Abstract
Many sex and gender differences in schizophrenic psychoses have been reported, but few have been soundly replicated. A stable finding is the later age of onset in women compared to men. Gender differences in symptomatology, comorbidity, and neurocognition seem to reflect findings in the general population. There is increasing evidence for estrogens being psychoprotective in women and for hypothalamic–pituitary–gonadal dysfunction in both sexes.
More methodologically sound, longitudinal, multi-domain, interdisciplinary research investigating both sex (biological) and gender (psychosocial) factors is required to better understand the different pathogenesis and etiologies of schizophrenic psychoses in women and men, thereby leading to better tailored treatments and improved outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sex and gender differences in schizophrenia provide a compelling basis for both psychiatry research and clinical practice. Such differences have been described in the incidence and prevalence, age at onset, symptomatology and course of schizophrenic psychoses, as well as the so-called “premorbid” adjustment and emerging psychosis, cognitive functioning, brain morphology and functioning, and a variety of risk factors, such as familial risk, hormonal, and psychosocial influences (Riecher-Rössler and Häfner 2000; Riecher-Rössler et al. 2010; Ochoa et al. 2012; Canuso and Pandina 2007).
Sex and gender difference findings, however, are inconsistently reported—mainly due to methodological differences in studies. For example, the fact that some results are not derived from representative, population-based studies but rather come from selected help-seeking patient groups, does not allow to draw valid conclusions on “true sex and gender differences.” It is vital to clearly delineate consistent differences in schizophrenic psychoses, such as regarding age of onset, to truly understand the underlying causes of these serious mental disorders.
Recent research has shown that sex and gender differences might arise from a complex interplay between biological (mainly hormonal), and psychosocial factors. Promising, new strategies to both understand and treat schizophrenia involve the exploration of the impact of estrogens on the central nervous system and hence several clinical parameters associated with schizophrenic psychoses.
More research in this area is urgently needed including better translation between clinical and basic research. Gender and sex differences could be a window to explore the etiology of some of the pathogenic pathways leading to psychosis in general. This would also allow the development of new therapeutic strategies for these disorders both in general and specifically tailored to meet the needs of women and men with schizophrenia. Personalized medicine approaches in other fields are proving to be successful, and tailoring the treatment of schizophrenic psychoses for each person, taking the sex/gender of the patient into account, would be an important step forward.
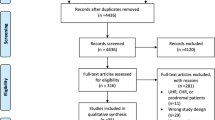
This review will focus on clinical aspects of sex and gender differences in schizophrenic psychoses and the potential underlying causes. Reviews focusing on sex differences in animal models can be found elsewhere (Ayhan et al. 2016; Hill 2016). We will primarily cite systematic reviews, meta-analyses, and more recent studies but also some older landmark studies (see Table 1). The term “sex” is used in describing biological aspects and “gender” for the psychosocial and cultural influences, while acknowledging that all these influences interact strongly and that sometimes both terms could be used. The plural term “schizophrenic psychoses” is used, because we believe it is a better descriptor for the broad term of “schizophrenia” which may actually comprise a group of disorders with different etiologies (Cuesta and Peralta 2008; Riecher-Rössler and Studerus 2016), possibly with a differing sex distribution.
The main goal of our review is to raise awareness of the importance of sex and gender differences in schizophrenic psychoses and to stimulate more methodologically sound research in this area.
Epidemiological and clinical sex and gender differences
Sex and gender differences in “schizophrenia” have been described for a long time. In particular, sex differences in the age at onset have been consistently described in many studies. Sex and gender differences in the incidence, symptomatology, cognitive functioning, or the course of the disease are less consistently reported.
Inconsistencies might partly be due to methodological problems. Many studies have not been community-based but were based on selected patient groups and are therefore not representative of all patients in a defined catchment area. This, however, would be a prerequisite for describing true sex and gender differences. The data gained from non-representative studies might be influenced by the differing help-seeking behaviors of both sexes and differing referral rates, i.e., selection into treatment (Walker and Lewine 1993). Furthermore, many studies have commented on the absence or presence of sex and gender differences, e.g., regarding symptomatology or cognition in psychoses, without studying untreated first-contact patients. Thus, the described sex/gender differences might partially be due not only to patient selection but also to treatment effects and other influencing factors as outlined subsequently.
Incidence and prevalence
Recent epidemiological studies report a slightly higher incidence of schizophrenia in men compared to women, with a risk ratio of about 1.4 (Aleman et al. 2003; McGrath et al. 2008), although previous studies had found equal incidence rates (Jablensky et al. 1992; Häfner et al. 1989, 1994). Differing results might be due to methodological issues as described previously. Furthermore, the incidence rates might be influenced by the diagnostic criteria applied, which can have broad or narrow definitions of schizophrenia. If, for example, schizoaffective psychoses are not included in studies, women might be underrepresented since they are more often diagnosed with schizoaffective disorder (Filatova et al. 2017) because they experience more affective symptoms (see subsequent discussions). An especially critical factor influencing the finding of sex differences in the incidence of schizophrenic psychoses is the diagnostic age limit applied. In older studies with an upper age limit of 45 years for the diagnosis of schizophrenia (as per DSM-III), men were usually described as having higher incidence rates, because these studies excluded a second peak of schizophrenia onset in women aged 45 years and older (see subsequent discussions). In studies where the upper age limit is set higher, the relative risk appears to be similar for both sexes (van der Werf et al. 2014; Häfner et al. 1989, 1991a, 1994). In two studies, Häfner and Riecher-Rössler examined all first hospitalized patients from two defined catchment areas—directly in the ABC study in Germany (Häfner et al. 1991a, 1993) and via a community-based case register in Denmark (Häfner et al. 1989). Both studies showed the same cumulative incidence rates for men and women, when the upper age limit for the diagnosis of schizophrenia was 60 years. In both studies, under age 40, the incidence was higher in men; after age 40, women had a higher incidence. Only 10% of all men had their first admission after age 40 compared with 21% of all women (Riecher-Rössler et al. 1997; Riecher-Rössler 2009).
More recently, van der Werf and colleagues performed a collaborative recalculation of 133,693 incidence cases of schizophrenia from 43 independent samples without a diagnostic age limit and showed an only slightly higher incidence in men than in women (odds ratio 1.15). This was mainly due to a higher risk for men in the group under age 40, whereas over age 50, the risk was higher in women (van der Werf et al. 2014). One study appeared after that review (Kühl et al. 2016) that was based on Danish case register data and showed a higher incidence in men. However, the age range for that study was a rather unusual 5–57 years. Interestingly, they reported an increasing incidence in women over the last decades, as did another epidemiological study (Filatova et al. 2017).
Regarding prevalence, no distinct sex/gender differences were found (Saha et al. 2005; McGrath et al. 2008). This disparity between incidence and prevalence seems astonishing but could be explained, for example, by the reported better treatment adherence by women (Ochoa et al. 2012; Cotton et al. 2009; Thorup et al. 2007).
Age of onset
The age at first onset of the disorder is on average significantly higher in women than in men. This difference has been shown in many studies quite consistently and worldwide (Aleman et al. 2003; Häfner et al. 1994; Jablensky et al. 1992; van der Werf et al. 2014; Leung et al. 2000; Canuso and Pandina 2007; Eranti et al. 2013; Häfner et al. 1989). Mean age at onset differs on average by 1–5 years, and this difference is already evident at the first onset of signs and symptoms of the disease and is not just due to a delay in help seeking or hospital admission (Eranti et al. 2013; Häfner et al. 1989, 1991a, 1993). In the ABC study, which was unfortunately not included in the meta-analysis by Eranti et al. (2013), data on men showed a peak of first admissions in their early twenties compared with women in their late twenties. Most importantly, women had a second smaller peak of first admission after age 40 (Häfner et al. 1989, 1993) (see Fig. 1). This was true for broadly defined (ICD-9: 295, 297, 298.3, 298.4) as well as for narrowly defined (ICD-9: 295 only) schizophrenia. So-called “late-onset” schizophrenia occurred twice as often in women as in men in the ABC study (Riecher-Rössler 1994; Riecher-Rössler et al. 1997). This second peak of onsets in women has also been shown in a recent meta-analysis (Kirkbride et al. 2012).
