Abstract
In light of the differences in hip fracture rates between men and women of different ages, age-related changes in bone structure that lead to bone fragility might differ depending on both age and gender. To investigate age-related bone loss and geometric deterioration of the femur, hip scans of 1,504 men and 2,076 women aged 19–92 years acquired during the Fourth Korean National Health and Nutrition Examination Survey (KNHANES IV) using dual-energy X-ray absorptiometry (DXA) were analyzed with a structural analysis program. Cross-sectional area and cortical thickness with bone mineral density in men started to decline from the third decade and continued to decline at a constant rate. However, in women, these parameters remained nearly constant until the fifth decade and then declined at a more rapid rate than that seen in men. Consequently, changes in the buckling ratio, earlier onset, and continuation of increase over the lifetime were observed in men. A relatively later onset with a greater acceleration with aging was observed in women. Taken together, there were obvious gender and age differences in structural trends with age. Bone aging, i.e., bone loss and geometric deterioration, actually begins at a young age, especially in men, and osteoporosis prevention strategies should target not only the elderly but also younger individuals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bone, a representative aging organ in humans, deteriorates both quantitatively and qualitatively with aging [1]. Therefore, osteoporosis represents a major health concern in aging societies, with fragility fractures having the highest impact on quality of life and medical expense [2, 3].
Bone strength reflects the integration of two main features: bone mineral density (BMD) and bone quality [4]. BMD is a well-known major predictor of fracture risk, and the pattern of declining hip BMD with age is well documented in numerous previous studies [5, 6]. However, loss of bone density caused by aging alone cannot fully explain the increase in bone fragility observed in the elderly. Bone geometry, the spatial distribution of bone, is a main component of bone quality. Therefore, the bone geometry also plays an important role in determining bone strength and risk of fracture [7]. Although bone geometry is very important for determining bone strength, most aging studies have only investigated the loss of BMD; information regarding the structural basis of bone loss is lacking, especially in East Asians.
Conventional theories state that peak BMD is attained at the end of the second or third decade of life and is followed by a prolonged plateau phase. It has long been held that bone loss begins during menopause in women and later in life in men [8]. Based on this concept, bone loss would begin during middle age, with presumably negligible bone loss during the younger years. However, two recent papers revealed that this might not be true and that bone loss begins at a younger age instead of in middle age, especially in men [9, 10]. In development of public health policy for prevention or treatment of osteoporosis, exact information on not only quantitative and but also qualitative changes of bone throughout all age groups should be important. However, little has been published about the progression of bone loss and geometric changes during young adulthood or on the differences in those changes between men and women [9].
Current interventions for osteoporosis are directed only at bone loss occurring in the later years of life. Therefore, it is important to clarify the age at which bone loss begins and when it accelerates so that interventions designed to prevent bone deterioration can be appropriately targeted for optimal effects.
The purpose of this study was to define the age-related trends of bone geometry with BMD across the entire adult lifespan and to investigate the gender differences of those changes. We further performed a correlation analysis to determine which parameters were associated with femoral geometry.
Materials and methods
Study sample and data sources
Bone mineral data were acquired for this study as a part of the Fourth Korean National Health and Nutrition Examination Survey (KNHANES IV). The KNHANES has been conducted periodically since 1998 by the Division of Chronic Disease Surveillance of the Korea Centers for Disease Control and Prevention to assess the health and nutritional status of the civilian, non-institutionalized population of Korea. The KNHANES IV was a cross-sectional and nationally representative survey conducted in 2007–2008. A stratified, multistage probability sampling design was used for the selection of household units. All men and nonpregnant women aged 19 years and older who received physical examinations in the mobile centers were eligible for bone densitometry analysis unless they had previously fractured both hips. Subjects with any pathological disorders (such as cancer, hyperthyroidism, malabsorption, renal failure, or hepatic failure) or using medications (such as corticosteroids, heparin, or anticonvulsants) known to alter calcium and bone metabolism were excluded from the analysis. Subjects who used antiresorptive agents such as raloxifene, bisphosphonate, or hormone replacement therapies were also excluded. Among those who participated in the survey, acceptable bone mineral measurements were obtained from a total of 3,580 men and women between the ages of 19 and 92 years, including 7 hip fracture participants. To investigate age trends of BMD and femoral geometry, participants were classified into seven groups by 10-year age intervals. We included 3 participants who were 19 years old in a 19–29 years group and 3 participants who were 90–92 years old in an 80–92 years group. The left hip was scanned unless there was a history of previous fracture or surgery.
