Abstract
Many pregnant and postpartum women worldwide suffer from high anxiety and/or depression, which can have detrimental effects on maternal and infant well-being. The first-line pharmacotherapies for prepartum and postpartum affective disorders continue to be the selective serotonin reuptake inhibitors (SSRIs), despite the lack of large well-controlled studies demonstrating their efficacy in reproducing women and the potential for fetal/neonatal exposure to the drugs. Prepartum or postpartum use of SSRIs or other drugs that modulate the brain’s serotonin system is also troubling because very little is known about the typical, let alone the atypical, changes that occur in the female central serotonin system across reproduction. We do know from a handful of studies of women and female laboratory rodents that numerous aspects of the central serotonin system are naturally dynamic across reproduction and are also affected by pregnancy stress (a major predisposing factor for maternal psychopathology). Thus, it should not be assumed that the maternal central serotonin system being targeted by SSRIs is identical to non-parous females or males. More information about the normative and stress-derailed changes in the maternal central serotonin system is essential for understanding how serotonin is involved in the etiology of, and the best use of SSRIs for potentially treating, affective disorders in the pregnant and postpartum populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Recent analyses indicate that at least 10–15% of the millions of pregnant and parturient women worldwide each year are faced with a depressive disorder and at least 8–10% suffer from an anxiety disorder (Fairbrother et al. 2016; Goodman et al. 2016; Le Strat et al. 2011; Reck et al. 2008). When one further considers the many pregnant and postpartum women with high, but subclinical, depressive and anxious symptoms, the number of affected women is extremely troubling. Mental health problems at any time of life are certainly a cause for concern, but heightened attention to them during this period of possibly increased susceptibility (see Davé et al. 2010; O'Hara et al. 1990; Britton, 2008) is especially important because there are few times in a woman’s life when the stakes of having a depressive or anxiety disorder are as high. Indeed, a peripartum psychiatric admission is a greater mortality risk for women compared to almost all other causes, including heavy smoking (Appleby 1998; Chesney et al. 2014). Depression or anxiety during pregnancy and postpartum are also each associated with a host of other negative outcomes for mothers and their infants. At their extreme, maternal depression and anxiety contribute to infant neglect and abuse, but more commonly are associated with lower rates of breastfeeding, lack of maternal emotional and behavioral sensitivity to the infant, poor mother-infant bonding, negative infant temperament, altered infant neurodevelopment, and emotional and behavioral problems in the children when they are older (Drury et al. 2016; Field 2010; Glasheen et al. 2010; Stein et al. 2014). Because of a desperate need for increased attention to maternal affective disorders, the United States Preventive Services Task Force and the American College of Obstetricians and Gynecologists each recently recommended routine mental health screening for all pregnant and postpartum women (Committee on Obstetric Practice 2015; O'Connor et al. 2016).
The first-line pharmacotherapies for affective disorders in pregnant and postpartum women are the serotonin reuptake inhibitors (SSRIs). SSRIs are prescribed to ~2–8% of pregnant women and ~ 4% of early postpartum women in the United States; even higher usage can be found elsewhere (e.g., > 9% in the U.K.) (Alwan et al. 2011; Andrade et al. 2008; Charlton et al. 2015; Hanley and Mintzes 2014; Huybrechts et al. 2013; Lupattelli et al. 2014; Munk-Olsen et al., 2012). This is true despite concerns about placental and breastmilk transference of the drugs or their metabolites impacting fetal and neonatal development (Glover and Clinton 2016; Oberlander et al. 2009; Weisskopf et al. 2015), as well as the lack of large double-blind, placebo-controlled studies of SSRIs involving reproducing women (De Crescenzo et al. 2014; McDonagh et al. 2014; Molyneaux et al. 2015).
How SSRIs may alleviate depression and anxiety is unclear, but the mechanisms at least initially involve elevated central serotonergic signaling. Some supporting evidence for this includes that SSRIs have lower clinical efficacy in people with serotonin transporter gene (SERT) polymorphisms that yield low transcriptional activity (Ruhé et al. 2009; Serretti and Kato 2008), that some strains of SERT-knockout rodents show abnormally high depressive- and anxiety-like behaviors (Holmes et al. 2002; Kalueff et al., 2007; Lira et al. 2003; Olivier et al. 2008), and that SERT-knockout mice are resistant to SSRIs’ antidepressant behavioral effects (Holmes et al. 2002). After elevating serotonergic activity, the downstream consequences of SSRIs on the brain include neuroplastic changes (e.g., cell birth and survival, cell death, synaptogenesis, dendrite morphology, and axonal outgrowth) within the hippocampus, cortex, and even back on the serotonin system itself that facilitate adaptation to stress (Haase and Brown 2015; Pittenger and Duman 2008). Eliminating the signaling of a major neurotrophic factor mediating many types of neuroplasticity, brain-derived neurotrophic factor (BDNF), by mutating its TrkB receptor gene in the hippocampus or midbrain dorsal raphe (DR; the source of most forebrain-projecting serotonin cells (Lowry et al. 2008) prevents SSRIs’ positive effects on neuroplasticity and affective behaviors in laboratory rodents (Adachi et al. 2017; Horne et al. 2008; Li et al., 2008; Monteggia et al. 2004; Saarelainen et al. 2003).
