Abstract
Multiple myeloma (MM) cell adhesion to stromal cells via very late antigen (VLA)-4 and vascular cell adhesion molecule (VCAM)-1 interaction causes enhanced secretion of osteoclastogenic activity by MM cells. We have reported that MM cell-derived macrophage inflammatory protein (MIP)-1α and MIP-1β are responsible for most of the osteoclastogenic activity in MM. Thus, adhesion-mediated osteoclastogenesis may be caused by enhanced production of MIP-1 via VLA-4–VCAM-1 interaction. The present study was undertaken to clarify whether MM cell-derived MIP-1 plays a role in VLA-4–VCAM-1 adhesion-mediated osteoclastogenesis. Adhesion of MM cells to VCAM-1 upregulated MIP-1α and MIP-1β production from MM cells and enhanced production of osteoclastogenic activity by MM cells. Blockade of MIP-1α and MIP-1β actions not only abrogated elaboration of osteoclastogenic activity, but also suppressed spontaneous MM cell adhesion to VCAM-1. These results demonstrate that MM cell adhesion to VCAM-1 upregulates MIP-1 production by MM cells to cause enhancement of osteoclastogenesis. In addition, the results suggest that the increased production of MIP-1 further enhances MM cell binding to stromal cells via stimulation of VLA-4–VCAM-1 adhesion, forming a “vicious cycle” between MM cell adhesion to stromal cells and MIP-1 production via VLA-4–VCAM-1 interaction.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple myeloma (MM) almost exclusively develops and expands in the bone marrow, generating devastating bone destruction by osteoclasts (OCs). Choi et al. [1] reported that an osteoclastogenic C–C chemokine, macrophage inflammatory protein (MIP)-1α, is a candidate for OC stimulatory factor(s) secreted from MM cells. We have reported that not only MIP-1α, but also MIP-1β is secreted by most primary MM cells from patients with multiple osteolytic lesions and that these chemokines mediate most of the osteoclastogenic activity produced by MM cells in vitro [2]. Furthermore, the ability of MM cells to secrete these chemokines correlates well with the extent of bone lesions as well as the levels of bone resorption markers in patients with MM [3]. These results suggest that MM cell-derived MIP-1α and MIP-1β are predominant factors responsible for the enhancement of bone resorption in MM and play a causal role in the development of lytic bone lesions in vivo.
The interaction between MM cells and stromal cells confers MM cell homing, growth, survival, and resistance to chemotherapy [4–9]. In this context, adhesion between very late antigen (VLA)-4 and its corresponding ligand, vascular cell adhesion molecule (VCAM)-1, is of particular note because VLA-4 and VCAM-1 are strongly and constitutively expressed on MM cells and bone marrow stromal cells, respectively [10–14]. VLA-4–VCAM-1 adhesion is also important for MM-induced osteoclastogenesis. Michigami et al. [13] reported that adhesion via VLA-4–VCAM-1 interaction induces the secretion of osteoclastogenic factors from a murine myeloma cell line, 5TGM1, and human myeloma-derived cell lines, ARH77 and U266, but not from stromal cells. The role of VLA-4 in MM-associated bone lesions was further demonstrated in syngeneic mice inoculated with 5TGM1 cells in which a neutralizing monoclonal antibody against VLA-4 significantly reduced osteoclastic osteolysis [14]. However, precise mechanisms by which MM cells activate osteoclastic bone resorption through VLA-4–VCAM-1 interaction remain unclear. To clarify the mechanism of osteoclastogenesis induced through MM cell adhesion to stromal cells via VLA-4–VCAM-1 interaction, we investigated whether MIP-1 plays a role in MM cell adhesion-mediated osteoclastogenesis via VLA-4–VCAM-1 interaction. We demonstrate herein that MIP-1 triggers VLA-4 activation in MM cells to enhance VLA-4–VCAM-1 interaction and that MM cell adhesion via VLA-4–VCAM-1 interaction upregulates MIP-1 secretion from MM cells, leading to further potentiation of osteoclastogenic activity of MM cells.
Materials and methods
Chemicals
Recombinant human (rh) MIP-1α and MIP-1β, mouse IgG1, neutralizing mouse antihuman MIP-1α and MIP-1β monoclonal antibodies (MoAbs), goat IgG, neutralizing goat antihuman MIP-1α and MIP-1β polyclonal antibodies, blocking mouse antihuman VLA-4 monoclonal antibody, and rhVCAM-1 were obtained from R&D Systems (Minneapolis, MN). Neutralizing mouse antihuman interleukin (IL)-6 and anti-IL-1β MoAbs were purchased from Genzyme (Cambridge, MA) and fluorescein isothiocyanate (FITC)-conjugated mouse antihuman VLA-4 and goat antimouse VCAM-1 antibodies from Pharmingen (San Diego, CA).