Interestingly, the sex difference in age of onset seems to disappear in patients with a family history of psychosis (Esterberg et al. 2010). Some, but not all, recent studies suggest that the earlier age of onset in men is at least partly due to their higher cannabis use. The ABC study excluded patients with severe cannabis use in the sense of a disorder but still reported a sex difference of 4 years in the age at first admission (Häfner et al. 1989, 1993).
Symptomatology and social functioning
Regarding gender differences in psychopathological symptoms, the findings are less conclusive. It has often been reported that negative symptoms (e.g., social withdrawal, blunted affect, or amotivation) occur more frequently in men whilst affective symptoms (e.g., depression) or specific psychotic symptoms (e.g., paranoia) occur more often in women (Abel et al. 2010; Ochoa et al. 2012; Canuso and Pandina 2007; Riecher-Rössler and Häfner 2000; Riecher-Rössler et al. 2010). However, many of these studies are not true population-based studies. In the ABC study, which examined a representative population-based sample of all first admitted with narrowly defined schizophrenia, very few gender differences in psychopathology were found, which disappeared after correction for multiple testing (Häfner et al. 1991a, 1993) (see Fig. 2). The differences found had more to do with comorbidity and illness behavior; for example, men had more substance and alcohol abuse, self-neglect, deficits in communication, and social disability, whereas women displayed more over-adaption and conformity (Häfner et al. 1992). More recent studies in representative first-episode populations were conducted by Salokangas and Stengard (1990), Thorup et al. (2007), Koster et al. (2008), Bertani et al. (2012), Hui et al. (2016), and Cotton et al. (2009), the latter being restricted to the age group of 15–29 years. These studies mainly reported that men with schizophrenia had more negative symptoms, less affective symptoms, more social isolation, and poorer social functioning (Bertani et al. 2012; Koster et al. 2008; Salokangas and Stengard 1990; Thorup et al. 2007; Hui et al. 2016; Holtzman et al. 2010). Men also had more substance abuse (mainly cannabis and alcohol) (Cotton et al. 2009; Koster et al. 2008; Thorup et al. 2007). This greater prevalence of substance abuse in men might have contributed to the gender differences in symptomatology, which many studies unfortunately did not control for.
Gender differences in psychopathological syndromes of first admitted patients with schizophrenia—narrow definition (ICD 295 only) (ABC study)*. CATEGO syndromes based on the Present State Examination (Wing et al. 1973, 1974). *Reprinted (in a translated version) from Häfner et al. (1991b) with permission from Thieme Publishers
Many of these differences can also be found in the general population, such as more affective symptoms, depression and anxiety in women, but more alcohol, substance and cannabis abuse in men (Seedat et al. 2009).
However, there seem to be more differences between women and men with late-onset schizophrenia. In the ABC study, men with schizophrenia onset over 40 years showed significantly milder symptoms than those with early onset, whereas late-onset women suffered from symptoms almost as severe as early-onset women (Riecher-Rössler et al. 1997) (Table 2).
Furthermore, women appear to experience a variation in symptom severity over the menstrual cycle (Riecher-Rössler et al. 1994), which is discussed in more detail subsequently.
Regarding social functioning, available evidence suggests that women outperform men. This was shown for first-episode psychosis but also during the later course of the disease (Ochoa et al. 2012; Canuso and Pandina 2007).
Cognitive functioning
Impairment of cognitive functioning—neurocognition and social cognition—is recognized as a core feature of schizophrenic psychoses (Fatouros-Bergman et al. 2014; Davidson et al. 2009; Brekke and Nakagami 2010). Since we do not have adequate treatments, this impairment is one of the main obstacles for patients’ full recovery and reintegration.
Neurocognitive functioning is known to show distinct sex and gender differences in healthy individuals. Healthy women for instance tend to perform better than men in tasks measuring verbal abilities, while men perform better in tests of visuospatial skills (Ittig et al. 2015).
Many sex/gender differences regarding neurocognition have also been found in patients with schizophrenic psychoses (Ittig et al. 2015; Ochoa et al. 2012; Riecher-Rössler et al. 2010). However, there are relatively few studies in first-episode patients. The latter show that women have a better performance in verbal learning and memory compared to men but do worse than men on tests of reaction time, visual memory, and executive functions (Ayesa-Arriola et al. 2014; Hoff et al. 1998; Ittig et al. 2015). In one study, men were noted to have a higher IQ and better performance in the visual domain (Hui et al. 2016).
As regards social cognition, healthy women were shown to have better emotion recognition than men, while findings regarding theory of mind were inconsistent (Danaher et al. 2017). The few studies analyzing gender differences of social cognition in schizophrenia have contradictory findings. Pinkham et al. (2017) did not find any differences, but in other studies, male schizophrenia patients showed greater deficits in emotion perception (Carter et al. 2009) which was associated with a worse functional outcome (Irani et al. 2012). In first-episode patients, one study showed no gender differences regarding theory of mind (Ayesa-Arriola et al. 2014).
It is important to note here that the impairment of neuropsychological functioning depends on a wide variety of conditions which might differ between women and men, for example, the severity of symptoms (O’Leary et al. 2000) and especially the fluctuation of estrogen levels during the menstrual cycle in women (Hoff et al. 2001). Most importantly, sex/gender differences were very similar to those found in the general population and in healthy controls (Ittig et al. 2015; Ayesa-Arriola et al. 2014). Hence, it appears that differences in neurocognition might not be disease-specific.
Emerging disease and “premorbid” characteristics
There is a plethora of literature about so-called “premorbid” functioning or “premorbid” adjustment in schizophrenia. This was often described as being better in women than in men (Ochoa et al. 2012). In light of newer research, however, it must be questioned if the worse or declining social functioning of people who developed schizophrenic psychoses later in life was really “pre”-morbid or rather an early sign of the disease. We now know that schizophrenic psychoses in about 70% of all cases do not start acutely with frank psychotic symptoms, such as delusions or hallucinations, but emerge slowly, on average, over four to five years with so-called prodromal symptoms. The prodrome includes nonspecific symptoms first and then more specific subthreshold or “attenuated” psychotic symptoms (Häfner et al. 1991a, 1994; Riecher-Rössler and McGorry 2016). Over the last two decades, there has been a tremendous effort in psychiatric research to identify these early stages (Riecher-Rössler and McGorry 2016). Early detection and intervention services have been established in many countries (Maric et al. 2017) with the aim of identifying these at-risk mental states for psychosis or at least to diagnose frank psychosis in the very early stages, the so-called first-episode psychosis.
More recently, many studies have been published on the characteristics of patients with an at-risk mental state and on the sex and gender differences observed in these populations. However, an important confounding factor is that this work has been mainly conducted in help-seeking populations, rather than in representative populations. Many patients at risk might be missed by early detection services (Fusar-Poli et al. 2017). Furthermore, there might be a selection bias with regard to gender. Thus, in studies based on the populations of these services, about 58% of the patients at-risk and 67% of the first episode patients were male (Wilson et al. 2017). So far, it is not clear to what extent this is due to gender differences in help seeking at these services or a sampling bias in the recruitment to studies (Longenecker et al. 2010). A further problem is that not all studies differentiate within their at-risk mental state populations, whether the patients have in fact made a later transition to psychosis or not. So, the findings not always refer to “true” emerging psychosis.
Regarding gender differences in the symptomatology of patients at risk, in a comprehensive review of twelve studies up until 2014, Barajas et al. (2015) described many inconsistent findings. Most studies reported no differences, but some reported more negative symptoms and worse psychosocial functioning in men.
More recent studies had similar results. While some found no gender differences in symptomatology (Kotlicka-Antczak et al. 2016), a few other studies described men showing more negative symptoms (Rietschel et al. 2017), violent behavior (Tseliou et al. 2017), and disorganized communication (Theodoridou et al. 2017). In contrast, women showed more depression and social anxiety (Rietdijk et al. 2013; Pruessner et al. 2017) and more unusual perceptual experiences (Waford et al. 2015). However, most of these studies had not corrected for multiple testing or confounding variables. Among others, differences found could be due to comorbidity, especially the well-described higher substance use in men.