Concern about the high rate of SSRI use by pregnant and postpartum women also comes from the fact that we know very little about how SSRIs may act uniquely on the pregnant and postpartum brain. Due to the physiological adaptations of reproduction that alter drug absorption, distribution, metabolism, and elimination (Anderson 2006; Pariente et al. 2016), SSRI doses are often increased for pregnant and early postpartum women in order to maintain drug blood levels and hopefully their clinical efficacy (Crescenzo et al. 2014; Hostetter et al. 2000; McDonagh et al. 2014; Molyneaux et al. 2015). However, this is based on insufficient empirical evidence. A small longitudinal study of 11 women found a late-pregnancy drop in plasma concentrations of the SSRI, citalopram, although most of the women did not require an increased dose to maintain euthymia (Heikkinen et al. 2002). Two other small longitudinal studies assessing women from pregnancy week 20 to 3 months postpartum also revealed increased SSRI drug clearance during pregnancy, but not in all of the women (Sit et al. 2008, 2010). Yet another small study found no significant differences across pregnancy in metabolism of the SSRI, sertraline, but noted very large individual differences among the women (Freeman et al. 2008). Such individual differences in SSRI metabolism are partly due to genotypic differences in drug-metabolizing cytochrome 450 liver enzymes, (Ververs et al. 2009) and are associated with women’s continuance or discontinuance of their antidepressants (Berard et al. 2017). To further complicate things, a very recent analysis of blood samples from almost 300 pregnant women found that third-trimester drug concentrations were lower than baseline only for some SSRIs (paroxetine, citalopram), were higher than baseline for another SSRI (sertraline), and did not change for two others (escitalopram and fluoxetine) (Westin et al. 2017). In addition to this complex collection of results raising questions about the frequent practice of increasing SSRI doses for pregnant and early postpartum women, adjusting SSRI doses to maintain blood drug levels does not consider any distinctive effects that SSRIs may have on the central nervous system of reproductive women, and assumes that their brain serotonin system is identical to non-reproductive women. The handful of studies detailed immediately below demonstrates that this is not the case.
Pregnancy and the postpartum period involve some of the most dramatic neurobiological modifications that can occur in adulthood, and these modifications collectively facilitate a mother’s ability to care for her young (Galea et al. 2014; Gammie et al. 2016; Kim et al. 2016; Leuner and Sabihi 2016). However, there has been little attention to how the brain’s serotonin system is naturally affected by female reproduction, even though it is known to be sensitive to experimental manipulations of ovarian hormones in female rodents and monkeys (Bethea et al., 2002; Chavez et al. 2010; Donner and Handa 2009; Fink et al. 1996; Inagaki et al. 2010). A number of studies have reported that female reproduction normatively upregulates central serotonergic activity. Women in their second trimester of pregnancy or at term have higher cerebrospinal fluid serotonin metabolites compared to non-pregnant women (Spielman et al. 1985), and pregnant or postpartum women have higher plasma serotonin than do non-reproducing women (Sekiyama et al. 2013). Seemingly inconsistent with these results are other studies finding that late pregnancy and the early postpartum period are associated with relatively low serum levels of the serotonin precursor, tryptophan (Handley et al. 1980; Badawy 2014; Maes et al. 2002; Veen et al., 2016). Although reduced plasma tryptophan may be expected to reduce the capacity for brain serotonin synthesis (Fernstrom and Wurtman 1971), it is important to note that plasma trytophan alone does not dictate the brain’s capacity to produce serotonin (Fernstrom and Wurtman 1972).
In laboratory rats, serotonin cell firing in the midbrain dorsal raphe is higher in pregnant and early postpartum females when compared to cycling females (Klink et al. 2002), and we have found that dorsal raphe levels of tryptophan hydroxylase 2 (TPH2; the rate-limiting enzyme for central serotonin synthesis) and serotonin metabolism (as indicated by the serotonin metabolite 5-hydroxyindoleacetic acid; 5HIAA) are higher in early postpartum rats compared to diestrus, nulliparous females (Harding and Lonstein 2016; Holschbach and Lonstein 2016). Early postpartum rats also have non-statistically significant, but considerably higher (> 30%), SERT in their dorsal raphe compared to non-maternal female rats (Harding and Lonstein 2016). On the other hand, a study using a small sample of postpartum day 10 laboratory mice found that these females had less serotonin immunoreactivity in their dorsal raphe compared to cycling females (Jury et al. 2015). We did not find this difference in dorsal raphe serotonin immunoreactivity in a large study of laboratory rats sacrificed as diestrous virgins or on postpartum days 8 or 19 (Holschbach and Lonstein 2016), though, perhaps suggesting species-specific effects of female reproduction on the midbrain serotonin system. At the serotonin receptor level, we recently found > 50% less excitatory serotonin 2C receptor mRNA expression in the postpartum rat dorsal raphe compared to females sacrificed during the estrus cycle or mid-pregnancy (Vitale et al. 2017). Because the serotonin 2C receptor is often found on inhibitory GABAergic cells in the dorsal raphe (Serrats et al., 2005), its reduced expression likely contributes to the elevated dorsal raphe serotonin cell excitability and output during late pregnancy and the early postpartum period (Boothman et al. 2006). Not only is the midbrain serotonin system affected by female reproduction, but frontocortical serotonin content and turnover rises across pregnancy and then falls postpartum in rats (Desan et al. 1988; Glaser et al. 1990), and serotonin turnover in two basal forebrain sites involved in maternal caregiving and anxiety (i.e., the medial preoptic area and bed nucleus of the stria terminalis) is higher in postpartum rats compared to diestrous virgin females (Lonstein et al. 2003; Smith et al. 2013).