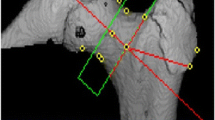
Bone densitometry, anthropometric parameters, and hip structural analysis
The femur neck was scanned at the left hip in the posteroanterior projection using dual X-ray absorptiometry (DXA) (QDR4500A; Hologic, Bedford, MA, USA) equipment located in mobile examination centers according to manufacturer protocol. All scans were further analyzed for geometric bone structure properties using the hip structure analysis (HSA) program included in APEX software of Hologic, as previously described [11, 12]. The HSA program automatically set the region of interest (ROI), defined as the narrow neck (NN), transversing the narrowest width of the femoral neck. In addition to hip axis length (HAL, mm), femur neck width (FNW, cm), and neck shaft angle (NSA, degree), the HSA program yielded data for cross-sectional area (CSA, cm2), cross-sectional moment of inertia (CSMI, cm4), mean cortical thickness (CT, cm), section modulus (SM, cm3), and buckling ratio (BR) at NN. Short-term coefficient of variance (CV) of HSA indices, calculated from the same images used for the precision assessment of BMD, appeared to be slightly greater than those of conventional BMD, but were approximately 2 %, which seemed to be similar to previously reported precision data [13, 14]. Whole-body DXA was also acquired and analyzed using Hologic Discovery software version 12.1 in its default configuration. DXA calibrations were applied as previously described [15].
Data analysis
All statistical analyses were conducted using the Statistical Package for the Social Sciences (PASW statistics) software (version 18; SPSS, Chicago, IL, USA). Data are represented as mean ± standard deviation (SD). To investigate age trends of BMD and femoral geometry, data were analyzed using a one-way analysis of variance (ANOVA) with Tukey’s post hoc analysis. Pearson’s correlation coefficients were calculated to explore relationships between femoral geometry and other anthropometric parameters.
Results
Subjects ranged in age from 19 to 92 years and included 1,504 men and 2,076 women. The sample size in each age and gender category ranged from 164 to 405 subjects, except for those older than 80 years (Table 1).
Age trends of BMD and geometry
For assessing age-related changes in BMD and geometry, the mean values of the 20-year-old group (i.e., 19–29 years) were used as the referents.
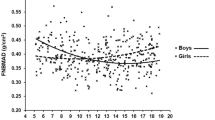
For BMD, men showed early significant bone loss before midlife (Fig. 1A). Compared to the reference age group, BMD in the 30–39 years age group already had significantly lower values (−7.8 %, p < 0.001). From the third decade, significant loss in BMD continued across all groups. However, in women, BMD loss began in the fifth decade and continued over the rest of the lifetime, accelerating during the postmenopausal period. Before the seventh decade, the mean percentage changes from the reference group in each decade were greater in men than they were in women (−7.80 % vs. −1.98 % in the fourth decade; −12.16 % vs. −2.81 % in the fifth decade; −15.57 % vs. −10.13 % in the sixth decade; p < 0.001 for all). However, from the eighth decade and onward, women showed steeper changes from the reference values than did men (−26.32 % vs. −28.91 % in the eighth decade, p < 0.05; −28.13 % vs. −37.58 % in the ninth decade, p < 0.001). Consequently, 71.87 % of the reference value for men and only 62.42 % for women remained in the oldest group. The essential trends of CSA were coincident with BMD changes in both genders (Fig. 1B).