Riecher-Rössler and colleagues examined all patients from the canton of Basel-Stadt who sought help in the early detection service, the only service for this catchment area, in the framework of the FePsy (Früherkennung von Psychosen; Early Detection of Psychosis) project (Riecher-Rössler et al. 2009). At referral to the service, both at-risk mental state and first-episode female patients with psychosis had slightly higher (pre-)psychotic symptom scores than men. Men had slightly higher negative symptom scores than women. However, the differences did not withstand correction for multiple testing. This was true for both observer-rated and self-reported symptoms (González-Rodríguez et al. 2014) (Fig. 3). Illness insight seemed to be the same in both women and men, since the discrepancy between self- and observer-rating was the same for both genders (Spitz et al. 2015). However, there have also been findings of a more strongly reduced illness insight in first-episode men compared with women (Cotton et al. 2009). Interestingly, the first self-perceived signs of the disease were different between the genders. While men more frequently first noticed negative and cognitive symptoms, women more frequently first noticed subthreshold positive and affective symptoms (Heitz et al. 2017).
Symptomatology in at-risk mental state (n = 117; 43 women, 74 men) and first-episode psychosis (n = 87; 31 women, 56 men) patients in the FePsy-Study*. Means and 95% confidence intervals of subscales of the Brief Psychiatric Rating Scale (BPRS), Scale for the Assessment of Negative Symptoms (SANS), and Frankfurt Complaint Questionnaire (FCQ) within the groups of at-risk mental state (ARMS) and first-episode psychosis (FEP) patients. All scales were z-transformed based on means and standard deviations of the total group. *Reprinted from González-Rodríguez et al. (2014) with permission from the Israel Journal of Psychiatry and Related Sciences
In a non-help-seeking representative general population sample of 7076 subjects in The Netherlands, men had a higher prevalence of negative symptoms, while women had higher rates of so-called positive psychotic experiences and depressive symptoms (Maric et al. 2003). These results imply that the few sex differences seen in symptomatology of psychosis are also seen in a subthreshold form in the general population. All in all, regarding emerging symptomatology, it seems that differences between women and men—if there are any—are small and often resemble those in the general population.
Cognition appears to be already impaired in individuals with an at-risk mental state (Ittig et al. 2015; Fusar-Poli et al. 2012a). There are a limited number of studies on sex/gender differences in this population. Walder et al. (2008) only found one difference with men showing a better performance in picture completion. Within the FePsy project, the same differences were found in at-risk mental state as in first-episode patients and healthy controls (Ittig et al. 2015) (Fig. 4).
Cognitive performance of women compared to men in patients with an at-risk mental state for psychosis (n = 118; 45 women, 73 men), first-episode psychosis patients (n = 88; 32 women, 56 men), healthy controls (n = 86; 41 women, 45 men), and in the total group (FePsy study)*. The dotted horizontal line at zero represents the performance of men. Differences are expressed in units of Cohen’s d and are significant if the 95% confidence interval (vertical line) does not overlap with zero. Variables with a minus sign were reversed so that positive scores always represent good performance. Differences are adjusted for the influence of age, years of education, and use of antipsychotics. In the total group, we additionally corrected for the diagnostic group. ARMS, at-risk mental state; FEP, first-episode psychosis; HC, healthy controls; total, ARMS + FEP + HC; ToH, Tower of Hanoi; WCS, Wisconsin Card Sorting Test; CPT, Continuous Performance Test; CVLT, California Verbal Learning Test. *Reprinted from Ittig et al. (2015) with permission from Elsevier.
When patients seek help for the first time in a specialized service, men in many studies show a longer duration of untreated illness or psychosis, but this difference usually does not reach significance (Barajas et al. 2015; Cascio et al. 2012). In the FePsy sample, there also was a slightly longer duration of untreated psychosis in men (Fridgen et al. 2013). A longer duration of untreated illness is in keeping with the worse help-seeking behavior generally described in men (Riecher-Rössler in print). A recent qualitative study in users of an early intervention service showed gender stereotypes to influence help-seeking behavior in this population (Ferrari et al. 2016). Thus, men described having difficulties in talking about their symptoms and that help-seeking was perceived as a sign of weakness by their peers. In contrast and most interestingly, when women were trying to seek help, this was often negatively questioned by family members and service providers (Ferrari et al. 2016).
Transition rates from at-risk mental state to first-episode psychosis might be slightly higher in male than female individuals (Barajas et al. 2015), although this has not been described in more recent studies (Riecher-Rössler and Studerus 2017). Within the male at-risk patients, social functioning and attenuated psychotic symptoms were seen to predict transition to psychosis, which was not true for female at-risk patients (Walder et al. 2013).
Course of psychoses
The further course of schizophrenic psychoses—after onset of the first episode—is heterogeneous. Many patients nowadays only experience one episode with full recovery, especially when they receive early treatment. Some patients, however, have several acute episodes and might suffer from chronic symptoms and/or cognitive impairments of varying severity in between the episodes (Riecher-Rössler and Rössler 1998; Newman et al. 2012).
Women have often been reported to have a more favorable course and a better psychosocial “outcome” than men. They seem to have fewer and shorter hospital stays and a better social adjustment than men, whereas the symptom-related course might be quite similar for both sexes (Riecher-Rössler and Rössler 1998; Canuso and Pandina 2007; Abel et al. 2010; Ochoa et al. 2012). In more recent studies, findings regarding hospitalizations were contradictory (Cotton et al. 2009; Tseliou et al. 2017). With regard to symptomatology, patients with persisting symptoms tended to be male in the large World Health Organization SOHO study on 17,000 outpatients in 37 countries (Novick et al. 2012). Men also showed higher levels of negative symptoms (Thorup et al. 2014; Shibre et al. 2015; Galderisi et al. 2012). In a 5-year-follow-up of 578 first episode patients, Thorup et al. (2014) found women to have better social functioning, being more often in employment or education and living with their own children, and more often reaching a state of recovery. In contrast, Galderisi et al. (2012) found no gender differences in any index of social functioning in chronic schizophrenia patients. In a recent meta-analysis, there was no gender difference concerning “recovery,” defined as improvement in both clinical and social domains persisting for at least two years in at least one of the domains (Jääskelainen et al. 2013). The long-term course in a 34-year follow-up study was similar for women and men (Newman et al. 2012). Standardized mortality rates seem to be the same for both women and men, as shown in a recent systematic review (McGrath et al. 2008).
However, most studies were not conducted in representative populations of all first-contact patients of a defined catchment area, they used differing diagnostic criteria and age limits, etc. (Riecher-Rössler and Rössler 1998). The few studies covering the whole age range and looking at the interaction of age and gender found a better course in women only up to age 40. After this, their course of illness seems to deteriorate (Riecher-Rössler et al. 2010). In late-onset schizophrenia, the course of the disease might be even worse in women than in men (Riecher-Rössler et al. 1997).
The presumably better course in women—at least the younger ones—might be explained by different factors (Riecher-Rössler and Rössler 1998; Riecher-Rössler and Häfner 2000). Among others, women seem to have a better compliance (Cotton et al. 2009; Thorup et al. 2014), a better treatment response (Riecher-Rössler et al. 2010), and a better illness insight (Cotton et al. 2009), although the latter was not replicated (Spitz et al. 2015). Their course is certainly also positively influenced by the fact that they have less comorbid substance abuse (Cotton et al. 2009; Thorup et al. 2014). In studies controlling for this, many gender differences disappeared or became smaller (Thorup et al. 2014). The better overall social course in women might also be a consequence of their later age of onset and, accordingly, a better social integration to start with. A further reason might be the differing stress sensitivities of both sexes (described further in the following). Last, but not least, the female sex hormone estradiol might offer some protection in women of the fertile age group (also described later).
Summing up the findings on epidemiological and clinical sex and gender differences, the lifetime risk for schizophrenic psychoses seems to be similar or potentially slightly higher in men than in women. Women become ill later in life and tend to have a better course of illness despite only a few differences in symptoms to begin with. This applies especially to young women. After age 40, women become ill much more often than men and their symptoms plus the course of their disease also seems to be worse.
Sex differences in the brain—developmental aspects and morphology
Schizophrenic psychoses are commonly regarded as neurodevelopmental disorders with genetic influences and/or environmental insults in utero or perinatally leading to alterations in neural development and connectivity (Baldwin and Srivastava 2015). The fact that the disorders nevertheless commonly only occur after puberty or later might be explained among others by the neuromaturational processes in adolescence (Trotman et al. 2014).