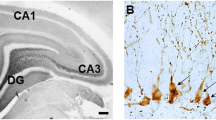
These motherhood-induced neurochemical changes in the serotonin system are accompanied by neuroplastic changes. Contrary to early thinking that the adult mammalian brain is extremely limited in its neuroplasticity, remarkable alterations in brain cell birth, survival, differentiation, and death are now known to continue throughout the lifespan and particularly during times of hormone-induced neurobehavioral flux (Sisk et al. 2013). For instance, a number of research groups have shown in laboratory rodents and sheep that giving birth and interacting with young affect the proliferation of newborn cells in the subgranular zone (SGZ) of the hippocampus, as well as the survival of those cells after they migrate to the nearby granule cell layer (Leuner and Sabihi, 2016; Lévy et al. 2017; Pawluski and Galea 2007). The functional significance of motherhood-induced changes in hippocampal cell birth and survival are unknown, but they may partly underlie how the hippocampus is involved in the blunted hypothalamic-pituitary adrenal (HPA) axis response to stress during pregnancy and postpartum (Brunton et al. 2008). Female reproduction also affects the number of cells born in the subventricular zone (SVZ) that lines the walls of lateral ventricles, from which the cells migrate to the main olfactory bulb and contribute to the postpartum display of maternal caregiving behaviors (Corona et al. 2017; Furuta and Bridges 2005; Larsen and Grattan 2010; Shingo et al. 2003).
While the far majority of studies of adult brain cell proliferation and survival have focused on the SGZ/hippocampus and SVZ/main olfactory bulb, a number of other adult brain regions do contain newborn cells (Akbari et al. 2007; Lévy et al. 2017). We recently found that this includes the midbrain dorsal raphe. By using systemic injections of the thymidine analogue, bromodeoxyuridine (Brdu), to later identify mitotic cells in the dorsal raphe of different groups of adult nulliparous, pregnant, and postpartum rats, we found that Brdu-containing cells born during the early postpartum period were less likely to survive almost 2 weeks later into late lactation when compared to cells that were born during late pregnancy (Holschbach and Lonstein 2016). Cytogenesis in the adult dorsal raphe had not previously been reported in any animal, but it was not completely unexpected because the lining of the cerebral aqueduct lying just above the dorsal raphe is a highly proliferative niche generating midbrain cells during other developmental epochs (Arenas et al. 2015). The differences we found between pregnancy-born and postpartum-born dorsal raphe cells in their survival were paralleled by dorsal raphe immunoreactivity for the cell differentiation factor, NeuroD, and many of the surviving cells could in fact be phenotyped as young neurons (Holschbach and Lonstein 2016). The relatively low survival of cells born in the early postpartum dorsal raphe required that mothers interacted with pups, because removing the litter soon after parturition increased dams’ newborn cell survival. Consistent with the ability of early litter removal to increase newborn cell survival in the maternal dorsal raphe, dams whose litters were removed at parturition also showed less programmed cell death (i.e., apoptosis) compared to dams that remained with their offspring (Holschbach and Lonstein 2016). It may seem surprising to some readers that we found that motherhood is associated with lower dorsal raphe newborn cell survival and higher cell death. Regressive events such as cell death and synaptic pruning are essential for refining and optimizing neural circuit function (Chechik et al. 1999; Fricker et al. 2018), and thus are surely relevant for neurobehavioral changes across the peripartum period and lactation (Pereira 2016). Whether the motherhood-related neuroplasticity we found in the dorsal raphe is a cause, result, or unrelated to the motherhood-related serotonin changes there and elsewhere in the brain remains to be determined.
The studies discussed above reveal a number of normative neurochemical and cellular changes in the serotonin system across female reproduction, but we know almost nothing about how these normative changes may be derailed by stress, or if stress can produce completely novel effects on this system. The dorsal raphe and other serotonin cell groups are rich in the receptors for stress-related hormones such us glucocorticoids and corticotrophin releasing hormone (CRH), and receive direct neuronal input from CRH cells in the amygdala, bed nucleus of the stria terminalis, and paraventricular nucleus of the hypothalamus (Aaronson et al. 1988; Fox and Lowry 2013). This is relevant because pregnancy stress is strongly associated with prepartum and postpartum affective disorders in women (Britton 2008; Lancaster et al. 2010; Robertson et al. 2004; Soderquist et al. 2009) and stress produces these effects, in part, by interacting with serotonin (Bethea et al. 2013; Costas et al. 2010; Mehta et al. 2012; Mitchell et al. 2011; Pinheiro et al. 2013). Pregnancy stress can also increase later postpartum depression- and anxiety-like behaviors in laboratory rodents (Darnaudery et al. 2004; Haim et al. 2014; Hillerer et al. 2011; Leuner et al. 2014; O'Mahony et al. 2006; Smith et al. 2004; although see Pawluski et al. 2011, 2012a), but only two studies have examined if pregnancy stress alters any aspect of the maternal central serotonin system. These studies found that stressed postpartum dams had higher serotonin turnover in the cortex (Gemmel et al. 2016) and lower cortical and hippocampal serotonin 1A receptor expression (Szewczyk et al. 2014), compared to unstressed dams when the subjects’ brains were assessed in late lactation. Relevant to SSRI’s/serotonin’s downstream effects on neurotrophic factors, pregnancy stress in rodents has also been found to reduce BDNF levels in the maternal hippocampus and cortex (Maghsoudi et al. 2014; Miao et al. 2018), as well as atrophy neuronal dendrites in the maternal hippocampus and nucleus accumbens (Haim et al. 2014; Pawluski et al. 2012b).
It is mostly unknown if the neurochemical and cellular changes in the serotonin system across reproduction described above affect mothers’ physiological or behavioral responses to SSRIs. It was recently found that the SSRI fluoxetine decreases body weight, lowers circulating cortisol, and increases neurogenesis in the hippocampus of nulliparous rats but not in postpartum mothers (Workman et al. 2016). On the other hand, only in mothers did fluoxetine interact with cortisol to reduce circulating estradiol (Workman et al. 2016). The parity difference in fluoxetine's effect on cortisol is particularly interesting given the association between hypothalamic-pituitary-adrenal axis dysfunction and some types of depression in non-parous humans (Stetler and Miller 2011). Studies in mice have revealed parity differences in the behavioral responses to an SSRI, with citalopram decreasing the latency for postpartum mothers but not nulliparous females to become immobile in a forced-swim test - a common paradigm used to assess depressive-like behavioral dispair in laboratory rodents (Jury et al. 2015). In rats, though, the high immobility in the forced-swim test shown by both mothers and nullipare treated with corticosterone can be reversed by fluoxetine (Workman et al. 2016).
