum Genet 91:343–348
Semler O, Garbes L, Keupp K, Swan D, Zimmermann K, Becker J, Iden S, Wirth B, Eysel P, Koerber F, Schoenau E, Bohlander SK, Wollnik B, Netzer C (2012) A mutation in the 5′-UTR of IFITM5 creates an in-frame start codon and causes autosomal-dominant osteogenesis imperfecta type V with hyperplastic callus. Am J Hum Genet 91:349–357
Koyer-Kuhn H, Semler O, Garbes L, Zimmermann K, Becker J, Wollnik B, Schoenau E, Netzer C (2014) A nonclassical IFITM5 mutation located in the coding region causes severe osteogenesis imperfect with prenatal onset. J Bone Miner Res 29:1387–1391
Guillen-Navarro E, Ballesta-Martinez MJ, Valencia M, Bueno AM, Martinez-Glez V, Lopez-Gonzalez V, Burnyte B, Utkus A, Lapunzia P, Ruiz-Perez VL (2014) Two mutations in IFITM5 causing distinct form of osteogenesis imperfect. Am J Med Genet A 164A:1136–1142
Farber CR, Reich A, Barnes AM, Becerra P, Rauch F, Cabral WA, Bae A, Quinlan A, Glorieux FH, Clemens TL, Marini JC (2014) A novel IFITM5 mutation in severe atypical osteogenesis imperfecta type VI impairs osteoblast production of pigment epithelium-derived factor. J Bone Miner Res 29:1402–1411
Marini JC, Blissett AR (2013) New genes in bone development: what’s new in osteogenesis imperfect. J Clin Endocrinol Metab 98:3095–3103
Dalgleish R (1997) The human type I collagen mutation database. Nucleic Acids Res 25:181–187
Dalgleish R (1998) The human type I collagen mutation database 1998. Nucleic Acids Res 26:253–255
Marini JC, Forlino A, Cabral WA, Barnes AM, San Antonio JD et al (2007) Consortium for osteogenesis imperfecta mutations in the helical domain of type I collagen: regions rich in lethal mutations align with collagen binding sites for integrins and proteoglycans. Hum Mutat 28:209–221
Sykes B, Francis MJ, Smith R (1977) Altered relation of two collagen types in osteogenesis inmperfecta. N Engl J Med 296:1200–1203
Trelstad RL, Rubin D, Gross J (1977) Osteogenesis imperfecta congenital: evidence for a generalized molecular disorder of collagen. Lab Invest 36:501–508
Chu ML, Williams CJ, Pepe G, Hirsch JL, Prockop DJ, Ramirez F (1983) Internal deletion in a collagen gene in a perinatal lethal form of osteogenesis imperfecta. Nature 304:78–80
Steinmann B, Rao VH, Vogel A, Bruckner P, Gitzelmann R, Byers PH (1984) Cysteine in the triple-helical domain of one allelic product of the alpha 1 (I) gene of type I collagen produces a lethal form of osteogenesis imperfecta. J Biol Chem 259:11129–11138
Cohn DH, Byers PH, Steinmann B, Gelinas RE (1986) Lethal osteogenesis imperfecta resulting from a single nucleotide change in one human pro plpha 1(I) collagen allele. Proc Natl Acad Sci USA 83:6045–6047
Sykes B, Ogilvie D, Wordsworth P, Wallis G, Mathew C, Beighton P, Nicholls A, Pope FM, Thompson E, Tsipouras P, Schwartz R, Jensson O, Arnason A, Børresen A-L, Heiberg A, Frey D, Steinman B (1990) Consistent linkage of dominantly inherited osteogenesis imperfecta to the type I collagen loci: COL1A1 and COL1A2. Am J Hum Genet 46:293–307