Consequently, psychotic disorders are associated with many structural changes in the brain (Bora et al. 2011; Abel et al. 2010), which are partly already present in patients at risk who later go on to develop psychosis (Fusar-Poli et al. 2012b; Smieskova et al. 2013; Cannon 2015).
Normal development of the brain is well known to differ between the sexes. This is mainly mediated by genes and by regulatory influences of sex steroids and leads to a structural sexual dimorphism of the healthy brain (Abel et al. 2010; McEwen and Milner 2017; Gillies and McArthur 2010), including sex differences in brain connectivity (Ingalhalikar et al. 2014).
Interestingly, the normal sexual dimorphism of the healthy brain seems to be disrupted in schizophrenic psychoses (Goldstein et al. 2002; Walder et al. 2016). This has been shown primarily in the cortex (Goldstein et al. 2002) but also in the volume of the amygdala (Gur et al. 2004; Takayanagi et al. 2011), hippocampus (Irle et al. 2011), hypothalamus (Goldstein et al. 2007), orbito-frontal and anterior cingulate (Goldstein et al. 2002; Takahashi et al. 2002; Gur et al. 2000, 2004), and insular cortex (Duggal et al. 2005), as well as regarding grey matter volume asymmetry (Frederikse et al. 2000), the gyrification index (Vogeley et al. 2000), and cortical folding (Vogeley et al. 2000; Narr et al. 2004).
Up to now, the sexual dimorphisms of the brain structure in patients with an at-risk mental state have been widely neglected. In a recently conducted study (Egloff et al. 2018) of 65 at-risk mental state patients, 50 first-episode patients, and 70 healthy controls, subcortical brain volumes were examined. Since the hippocampus was the only structure affected by reversed sexual dimorphism, it was concluded that subcortical volumes may not be primarily afflicted by disruption of sexual dimorphism, which is well in line with the findings of Goldstein et al. (2002).
In a recent meta-analysis, Nordholm et al. (2013) described that psychoses are associated with increased pituitary volumes, even in untreated first-episode patients and in individuals at risk, especially those with later transition. Women show even larger volumes than men. The same-sex difference was found in a more recent study (Takahashi et al. 2013) and in the FePsy longitudinal study of at-risk patients with and without later transition to psychosis at each time point (Walter et al. 2015). However, pituitary volumes are known to also be larger in healthy women (MacMaster et al. 2007), and it is unclear if the increase in female patients was stronger than in male patients.
Further understanding of these abnormalities might provide important etiological clues. Thus, Goldstein et al. (2002) have hypothesized that sex differences in brain abnormalities in schizophrenia are initiated at the time of the early sex differentiation of the brain, i.e., during fetal and early postnatal development which would mean that the reversal of sexual dimorphism in people who develop schizophrenia also occurs early. Other neurodevelopmental theories propose that male brains are more vulnerable to pre- and perinatal complications due to slower cerebral maturation or that sex differences occur due to excessive synaptic pruning during adolescence, especially in men (Falkenburg and Tracy 2014). To further elucidate when these abnormalities occur, it would be important to conduct more longitudinal studies with patients at risk who transition to psychosis. Furthermore, it would be of great interest if the sex differences in brain development are associated with the age of illness onset.
Of further interest in this context are functional neuroimaging studies showing sex differences in cerebral activation in schizophrenia patients that partly deviate from those in healthy controls, indicating also a disturbed normal sexual dimorphism (Mendrek et al. 2007; Mendrek and Stip 2011). Finally, it has to be noted that sexual dimorphism occurs in a wide array of neurotransmitter systems which might partly be relevant in schizophrenic psychoses (Cahill 2006). These important and extensive fields cannot be adequately covered in this review.
Finally, it should be emphasized that sex differences in brain structure and function refer to average differences between women and men and that differences between individuals within each sex might sometimes be larger than the average difference between the sexes (Resnick and Driscoll 2008).
Sex and gender differences in pathogenic pathways, risk, and protective factors
It is generally believed that schizophrenic psychoses are multifactorial in nature with gene–environment interactions (van Os and EU-GEI-Study-Group 2014). The widely accepted vulnerability stress model (Zubin and Spring 1977) suggests that individuals with an underlying vulnerability for psychosis only develop the disease when it is triggered by different forms of “stress” or the loss of protective factors. Recently, as already described, there has also been more consensus about probably dealing with a group of disorders with different etiologies rather than “one” schizophrenia (Cuesta and Peralta 2008; Riecher-Rössler and Studerus 2016).
Genetics/familial risk
Regarding the underlying vulnerability for schizophrenic psychoses, genetic factors certainly play a critical role. Early evidence from family, twin, and adoption studies suggest a heritability of up to 70–80% (Goldstein et al. 2013). Molecular genetic strategies have identified several plausible polymorphisms and rare mutations. Environmental factors seem to interact with genes via epigenetic mechanisms (Goldstein et al. 2013).
Sex differences in the genetics of schizophrenic psychoses have for a long time been thought to be absent, although some studies had reported higher risks in relatives of women than in those of men (Ochoa et al. 2012). Recent evidence suggests the presence of some sex-dependent risks (i.e., quantitative differences in risk between the sexes) and even sex-specific risks (i.e., present in only one sex) (Goldstein et al. 2013). Considering the offspring of mothers with psychosis, their sons seem to develop psychosis more often than their daughters. In contrast, fathers more often seem to transfer the disorder to their daughters than to their sons (Goldstein et al. 2011). Recent molecular genetic studies point to a possible involvement of the X chromosome (Goldstein et al. 2013). Further evidence comes from candidate gene approaches that have suggested sex-dependent or sex-specific effects on psychosis risk. Here, genome-wide association studies (GWAS) suggest sex-specific effects primarily among women with schizophrenic disorders; however, more studies are required (Goldstein et al. 2013; Seeman 2013).
The same is true for studies on epigenetics (Chase et al. 2015) or studies on sex differences in mitochondrial function (Marchbanks et al. 2003), contributing to the etiology of psychosis.
A further line of evidence involves sex differences in dopaminergic pathways, which might partly be also genetically determined and not only by gonadal steroids as thought so far (Ngun et al. 2011) (see following discussions). This is of great interest since the neurotransmitter dopamine and its pathways are thought to be mainly involved in the development and expression of psychotic symptoms (Howes and Kapur 2009).
Obstetric complications
In line with the neurodevelopmental theory of schizophrenic disorders, obstetric complications have been shown to increase the risk for the disorders. However, whether this risk has a sex-dependent distribution is unclear, since the studies report contradictory results (Ochoa et al. 2012).
Substance abuse
People with schizophrenic psychoses have a high comorbidity of substance abuse. This is especially important, because many drugs (such as cannabis, amphetamines, hallucinogens, cocaine, and phencyclidine) are known to increase the risk for psychosis or at least act as a trigger in vulnerable individuals.
The most commonly abused illicit drug in the Western world is cannabis, which is significantly more often used by men than by women (Khan et al. 2013). In patients with early-phase or first-episode psychosis, lifetime exposure is up to 60–80% and current use in at-risk or first-episode patients at entry to care is 30–40% (Crocker and Tibbo 2017; Bugra et al. 2013). Cannabis is associated with an earlier age of onset (Murray et al. 2016; Crocker and Tibbo 2017; Di Forti et al. 2014; Large et al. 2011) and a more severe course of illness, i.e., a greater severity of symptoms, stronger impairment of global functioning, and a higher risk of relapse (Crocker and Tibbo 2017).
Regarding gender differences in psychoses, men with schizophrenia use more cannabis than women (Koskinen et al. 2010), which is apparent at first contact and in first-episode patients (Crocker and Tibbo 2017; Nunez et al. 2016; Menghini-Müller et al. 2016). Moreover, cannabis-induced acute psychosis in men more often leads to full-blown schizophrenia in the following three years (Arendt et al. 2005). The age at onset of schizophrenic psychoses is decreased in cannabis users of both sexes (Di Forti et al. 2014; Large et al. 2011).
Men with schizophrenia also have a higher consumption of cocaine, hallucinogens, and alcohol (Ochoa et al. 2012). However, women who present with substance abuse may have a more detrimental course of illness than men with substance abuse (Lange et al. 2014).
