Abstract
Due to the increasing elderly population, the prevalence of osteoporotic hip fractures in Japanese patients continues to rise. It is well established that patients with either hip fracture or both symptomatic and asymptomatic morphometric vertebral compression fracture (VCF) have a poor health prognosis compared with the general population. The purpose of this study was to retrospectively investigate vertebral fracture rates among patients with hip fracture and their influence on mortality. We examined 182 cases of osteoporotic hip fracture in patients admitted to our institution between January 2009 and May 2011. The average age at the time of fracture was 85 years. Radiographs of the lumbar spine were obtained from all of the participants and the lateral spinal radiographs were examined for evidence of VCF. The patients were classified into two groups, those with VCF and those without. A VCF was identified in approximately 78 % of the patients. The mortality rate 1 year after the hip fracture was approximately 22 % and it was significantly higher in patients with VCF. Through multivariate statistics we found that VCF, post-operative complication, loss of ambulation after operation and medication for osteoporosis were statistically significant. In other words, VCF, post-operative complication and loss of ambulation were considered to be poor prognostic factors and medication for osteoporosis was likely to improve the prognosis. We concluded that the risk of mortality after hip fracture is significantly greater in patients who also have VCF compared to patients without VCF, and that medication for osteoporosis is likely to improve prognosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Due to the increasing size of the elderly population in Japan, the prevalence of patients with osteoporotic hip fractures continues to rise [1–3], while the fracture rates in European and American populations are declining [4–6]. Several investigators propose that patients with hip fracture or both symptomatic and asymptomatic morphometric vertebral compression fracture (VCF) have a poor prognosis compared with the general population [7–9]. However, a detailed investigation of the impact of VCF on mortality in Japanese patients with hip fracture has not been undertaken previously.
The city where our hospital is located had a population of approximately 38,000 in March 2009, and around 27 % of them were aged 65 years or older. This value is a little higher than that for the entire prefecture, where the elderly represent approximately 25 % of the population. This hospital is the only one in the city that provides an orthopedic service; therefore, most patients who sustain hip fracture attend our institution.
The purpose of this study was to retrospectively investigate the rates of VCF in patients with hip fracture and the influence of VCF on mortality after hip fracture by using multivariate analysis.
Materials and methods
Patients
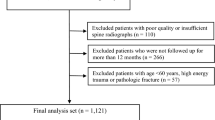
One hundred and eighty-four patients with primary hip fracture (femoral neck or trochanteric fracture) were admitted to our hospital between January 2009 and December 2011. We excluded two patients with a fracture caused by a high-energy injury (fall or traffic accident), and thus a total of 182 patients with low-trauma osteoporotic hip fracture (47 males and 135 females) participated in this study. The local hospital Institutional Research Board approved the present study and informed consent was obtained from each patient. The average age at the time of injury was 84.9 ± 7.0 years, and the range was 66–99 years. Sixty-five patients had femoral neck fracture and 117 patients had trochanteric fractures. We obtained survival and mortality data on all 182 patients from medical records and from telephone calls to the patients’ families.
Assessment of VCF and mortality data
Lumbar spine radiographs were obtained for all patients on admission. Lateral spinal radiographs were examined by two orthopedic surgeons (N.I. and T.H.) and VCFs were defined based on the criteria of The Japanese Society for Bone and Mineral Research (Fig. 1) [10]. Patients were categorized into two groups, namely those with VCF (VCF group) and those without VCF (N group). Patients were also grouped according to whether or not they had been taking anti-osteoporosis drugs before they sustained hip fracture (medication and non-medication group, respectively). We classified the patients who suffered from cardiac disease (except for hypertension), pulmonary disease, cerebrovascular disease, malignant tumor, diabetes mellitus, renal failure and others before the injury of hip fracture as having pre-operative complications, because these diseases were considered to affect mortality. We also defined those patients in whom cardiac disease, pulmonary disease, cerebrovascular disease, malignant tumor, diabetes mellitus, renal failure and others had newly occurred, or became worse, as having post-operative complications. Patients who could walk with a walker or could walk with or without crutches were classified as ambulatory. Patients who required assistance to walk were considered to have had loss of ambulation. We collected data on age, gender, presence or absence of VCF, pre- or post-operative complications, ambulatory or not before and after operation, percentage of patients taking medication for osteoporosis before hip fracture, and deaths during the 1-year study period, and subjected them to statistical analysis.
Diagnostic criteria for vertebral compression fracture (from [10])
Statistical analysis
The statistical analysis was performed using SPSS software version 18.0 (SPSS Inc, Chicago, IL, USA). We applied multivariate analysis to investigate the factors with regard to mortality such as age, gender, presence or absence of VCF, pre- or post-operative complication, ambulant or not before and after operation and on medication for osteoporosis or not. A p value of <0.05 was considered to be statistically significant.