Cells
A human myeloma-derived cell line, ARH77, a murine bone marrow stromal cell line, ST-2, and a murine preosteoblastic cell line, MC3T3-E1, were obtained from the American Type Culture Collection (Rockville, MD). Highly purified MM cells were subsequently prepared by a positive selection using magnetic beads coated with a human MM cell-specific anti-CD138 MoAb (Dynal, Great Neck, NY). Purity of the MM cells thus obtained was more than 95%. All procedures involving human specimens were performed according to the protocol approved by the institutional review board for human protection, and informed consent was given.
Cell adhesion assays
rhVCAM-1 was applied to 24-well culture plates at 10 μg/ml in Ca- and Mg-free phosphate-buffered saline (PBS) and incubated at 4°C overnight. Nonspecific binding sites were subsequently blocked with 3% bovine serum albumin (BSA; Sigma) in Ca-/Mg-free PBS for 2 h at 37°C. MM cells were labeled with 10 μg/ml fluorescent dye (BCECF-AM; Dojindo, Kumamoto, Japan) in GIT medium for 2 h at 37°C. A total of 1 × 106 MM cells were washed, resuspended in GIT medium with or without the indicated antibodies at a saturating concentration (20 μg/ml) or pertussis toxin (Sigma), plated onto prewashed rhVCAM-1-coated plates, incubated at 4°C for 30 min, and then rapidly warmed to 37°C and further incubated for 30 min. After gently washing four times with GIT medium at room temperature, fluorescence intensity of lysed adherent cells was measured as previously described [15].
Flow cytometry
Cell preparation and staining for flow cytometry were performed as described previously [16]. Approximately 106 cells were incubated with saturating concentrations of FITC-conjugated MoAbs on ice for 1 h. For indirect fluorescence staining, cells were incubated first with primary antibodies on ice for 1 h, washed, and then incubated with FITC-conjugated secondary antibodies on ice for 30 min. Samples were analyzed by flow cytometry using EPICS-Profile (Coulter Electronics, Hialeah, FL).
Collection of conditioned media and measurement of cytokine secretion
Conditioned media (CM) were harvested from ARH77 cells at 5 × 105 cells/ml after culturing on VCAM-1- or BSA (Sigma)-coated wells for 2 days. For coculture experiments, we collected CM from ARH77 cells alone or their cocultures with murine osteoblastic MC3T3-E1 cells, which constitutively express VCAM-1 at high levels. MIP-1α, MIP-1β, VEGF, and HGF were measured using Quantikine Enzyme Immunoassay kits, respectively (R&D Systems), according to the manufacturer’s instructions.
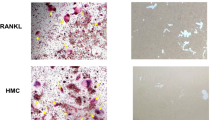
In vitro osteoclastogenesis
For in vitro osteoclastogenesis, osteoclast precursors were first prepared from unfractionated bone cells according to the previously described procedure [17] with a slight modification. In brief, minced long bones of 5-day-old white rabbits were agitated by vortexing, and bone particles were removed by sedimentation for 30 s in Eagle’s minimal essential medium (MEM; Life Technologies, Gaithersburg, MD). After centrifugation at 300g for 3 min, two-thirds of the supernatant from the top was removed. Remaining fractions were used as a source of osteoclast precursors. Thus, obtained preosteoclast-rich fractions of rabbit bone cells were seeded in 96-well plates containing a bovine dentine at 5 × 103 cells/well and cultured for 96 h in MEM containing 10% FBS in the absence or presence of various factors or CM. For coculture experiments, rabbit bone cells thus obtained at 5 × 103 cells/100 μl/well were cocultured for 96 h with ARH77 cells at 2 × 103 cells/100 μl/well. To evaluate osteoclast-like cell formation, cells were stained for tartrate-resistant acid phosphatase (TRAP) using a leukocyte acid phosphatase kit (Sigma), and the numbers of TRAP-positive multinucleated cells were counted.