In sum, SSRI use is widespread during pregnancy and the early postpartum period, and there is no reason to expect that this will change anytime soon (Hanley and Mintzes 2014). There are relatively few studies of the normative and stress-induced changes in the central serotonin system across female reproduction in either humans or laboratory rodents, but this information is critical for understanding how serotonin and its downstream effects on neuroplasticity and other brain processes contribute to the etiology of postpartum depression and anxiety. Understanding the unique aspects of the maternal serotonin system is also essential for optimizing the dose and timing of SSRIs, or any other pharmacotherapies affecting the brain’s serotonin system, when they are to be used as potential treatments for prepartum and postpartum affective disorders.
References
Adachi M, Autry AE, Mahgoub M, Suzuki K, Monteggia LM (2017) TrkB signaling in dorsal raphe nucleus is essential for antidepressant efficacy and normal aggression behavior. Neuropsychopharmacology 42(4):886–894
Akbari EM, Chatterjee D, Lévy F, Fleming AS (2007) Experience-dependent cell survival in the maternal rat brain. Behav Neurosci 121(5):1001–1011
Alwan S, Reefhuis J, Rasmussen SA, Friedman JM, National Birth Defects Prevention Study (2011) Patterns of antidepressant medication use among pregnant women in a United States population. J Clin Pharmacol 51(2):264–270
Anderson GD (2006) Using pharmacokinetics to predict the effects of pregnancy and maternal-infant transfer of drugs during lactation. Exp Opin Drug Metabol Toxicol 2(6):947–960
Andrade SE, Raebel MA, Brown J, Lane K, Livingston J, Boudreau D, Rolnick SJ, Roblin D, Smith DH, Dal Pan GJ, Scott PE, Platt R (2008) Use of antidepressant medications during pregnancy: a multisite study. Am J Obstet Gynecol 198(2):194 e191–195
Appleby L (1998) Violent suicide and obstetric complications The link is mental illness. Br Med J 317(7169):1333–1334
Arenas E, Denham M, Villaescusa JC (2015) How to make a midbrain dopaminergic neuron. Development 142(11):1918–1936
Badawy AA (2014) The tryptophan utilization concept in pregnancy. Obstet Gynecol Sci 57(4):249–259
Bérard A, Gaedigk A, Sheehy O, Chambers C, Roth M, Bozzo P, Johnson D, Kao K, Lavigne S, Wolfe L, Quinn D, Dieter K, Zhao JP, OTIS (MotherToBaby) Collaborative Research Committee (2017) Association between CYP2D6 genotypes and the risk of antidepressant discontinuation, dosage modification and the occurrence of maternal depression during pregnancy. Front Pharmacol 17(8):402
Bethea CL, Lu NZ, Gundlah C, Streicher JM (2002) Diverse actions of ovarian steroids in the serotonin neural system. Front Neuroendocrinol 23:41–100
Bethea CL, Phu K, Reddy AP, Cameron JL (2013) The effect of short-term stress on serotonin gene expression in high and low resilient macaques. Prog Neuro-Psychopharmacol Biol Psychiat 44:143–153
Boothman L, Raley J, Denk F, Hirani E, Sharp T (2006) In vivo evidence that 5-HT(2C) receptors inhibit 5-HT neuronal activity via a GABAergic mechanism. Br J Pharmacol 149(7):861–869
Britton JR (2008) Maternal anxiety: course and antecedents during the early postpartum period. Depress Anx 25(9):793–800
Brunton PJ, Russell JA, Douglas AJ (2008) Adaptive responses of the maternal hypothalamic-pituitary-adrenal axis during pregnancy and lactation. J Neuroendocrinol 20(6):764–776
Charlton RA, Jordan S, Pierini A, Garne E, Neville AJ, Hansen AV, Gini R, Thayer D, Tingay K, Puccini A, Bos HJ, Nybo Andersen AM, Sinclair M, Dolk H, de Jong-van den Berg LT (2015) Selective serotonin reuptake inhibitor prescribing before, during and after pregnancy: a population-based study in six European regions. Brit J Obstet Gynaecol 122(7):1010–1020
Chavez C, Hollaus M, Scarr E, Pavey G, Gogos A, van den Buuse M (2010) The effect of estrogen on dopamine and serotonin receptor and transporter levels in the brain: an autoradiography study. Brain Res 1321:51–59
Chechik G, Meilijson I, Ruppin E (1999) Neuronal regulation: a mechanism for synaptic pruning during brain maturation. Neural Comput 11(8):2061–2080
Chesney E, Goodwin GM, Fazel S (2014) Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiat 13(2):153–160
Committee on Obstetric Practice (2015) The American College of Obstetricians and Gynecologists Committee Opinion no. 630. Screening for perinatal depression. Obstet Gynecol 125(5):1268–1271
Corona R, Meurisse M, Cornilleau F, Moussu C, Keller M, Lévy F (2017) Exposure to young preferentially activates adult-born neurons in the main olfactory bulb of sheep mothers. Brain Struct Funct 222(3):1219–1229
Costas J, Gratacos M, Escaramis G, Martín-Santos R, de Diego Y, Baca-García E, Canellas F, Estivill X, Guillamat R, Guitart M, Gutiérrez-Zotes A, García-Esteve L, Mayoral F, Moltó MD, Phillips C, Roca M, Carracedo A, Vilella E, Sanjuán J (2010) Association study of 44 candidate genes with depressive and anxiety symptoms in post-partum women. J Psychiat Res 44(11):717–724