Stress and trauma
Traumatic life events, such as physical, sexual, or emotional abuse and bullying in childhood, as well as trauma in later life, including rape, seem to interact with underlying vulnerability and other risk factors to increase the risk for psychosis and influence other psychosis outcomes. Within clinical at-risk populations, childhood trauma, in particular, seems to predict psychosis onset (Mayo et al. 2017). However, the causality is not yet clear (Kraan et al. 2017; Trotman et al. 2014), and these risk factors are not specific for psychosis because they are also present in other mental disorders (Gibson et al. 2016; Kraan et al. 2017).
Only a few studies have looked at the effect of gender when considering trauma and psychosis. The findings were inconsistent, but there are studies showing that women with psychosis have a history of trauma and sexual abuse more often than men (Mayo et al. 2017; Cotton et al. 2009). Some studies report a greater risk of psychosis in women after traumatic life experiences compared with men (Gibson et al. 2016). Furthermore, women with schizophrenia who report childhood abuse seem to have more psychotic and depressive symptoms than women without a trauma history or men (Kelly et al. 2016; Garcia et al. 2016).
In a population of college students, stress sensitivity mediated the relationship between traumatic life events and attenuated subthreshold psychotic symptoms more strongly in women than in men (Gibson et al. 2014).
Considering stress sensitivity in healthy women and men, the studies are contradictory (Goel et al. 2014). While most studies report that women are generally more sensitive to stress and trauma than men (Gibson et al. 2016; Newhouse and Albert 2015), some have reported the opposite (Kudielka and Kirschbaum 2005).
Also, regarding gender differences of stress response in psychoses, studies are contradictory. While Myin-Germeys et al. (2004) found that women with a psychotic disorder report significantly increased emotional reactivity to daily life stress, Pruessner et al. (2015) found indications for higher stress sensitivity in men—not women—with schizophrenia, i.e., a blunted cortisol response after awakening and reduced hippocampal volume.
The inconsistencies are partly due to methodological differences and seem to depend on the type of stress stimuli (Goel et al. 2014). Furthermore, stress responsivity may fluctuate in women, depending on their estradiol levels, with fluctuating or low levels during the premenstrual cycle phase or after menopause being associated with higher stress responsivity (Albert et al. 2015; Goldstein et al. 2010; Goel et al. 2014; Baldwin and Srivastava 2015).
Hormonal influences and the hypothalamo-pituitary-gonadal axis
It is increasingly accepted that gonadal steroids, especially estrogens, might be responsible for some sex differences in schizophrenia. Estrogens influence brain development and brain functioning (McEwen and Milner 2017). Numerous studies have shown that estradiol, the main component of estrogens, exerts protective effects in psychosis (Markham 2012; Riecher-Rössler 2017) (see subsequent texts). There is mounting evidence that many women with psychosis have subnormal estrogen levels, even in the prodromal and untreated phases of the disease (Riecher-Rössler and Kulkarni 2011; Riecher-Rössler and Häfner 1993; Riecher-Rössler 2017; da Silva and Ravindran 2015; Melcangi et al. 2011; Markham 2012). Recently, there have also been reports of hyperprolactinemia in many antipsychotic-naïve patients (Gonzalez-Blanco et al. 2016; Petrikis et al. 2016; Riecher-Rössler et al. 2013; Ittig et al. 2017). As prolactin suppresses the production of gonadal hormones, this could explain the lowered estrogen levels in women with psychosis.
These observations led Riecher-Rössler and colleagues to propose two, strongly interconnected hypotheses (Riecher-Rössler and Häfner 1993):
-
firstly, that estrogens provide protection against psychosis (estrogen protection hypothesis);
-
and secondly, that psychosis is associated with hypoestrogenism and dysfunction of the hypothalamo-pituitary-gonadal axis (hypothesis of hypoestrogenism and gonadal dysfunction).
In this context, it has also been suggested that women who are “vulnerable” to the development of schizophrenia may have a generally lower level of endogenous estrogens than healthy women. Therefore, they are less likely to experience the neuroprotective effects of endogenous estrogens, and this potentially contributes to the onset of schizophrenia (Taylor et al. 2009).
Estrogens and the brain
As outlined previously, schizophrenic disorders are associated with many brain abnormalities, which seem to be the basis for an enhanced vulnerability to psychosis. The occurrence of symptoms is also associated with neurotransmitter dysfunctions. All abnormalities described can obviously be influenced by estrogens, which have “organizational” effects leading to structural changes as well as “activational” effects that affect neuronal function (Goldstein et al. 2002; Trotman et al. 2014; Taylor et al. 2009).
Generally, estrogens and testosterone strongly influence brain development during late gestation, in the early postnatal period, and during puberty. During these critical periods of brain sexual differentiation, gonadal steroids have permanent effects leading to brain sexual dimorphism (McCarthy 2008; Melcangi et al. 2011; Sanchez et al. 2010; Herting et al. 2012), which might be disrupted in schizophrenic psychoses as discussed above (Jimenez et al. 2010; Mendrek 2007; Goldstein et al. 2002). Estrogens also influence brain maturational processes in adolescence and young adulthood and continue to be important in normal maintenance of brain function during the entire lifespan (Sanchez et al. 2010; Trotman et al. 2014).
Estrogens, especially 17-β-estradiol, which is most active in the brain, obviously have many neuroprotective effects presumably relevant for psychoses. Thus, they appear to promote neuronal sprouting and myelination, enhance synaptic density and plasticity, facilitate neuronal connectivity, act as an anti-inflammatory and as an antioxidant, inhibit neuronal cell death, might mediate BDNF expression and activity, and positively influence mitochondrial function (Riecher-Rössler 2017; Shimamoto and Rappeneau 2017; McEwen and Milner 2017).
Acute symptomatology probably depends mainly on acute neurotransmitter dysregulations. Estrogens play an important role in acute symptom expression through the modulation of dopaminergic and other key neurotransmitter systems, such as the glutamatergic, serotonergic, noradrenergic, and cholinergic systems—which are all associated with psychosis symptom development and expression (Riecher-Rössler 2017). In particular, estrogens can modulate the sensitivity and number of dopamine receptors (Riecher-Rössler 2017).
Estrogens not only act via the classical genomic pathway but also have nongenomic, rapid interactions. There are at least two subtypes of estrogen receptors, namely estrogen receptor-α and -β. They are expressed in many areas of the human brain which are not only associated with neuroendocrine function but also with emotion, memory, and cognition. Variations in the estrogen receptor-α (ESR1) were found to be associated with schizophrenia (Riecher-Rössler 2017). Some authors suggested that the brain response to estrogens in patients with schizophrenia might be inadequate (Riecher-Rössler 2005; Riecher-Rössler and Häfner 1993). More details on recent molecular and preclinical findings are given in a comprehensive review by Gogos et al. (2015).
In animal models, estrogens have been shown to have similar effects as antipsychotics (Riecher-Rössler and Kulkarni 2011). They also positively influence many processes that are disturbed in psychoses, such as changes in latent inhibition, prepulse inhibition, auditory processing/mismatch negativity, and selective attention (Riecher-Rössler 2017).
Estrogens as protective factors—epidemiological and clinical findings
Acute, short, psychotic episodes with a wide range of symptoms have been described after estrogen withdrawal in formerly healthy persons, such as in premenstrual psychosis, post-abortion psychosis, psychosis after the removal of a hydatidiform mole, after stopping oral contraceptives or with administration of estrogen receptor antagonists or a gonadorelin agonist. These types of psychoses appear to occur especially in women with a noted previous sensitivity to estrogen withdrawal and usually remit with estrogen substitution (Riecher-Rössler 2017).
Regarding schizophrenic psychoses, many of the sex differences described earlier might at least partly be attributable to the influence of estrogens. The slightly lower overall lifetime incidence in women as well as the particularly low incidence in young women might be due to the protective effect that estrogens exert in women in the fertile age group. Falling estrogen levels with the menopause might account for an increased incidence of psychosis in women over 40 years of age. Thus, it is proposed that via their different neuroprotective effects, estrogens delay the age of onset of schizophrenia in women. Due to this protection, women with the same vulnerability as men might only develop psychosis after age 40 with the loss of estrogen protection in the (pre-)menopause. This could also explain the findings that the course of the disease is more favorable in younger women than after age 40 (Riecher-Rössler 2017) (see previous texts and Fig. 1).