Age trends in bone mineral density (BMD) (A) and cross-sectional area (CSA) (B) at the femur neck. a Trends for men. b Trends for women. a’ p < 0.05, a’’ p < 0.01, a’’’ p < 0.001 compared with the reference group (19–29 years of age); b’ p < 0.05, b’’ p < 0.01, b’’’ p < 0.001 compared with the previous age group. c Mean percentage changes from the mean values of the reference group (19–29 years of age) in each age group. a’ p < 0.05, a’’ p < 0.01, a’’’ p < 0.001, men compared with women. BMD bone mineral density, CSA cross-sectional area
Mean values of cortical thickness (A) and width (FNW) (B) at the femur neck in men (a) and women (b) are shown in Fig. 2. Age trends of cortical thickness were similar for BMD and CSA in men, in whom significant loss (−8.41 %, p < 0.001) of cortical thickness was already noted in the fourth decade; significant loss continued to be shown in all decades thereafter. However, in women, no significant difference was observed in the 30–39 years age group compared to that of the reference decade. In women, statistically significant cortical thinning began in the fifth decade, with a relatively constant subsequent rate of loss thereafter. Before the seventh decade, the amount of decrease was also much greater in men than in women (−8.41 % vs. −2.15 % in the fourth decade; −13.08 % vs. −2.68 % in the fifth decade; and −16.35 % vs. −10.75 % in the sixth decade; p < 0.001 for all). However, by the eighth decade, the rate of decline in the cortical thickness in women was steeper than that seen in men (−27.57 % vs. −30.64 % in the eighth decade, p < 0.05; −29.43 % vs. −39.24 % in the ninth decade, p < 0.001). In the patterns of FNW according to age, we observed more changes in women and fewer changes in men. Significantly higher values of FNW compared to the reference value were observed only in the fifth (+2.01 %, p < 0.05), sixth (+1.84 %, p < 0.05), and seventh decades (+1.87 %, p < 0.05) for men, but there were no significant differences in any other decade-to-decade comparisons. However, in women, the mean values of FNW in all other decade groups were higher than that of the reference decade, and the degrees of increase were larger than those seen in men. Nonetheless, no other additional, significant changes occurred in women after the fourth decade. Consequently, the significant widening of FNW across entire decades was 2.7 fold larger in women than it was in men (+1.87 % vs. +4.94 %, p < 0.05).
Age trends in cortical thickness (A) and width (B) at the femur neck. a Trends for men. b Trends for women. a′ p < 0.05, a′′ p < 0.01, a′′′ p < 0.001 compared with the reference group (19–29 years of age); b′ p < 0.05, b′′ p < 0.01, b′′′ p < 0.001 compared with the previous age group. c Mean percentage changes from the mean values of the reference group (19–29 years of age) in each age group. a′ p < 0.05, a′′ p < 0.01, a′′′ p < 0.001, men compared with women
Trends of the femur strength marker, cross-sectional moment of inertia (CSMI) (A), section modulus (B), and BR (C) at the femur neck in both genders along with the mean percentage changes from the reference values (c), are provided in Fig. 3. Until the fifth decade, there were no significant changes of CSMI in men. Statistically significant decreases occurred thereafter, with acceleration observed for men in their eighth decade. However, in women, the mean value in the fifth decade was 8.46 % higher than the reference value, and a significant decrease began thereafter, reaching a value 26.46 % lower than that of the reference in the oldest group. The mean percentage decreases from the reference group in the sixth and seventh decade were larger in men, and these decreases were greater in women only for those in their ninth decade (−8.01 % vs. +2.66 % in the sixth decade, p < 0.001; −10.95 % vs. −7.06 % in the seventh decade, p < 0.01; and −19.64 % vs. −26.46 % in the ninth decade, p < 0.01).