De Crescenzo F, Perelli F, Armando M, Vicari S (2014) Selective serotonin reuptake inhibitors (SSRIs) for post-partum depression (PPD): a systematic review of randomized clinical trials. J Affect Disord 152-154:39–44
Darnaudery M, Dutriez I, Viltart O, Morley-Fletcher S, Maccari S (2004) Stress during gestation induces lasting effects on emotional reactivity of the dam rat. Behav Brain Res 153(1):211–216
Davé S, Petersen I, Sherr L, Nazareth I (2010) Incidence of maternal and paternal depression in primary care: a cohort study using a primary care database. Arch Pediatr Adolesc Med 164(11):1038–1044
Desan PH, Woodmansee WW, Ryan SM, Smock TK, Maier SF (1988) Monoamine neurotransmitters and metabolites during the estrous cycle, pregnancy, and the postpartum period. Pharmacol Biochem Behav 30(3):563–568
Donner N, Handa RJ (2009) Estrogen receptor beta regulates the expression of tryptophan-hydroxylase 2 mRNA within serotonergic neurons of the rat dorsal raphe nuclei. Neuroscience 163(2):705–718
Drury SS, Scaramella L, Zeanah CH (2016) The neurobiological impact of postpartum maternal depression: prevention and intervention approaches. Child Adol Psych 25(2):179–200
Fairbrother N, Janssen P, Antony MM, Tucker E, Young AH (2016) Perinatal anxiety disorder prevalence and incidence. J Affect Disord 200:148–155
Fernstrom JD, Wurtman RJ (1971) Brain serotonin content: physiological dependence on plasma tryptophan levels. Science 173(3992):149–152
Fernstrom JD, Wurtman RJ (1972) Brain serotonin content: physiological regulation by plasma neutral amino acids. Science 178(4059):414–416
Field T (2010) Postpartum depression effects on early interactions, parenting, and safety practices: a review. Inf Behav Dev 33(1):1–6
Fox JH, Lowry CA (2013) Corticotropin-releasing factor-related peptides, serotonergic systems, and emotional behavior. Front Neurosci 7:169
Freeman MP, Nolan PE, Davis MF, Anthony M, Fried K, Fankhauser M, Woosley RL, Moreno F (2008) Pharmacokinetics of sertraline across pregnancy and postpartum. J Clin Psychopharmacol 28(6):646–653
Fink G, Sumner BE, Rosie R, Grace O, Quinn JP (1996) Estrogen control of central neurotransmission: Effect on mood, mental state, and memory. Cell Mol Neurobiol 16(3):325–344
Fricker M, Tolkovsky AM, Borutaite V, Coleman M, Brown GC (2018) Neuronal cell death. Physiol Rev 98(2):813–880
Furuta M, Bridges RS (2005) Gestation-induced cell proliferation in the rat brain. Brain Res Dev Brain Res 156(1):61–6
Galea LA, Leuner B, Slattery DA (2014) Hippocampal plasticity during the peripartum period: influence of sex steroids stress and ageing. J Neuroendocrinol 26(10):641–648
Gammie SC, Driessen TM, Zhao C, Saul MC, Eisinger BE (2016) Genetic and neuroendocrine regulation of the postpartum brain. Front Neuroendocrinol 42:1–17
Gemmel M, Rayen I, van Donkelaar E, Loftus T, Steinbusch HW, Kokras N, Dalla C, Pawluski JL (2016) Gestational stress and fluoxetine treatment differentially affect plasticity, methylation and serotonin levels in the PFC and hippocampus of rat dams. Neuroscience 327:32–43
Glaser J, Russell VA, de Villiers AS, Searson JA, Taljaard JJ (1990) Rat brain monoamine and serotonin S2 receptor changes during pregnancy. Neurochem Res 15(10):949–956
Glasheen C, Richardson GA, Fabio A (2010) A systematic review of the effects of postnatal maternal anxiety on children. Arch Women’s Mental Health 13(1):61–74
Glover ME, Clinton SM (2016) Of rodents and humans: a comparative review of the neurobehavioral effects of early life SSRI exposure in preclinical and clinical research. Int J Dev Neurosci 51:50–72
Goodman JH, Watson GR, Stubbs B (2016) Anxiety disorders in postpartum women: a systematic review and meta-analysis. J Affect Disord 203:292–331
Haase J, Brown E (2015) Integrating the monoamine, neurotrophin and cytokine hypotheses of depression—a central role for the serotonin transporter? Pharmacol Therap 147:1–11
Haim A, Sherer M, Leuner B (2014) Gestational stress induces persistent depressive-like behavior and structural modifications within the postpartum nucleus accumbens. Eur J Neurosci 40(12):3766–3773
Handley SL, Dunn TL, Waldron G, Baker JM (1980) Tryptophan, cortisol and puerperal mood. British J Psychiatry 136:498–508
Hanley GE, Mintzes B (2014) Patterns of psychotropic medicine use in pregnancy in the United States from 2006 to 2011 among women with private insurance. BMC Preg Childbirth 14:242
Harding KM, Lonstein JS (2016) Extensive juvenile “babysitting” facilitates later adult maternal responsiveness, decreases anxiety, and increases dorsal raphe tryptophan hydroxylase-2 expression in female laboratory rats. Dev Psychobiol 58(4):492–508
Heikkinen T, Ekblad U, Kero P, Ekblad S, Laine K (2002) Citalopram in pregnancy and lactation. Clin Pharmacol Ther 72(2):184–191
Hillerer KM, Reber SO, Neumann ID, Slattery DA (2011) Exposure to chronic pregnancy stress reverses peripartum-associated adaptations: implications for postpartum anxiety and mood disorders. Endocrinology 152(10):3930–3940