Reverse transcription-polymerase chain reaction
Total RNA was extracted from various cells using TRIZOL reagent (Invitrogen, Carlsbad, CA). Then, 2 μg total RNA was reverse transcribed with Superscript II (Invitrogen) in a 20-μl reaction. Of the 20-μl reaction, 2 μl was used for the subsequent polymerase chain reaction (PCR) analysis with cycles of 95°C for 30 s, 58°C for 30 s, and 72°C for 30 s. Primers used are as follows: 5′-GTTCCTGTACTTTCGAGCGCAGAT-3′ (nucleotides 336–360) and 5′-TGACTTTATGGGAACCCGATGGGA-3′ (nucleotides 357–380) for mouse receptor activator of nuclear factor-kappaB (RANK) ligand, and 5′-TGTCTTCACCACCATGGAGAAGG-3′ (nucleotides 340–362) and 5′-GTGGATGCAGGGATGATGTTCTG-3′ (nucleotides 672–650) for mouse glyceraldehyde phosphate dehydrogenase (GAPDH). Amplified products were separated and stained with ethidium bromide for visualization.
Statistical analysis
Statistical significance was determined by one-way analysis of variance (ANOVA) with Scheffe post hoc tests. The minimum level of significance was P = 0.05.
Results
VLA-4 activation by endogenous MIP-1 in ARH77 cells
Because ARH77 cells are shown to produce the most potent osteoclastogenic activity by their adhesion to VCAM-1 among human MM cell lines tested [13] and are able to generate human MM-like bone destructive lesions in vivo [18], we first used ARH77 cells to investigate the mechanism of osteoclastogenesis by VLA-4–VCAM-1 interaction. ARH77 cells constitutively express VLA-4 on their surface (Fig. 1a) and abundantly secrete MIP-1α and MIP-1β, which are responsible for the enhancement of OC formation and activation by these cells [1, 2, 19]. Because MIP-1α and MIP-1β trigger integrins in leukocytes as well as lymphoid tumor cells and induce integrin-mediated adhesion of these cells [20–23], we investigated whether these chemokines affect adhesion of MM cells to VCAM-1. About one-half of ARH77 cells spontaneously adhered to VCAM-1-coated plates (Fig. 1b), which was mostly inhibited by anti-VLA-4 antibody. Thus, VLA-4–VCAM-1 interaction appears to play a predominant role in adhesion of MM cells to VCAM-1-expressing stromal cells. Interestingly, the addition of anti-MIP-1α and anti-MIP-1β neutralizing antibodies together to block the actions of endogenous MIP-1α and MIP-1β also reduced spontaneous adhesion of the MM cells substantially. These results suggest that MM cell-derived MIP-1α and MIP-1β mediate spontaneous adhesion of MM cells in an autocrine/paracrine fashion. To further clarify the role of these chemokines in the adhesion of MM cells, we next investigated the effects of pertussis toxin, an inhibitor of Gs protein, to block the downstream signaling of Gs protein-coupled chemokine receptors on MM cell adhesion to VCAM-1-coated plates. Addition of pertussis toxin suppressed ARH77 cell adhesion to VCAM-1 to a level similar to that by anti-MIP-1 antibodies. These results are consistent with the notion that MIP-1 signaling is spontaneously activated in ARH77 cells to trigger VLA-4 adhesion to VCAM-1 in an autocrine/paracrine fashion. MIP-1-mediated MM cell adhesion was also observed using patients’ MM cells (Fig. 1c). Cell-surface expression of VLA-4 on ARH77 cells was not changed as shown in flow cytometry after blocking MIP-1 actions (data not shown). Taken together, these results suggest that MM cell-derived MIP-1α and MIP-1β activate VLA-4 on MM cells and contribute to VLA-4-dependent adhesion of MM cells to VCAM-1 expressed on bone marrow stromal cells.
Spontaneous multiple myeloma (MM) cell adhesion to vascular cell adhesion molecule (VCAM)-1. a Expression of very late antigen (VLA)-4 by ARH77 cells. Surface expression of VLA-4 was analyzed by flow cytometry as described in “Materials and methods.” ARH77 (b) cells and primary MM cells (c) adhered to rhVCAM-1-coated plates in quadruplicate were counted as described in “Materials and methods” and expressed as percent ratios of the input cell numbers. Anti-macrophage inflammatory protein (MIP)-1α and anti-MIP-1β neutralizing antibodies in combination, anti-VLA-4 blocking antibody, or control IgG was added at 20 μg/ml to the indicated wells. The treatment with pertussis toxin (PTX) was described in “Materials and methods.” The data are expressed as mean ± SD. *Significantly different from the controls by one-way analysis of variance (ANOVA) with Scheffe post hoc tests, P < 0.05
Suppression of OC formation and function by blockade of VLA-4-mediated ARH77 cell adhesion
To clarify the role of VLA-4-mediated adhesion in the enhancement of osteolysis by MM cells, we examined the effect of a blocking antibody against VLA-4 on osteoclastogenesis in coculture experiments. As shown in Fig. 2, anti-VLA-4 antibody as well as anti-MIP-1α and anti-MIP-1β antibodies in combination significantly reduced OC formation and function induced by ARH77 cells. Because blockade of MIP-1 actions mostly abolished VLA-4-mediated adhesion of MM cells (as shown in Fig. 1b), it is plausible to assume that MIP-1α and MIP-1β enhance osteoclastic bone resorption via both VLA-4-dependent and VLA-4-independent mechanisms.