Morello R, Bertin TK, Chen Y, Hicks J, Tonachini L, Monticone M, Castagnola P, Rauch F, Glorieux FH, Vranka J, Bachinger HP, Pace JM, Schwarze U, Byers PH, Weis M, Fernandes RJ, Eyre DR, Yao Z, Boyce BF, Lee B (2006) CRTAP is required for prolyl 3-hydroxylation and mutations cause recessive osteogenesis imperfecta. Cell 127:291–304
Cabral WA, Barnes AM, Adeyemo A, Cushing K, Chitayat D, Porter FD, Panny SR, Gulamali-Majid F, Tishkoff SA, Rebbeck TR, Gueye SM, Bailey-Wilson JE, Brody LC, Rotimi CN, Marini JC (2012) A founder mutation in LEPRE1 carried by 1.5 % of West Africans and 0.4 % of African Americans causes lethal recessive osteogenesis imperfecta. Genet Med Off J Am Coll Med Genet 14:543–551
van Dijk FS, Nesbitt IM, Zwikstra EH, Nikkels PG, Piersma SR, Fratantoni SA, Jimenez CR, Huizer M, Morsman AC, Cobben JM, van Roij MH, Elting MW, Verbeke JI, Wijnaendts LC, Shaw NJ, Hogler W, McKeown C, Sistermans EA, Dalton A, Meijers-Heijboer H, Pals G (2009) PPIB mutations cause severe osteogenesis imperfecta. Am J Hum Genet 85:521–527
Christiansen HE, Schwarze U, Pyott SM, AlSwaid A, Al Balwi M, Alrasheed S, Pepin MG, Weis MA, Eyre DR, Byers PH (2010) Homozygosity for a missense mutation in SERPINH1, which encodes the collagen chaperone protein HSP47, results in severe recessive osteogenesis imperfecta. Am J Hum Genet 86:389–398
Alanay Y, Avaygan H, Camacho N, Utine GE, Boduroglu K et al (2010) Mutations in the gene encoding the RER protein FKBP65 cause autosomal-recessive osteogenesis imperfect. Am J Hum Genet 86:551–559
Drögemüller C, Becker D, Brunner A, Haase B, Kircher P, Seeliger F, Fehr M, Baumann U, Lindblad-Toh K, Leeb T (2009) A missense mutation in the SERPINH1 gene in dachshunds with osteogenesis imperfecta. PLoS Genet 5:e1000579
Christiansen HE, Schwarze U, Pyott SM, AlSwaid A, Balwi MA, Alrasheed S, Pepin MG, Weis MA, Eyre DR, Byers PH (2010) Homozygosity for a missense mutation in SERPINH1, which encodes the collagen chaperone protein HSP47, results in severe recessive osteogenesis imperfecta. Am J Hum Genet 86:389–398
Martínez-Glez V, Valencia M, Caparrós-Martín JA, Aglan M, Temtamy S, Tenorio J, Pulido V, Lindert U, Rohrbach M, Eyre D, Giunta C, Lapunzina P, Ruiz-Perez VL (2012) Identification of a mutation causing deficient BMP1/mTLD proteolytic activity in autosomal recessive osteogenesis imperfecta. Hum Mutat 33:343–350
Homan EP, Rauch F, Grafe I, Lietman C, Doll JA, Dawson B, Bertin T, Napierala D, Morello R, Gibbs R, White L, Miki R, Cohn DH, Crawford S, Travers R, Glorieux FH, Lee B (2011) Mutations in SERPINF1 cause osteogenesis imperfecta type VI. J Bone Miner Res 26(12):2798–2803
Becker J, Semler O, Gilissen C, Li Y, Bolz HJ, Giunta C, Bergmann C, Rohrbach M, Koerber F, Zimmermann K, de Vries P, Wirth B, Schoenau E, Wollnik B, Veltman JA, Hoischen A, Netzer C (2011) Exome sequencing identifies truncating mutations in human SERPINF1 in autosomal-recessive osteogenesis imperfecta. Am J Hum Genet 88:362–371
Lapunzina P, Aglan M, Temtamy S, Caparrós-Martín JA, Valencia M, Letón R, Martínez-Glez V, Elhossini R, Amr K, Vilaboa N, Ruiz-Perez VL (2010) Identification of a frameshift mutation in Osterix in a patient with recessive osteogenesis imperfecta. Am J Hum Genet 87:110–114