Holmes A, Yang RJ, Murphy DL, Crawley JN (2002) Evaluation of antidepressant-related behavioral responses in mice lacking the serotonin transporter. Neuropsychopharmacology 27(6):914–923
Holschbach MA, Lonstein JS (2016) Motherhood and infant contact regulate neuroplasticity in the serotonergic midbrain dorsal raphe. Psychoneuroendocrinology 76:97–106
Horne MK, Lee J, Chen F, Lanning K, Tomas D, Lawrence AJ (2008) Long-term administration of cocaine or serotonin reuptake inhibitors results in anatomical and neurochemical changes in noradrenergic, dopaminergic, and serotonin pathways. J Neurochem 106(4):1731–1744
Hostetter A, Stowe ZN, Strader JR Jr, McLaughlin E, Llewellyn A (2000) Dose of selective serotonin uptake inhibitors across pregnancy: clinical implications. Depress Anx 11(2):51–57
Huybrechts KF, Palmsten K, Mogun H, Kowal M, Avorn J, Setoguchi-Iwata S, Hernández-Díaz S (2013) National trends in antidepressant medication treatment among publicly insured pregnant women. Gen Hosp Psych 35(3):265–271
Inagaki T, Gautreaux C, Luine V (2010) Acute estrogen treatment facilitates recognition memory consolidation and alters monoamine levels in memory-related brain areas. Horm Behav 58(3):415–426
Jury NJ, McCormick BA, Horseman ND, Benoit SC, Gregerson KA (2015) Enhanced responsiveness to selective serotonin reuptake inhibitors during lactation. PLoS One 10(2):e0117339
Kalueff AV, Fox MA, Gallagher PS, Murphy DL (2007) Hypolocomotion, anxiety and serotonin syndrome-like behavior contribute to the complex phenotype of serotonin transporter knockout mice. Genes Brain Behav 6(4):389–400
Kim P, Strathearn L, Swain JE (2016) The maternal brain and its plasticity in humans. Horm Behav 77:113–123
Klink R, Robichaud M, Debonnel G (2002) Gender and gonadal status modulation of dorsal raphe nucleus serotonergic neurons. Part I: effects of gender and pregnancy. Neuropharmacology 43(7):1119–1128
Lancaster CA, Gold KJ, Flynn HA, Yoo H, Marcus SM, Davis MM (2010) Risk factors for depressive symptoms during pregnancy: a systematic review. Amer J Obstet Gynecol 202(1):5–14
Larsen CM, Grattan DR (2010) Prolactin-induced mitogenesis in the subventricular zone of the maternal brain during early pregnancy is essential for normal postpartum behavioral responses in the mother. Endocrinology 151(8):3805–3814
Le Strat Y, Dubertret C, Le Foll B (2011) Prevalence and correlates of major depressive episode in pregnant and postpartum women in the United States. J Affect Disord 135(1–3):128–138
Leuner B, Sabihi S (2016) The birth of new neurons in the maternal brain: hormonal regulation and functional implications. Front Neuroendocrinol 41:99–113
Leuner B, Fredericks PJ, Nealer C, Albin-Brooks C (2014) Chronic gestational stress leads to depressive-like behavior and compromises medial prefrontal cortex structure and function during the postpartum period. PLoS One 9(3):e89912
Lévy F, Batailler M, Meurisse M, Migaud M (2017) Adult neurogenesis in sheep: characterization and contribution to reproduction and behavior. Front Neurosci 11:570
Li Y, Luikart BW, Birnbaum S et al (2008) TrkB regulates hippocampal neurogenesis and governs sensitivity to antidepressive treatment. Neuron 59(3):399–412
Lira A, Zhou M, Castanon N, Ansorge MS, Gordon JA, Francis JH, Bradley-Moore M, Lira J, Underwood MD, Arango V, Kung HF, Hofer MA, Hen R, Gingrich JA (2003) Altered depression-related behaviors and functional changes in the dorsal raphe nucleus of serotonin transporter-deficient mice. Biol Psychiatry 54(10):960–971
Lonstein JS, Dominguez JM, Putnam SK, De Vries GJ, Hull EM (2003) Intracellular preoptic and striatal monoamines in pregnant and lactating rats: possible role in maternal behavior. Brain Res 970(1–2):149–158
Lowry CA, Evans AK, Gasser PJ, Hale MW, Staub DR, Shekhar A (2008) Topographic organization and chemoarchitecture of the dorsal raphe nucleus and the median raphe nucleus. In: Monti JM, Pandi-Perumal SR, Jacobs BL, Nutt DJ (eds) Serotonin and sleep: molecular, functional and clinical aspects. Birkhäuser Verlag, Switzerland
Lupattelli A, Spigset O, Twigg MJ, Zagorodnikova K, Mårdby AC, Moretti ME, Drozd M, Panchaud A, Hämeen-Anttila K, Rieutord A, Gjergja Juraski R, Odalovic M, Kennedy D, Rudolf G, Juch H, Passier A, Björnsdóttir I, Nordeng H (2014) Medication use in pregnancy: a cross-sectional, multinational web-based study. BMJ Open 4(2):e004365
Maes M, Verkerk R, Bonaccorso S, Ombelet W, Bosmans E, Scharpe S (2002) Depressive and anxiety symptoms in the early puerperium are related to increased degradation of tryptophan into kynurenine, a phenomenon which is related to immune activation. Life Sci 71(16):1837–1848
Maghsoudi N, Ghasemi R, Ghaempanah Z, Ardekani AM, Nooshinfar E, Tahzibi A (2014) Effect of chronic restraint stress on HPA axis activity and expression of BDNF and Trkb in the hippocampus of pregnant rats: possible contribution in depression during pregnancy and postpartum period. Basic Clin Neurosci 5(2):131–137