Suppression of ARH77 cell-mediated osteoclast formation and function by anti-VLA-4 antibody. ARH77 cells were cocultured with rabbit bone cells on dentine slices as described in “Materials and methods.” The data represent the number of tartrate-resistant acid phosphatase (TRAP)-positive multinucleated cells (MNCs) (a) and pits on dentine slices (b). Anti-MIP-1α and anti-MIP-1β neutralizing antibodies in combination, anti-VLA-4 blocking antibody, or control IgG was added at 20 μg/ml to the indicated wells. The data are expressed as mean ± SD of five samples. *Significantly different from the controls by one-way ANOVA with Scheffe post hoc tests, P < 0.05
Upregulation of MIP-1α and MIP-1β secretion from ARH77 cells by VLA-4–VCAM-1 interaction
Michigami et al. [13] reported that direct contact of MM cells with bone marrow stromal cells enhances the production of osteoclastogenic activity from MM cells, but not from stromal cells, and that disruption of cell–cell interaction by an anti-VLA-4 antibody suppressed the production of osteoclastogenic activity. Such osteoclastogenic activity was not blocked by neutralizing antibodies against known osteoclastogenic factors, including IL-1α, IL-1β, IL-6, tumor necrosis factor (TNF)-α, TNF-β, or parathyroid hormone-related protein [13]. To identify MM cell-derived factors responsible for the enhancement of osteoclastogenesis by VLA-4-mediated adhesion, we collected CM from ARH77 cells cultured on VCAM-1-coated or BSA-coated wells and measured the levels of osteoclastogenic cytokines that were not studied by Michigami et al. [13], including MIP-1α, MIP-1β, and vascular endothelial growth factor (VEGF). Culturing ARH77 cells on VCAM-1-coated plates enhanced secretion of both MIP-α and MIP-1β by almost twofold, and the enhancement of MIP-1 production was almost completely reversed by anti-VLA-4 blocking antibody (Fig. 3). Secretion level of VEGF was not altered by addition of ARH77 cells to VCAM-1-coated plates (data not shown). These results demonstrate that VLA-4–VCAM-1 interaction triggers the upregulation of MIP-1 production by ARH77 cells and suggest that the increased osteoclastogenic activity secreted from MM cells by VLA-4–VCAM-1 interaction may be MIP-1.
Upregulation of MIP-1α and MIP-1β secretion by ARH77 cells through VLA-4–VCAM-1 adhesion. ARH77 cells were cultured in quadruplicate on rhVCAM-1 or bovine serum albumin (BSA)-coated wells for 2 days as described in “Materials and methods.” Anti-VLA-4 antibody was added at 20 μg/ml to the indicated wells. MIP-1α (left) and MIP-1β (right) levels in the culture supernatants were measured by enzyme-linked immunosorbent assay (ELISA). The data are expressed as mean ± SD. *Significantly different by one-way ANOVA with Scheffe post hoc tests, P < 0.05
Role of MIP-1 in osteoclastogenesis induced by VLA-4–VCAM-1 interaction
To clarify whether MIP-1 is responsible for VLA-4–VCAM-1 adhesion-mediated enhancement of osteoclastogenesis, CM from ARH77 cells cultured on either VCAM-1-coated or BSA-coated plates for 2 days were harvested, and their osteoclastogenic activity was examined in the presence of either anti-MIP-1α and anti-MIP-1β antibodies in combination or control IgG. Although CM from ARH77 cells cultured on BSA-coated plates enhanced osteoclastogenesis, those from cells on VCAM-1-coated plates enhanced osteoclastogenesis to a significantly higher degree compared to those from cells on the BSA-coated plates (Fig. 4). The enhancement of osteoclastogenesis was almost completely abolished by addition of antibodies against MIP-1α and MIP-1β in combination. Antibodies against IL-1β or IL-6 showed no significant effects. These observations demonstrate that MM cell-derived MIP-1α and MIP-1β are predominant factors responsible for osteoclastogenesis enhanced by MM cell adhesion to VCAM-1.