Shaheen R, Alazami AM, Alshammari MJ, Faqeih E, Alhashmi N, Mousa N, Alsinani A, Ansari S, Alzahrani F, Al-Owain M, Alzayed ZS, Alkuraya FS (2012) Study of autosomal recessive osteogenesis imperfecta in Arabia reveals a novel locus defined by TMEM38B mutation. J Med Genet 49:630–635
Volodarsky M, Markus B, Cohen I, Staretz-Chacham O, Flusser H, Landau D, Shelef I, Langer Y, Birk OS (2013) A deletion mutation in TMEM38B associated with autosomal recessive osteogenesis imperfecta. Hum Mutat 34:582–586
Keupp K, Beleggia F, Kayserili H, Staretz-Chacham O, Flusser H, Landau D, Shelef I, Langer Y, Birk OS (2013) Mutations in WNT1 cause different forms of bone fragility. Am J Hum Genet 92:565–574
Fahiminiya S, Majewski J, Mort J, Moffatt P, Glorieux FH, Rauch F (2013) Mutations in WNT1 are a cause of osteogenesis imperfecta. J Med Genet 50:345–348
Pyott SM, Tran TT, Leistritz DF, Pepin MG, Mendelsohn NJ, Temme RT, Fernandez BA, Elsayed SM, Elsobky E, Verma I, Nair S, Turner EH, Smith JD, Jarvik GP, Byers PH (2013) WNT1 mutations in families affected by moderately severe and progressive recessive osteogenesis imperfecta. Am J Hum Genet 92:590–597
Glorieux FH, Rauch F, Plotkin H, Ward L, Travers R, Roughley P, Lalic L, Glorieux DF, Fassier F, Bishop NJ (2000) Type V osteogenesis imperfecta: a new form of brittle bone disease. J Bone Miner Res 15:1650–1658
Rauch F, Glorieux FH (2004) Osteogenesis imperfecta. Lancet 363:1377–1385
Rauch F, Moffatt P, Cheung M, Roughley P, Lalic L, Lund AM, Ramirez N, Fahiminiya S, Majewski J, Glorieux FH (2013) Osteogenesis imperfecta type V: Marker pheneotypic variability despite the presence of the IFITM5 c.-14C>T mutation in all patients. J Med Genet 50:21–24
Shapiro JR, Lietman C, Grover M, Lu JT, Nagamani SC, Dawson BC, Baldridge DM, Bainbridge MN, Cohn DH, Blazo M, Roberts TT, Brennen FS, Wu Y, Gibbs RA, Melvin P, Campeau PM, Lee BH (2013) Phenotypic variability of osteogenesis imperfecta type V caused by an IFITM5 mutation. J Bone Miner Res 28:1523–1530
Cheung MS, Glorieux FH, Rauch F (2007) Natural history of hyperplastic callus formation in osteogenesis imperfecta type V. J Bone Miner Res 22:1181–1186
Zeitlin L, Rauch F, Travers R, Munns C, Glorieux FH (2006) The effect of cyclical intravenous pamidronate in children and adolescents with osteogenesis imperfecta type V. Bone 38:13–20
Fitzgerald J, Holden P, Wright H, Wilmot B, Hata A, Steiner RD, Basel D (2013) Phenotypic variability in individuals with type V osteogenesis imperfecta with identical IFITM5 mutations. J Rare Disord 1:37–42
Arundel P, Offiah A, Bishop NJ (2011) Evolution of the radiographic appearance of the metaphyses over the first year of life in type V osteogenesis imperfecta: clues to pathogenesis. J Bone Miner Res 26:894–898
Glorieux FH, Ward LM, Rauch F, Lalic L, Roughley PJ, Travers R (2002) Osteogenesis imperfecta type VI: a form of brittle bone disease with a mineralization defect. J Bone Miner Res 17:30–38
Campeau PM, Lee BH (2013) Phenotyic variability of osteogenesis imperfect type V caused by an IFITM5 mutation. J Bone Miner Res 28:1523–1530