McDonagh MS, Matthews A, Phillipi C, Romm J, Peterson K, Thakurta S, Guise JM (2014) Depression drug treatment outcomes in pregnancy and the postpartum period: a systematic review and meta-analysis. Obstet Gynecol 124(3):526–534
Mehta D, Quast C, Fasching PA, Seifert A, Voigt F, Beckmann MW, Faschingbauer F, Burger P, Ekici AB, Kornhuber J, Binder EB, Goecke TW (2012) The 5-HTTLPR polymorphism modulates the influence on environmental stressors on peripartum depression symptoms. J Affect Disord 136(3):1192–1197
Miao Z, Mao F, Liang J, Szyf M, Wang Y, Sun ZS (2018) Anxiety-related behaviours associated with microRNA-206-3p and BDNF expression in pregnant female mice following psychological social stress. Mol Neurobiol 55(2):1097–1111
Mitchell C, Notterman D, Brooks-Gunn J, Hobcraft J, Garfinkel I, Jaeger K, Kotenko I, McLanahan S (2011) Role of mother’s genes and environment in postpartum depression. Proc Nat Acad Sci USA 108(20):8189–8193
Molyneaux E, Trevillion K, Howard LM (2015) Antidepressant treatment for postnatal depression. JAMA 313(19):1965–1966
Monteggia LM, Barrot M, Powell CM, Berton O, Galanis V, Gemelli T, Meuth S, Nagy A, Greene RW, Nestler EJ (2004) Essential role of brain-derived neurotrophic factor in adult hippocampal function. Proc Nat Acad Sci USA 101(29):10827–10832
Munk-Olsen T, Gasse C, Laursen TM (2012) Prevalence of antidepressant use and contacts with psychiatrists and psychologists in pregnant and postpartum women. Acta Psych Scand 125(4):318–324
Oberlander TF, Gingrich JA, Ansorge MS (2009) Sustained neurobehavioral effects of exposure to SSRI antidepressants during development: molecular to clinical evidence. Clin Pharmacol Ther 86(6):672–677
O'Connor E, Rossom RC, Henninger M, Groom HC, Burda BU (2016) Primary care screening for and treatment of depression in pregnant and postpartum women: evidence report and systematic review for the US Preventive Services Task Force. JAMA 315(4):388–406
O'Hara MW, Zekoski EM, Philipps LH, Wright EJ (1990) Controlled prospective study of postpartum mood disorders: comparison of childbearing and nonchildbearing women. J Abnorm Psychol 99(1):3–15
Olivier JD, Van Der Hart MG, Van Swelm RP, Dederen PJ, Homberg JR, Cremers T, Deen PM, Cuppen E, Cools AR, Ellenbroek BA (2008) A study in male and female 5-HT transporter knockout rats: an animal model for anxiety and depression disorders. Neuroscience 152(3):573–584
O'Mahony SM, Myint AM, van den Hove D, Desbonnet L, Steinbusch H, Leonard BE (2006) Gestational stress leads to depressive-like behavioural and immunological changes in the rat. Neuroimmunomodulation 13(2):82–88
Pariente G, Leibson T, Carls A, Adams-Webber T, Ito S, Koren G (2016) Pregnancy-associated changes in pharmacokinetics: a systematic review. PLoS Med 13(11):e1002160
Pawluski JL, Galea LA (2007) Reproductive experience alters hippocampal neurogenesis during the postpartum period in the dam. Neuroscience 149(1):53–67
Pawluski JL, van den Hove DL, Rayen I, Prickaerts J, Steinbusch HW (2011) Stress and the pregnant female: impact on hippocampal cell proliferation, but not affective-like behaviors. Horm Behav 59(4):572–580
Pawluski JL, Charlier TD, Fillet M, Houbart V, Crispin HT, Steinbusch HW, van den Hove DL (2012a) Chronic fluoxetine treatment and maternal adversity differentially alter neurobehavioral outcomes in the rat dam. Behav Brain Res 228(1):159–168
Pawluski JL, Valenca A, Santos AI, Costa-Nunes JP, Steinbusch HW, Strekalova T (2012b) Pregnancy or stress decrease complexity of CA3 pyramidal neurons in the hippocampus of adult female rats. Neuroscience 227:201–210
Pereira M (2016) Structural and functional plasticity in the maternal brain circuitry. New Dir Child Adolesc Dev 2016(153):23–46
Pinheiro RT, Coelho FM, Silva RA, et al. (2013) Association of a serotonin transporter gene polymorphism (5-HTTLPR) and stressful life events with postpartum depressive symptoms: a population-based study. J Psychosomatic Obstet Gynaecol 34(1):29–33
Pittenger C, Duman RS (2008) Stress, depression, and neuroplasticity: a convergence of mechanisms. Neuropsychopharmacology 33(1):88–109
Reck C, Struben K, Backenstrass M et al (2008) Prevalence, onset and comorbidity of postpartum anxiety and depressive disorders. Acta Psychiat Scand 118(6):459–468
Robertson E, Grace S, Wallington T, Stewart DE (2004) Antenatal risk factors for postpartum depression: a synthesis of recent literature. Gen Hosp Psych 26(4):289–295
Ruhé HG, Ooteman W, Booij J, Michel MC, Moeton M, Baas F, Schene AH (2009) Serotonin transporter gene promoter polymorphisms modify the association between paroxetine serotonin transporter occupancy and clinical response in major depressive disorder. Pharmacogenet Genomics 19(1):67–76
Saarelainen T, Hendolin P, Lucas G, Koponen E, Sairanen M, MacDonald E, Agerman K, Haapasalo A, Nawa H, Aloyz R, Ernfors P, Castrén E (2003) Activation of the TrkB neurotrophin receptor is induced by antidepressant drugs and is required for antidepressant-induced behavioral effects. J Neurosci 23(1):349–357