Inhibition of osteoclastogenesis induced by ARH77 adhesion to VCAM-1 by anti-MIP-1 antibodies. Rabbit bone cells were cultured as described in “Materials and methods.” Conditioned media (CM) were collected from ARH77 cells cultured either on rhVCAM-1- or bovine serum albumin (BSA)-coated wells, and added at a final dilution of 1/2 to the indicated wells. Antibodies against MIP-1α and MIP-1β in combination, interleukin (IL)-1β and IL-6, or control IgG was added at 20 μg/ml to the indicated wells. The numbers of TRAP-positive multinucleated cells (MNCs) were counted at day 4. The data are expressed as mean ± SD of five samples. *Significantly different by one-way ANOVA with Scheffe post hoc tests, P < 0.05
Enhancement of MIP-1α production via VLA-4–VCAM-1 adhesion between ARH77 and MC3T3-E1 preosteoblastic cells
To further confirm a role for VLA-4-mediated adhesion in MM cell production of MIP-1 in the context of MM cell-stromal/osteoblastic cell interactions, we cocultured human ARH77 cells with murine MC3T3-E1 preosteoblastic cells, which constitutively express VCAM-1 at high levels (Fig. 5a). The cocultures of ARH77 cells and MC3T3-E1 cells upregulated the levels of human MIP-1α in their culture supernatants (Fig. 5b), but not murine MIP-1α. The enhancement of human MIP-1α production was mostly reversed by addition of a blocking antibody against VLA-4. These results suggest that VLA-4-mediated MM cell adhesion to VCAM-1-expressing stromal or osteoblastic cells can enhance the secretion of MIP-1 by MM cells.
Enhancement of MIP-1α production in cocultures of ARH77 cells with MC3T3-E1 cells. a Expression of VCAM-1 by murine MC3T3-E1 preosteoblastic cells. Surface expression of VCAM-1 was analyzed by flow cytometry as described in “Materials and methods.” b ARH77 cells (2 × 105 per ml) were cocultured in quadruplicate for 2 days with MC3T3-E1 cells confluent in 24-well culture plates, and human MIP-1α levels in the culture supernatants were measured by ELISA. Anti-VLA-4 antibody was added at 20 μg/ml to the indicated wells. The data are expressed as mean ± SD. *Significantly different by one-way ANOVA with Scheffe post hoc tests, P < 0.05
Suppression of MM cell-induced RANK ligand expression in stromal cells by anti-MIP-1 as well as anti-VLA-4 antibodies
To clarify the involvement of RANK ligand induction in stromal cells as the downstream signaling, we investigated RANK ligand mRNA expression in ST-2 stromal cells in cocultures with MM cells. When MIP-1-producing U266 MM cells were cocultured with ST-2 stromal cells, RANK ligand mRNA expression by ST-2 cells was upregulated (Fig. 6). Addition of neutralizing antibodies against MIP-1α and MIP-1β in combination or VLA-4 reversed the RANK ligand upregulation by ST-2 cells in the coculture. These results demonstrate the involvement of RANK ligand induction in stromal cells as downstream signaling.