Similarly, a later menarche, i.e., a later rise of estrogen levels in young girls, seems to be associated with an earlier onset of the disorder (Riecher-Rössler 2017).
The symptomatology of psychotic disorders has also been found to correlate with the estrogenic state in women. Thus, chronic psychoses have been reported to improve during pregnancy (when estrogen levels are increased about 100- to 200-fold), although this has not been studied rigorously. However, after delivery, with its sudden drop of estrogens to normal or even subnormal levels, there is an excess of psychosis relapses (Riecher-Rössler 2017; Vigod and Ross 2010).
In women with schizophrenia, psychotic symptoms often deteriorate pre- or perimenstrually, i.e., in the low estrogen phase of the cycle (Riecher-Rössler and Kulkarni 2011; Markham 2012). The few studies, which directly measured the estradiol blood levels, showed that during the menstrual cycle rising 17-β-estradiol blood levels were associated with decreasing symptoms (Riecher-Rössler et al. 1994) as well as improvement of cognition (Riecher-Rössler and Kulkarni 2011).
Based on these observations, it has been suggested that estrogens, especially 17-β-estradiol, may have antipsychotic properties, leading to the potential use of estrogens as a treatment for schizophrenia. This is described in more detail in the “Limitations, open questions, and implications for research” section. However, the influence of estrogens does not seem to be specific for psychotic symptomatology - as expected from the multiple effects of estrogens on mental functioning (Gillies and McArthur 2010; Watson et al. 2010; Riecher-Rössler 2017). Estrogens also seem to improve affective symptoms, aggressive and suicidal behavior, and cognitive functioning (Gillies and McArthur 2010; Riecher-Rössler and Kulkarni 2011; Boss et al. 2014; Maki and Dumas 2009; Weickert et al. 2016; Pompili et al. 2012; Riecher-Rössler 2003; Toffol et al. 2015; Fischer et al. 2014)—which are all symptoms that play an important role in schizophrenia patients. Furthermore, estrogens seem to also have a stress-protective role (Albert et al. 2015; Carlson and Sherwin 1999; Goldstein et al. 2010).
Hypothalamo-pituitary-gonadal dysfunction and hyperprolactinemia
Women with schizophrenic psychoses have often been reported to have a disturbed gonadal function with menstrual irregularities and reduced blood levels of estradiol, progesterone, and gonadotrophins (follicle-stimulating hormone, luteinizing hormone) throughout the menstrual cycle as well as anovulation (da Silva and Ravindran 2015; Markham 2012; Melcangi et al. 2011; Riecher-Rössler and Häfner 1993; Riecher-Rössler and Kulkarni 2011; Riecher-Rössler et al. 2013). Men with (emerging) psychosis also seem to have decreased levels of estradiol and testosterone (Akhondzadeh et al. 2006; van Rijn et al. 2011; Huber et al. 2005; Taherianfard and Shariaty 2004; Heringa et al. 2015; da Silva and Ravindran 2015). Furthermore, women with first-episode psychosis reported clinical signs of gonadal dysfunction long before the onset of the disease (Riecher-Rössler and Häfner 1993). Well in line with this, fertility seems to be reduced in both women and men (Bundy et al. 2011), and women show reduced bone mineral density (Maric et al. 2005).
Also in line with this, recent studies show that men and especially women with (emerging) psychosis have increased levels of prolactin (Riecher-Rössler 2017) (see also previous texts). As increased prolactin suppresses gonadal function, this could explain the mentioned findings.
For a long time, it was thought that these abnormalities were due to antipsychotic medication. However, “hypoestrogenism” has been observed long before the introduction of antipsychotics (Riecher-Rössler and Häfner 1993). Most importantly, hyperprolactinemia has recently also been shown in antipsychotic-naïve first-episode and even at-risk patients, especially in women (see previous texts). Women with (emerging) psychosis had a greater increase in prolactin levels than men with (emerging) psychosis, even after correction for the higher prolactin levels in healthy women (Ittig et al. 2017; Riecher-Rössler 2017) (Fig. 5; Table 3).
Prolactin serum levels in at-risk mental state (n = 116; 34 women, 82 men) and first-episode (n = 49; 15 women, 34 men) patients subdivided by sex (FePsy Study)*. The dotted horizontal lines represent the upper and lower levels of the normal range for men and women. ARMS, at-risk mental state; FEP, first-episode psychosis. *Reprinted from Ittig et al. (2017) with permission from Elsevier
Since an increase of prolactin production—similarly to that of ACTH/cortisol—is associated with an enlargement of the pituitary gland (MacMaster et al. 2007), these findings are well in accordance with the above-mentioned enlarged pituitary volumes in these patient groups, especially in female patients (Nordholm et al. 2013; Takahashi et al. 2013; Walter et al. 2015).
As prolactin—along with cortisol and ACTH—is a well-known stress hormone (Low 2016; Lennartsson and Jonsdottir 2011) and “emergency amenorrhea” is known to occur in healthy women under stress, Riecher-Rössler speculated that hyperprolactinemia in prodromal and first-episode psychosis is caused by psychological stress, associated with the emerging illness, and that hyperprolactinemia in itself might then trigger psychotic breakdown, as it stimulates prolactin-inhibiting factor, which is dopamine (Riecher-Rössler et al. 2013; Riecher-Rössler 2017) (Fig. 6). However, this would mean that the tubero-infundibular dopamine pathway would be involved in the pathogenesis of schizophrenic psychoses, and not just the mesolimbic and mesocortical pathways, as hypothesized prominently in the literature so far.
Control of prolactin production and secretion. PRL, prolactin; PRF, prolactin-releasing factor; TRH, thyrotropin-releasing hormone; VIP, vasoactive intestinal polypeptide; GABA, γ-aminobutyric acid; CNS, central nervous system. Reproduced from Low (2016) with permission from Elsevier
Studies testing these hypotheses in antipsychotic-free patients so far are few and inconclusive (Lally et al. 2017; Labad et al. 2015). The different dopamine pathways (tuberoinfundibular, mesolimbic, and mesocortical) will have to be considered here (Riecher-Rössler 2017) as well as the complex interactions between the HPG (hypothalamo-pituitary-gonadal) and HPA (hypothalamo-pituitary-adrenal) axes (Trotman et al. 2014).
The fact that prolactin levels show a stronger increase in women than in men (Ittig et al. 2017) could indicate that (emerging) psychosis is associated with even more (subjectively experienced) stress in women than in men.
Hyperprolactinemia is clinically relevant because it can lead not only to gynecomastia and galactorrhea but also to many consequences of gonadal suppression, such as estrogen and testosterone deficiency, sexual dysfunction, infertility, or osteopenia (Riecher-Rössler 2017).
Other hormones: progesterone, testosterone, DHEA, oxytocin
Other hormones might also be important in this context but will not be reviewed in depth here. They are much less studied in schizophrenic psychoses compared with estrogens, but there are some hints that they might also be involved in the pathophysiology (Ritsner 2011). There is some evidence that androgens, progesterone, and dehydroepiandrosterone (DHEA), the precursor of estrogens and androgens, might modulate brain dopamine neurotransmission (Sanchez et al. 2010; Sun et al. 2016; Höfer et al. 2013; Morris et al. 2015; Vuksan-Cusa et al. 2016).
Regarding testosterone, it has to be noted that it can be converted to estrogen in the brain. Hence, the above-mentioned estrogen actions in the brain might to a lower extent also be relevant for men (Weickert et al. 2016; Gillies and McArthur 2010). More research has to be done on this question. In antipsychotic-free men with (emerging) psychoses, lower testosterone levels than in healthy controls have been observed (Riecher-Rössler 2017). Results regarding a relationship between testosterone levels and symptoms in men with psychosis were contradictory.
DHEA(S) concentrations appear to positively correlate with cognitive functioning in men with schizophrenia (Moore et al. 2013). Endogenous oxytocin levels seem to correlate positively with prosocial behavior in patients of both sexes but negatively with psychopathological symptoms in female patients (Rubin et al. 2010).