Age trends in cross-sectional moment of inertia (CSMI) (A), section modulus (B), and buckling ratio (BR) (C) at the femur neck. a Trends for men. b Trends for women. a′ p < 0.05, a′′ p < 0.01, a′′′ p < 0.001 compared with the reference group (19–29 years of age); b′ p < 0.05, b′′ p < 0.01, b′′′ p < 0.001 compared with the previous age group. c Mean percentage changes from the mean values of the reference group (19–29 years of age) in each age group. a′ p < 0.05, a′′ p < 0.01, a′′′ p < 0.001, men compared with women
For trends of section modulus, there were greater reductions with age in both genders, but the patterns differed between them. Essentially, the entire decline in neck section modulus of women occurred at the sixth decade and beyond; paradoxically, a more apparent decline occurred before this age in male participants. In age trends of BR at the femur neck, we observed significant changes across all decade groups, but the patterns were quite different according to gender. BR in men already showed apparent increases starting at the fourth decade, with consistently slow rates across all decades. However, in women, no significant increase was observed until the fourth decade, with steeper increases occurring thereafter. As a result, BRs in the oldest groups increased by 51.91 % in men and by 94.93 % in women compared to the reference values. In age trends with HAL and NSA, we did not observe any significant changes according to age group (data not shown).
Relationships between geometric properties and other clinical parameters
BMD, CSA, cortical thickness, CSMI, and section modulus of the femur neck were negatively correlated with both leg fat mass and leg fat percentage but were positively correlated with lean leg mass (p < 0.001 for all correlations). However, for BR, only a negative correlation with lean leg mass was observed (p < 0.05). These correlations were similarly observed in analysis with whole-body composition (Table 2).
Discussion
In this study, we observed an apparent decline in bone geometry parameters and bending stress with BMD according to aging. These trends differed significantly between two genders; in addition, it was observed that the structural deterioration of bone begins at a young age, especially in men.
Almost all studies on age-related changes in bone have been limited to the observation of BMD. Considering the importance of geometry on bone strength, BMD loss may not be sufficient to demonstrate age-related skeletal deterioration. Therefore, understanding the exact patterns, the timing of bone loss, and the changes of geometry in both genders may be important for the proper design of prevention and interventions for osteoporosis.
We observed significant gender differences by tracking the changes in geometry, BMD, and markers of bone rigidity according to aging. In contrast to the generally known concept of bone loss, we were able to observe an earlier bone loss in young men before midlife. However, in women, a modest decline started at the perimenopausal period and was accompanied by a subsequent rapid loss during the postmenopausal period. Bone loss occurred more rapidly in men than in women before midlife, but this tendency was reversed after midlife. Overall, an earlier onset of bone loss and a consistent loss after the third decade were observed in men, but a relatively stable bone loss until midlife and a steep loss from perimenopause were observed in women. These gender patterns of our ethnic group were different from those of subjects of European descent, but were very similar to those reported in Mexican-Americans [5]. Although several studies have reported, using QCT, that cortical bone remains relatively stable in young adult life, our observations showed that cortical thinning also started before midlife, especially in men [16]. However, DXA is not a primary tool to distinguish between trabecular and cortical bone, so we were unable to confirm whether these differences result from real ethnic characteristics or from limitations of the assessment tool.
Sexual hormones, especially estrogen and testosterone, are the main regulators of bone metabolism, and the sexual hormone changes associated with aging show very similar trends to those of the structural changes in bone of both sexes [17]. Moreover, other hormonal factors such as insulin-like growth factor (IGF)-1 and physical activity, both of which are well-known regulators of bone metabolism, could be the cause of these earlier changes in men [18]. In addition, aging per se should be considered because bone loss begins as early as the third decade of life in both men and women [9]. Meanwhile, genetic influence on bone loss is just one area of interest that has recently begun to receive much attention [19].