Suppression of MM cell-induced receptor activator of nuclear factor-kappa B (RANK) ligand expression in stromal cells by anti-MIP-1 as well as anti-VLA-4 antibodies. MIP-1-producing U266 MM cells (2 × 105 per ml) were cocultured for 2 days with ST-2 stromal cells confluent in 24-well culture plates. Anti-MIP-1α and anti-MIP-1β neutralizing antibodies in combination, anti-VLA-4 blocking antibody, or control IgG was added at 20 μg/ml to the indicated wells. After washing to remove the MM cells, total RNA was extracted from ST-2 cells. RANK ligand and glyceraldehyde phosphate dehydrogenase (GAPDH) mRNA expression by ST-2 cells was determined as described in “Materials and methods”
Discussion
The present study confirmed the previous study by Michigami et al. that showed VLA-4-mediated adhesion of MM cells to VCAM-1 potentiates the production of osteoclastogenic activity and demonstrated that VLA-4–VCAM-1 interaction upregulates the production of MIP-1α and MIP-1β by MM cells. Because the osteoclastogenic activity enhanced by VLA-4–VCAM-1 interaction was abrogated by anti-MIP-1α and anti-MIP-1β antibodies, osteoclastogenesis enhanced by CM from MM cells adhered to VCAM-1 is mostly mediated by these chemokines elaborated by MM cells. Interactions between RANK on OC lineage cells and RANK ligand on stromal cells play a key role in the development and activation of OCs [24–28]. MM cells stimulate osteoclastogenesis by an increase in RANK ligand expression in bone marrow stromal cells [29–31]. We previously demonstrated that these chemokines are able to induce RANK ligand expression in stromal cells and enhance osteoclastogenesis in a RANK ligand-dependent manner [2]. MM cell adhesion to stromal cells via VLA-4–VCAM-1 interaction has been also reported to enhance RANK ligand expression in stromal cells [30]. Consistently, blockade of MIP-1 actions or VLA-4-mediated adhesion reversed MM cell-induced RANK ligand upregulation in ST-2 stromal cells, which suggests the involvement of RANK ligand induction in stromal cells as downstream signaling. Therefore, overproduction of these chemokines by MM cells via VLA-4–VCAM-1 interaction may lead to further upregulation of RANK ligand expression in stromal cells.
It is intriguing that VLA-4-mediated adhesion of MM cells to VCAM-1-coated plates was mostly inhibited by addition of anti-MIP-1 neutralizing antibodies (see Fig. 1b, c). Integrins such as VLA-4 are normally inactive and require their conformational change to expose their active binding sites to their ligands for firm adhesion. The integrin activation is induced by intracellular signaling triggered by engagement of chemokine receptors (inside-out activation). Binding of MIP-1α or MIP-1β to their cognate receptors has been demonstrated to trigger the activation of integrins [20–23]. Because MM cells constitutively express receptors for MIP-1, including CCR1 and CCR5 [2, 32], MIP-1 is able to act on MM cells in an autocrine/paracrine fashion to activate VLA-4 on MM cells. Disruption of the transduction of downstream signaling from MIP-1 receptors by pertussis toxin as well as blocking MIP-1 actions by anti-MIP-1 antibodies inhibited MM cell adhesion to VCAM-1 to a level similar to that by an anti-VLA-4 antibody. These results suggest that activation of VLA-4 by endogenous MIP-1 signaling significantly contributes to adhesion of MM cells to stromal cells.
In addition to osteoclastogenesis, MM cell adhesion to stromal cells via VLA-4–VCAM-1 interaction plays a critical role in the growth and survival of MM cells. Of note, ligation of VLA-4 confers resistance of MM cells to chemotherapeutic agents, known as cell adhesion-mediated drug resistance (CAM-DR) [8, 9]. Along with stromal cells, OCs induced by MM promote MM cell growth and survival as well as their resistance to anticancer drugs [33–35]. Because MIP-1 enhances both VLA-4-dependent MM cell adhesion to stromal cells and osteoclastogenesis, it is plausible that MIP-1 may contribute to accumulation and expansion of MM cells in the bone marrow as well as refractoriness of MM cells to chemotherapy. Therefore, antagonists of MIP-1 activity or inhibitors of MIP-1 signaling may provide new therapeutic approaches to suppress tumor progression and ameliorate bone destruction in MM patients.