Sekiyama T, Nakatani Y, Yu X, Seki Y, Sato-Suzuki I, Arita H (2013) Increased blood serotonin concentrations are correlated with reduced tension/anxiety in healthy postpartum lactating women. Psych Res 209(3):560–565
Serrats J, Mengod G, Cortés R (2005) Expression of serotonin 5-HT2C receptors in GABAergic cells of the anterior raphe nuclei. J Chem Neuroanat 29(2):83–91
Serretti A, Kato M (2008) The serotonin transporter gene and effectiveness of SSRIs. Expert Rev Neurotherpeutics 8(1):111–120
Shingo T, Gregg C, Enwere E, Fujikawa H, Hassam R, Geary C, Cross JC, Weiss S (2003) Pregnancy-stimulated neurogenesis in the adult female forebrain mediated by prolactin. Science 299(5603):117–120
Sisk CL, Lonstein JS, Gore AC (2013) Hormonal influences on neurobehavioral transitions across the lifespan. In: Neuroscience in the 21st century: basic and clinical. Pfaff DW, Supervisory Editor (Neuroendocrinology). Springer Press, pp 1715–1752. https://doi.org/10.1007/978-1-4614-1997-6_61
Sit DK, Perel JM, Helsel JC, Wisner KL (2008) Changes in antidepressant metabolism and dosing across pregnancy and early postpartum. J Clin Psychiatry 69(4):652–658
Sit D, Perel JM, Luther JF, Wisniewski SR, Helsel JC, Wisner KL (2010) Disposition of chiral and racemic fluoxetine and norfluoxetine across childbearing. J Clin Psychopharmacol 30(4):381–6
Smith JW, Seckl JR, Evans AT, Costall B, Smythe JW (2004) Gestational stress induces post-partum depression-like behaviour and alters maternal care in rats. Psychoneuroendocrinology 29(2):227–244
Smith CD, Piasecki CC, Weera M, Olszewicz J, Lonstein JS (2013) Noradrenergic alpha-2 receptor modulators in the ventral bed nucleus of the stria terminalis: effects on anxiety behavior in postpartum and virgin female rats. Behav Neurosci 127(4):582–597
Soderquist J, Wijma B, Thorbert G, Wijma K (2009) Risk factors in pregnancy for post-traumatic stress and depression after childbirth. Brit J Obstet Gynaecol 116(5):672–680
Spielman FJ, Mueller RA, Corke BC (1985) Cerebrospinal fluid concentration of 5-hydroxyindoleactic acid in pregnancy. Anesthesiology 62(2):193–195
Stein A, Pearson RM, Goodman SH, Rapa E, Rahman A, McCallum M, Howard LM, Pariante CM (2014) Effects of perinatal mental disorders on the fetus and child. Lancet 384(9956):1800–1819
Stetler C, Miller GE (2011) Depression and hypothalamic-pituitary-adrenal activation: a quantitative summary of four decades of research. Psychosomatic Med 73(2):114–126
Szewczyk B, Kotarska K, Daigle M, Misztak P, Sowa-Kucma M, Rafalo A, Curzytek K, Kubera M, Basta-Kaim A, Nowak G, Albert PR (2014) Stress-induced alterations in 5-HT1A receptor transcriptional modulators NUDR and Freud-1. Int J Neuropsychopharmacol 17(11):1763–1775
Veen C, Myint AM, Burgerhout KM, Schwarz MJ, Schütze G, Kushner SA, Hoogendijk WJ, Drexhage HA, Bergink V (2016) Tryptophan pathway alterations in the postpartum period and in acute postpartum psychosis and depression. J Affect Dis 189:298–305
Ververs FF, Voorbij HA, Zwarts P, Belitser SV, Egberts TC, Visser GH, Schobben AF (2009) Effect of cytochrome P450 2D6 genotype on maternal paroxetine plasma concentrations during pregnancy. Clin Pharmacokinet 48(10):677–683
Vitale EM, Washington CL, Lonstein JS (2017) Female reproductive state influences raphe and forebrain serotonin 1A, 2A, and 2C receptor expression. Soc Neurosci Abstr 782:04
Weisskopf E, Fischer CJ, Bickle Graz M, Morisod Harari M, Tolsa JF, Claris O, Vial Y, Eap CB, Csajka C, Panchaud A (2015) Risk-benefit balance assessment of SSRI antidepressant use during pregnancy and lactation based on best available evidence. Exp Opin Drug Safety 14(3):413–427
Westin AA, Brekke M, Molden E, Skogvoll E, Spigset O (2017) Selective serotonin reuptake inhibitors and venlafaxine in pregnancy: changes in drug disposition. PLoS One 12(7):e0181082
Workman JL, Gobinath AR, Kitay NF, Chow C, Brummelte S, Galea LA (2016) Parity modifies the effects of fluoxetine and corticosterone on behavior, stress reactivity, and hippocampal neurogenesis. Neuropharmacology 105:443–453
Acknowledgements
The author would like to thank M. Allie Holschbach, Erika M. Vitale, Carl D. Smith, and Katie M. Harding for conducting the research from the author’s lab that was discussed in this review.
Funding
Some of the author’s research described herein was supported in part by NIH grants R01HD057962, NRSA F32MH099892, and NRSA F32MH83344.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that there is no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
This article is part of the Topical Collection on Neurobiology of Maternal Mental Illness
Guest Editor: Jodi Pawluski
Rights and permissions
About this article
Cite this article
Lonstein, J.S. The dynamic serotonin system of the maternal brain. Arch Womens Ment Health 22, 237–243 (2019). https://doi.org/10.1007/s00737-018-0887-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00737-018-0887-1