Periosteal widening was commonly believed to be a compensatory mechanism to endocortical resorption caused by estrogen deficiency [20]. However, significant increases in FNW already occurred in young age groups of both genders, even in the premenopausal period in women, and these findings were similar to recently reported Japanese data [13] Szulc et al. [21] also reported that periosteal apposition decreased after menopause and that bone fragility in the elderly was a consequence of reduced periosteal bone formation. Specifically, they proposed that periosteal apposition is a compensatory mechanism for bone loss with aging after achievement of peak bone mass, but that it is not correlated to nor amplified by estrogen loss in this study. Meanwhile, regarding the other geometric parameters, we saw no significant changes with aging for either NSA or HAL, likely because the most important determinant of HAL and NSA is not age related but genetic [22]. The other factor for determining NSA is the amount of physical activity on the hip during development [22]. Therefore, these two parameters do not reflect major age-related deteriorative changes in bone.
Recently, Zebaze et al. [23] published a cross-sectional study describing the importance of increased cortical porosity and subsequent cortical bone loss in aging bone. However, measurement of only BMD could not adequately capture this important deterioration in cortical bone. Furthermore, we recently reported that there was some discrepancy between absolute femoral BMD and cortical thickness in a considerable proportion of patients [24]. Therefore, DXA, the gold standard for the diagnosis of osteoporosis, which still has limitations in differentiating cortical and trabecular bone, could give secondhand information on cortical bone loss and the architecture change with aging.
From epidemiological studies, higher body weight and BMI are the protective determinants of bone mass, whereas thinness is a major risk factor for low bone mass [25, 26]. However, recent animal studies have reported contradictory findings about the relationship between fat and bone, which implies not only a direct mechanical effect but also other indirect effects of fat on bone [27]. Our findings also demonstrate that fat mass is inversely associated with bone strength indices, whereas lean mass has positive influences on these parameters. Fat mass negatively affects bone, outweighing the positive effects of weight-bearing itself. Possible explanations include a shared common origin or oxidative stress from pathological fat cells [28, 29]. Moreover, positive associations with lean mass corroborate the previously described mechanostat theory, which states that bone geometry adapts mainly to the dynamic load imposed by muscle force [30].
Our study has several limitations. First, the geometries of the femur were calculated based on two-dimensional DXA images under several assumptions. We used simple models of the femoral neck with measured dimensions to estimate CSA and mean cortical thickness. These indices were estimated based on anatomical models of the femur neck and therefore were relatively crude. This fact might compromise the accuracy of these HSA indices [31]. Second, our study was a cross-sectional study and not a longitudinal study. Therefore, our aging trends are only estimates, not observed changes. Finally, our study samples were limited to a population of 19 years of age and older. We had no pubertal and pre-pubertal participants, so we were unable to assess the changes of bone in these younger age groups.
Taken together, we showed apparent declines in bone geometry and bending stress with age, and these structural trends differed significantly according to gender and age. Based on our analysis of the relationships between geometry and body composition, we found a favorable effect of lean mass on bone geometry and bone strength and an opposite effect of fat mass. In conclusion, in contrast to prevailing concepts, bone aging—bone loss and geometric deterioration—begins at a young age, especially in men. Therefore, we should target not only the elderly population but also those of younger ages for the proper prevention of osteoporosis. Intervention for changes of body composition in a favorable direction could be considered as a preventive or therapeutic option for increasing bone strength in young adults who are at high risk for osteoporosis.