References
Choi SJ, Cruz JC, Craig F, Chung H, Devlin RD, Roodman GD, Alsina M (2000) Macrophage inflammatory protein 1-alpha is a potential osteoclast stimulatory factor in multiple myeloma. Blood 96:671–675
Abe M, Hiura K, Wilde J, Moriyama K, Hashimoto T, Ozaki S, Wakatsuki S, Kosaka M, Kido S, Inoue D, Matsumoto T (2002) Role for macrophage inflammatory protein (MIP)-1alpha and MIP-1beta in the development of osteolytic lesions in multiple myeloma. Blood 100:2195–2202
Hashimoto T, Abe M, Oshima T, Shibata H, Ozaki S, Inoue D, Matsumoto T (2004) Ability of myeloma cells to secrete macrophage inflammatory protein (MIP)-1alpha and MIP-1beta correlates with lytic bone lesions in patients with multiple myeloma. Br J Haematol 125:38–41
Caligaris-Cappio F, Bergui L, Gregoretti MG, Gaidano G, Gaboli M, Schena M, Zallone AZ, Marchisio PC (1991) Role of bone marrow stromal cells in the growth of human multiple myeloma. Blood 77:2688–2693
Roodman GD (2002) Role of the bone marrow microenvironment in multiple myeloma. J Bone Miner Res 17:1921–1925
Nefedova Y, Landowski TH, Dalton WS (2003) Bone marrow stromal-derived soluble factors and direct cell contact contribute to de novo drug resistance of myeloma cells by distinct mechanisms. Leukemia 17:1175–1182
De Raeve HR, Vanderkerken K (2005) The role of the bone marrow microenvironment in multiple myeloma. Histol Histopathol 20:1227–1250
Damiano JS, Cress AE, Hazlehurst LA, Shtil AA, Dalton WS (1999) Cell adhesion mediated drug resistance (CAM-DR): role of integrins and resistance to apoptosis in human myeloma cell lines. Blood 93:1658–1667
Dalton WS, Hazlehurst L, Shain K, Landowski T, Alsina M (2004) Targeting the bone marrow microenvironment in hematologic malignancies. Semin Hematol 41:1–5
Faid L, Van Riet I, De Waele M, Facon T, Schots R, Lacor P, Van Camp B (1996) Adhesive interactions between tumour cells and bone marrow stromal elements in human multiple myeloma. Eur J Haematol 57:349–358
Sanz-Rodriguez F, Ruiz-Velasco N, Pascual-Salcedo D, Teixido J (1999) Characterization of VLA-4-dependent myeloma cell adhesion to fibronectin and VCAM-1. Br J Haematol 107:825–834
Hideshima T, Chauhan D, Podar K, Schlossman RL, Richardson P, Anderson KC (2001) Novel therapies targeting the myeloma cell and its bone marrow microenvironment. Semin Oncol 28:607–612
Michigami T, Shimizu N, Williams PJ, Niewolna M, Dallas SL, Mundy GR, Yoneda T (2000) Cell-cell contact between marrow stromal cells and myeloma cells via VCAM-1 and alpha(4)beta(1)-integrin enhances production of osteoclast-stimulating activity. Blood 96:1953–1960
Mori Y, Shimizu N, Dallas M, Niewolna M, Story B, Williams PJ, Mundy GR, Yoneda T (2004) Anti-alpha4 integrin antibody suppresses the development of multiple myeloma and associated osteoclastic osteolysis. Blood 104:2149–2154
Rice GE, Munro JM, Bevilacqua MP (1990) Inducible cell adhesion molecule 110 (INCAM-110) is an endothelial receptor for lymphocytes. A CD11/CD18-independent adhesion mechanism. J Exp Med 171:1369–1374
Goto T, Kennel SJ, Abe M, Takishita M, Kosaka M, Solomon A, Saito S (1994) A novel membrane antigen selectively expressed on terminally differentiated human B cells. Blood 84:1922–1930
Takada Y, Kusuda M, Hiura K, Sato T, Mochizuki H, Nagao Y, Tomura M, Yahiro M, Hakeda Y, Kawashima H (1992) A simple method to assess osteoclast-mediated bone resorption using unfractionated bone cells. Bone Miner 17:347–359
Alsina M, Boyce B, Devlin RD, Anderson JL, Craig F, Mundy GR, Roodman GD (1996) Development of an in vivo model of human multiple myeloma bone disease. Blood 87:1495–1501
Choi SJ, Oba Y, Gazitt Y, Alsina M, Cruz J, Anderson J, Roodman GD (2001) Antisense inhibition of macrophage inflammatory protein 1-alpha blocks bone destruction in a model of myeloma bone disease. J Clin Invest 108:1833–1841
Tanaka Y, Adams DH, Hubscher S, Hirano H, Siebenlist U, Shaw S (1993) T-cell adhesion induced by proteoglycan-immobilized cytokine MIP-1 beta. Nature 361:79–82
Tanaka Y, Mine S, Figdor CG, Wake A, Hirano H, Tsukada J, Aso M, Fujii K, Saito K, van Kooyk Y, Eto S (1998) Constitutive chemokine production results in activation of leukocyte function-associated antigen-1 on adult T-cell leukemia cells. Blood 91:3909–3919