Balasubramanian M, Parker MJ, Dalton A, Giunta C, Lindert U, Peres LC, Wagner BE, Arundel P, Offiah A, Bishop NJ (2013) Genotype-phenotype study in type V osteogenesis imperfecta. Clin Dysmorphol 22:93–101
Takagi M, Sato S, Hara K, Tani C, Miyazaki O, Nishimura G, Hasegawa T (2013) A recurrent mutation in the 5′-UTR of IFITM5 causes osteogenesis imperfecta type V. Am J Med Genet A 161A:1980–1982
Zhang Z, Li M, He JW, Fu WZ, Zhang CQ, Zhang ZL (2013) Phenotype and genotype analysis of Chinese patients with osteogenesis imperfect type V. PLoS One 8:e72337
Grover M, Campeau PM, Lietman CD, Lu JT, Gibbs RA, Schlesinger AE, Lee BH (2013) Osteogenesis imperfecta type without features of type V caused by a mutation in the IFITM5 gene. J Bone Miner Res 28:2333–2337
Kim OH, Jin DK, Kosaki K, Kim JW, Cho SY, Yoo WJ, Choi IH, Nishimura G, Ikegawa S, Cho TJ (2013) Osteogenesis imperfecta type V: Clinical and radiographic manifestations in mutation confirmed patients. Am J Med Genet A 161A:1972–1979
Lazaus S, Mclnerney-Leo AM, McKenzie FA, Baynam G, Beoley S, Cavan BV, Munns CF, Pruijs JEH, Sillence D, Terhal PA, Pryce K, Brown M, Zankl A, Thomas G, Duncan EL (2014) The IFITM5 mutation c.-14C>T results in an elongated transcript expressed in human bone; and causes varying phenotypic severity of osteogenesis imperfecta type V. BMC Musculoskelet Disord 15:107
Lange UC, Adams DJ, Lee C, Barton S, Schneider R, Bradley A, Surani A (2008) Normal germ line establishment in mice carrying a deletion of the Ifitm/Fragilis gene family cluster. Mol Cell Biol 28:4688–4696
Lietman CD, Marom R, Munivez E, Bertin TK, Jiang M-M, Chen Y, Dawson B, Weis MA, Eyre D, Lee B (2015) A transgenic mouse model of OI type V supports a neomorphic mechanism of the IFITM5 mutation. J Bone Miner Res 30:498–507
Becerra SP, Notario V (2013) The effects of PEDF on cancer biology: mechanisms of action and therapeutic potential. Nat Rev Cancer 13:258–271
Borg ML, Andrews ZB, Duh EJ, Zechner R, Meikle PJ, Watt MJ (2011) Pigment epithelium-derived factor regulates lipid metabolism via adipose triglyceride lipase. Diabetes 60:1458–1466
Dawson DW, Volpert OV, Gillis P, Crawford SE, Xu H, Benedict W, Bouck NP (1999) Pigment epithelium-derived factor: a potent inhibitor of angiogenesis. Science 285:245–248
Filleur S, Nelius T, de Riese W, Kennedy RC (2009) Characterization of PEDF: a multi-functional serpin family protein. J Cell Biol 106:769–775
Bogan R, Riddle R, Li Z, Kumar S, Nandal A, Faugere M-C, Boskey A, Crawford SE, Clemens T (2013) A mouse model for human osteogenesis imperfecta type VI. J Bone Miner Res 28:1531–1536
Gattu AK, Swenson ES, Iwakiri Y, Samuel VT, Troiano N, Berry R, Church CD, Rodeheffer MS, Carpenter TO, Chung C (2013) Determination of mesenchymal stem cell fate by pigment epithelium-derived factor (PEDF) results in increased adiposity, reduced bone mineral content. FASEB J 27:4384–4394
Li F, Song N, Tombran-Tink J, Niyibizi C (2013) Pigment epithelium derived factor enhances differentiation and mineral deposition of human mesenchymal stem cells. Stem Cell 31:2714–2723
Hanagata N, Li X (2011) Osteoblast-enriched membrane protein IFITM5 regulates the association of CD9 with an FKBP11-CD81-FPRP complex and stimulates expression of interferon-induced genes. Biochem Biophys Res Commun 409:378–384