References
Seeman E, Delmas PD (2006) Bone quality–the material and structural basis of bone strength and fragility. N Engl J Med 354:2250–2261
Cummings SR, Melton LJ (2002) Epidemiology and outcomes of osteoporotic fractures. Lancet 359:1761–1767
Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA (1999) Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet 353:878–882
Klibanski A, Adams-Campbell L, Bassford T, Blair SN, Boden SD, Dickersin K, Gifford DR, Glasse L, Goldring SR, Hruska K, Johnson SR, McCauley LK, Russell WE (2001) Osteoporosis prevention, diagnosis, and therapy. J Am Med Assoc 285:785–795
Looker AC, Wahner HW, Dunn WL, Calvo MS, Harris TB, Heyse SP, Johnston CC Jr, Lindsay RL (1995) Proximal femur bone mineral levels of US adults. Osteoporos Int 5:389–409
Wu XP, Liao EY, Huang G, Dai RC, Zhang H (2003) A comparison study of the reference curves of bone mineral density at different skeletal sites in native Chinese, Japanese, and American Caucasian women. Calcif Tissue Int 73:122–132
Riggs BL, Melton LJ 3rd, Robb RA, Camp JJ, Atkinson EJ, Oberg AL, Rouleau PA, McCollough CH, Khosla S, Bouxsein ML (2006) Population-based analysis of the relationship of whole bone strength indices and fall-related loads to age- and sex-specific patterns of hip and wrist fractures. J Bone Miner Res 21:315–323
Seeman E (2002) Pathogenesis of bone fragility in women and men. Lancet 359:1841–1850
Riggs BL, Melton LJ, Robb RA, Camp JJ, Atkinson EJ, McDaniel L, Amin S, Rouleau PA, Khosla S (2008) A population-based assessment of rates of bone loss at multiple skeletal sites: evidence for substantial trabecular bone loss in young adult women and men. J Bone Miner Res 23:205–214
Orwoll ES, Oviatt SK, McClung MR, Deftos LJ, Sexton G (1990) The rate of bone mineral loss in normal men and the effects of calcium and cholecalciferol supplementation. Ann Intern Med 112:29–34
Uusi-Rasi K, Semanick LM, Zanchetta JR, Bogado CE, Eriksen EF, Sato M, Beck TJ (2005) Effects of teriparatide [rhPTH (1-34)] treatment on structural geometry of the proximal femur in elderly osteoporotic women. Bone (NY) 36:948–958
Beck TJ, Looker AC, Ruff CB, Sievanen H, Wahner HW (2000) Structural trends in the aging femoral neck and proximal shaft: analysis of the Third National Health and Nutrition Examination Survey dual-energy X-ray absorptiometry data. J Bone Miner Res 15:2297–2304
Iki M, DongMei N, Tamaki J, Sato Y, Kagamimori S, Kagawa Y, Yoneshima H (2011) Age-specific reference values of hip geometric indices from a representative sample of the Japanese female population: Japanese Population-based Osteoporosis (JPOS) Study. Osteoporos Int 22:1987–1996
Khoo BC, Beck TJ, Qiao QH, Parakh P, Semanick L, Prince RL, Singer KP, Price RI (2005) In vivo short-term precision of hip structure analysis variables in comparison with bone mineral density using paired dual-energy X-ray absorptiometry scans from multi-center clinical trials. Bone (NY) 37:112–121
Hong S, Oh HJ, Choi H, Kim JG, Lim SK, Kim EK, Pyo EY, Oh K, Kim YT, Wilson K, Choi WH (2011) Characteristics of body fat, body fat percentage and other body composition for Koreans from KNHANES IV. J Korean Med Sci 26:1599–1605
Riggs BL, Melton LJ III, Robb RA, Camp JJ, Atkinson EJ, Peterson JM, Rouleau PA, McCollough CH, Bouxsein ML, Khosla S (2004) Population-based study of age and sex differences in bone volumetric density, size, geometry, and structure at different skeletal sites. J Bone Miner Res 19:1945–1954
Khosla S, Melton LJ, Atkinson EJ, O’Fallon WM, Klee GG, Riggs BL (1998) Relationship of serum sex steroid levels and bone turnover markers with bone mineral density in men and women: a key role for bioavailable estrogen. J Clin Endocrinol Metab 83:2266–2274