Results
Forty out of the total of 182 patients (22.0 %) died within 1 year of hip fracture (1–11 months, average 5.1 months) (Table 1). There were 133 out of 182 patients (73.1 %) with 155 pre-operative complications: 41 with cardiac disease, 28 with pulmonary disease, 26 with cerebrovascular disease, 15 with malignant tumor, 25 with diabetes mellitus, 15 with renal failure and 5 others (4 with liver disease and 1 with dermatomyelitis). There were 47 out of 182 patients (25.8 %) with 53 post-operative complications: 13 with cardiac disease, 19 with pulmonary disease, 9 with cerebrovascular disease, 2 with malignant tumor, 5 with diabetes mellitus, 4 with renal failure, and 1 showing other complication 1 (melena). Out of 182 patients, 32 (17.6 %) were taking anti-osteoporosis drugs before they sustained hip fracture: 17 on bisphosphonates, 8 on selective androgen receptor modulators and 7 on vitamin D (alfacalcidol). All 32 patients were taking each anti-osteoporosis drug alone, and not in combination with any other anti-osteoporosis drugs.
Another finding of this analysis was that we identified VCF in 141 patients (77.5 %). The details of both VCF and N groups are shown in Table 2.
We applied multiple logistic regression to identify the factors which affected prognosis; death during the first year was adopted as a dependent variable. We found that VCF, post-operative complication, loss of ambulation after operation and medication for osteoporosis were statistically significant (Table 3).
Discussion
Factors that have been associated with increased risk of mortality after hip fracture include older age, male gender, dementia, pre-fracture gait and pre- or post-operative complications [11–14]. Mortality within a year of hip fracture has been reported to range from 11 to 35 %, which is in keeping with our findings (22.0 % mortality rate) [11, 13–15]. Lau [16] et al. reported 20 % mortality after VCF, which is similar to post-hip fracture mortality, but there is little evidence on mortality rates among patients with both hip fracture and VCF. Sakuma et al. [17] reported that from a group of 85 random hip fracture patients, 44 underwent spinal radiography, and it was found that of them 36 patients (81.4 %) had a pre-existing (prevalent) vertebral fracture, suggesting that patients with vertebral fracture have increased risk of a subsequent hip fracture. This evidence tallies with our current investigation.
We had speculated that VCF could have led to an unstable gait and reduced activity levels. Hip fracture would have led to a further decrease in physical activity and this could have precipitated complications such as pneumonia, heart failure and dementia. Consequently, the prognosis of the patients with VCF seems to be worse.
Our results show that the presence of VCF is a risk factor for mortality after hip fracture. It is important, therefore, to prevent both hip fractures and VCF. Fracture prevention requires treatment for osteoporosis. The effectiveness of anti-osteoporosis drugs is well established [18–20], but in our study only 32 out of 182 patients (17.6 %) were receiving medication. However, there was a significantly lower mortality in patients who had been on medication versus those who had not. Many patients in the Medication group had consulted our institution at the time of the onset of VCF, and had subsequently started taking osteoporosis drugs. We speculate that this would have reduced the risk of further collapse at the site of the VCF or the incidence of new fractures in other vertebrae, and helped alleviate the pain.
The current study has its limitations since only Japanese patients were included. The data may be typical of elderly Asian people but they may differ significantly from Caucasian or other populations in relation to factors such as bone density, the incidence of hip or vertebral fracture, and the age at the time of fracture. On the other hand, the strength of our study is that we are confident that our assessment of mortality is accurate because we were able to collect data for all participating patients.
The number of patients with hip fragility fractures is still increasing [1, 3] and, since bone density decreases with age, it is imperative to offer early treatment with anti-osteoporosis drugs to reduce fracture risk. Preventive treatment should therefore be more widely available to elderly patients with osteoporosis.
Conclusions
Vertebral compression fracture was observed in 77.5 % of patients with hip fracture. Among patients with hip fracture, those who also had a VCF had significantly increased risk of mortality compared to patients without VCF and medication for osteoporosis is likely to improve prognosis. Moreover, post-operative complication and loss of ambulation were likely to more frequently occur in patients with VCF; consequently, the prognosis of patients with VCF seems to be worse.