Tsukamoto T, Li X, Morita H, Minowa T, Aizawa T, Hanagata N, Demura M (2013) Role of S-palmitoylation on IFITM5 for the interaction with FKBP11 in osteoblast cells. PLoS One 8:e75831
Kelley BP, Malfait F, Bonafe L, Baldridge D, Homan E, Symoens S, Willaert A, Elcioglu N, Maldergem LV, Verellen-Dumoulin C, Gillerot Y, Napierala D, Krakow D, Beighton P, Superti-Furga A, Paepe AD, Lee B (2011) Mutations in FKBP10 cause recessive osteogenesis imperfecta and Bruck syndrome. J Bone Miner Res 26:666–672
Schwarze U, Cundy T, Pyott SM, Christiansen HE, Hegde MR et al (2013) Mutations in FKBP10, which result in Bruck syndrome and recessive forms of osteogenesis imperfecta, inhibit the hydroxylation of telopeptide lysines in bone collagen. Hum Mol Genet 22:1–17
Steinlein O, Aichinger E, Trucks H, Sander T (2011) Mutations in FKBP10 can cause a severe form of isolated osteogenesis imperfecta. BMC Med Genet 12:152
Lietman C, Rajagopal A, Homan EP, Munivez E, Jiang M-M, Bertin TK, Chen Y, Hicks J, Weis M, Eyre D, Lee B, Krakow D (2014) Connective tissue alterations in FKBP10 −/− mice. Hum Mol Genet 23:4822–4831
Smotry JE, Linder ME (2004) Palmitoylation of intracellular signaling proteins: regulation and function. Annu Rev Biochem 73:559–587
Ahearn IM, Tsai FD, Court H, Zhou M, Jennings BC, Ahmed M, Fehrenbacher N, Linder ME, Phillip MR (2011) FKBP12 binds to acylated H-Ras and promotes depalmitoylation. Mol Cell 47:173–185
Goodwin JS, Drake KR, Rogers C, Wright L, Lippincott-Schwartz J, Phillips MR, Kenworthy AK (2005) Depalmitoylated Ras traffics to and from the Gorgi complex via a nonvesicular pathway. J Cell Biol 170:261–272
Rocks O, Peyker A, Kahms M, Verveer PJ, Koerner C, Lumbierres M, Kuhlmann J, Waldmann H, Wittinghofer A, Bastiaens PI (2005) An acylation cycle regulates localization and activity of palmitoylated Ras isoforms. Science 307:1746–1752
Rocks O, Gerauer M, Vartak N, Koch S, Huang ZP, Pechivanis M, Kuhlmann J, Brunsveld L, Chandra A, Ellinger B, Waldmann H, Bastiaens PI (2010) The palmitoylation machinery is a spatially organizing system for peripheral membrane proteins. Cell 141:458–471
Takeda Y, He P, Tachibana I, Zhou B, Miyado K, Kaneko H, Suzuki M, Minami S, Iwasaki T, Goya S, Kijima T, Kumagai T, Yoshida M, Osaki T, Komori T, Mekada E, Kawase I (2008) Double deficiency of tetraspanins CD9 and CD81 alters cell motility and protease production of macrophages and causes chronic obstructive pulmonary disease-like phenotype in mice. J Biol Chem 283:26089–26097
Reich A, Bae AS, Barnes AM, Cabral WA, Hinek A, Stimec J, Hill SC, Chitayat D, Marini JC (2015) Type V OI primary osteoblasts display increased mineralization despite decreased COL1A1 expression. J Clin Endocrinol Metab 100:E325–E332
Conflict of interest
The author has no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Hanagata, N. IFITM5 mutations and osteogenesis imperfecta. J Bone Miner Metab 34, 123–131 (2016). https://doi.org/10.1007/s00774-015-0667-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-015-0667-1