Limitations, open questions, and implications for research
Health research and especially mental health research has often ignored sex and gender differences as well as the different risk factors and protective factors of both women and men. This applies to animal as well as to clinical studies (Zucker and Beery 2010; Howard et al. 2017) and might partly be due to the misconception that sex influences are small and unreliable (Cahill 2006). This neglect might have serious consequences. Thus, a European Parliament Report recently stated that “[…] the exclusion and under-representation of women as subjects and of gender and sex as factors in biomedical research and clinical trials put women’s lives and health at risk […]” (2016) (EU Report on Promoting Gender Equality in Mental Health and Clinical Research (2016/2096(INI)) by the Committee on Women’s Rights and Gender Equality 2016).
A similar critique applies to schizophrenia research. Only half of all articles on schizophrenia up to 2010 reported sex and solely 2.5% analyzed research findings by sex (Barker-Collo and Read 2011).
If sex and gender differences in schizophrenic psychoses are reported, they have often not been investigated rigorously with sound methodology. Thus, for example, results are often based on selected help-seeking samples rather than on representative community-based populations. In such samples, gender differences cannot reliably be described, among others because women and men have different help-seeking behaviors and might therefore be differently represented in different services. Moreover, there recently has even been a trend for services to reach out for special age groups. Thus, most early detection services concentrate on the age group under age 35 with the consequence that the many women with later age of onset might be missed. Furthermore, women and men might disproportionately take part in research projects. These factors have hardly been investigated.
Another limitation concerns the lack of control groups. Thus, if a gender difference is described in patients with schizophrenia, we often do not know if the differences found are specific for psychosis or mental illness or just reflecting gender differences in the general population. Furthermore, there often is a lack of control for influencing factors. Thus, the influence of the menstrual cycle is often not taken into account although there are hints at some sex differences diminishing during the low estrogen phase of the menstrual cycle, i.e., when women are more similar to men regarding the hormonal status. Another example is the higher rate of illicit drug use, including cannabis, by men, which might influence symptomatology and cognition and is often not controlled for.
Meta-analyses and systematic reviews, which have been widely published recently, have similar limitations, if e.g., important original studies are neglected or if the authors do not critically review the original data. Most importantly, much of the research on sex and gender differences is largely descriptive and does not explore the causes of these differences.
This has important implications for future research. Thus, sex and gender should be routinely integrated into study designs, data analyses, reporting, and interpretation of findings using, e.g., the SAGER guidelines (Heidari et al. 2016). Sex should also be incorporated as a variable in animal studies (McCarthy 2015). Not only sex- but also gender-based analyses have been suggested (Haarmans 2015).
Clinically, there are many open research questions which should be further addressed with sound methodology. What are the really “true” sex and gender differences in schizophrenic psychoses? And if there are such differences, are they specific for schizophrenic psychoses, or do these differences also occur in other mental disorders or even in the general population, as has to be suspected, e.g., for cognition, affective symptoms, and illness behavior? Is the normal sexual dimorphism of healthy individuals even reversed in people with psychoses, as some studies indicate, e.g., regarding brain structure and functioning?
If there are any differences specific for schizophrenic psychoses, when do they occur? Are they already present during the prodromal phase? Thorough long-term longitudinal multidomain studies of at-risk samples with identification of the “true” prodromals after transition and post-hoc analyses of the development of sexual dimorphism are needed. Are the pathogenic pathways to psychoses different for women and men? Do they possibly even suffer from different disorders within this group of disorders called “schizophrenia”? Do they, for example, have different genetic risks or differing stress sensitivity and/or different psychosocial or biological “stressors” triggering the outbreak of the disease?
Why do schizophrenic psychoses usually only start after puberty or later, although they are mainly regarded as having a neurodevelopmental basis? And why do women have a later onset and a second peak of onsets after age 45? What about the hormonal influences? It is widely accepted that the female sex hormone estradiol has some influence here. Many potential mechanisms of estrogens on neurodevelopment, neuromaturation, neurodegeneration, and neurotransmission have been shown, but what exactly is the interplay between these mechanisms, and their interplay with genetic and other risk factors? And what is the role of the hypothalamo-pituitary-gonadal (HPG) axis in the pathogenesis of these psychoses? Why do a substantial proportion of “at risk” individuals and untreated first-episode patients already show a marked disturbance of the HPG axis with enhanced prolactin, decreased estrogen, and possibly also decreased testosterone levels? Is this a preexisting abnormality predisposing to psychosis, or does it occur during the process of the emerging disease, potentially secondary to perceived stress? Again, it will require longitudinal studies with both women and men to elucidate the cascade of genetic, hormonal, and environmental processes leading to this group of disorders and the observed sex differences.
Moreover, there are hardly any studies on men with (emerging) psychoses. How many do suffer from low testosterone levels, what are the clinical consequences, and how should they be treated?
Summary and conclusions
Sex and gender differences in schizophrenic psychoses have been described for a long time, but results are not always based on methodologically sound studies and are sometimes uncritically passed on. This is unfortunate since if we could show true sex and gender differences in these disorders, explaining these differences could give us important insights into etiological and pathogenic mechanisms and they could improve our therapeutic approaches for both women and men.
Many clinical differences are reported, but studies were often based on selected populations. Furthermore, regarding the few differences found, it is sometimes not clear if these apply specifically to men and women with schizophrenic psychoses or if they are just differences as seen in the general population. Thus, future studies on clinical sex and gender differences should always be performed on unselected populations and in comparison to the general population/healthy controls.
Regarding the current status of research, the following findings seem relatively reliable:
The incidence of these disorders might be slightly higher in men. It is definitely higher in men of the younger age group and higher in women after age 45. In contrast to that, prevalence obviously does not show any sex differences. Age of onset is higher in women: while men have their peak of onsets in their early twenties, it is slightly later in women, and they have a second peak of onsets after age 45. With regard to symptomatology, gender differences—if there are any—are small with men tending to have more negative, women more affective symptoms. However, this might reflect the finding of more affective symptoms in women with higher rates of depression in the general population (Seedat et al. 2009) and higher emotional expressivity (Kring and Gordon 1998). Men, in contrast, show more substance and alcohol abuse, also reflecting gender differences in the general population, and worse social functioning, which might partly be due to their higher alcohol, drug, and cannabis abuse. There are some sex/gender differences in neurocognition, which were, however, also shown to be similar to those found in healthy controls or in the general population. In women, both symptomatology and neurocognition seem to be influenced by their physiological estrogen status with more severe impairments during the low estrogen state of the menstrual cycle and after menopause.
Similar gender differences regarding symptomatology and social and cognitive functioning can already be found in the prodromal phase of psychosis—again at least partly reflecting differences in the general population. Regarding the long-term course, women seem to perform better with lower levels of negative or persisting symptoms, better social functioning, and recovery. Standardized mortality rates seem to be the same for both genders. Again, the better course in women mainly seems to concern younger women, whereas in higher age groups or in late-onset schizophrenia, the course might be worse.
Concerning brain structure and functioning, the normal sexual dimorphism seen in healthy individuals seems to be disrupted in schizophrenic psychoses.
Regarding sex and gender differences in pathogenic pathways and risk and protective factors, more studies from genetics are urgently awaited. The same is true for the potential risk factor “obstetric complications”. Cannabis abuse is more frequent in men than in women with (emerging) psychoses. This could not only increase the incidence of psychosis but also reduce the age of onset, influence symptomatology, and the course of the disease. Regarding the association of trauma and psychosis, studies on gender differences are inconsistent as are studies on gender differences of stress responsivity.
There is increasing evidence that estrogens, especially 17-β-estradiol, is one of the influencing factors in schizophrenic psychoses, influencing brain development and brain functioning. The physiologically higher levels of estrogens in women might not only lead to their potentially slightly lower overall incidence but also to a delay in the age of onset with a second peak of onset after (pre-)menopause, when physiological estrogen levels decline. Lower estrogen levels during the menstrual cycle and after menopause might also be associated with more severe symptomatology in women.
Patients with (emerging) psychosis might also show hypothalamo-pituitary-gonadal dysfunction with hyperprolactinemia and suppressed gonadal function, i.e., low production of estrogens and testosterone. These findings, if replicated, could point to an important pathogenetic pathway to psychoses.