References
Morita Y, Endo N, Iga T, Kunihiko T, Ohkawa Y (2002) The incidence of cervical and trochanteric fractures of the proximal femur in 1999 in Niigata Prefecture, Japan. J Bone Miner Metab 20:311–318
Orimo H, Yaegashi Y, Onoda T, Yasumasa F, Hosoi T, Sakata K (2009) Hip fracture incidence in Japan: estimates of new patients in 2007 and 20-year trends. Arch Osteoporos 4:71–77
Hagino H, Furukawa K, Fujiwara S, Okano T, Katagiri H, Yamamoto K, Teshima R (2009) Recent trends in the incidence and lifetime risk of hip fracture in Tottori, Japan. Osteoporos Int 20:543–548
Chevally T, Guilley E, Herrmann FR, Hoffmeyer P, Rapin CH, Rizzoli R (2007) Incidence of hip fracture over a 10-year period (1991–2000): reversal of a secular trend. Bone 40:1284–1289
Jaglal S (2006) Falling hip fracture rates. J Bone Miner Res 21:1098
Kannus P, Niemi S, Parkkari J, Palvanen M, Vuori I, Järivinen M (2006) Nationwide decline in incidence of hip fracture. J Bone Miner Res 21:1836–1838
Johnell O, Kanis JA, Odén A, Sernbo L, Redlund-Johnell C, Petterson C, Laet C, Jönsson B (2004) Mortality after osteoporotic fractures. Osteoporos Int 15:38–42
Bliuc D, Nguyen D, Milch VE, Nguyen TV, Eisman JA, Center JR (2009) Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA 301:513–521
Ioannidis G, Papaioannou A, Hopman WN, Akhtar-Danesh N, Anastassiades T, Pickard L, Kennedy CC, Prior JC, Olszynski WP, Davison KS, Goltzman D, Thabane L, Gafni A, Papadimitropoulos EA, Brown JP, Josse RG, Hanley DA, Adachi JD (2009) Relation between fractures and mortality: results from the Canadian multicentre osteoporosis study. CMAJ 181:265–271
Orimo H, Hayashi Y, Fukunaga M, Sone T, Fujiwara S, Shiraki M, Kushida K, Miyamoto S, Soen S, Nishimura J, Ohashi Y, Hosoi T, Gomi I, Takana H, Ikai T, Kishimoto H (2001) Gempatsusei kotusosyousyou no sindan kijun 2000 nendo kaitei ban. Nihon Kotsutaisya Gakkai Zasshi 14:76–82 (in Japanese)
Chirodian N, Arch B, Parker MJ (2005) Sliding hip screw fixation of trochanteric hip fractures: outcome of 1024 procedures. Injury 36:793–800
McLeod K, Brodie MP, Fahey PP, Gray RA (2005) Long-term survival of surgically treated hip fracture in an Australian regional hospital. Anaesth Intensive Care 33:749–755
Petersen MB, Jørgensen HL, Hansen K, Duus BR (2006) Factors affecting post-operative mortality of patients with displaced femoral neck fracture. Injury 37:705–711
Alarcón T, González-Montalvo JI, Bárcena A, Saez P (2001) Further experience of nonagenarians with hip fractures. Injury 32:555–558
Sakamoto K, Nakamura T, Hagino H, Endo N, Mori S, Muto Y, Harad A, Yamamoto S, Tomita K, Yoshimura M, Yamamoto H (2006) Report on the Japanese Orthopaedic Association’s 3-year project observing hip fractures at fixed-point hospitals. J Orthop Sci 11:127–134
Lau E, Ong K, Kurtz S, Schmier J, Edidin A (2008) Mortality following the diagnosis of vertebral compression fracture in the Medicare population. J Bone Joint Surg 90:1479–1486
Sakuma M, Endo N, Oinuma T, Endo E, Yazawa T, Watanabe K, Watanabe S (2008) Incidence and outcome of osteoporotic fractures in 2004 in Sado City, Niigata Prefecture, Japan. J Bone Miner Metab 26:373–378
Boonen S, Lips P, Bouillon R, Bischoff-Ferrari A, Vanderschueren D, Haentjens P (2007) Need for additional calcium to reduce the risk of hip fracture with vitamin D supplementation: evidence from a comparative metaanalysis of randomized controlled trials. J Clin Endocrinol Metab 92:1415–1423
Papapoulos SE, Quandt SA, Liberman UA, Hochberg MC, Thompson DE (2005) Meta-analysis of the efficacy of alendronate for the prevention of hip fractures in postmenopausal women. Osteoporos Int 16:468–474
Lyles KW, Colón-Emeric CS, Magaziner JS, Adachi JD, Pieper CF, Mautalen C, Hyldstrup L, Recknor C, Nordsletten L, Moore KA, Lavecchia C, Zhang J, Mesenbrink P, Hodgson PK, Abrams K, Orloff JJ, Horowitz Z, Eriksen EF, Boonen S (2007) Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med 357:1799–1809
Acknowledgments
We thank Dr. Yugo Shobugawa (Division of International Health, Niigata University, Graduated School of Medical and Dental Science) for his assistance in statistical analyses.
Conflict of interest
The authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Imai, N., Endo, N., Hoshino, T. et al. Mortality after hip fracture with vertebral compression fracture is poor. J Bone Miner Metab 34, 51–54 (2016). https://doi.org/10.1007/s00774-014-0640-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-014-0640-4