Leifke E, Gorenoi V, Wichers C, Von Zur MA, Von Buren E, Brabant G (2000) Age-related changes of serum sex hormones, insulin-like growth factor-1 and sex-hormone binding globulin levels in men: cross-sectional data from a healthy male cohort. Clin Endocrinol (Oxf) 53:689–695
Rivadeneira F, Styrkarsdottir U, Estrada K, Halldorsson BV, Hsu YH et al (2009) Twenty bone-mineral-density loci identified by large-scale meta-analysis of genome-wide association studies. Nat Genet 41:1199–1206
Ahlborg HG, Johnell O, Turner CH, Rannevik G, Karlsson MK (2003) Bone loss and bone size after menopause. N Engl J Med 349:327–334
Szulc P, Seeman E, Duboeuf F, Sornay-Rendu E, Delmas PD (2006) Bone fragility: failure of periosteal apposition to compensate for increased endocortical resorption in postmenopausal women. J Bone Miner Res 21:1856–1863
Anderson JY, Trinkaus E (1998) Patterns of sexual, bilateral and interpopulational variation in human femoral neck-shaft angles. J Anat 192:279–285
Zebaze RM, Ghasem-Zadeh A, Bohte A, Iuliano-Burns S, Mirams M, Price RI, Mackie EJ, Seeman E (2010) Intracortical remodelling and porosity in the distal radius and post-mortem femurs of women: a cross-sectional study. Lancet 375:1729–1736
Kim KM, Brown JK, Kim KJ, Choi HS, Kim HN, Rhee Y, Lim SK (2011) Differences in femoral neck geometry associated with age and ethnicity. Osteoporos Int 22:2165–2174
De Laet C, Kanis JA, Oden A, Johanson H, Johnell O, Delmas P, Eisman JA, Kroger H, Fujiwara S, Garnero P, McCloskey EV, Mellstrom D, Melton LJ 3rd, Meunier PJ, Pols HA, Reeve J, Silman A, Tenenhouse A (2005) Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos Int 16:1330–1338
Nguyen TV, Sambrook PN, Eisman JA (1998) Bone loss, physical activity, and weight change in elderly women: the Dubbo Osteoporosis Epidemiology Study. J Bone Miner Res 13:1458–1467
Parhami F, Jackson SM, Tintut Y, Le V, Balucan JP, Territo M, Demer LL (1999) Atherogenic diet and minimally oxidized low density lipoprotein inhibit osteogenic and promote adipogenic differentiation of marrow stromal cells. J Bone Miner Res 14:2067–2078
Almeida M, Ambrogini E, Han L, Manolagas SC, Jilka RL (2009) Increased lipid oxidation causes oxidative stress, increased peroxisome proliferator-activated receptor-gamma expression, and diminished pro-osteogenic Wnt signaling in the skeleton. J Biol Chem 284:27438–27448
Takada I, Kouzmenko AP, Kato S (2009) Wnt and PPARgamma signaling in osteoblastogenesis and adipogenesis. Nat Rev Rheumatol 5:442–447
Lanyon LE, Rubin CT (1984) Static vs dynamic loads as an influence on bone remodelling. J Biomech 17:897–905
Khoo BC, Brown K, Zhu K, Pollock M, Wilson KE, Price RI, Prince RL (2012) Differences in structural geometrical outcomes at the neck of the proximal femur using two-dimensional DXA-derived projection (APEX) and three-dimensional QCT-derived (BIT QCT) techniques. Osteoporos Int 23:1393–1398
Acknowledgments
This work was supported by the National Research Foundation of Korea (NRF) Grant funded by the Korea government (MEST) (No. 20110001024). We also express our heartfelt thanks to the Korean Osteoporosis Society.
Conflict of interest
The authors disclose that they have no conflicting interests in this work.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Kim, K.M., Lim, J.S., Kim, K.J. et al. Dissimilarity of femur aging in men and women from a Nationwide Survey in Korea (KNHANES IV). J Bone Miner Metab 31, 144–152 (2013). https://doi.org/10.1007/s00774-012-0386-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-012-0386-9