Tanaka Y, Mine S, Hanagiri T, Hiraga T, Morimoto I, Figdor CG, van Kooyk Y, Ozawa H, Nakamura T, Yasumoto K, Eto S (1998) Constitutive up-regulation of integrin-mediated adhesion of tumor-infiltrating lymphocytes to osteoblasts and bone marrow-derived stromal cells. Cancer Res 58:4138–4145
Kinashi T (2005) Intracellular signalling controlling integrin activation in lymphocytes. Nat Rev Immunol 5:546–559
Miyamoto A, Kunisada T, Hemmi H, Yamane T, Yasuda H, Miyake K, Yamazaki H, Hayashi SI (1998) Establishment and characterization of an immortal macrophage-like cell line inducible to differentiate to osteoclasts. Biochem Biophys Res Commun 242:703–709
Nakagawa N, Kinosaki M, Yamaguchi K, Shima N, Yasuda H, Yano K, Morinaga T, Higashio K (1998) RANK is the essential signaling receptor for osteoclast differentiation factor in osteoclastogenesis. Biochem Biophys Res Commun 253:395–400
Simonet WS, Lacey DL, Dunstan CR, Kelley M, Chang MS et al (1997) Osteoprotegerin: a novel secreted protein involved in the regulation of bone density. Cell 89:309–319
Kong YY, Yoshida H, Sarosi I, Tan HL, Timms E, Capparelli C, Morony S, Oliveira-dos-Santos AJ, Van G, Itie A, Khoo W, Wakeham A, Dunstan CR, Lacey DL, Mak TW, Boyle WJ, Penninger JM (1999) OPGL is a key regulator of osteoclastogenesis, lymphocyte development and lymph-node organogenesis. Nature 397:315–323
Dougall WC, Glaccum M, Charrier K, Rohrbach K, Brasel K, De Smedt T, Daro E, Smith J, Tometsko ME, Maliszewski CR, Armstrong A, Shen V, Bain S, Cosman D, Anderson D, Morrissey PJ, Peschon JJ, Schuh J (1999) RANK is essential for osteoclast and lymph node development. Genes Dev 13:2412–2424
Pearse RN, Sordillo EM, Yaccoby S, Wong BR, Liau DF, Colman N, Michaeli J, Epstein J, Choi Y (2001) Multiple myeloma disrupts the TRANCE/osteoprotegerin cytokine axis to trigger bone destruction and promote tumor progression. Proc Natl Acad Sci USA 98:11581–11586
Giuliani N, Bataille R, Mancini C, Lazzaretti M, Barille S (2001) Myeloma cells induce imbalance in the osteoprotegerin/osteoprotegerin ligand system in the human bone marrow environment. Blood 98:3527–3533
Sezer O, Heider U, Zavrski I, Kuhne CA, Hofbauer LC (2003) RANK ligand and osteoprotegerin in myeloma bone disease. Blood 101:2094–2098
Van de Broek I, Leleu X, Schots R, Facon T, Vanderkerken K, Van Camp B, Van Riet I (2006) Clinical significance of chemokine receptor (CCR1, CCR2 and CXCR4) expression in human myeloma cells: the association with disease activity and survival. Haematologica 91:200–206
Yaccoby S, Wezeman MJ, Henderson A, Cottler-Fox M, Yi Q, Barlogie B, Epstein J (2004) Cancer and the microenvironment: myeloma-osteoclast interactions as a model. Cancer Res 64:2016–2023
Abe M, Hiura K, Wilde J, Shioyasono A, Moriyama K, Hashimoto T, Kido S, Oshima T, Shibata H, Ozaki S, Inoue D, Matsumoto T (2004) Osteoclasts enhance myeloma cell growth and survival via cell-cell contact: a vicious cycle between bone destruction and myeloma expansion. Blood 104:2484–2491
Abe M, Kido S, Hiasa M, Nakano A, Oda A, Amou H, Matsumoto T (2006) BAFF and APRIL as osteoclast-derived survival factors for myeloma cells: a rationale for TACI-Fc treatment in patients with multiple myeloma. Leukemia 20:1313–1315
Acknowledgments
We thank Ms. Hiroe Amou, Ms. Asuka Oda, and Dr. Masahiro Hiasa for their expert technical assistance. This work was supported in part by Grants-in-Aid for Scientific Research (A) to T. M. and (C) to M. A., and for the 21st Century Center of Excellence Program from the Ministry of Education, Culture, Science, and Sports of Japan, and a Grant-in-Aid for Cancer Research (17-16) from the Ministry of Health, Labor, and Welfare of Japan.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Abe, M., Hiura, K., Ozaki, S. et al. Vicious cycle between myeloma cell binding to bone marrow stromal cells via VLA-4–VCAM-1 adhesion and macrophage inflammatory protein-1α and MIP-1β production. J Bone Miner Metab 27, 16–23 (2009). https://doi.org/10.1007/s00774-008-0012-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-008-0012-z