In conclusion, research as well as clinical practice should consider sex and gender aspects of schizophrenic psychoses much more strongly. If we do not investigate potentially differing pathogenetic pathways of both sexes/genders, this does not only undermine scientific validity but might also result in a failure to offer sex- and gender-sensitive treatments. More methodologically sound, longitudinal, multidomain, and interdisciplinary research should be done, investigating influencing factors both on the sex (biological) and gender (psychosocial) side. More research should also be done on gender differences in illness behavior, coping, help seeking, and compliance, as well as on sex-specific aspects of psychopharmacology, hormone therapies, and gender-sensitive psychosocial treatments.
The ultimate goal of translational research into sex and gender differences in this area would be to understand more about the different pathogenetic pathways in women and men and thereby possibly the etiology of these disorders in general.
References
Abel KM, Drake R, Goldstein JM (2010) Sex differences in schizophrenia. Int Rev Psychiatry 22(5):417–428. https://doi.org/10.3109/09540261.2010.515205
Akhondzadeh S, Rezaei F, Larijani B, Nejatisafa AA, Kashani L, Abbasi SH (2006) Correlation between testosterone, gonadotropins and prolactin and severity of negative symptoms in male patients with chronic schizophrenia. Schizophr Res 84(2-3):405–410. https://doi.org/10.1016/j.schres.2006.02.008
Albert K, Pruessner J, Newhouse P (2015) Estradiol levels modulate brain activity and negative responses to psychosocial stress across the menstrual cycle. Psychoneuroendocrinology 59:14–24. https://doi.org/10.1016/j.psyneuen.2015.04.022
Aleman A, Kahn RS, Selten JP (2003) Sex differences in the risk of schizophrenia: evidence from meta-analysis. Arch Gen Psychiatry 60(6):565–571. https://doi.org/10.1001/archpsyc.60.6.565
Arendt M, Rosenberg R, Foldager L, Perto G, Munk-Jorgensen P (2005) Cannabis-induced psychosis and subsequent schizophrenia-spectrum disorders: follow-up study of 535 incident cases. Br J Psychiatry 187:510–515. https://doi.org/10.1192/bjp.187.6.510
Ayesa-Arriola R, Rodriguez-Sanchez JM, Gomez-Ruiz E, Roiz-Santiáñez R, Reeves LL, Crespo-Facorro B (2014) No sex differences in neuropsychological performance in first episode psychosis patients. Prog Neuro-Psychopharmacol Biol Psychiatry 48(Supplement C):149–154. https://doi.org/10.1016/j.pnpbp.2013.09.009
Ayhan Y, McFarland R, Pletnikov MV (2016) Animal models of gene–environment interaction in schizophrenia: a dimensional perspective. Prog Neurobiol 136:1–27. https://doi.org/10.1016/j.pneurobio.2015.10.002
Baldwin CH, Srivastava LK (2015) Can the neurodevelopmental theory account for sex differences in schizophrenia across the life span? J Psychiatry Neurosci 40(2):75–77
Barajas A, Ochoa S, Obiols JE, Lalucat-Jo L (2015) Gender differences in individuals at high-risk of psychosis: a comprehensive literature review. Sci World J 2015:430735. https://doi.org/10.1155/2015/430735
Barker-Collo S, Read J (2011) The roles of gender and coping styles in the relationship between child abuse and the SCL90-R subscales ‘psychoticism’ and ‘paranoid ideation’. NZ J Psychol 40:28–38
Bertani M, Lasalvia A, Bonetto C, Tosato S, Cristofalo D, Bissoli S, De Santi K, Mazzoncini R, Lazzarotto L, Santi M, Sale A, Scalabrin D, Abate M, Tansella M, Rugger M (2012) The influence of gender on clinical and social characteristics of patients at psychosis onset: a report from the Psychosis Incident Cohort Outcome Study (PICOS). Psychol Med 42(4):769–780. https://doi.org/10.1017/S0033291711001991
Bora E, Fornito A, Radua J, Walterfang M, Seal M, Wood SJ, Yucel M, Velakoulis D, Pantelis C (2011) Neuroanatomical abnormalities in schizophrenia: a multimodal voxelwise meta-analysis and meta-regression analysis. Schizophr Res 127(1-3):46–57. https://doi.org/10.1016/j.schres.2010.12.020
Boss L, Kang DH, Marcus M, Bergstrom N (2014) Endogenous sex hormones and cognitive function in older adults: a systematic review. West J Nurs Res 36(3):388–426. https://doi.org/10.1177/0193945913500566
Brekke JS, Nakagami E (2010) The relevance of neurocognition and social cognition for outcome and recovery in schizophrenia. Neurocognition and social cognition in schizophrenia patients. Basic concepts and treatment. Karger, Basel
Bugra H, Studerus E, Rapp C, Tamagni C, Aston J, Borgwardt S, Riecher-Rössler A (2013) Cannabis use and cognitive functions in at-risk mental state and first episode psychosis. Psychopharmacology 230(2):299–308. https://doi.org/10.1007/s00213-013-3157-y
Bundy H, Stahl D, MacCabe JH (2011) A systematic review and meta-analysis of the fertility of patients with schizophrenia and their unaffected relatives. Acta Psychiatr Scand 123(2):98–106. https://doi.org/10.1111/j.1600-0447.2010.01623.x
Cahill L (2006) Why sex matters for neuroscience. Nat Rev Neurosci 7(6):477–484. https://doi.org/10.1038/nrn1909
Cannon TD (2015) How schizophrenia develops: cognitive and brain mechanisms underlying onset of psychosis. Trends Cogn Sci 19(12):744–756. https://doi.org/10.1016/j.tics.2015.09.009
Canuso CM, Pandina G (2007) Gender and schizophrenia. Psychopharmacol Bull 40(4):178–190
Carlson LE, Sherwin BB (1999) Relationships among cortisol (CRT), dehydroepiandrosterone-sulfate (DHEAS), and memory in a longitudinal study of healthy elderly men and women. Neurobiol Aging 20(3):315–324. https://doi.org/10.1016/S0197-4580(99)00052-4
Carter CS, Barch DM, Gur R, Gur R, Pinkham A, Ochsner K (2009) CNTRICS final task selection: social cognitive and affective neuroscience-based measures. Schizophr Bull 35(1):153–162. https://doi.org/10.1093/schbul/sbn157
Cascio MT, Cella M, Preti A, Meneghelli A, Cocchi A (2012) Gender and duration of untreated psychosis: a systematic review and meta-analysis. Early Interv Psychiatry 6(2):115–127. https://doi.org/10.1111/j.1751-7893.2012.00351.x
Chase KA, Rosen C, Rubin LH, Feiner B, Bodapati AS, Gin H, Hu E, Sharma RP (2015) Evidence of a sex-dependent restrictive epigenome in schizophrenia. J Psychiatr Res 65:87–94. https://doi.org/10.1016/j.jpsychires.2015.04.005
Cotton SM, Lambert M, Schimmelmann BG, Foley DL, Morley KI, McGorry PD, Conus P (2009) Gender differences in premorbid, entry, treatment, and outcome characteristics in a treated epidemiological sample of 661 patients with first episode psychosis. Schizophr Res 114(1-3):17–24. https://doi.org/10.1016/j.schres.2009.07.002
Crocker CE, Tibbo PG (2017) The interaction of gender and cannabis in early phase psychosis. Schizophr Res. https://doi.org/10.1016/j.schres.2017.04.046
Cuesta MJ, Peralta V (2008) Current psychopathological issues in psychosis: towards a phenome-wide scanning approach. Schizophr Bull 34(4):587–590. https://doi.org/10.1093/schbul/sbn041
Danaher H, Allott K, Killackey E, Hester R, Cotton S (2017) An examination of sex differences in neurocognition and social cognition in first-episode psychosis. Psychiatry Res 259:36–43. https://doi.org/10.1016/j.psychres.2017.09.053
Davidson M, Galderisi S, Weiser M, Werbeloff N, Fleischhacker WW, Keefe RS, Boter H, Keet IP, Prelipceanu D, Rybakowski JK, Libiger J, Hummer M, Dollfus S, Lopez-Ibor JJ, Hranov LG, Gaebel W, Peuskens J, Lindefors N, Riecher-Rössler A, Kahn RS (2009) Cognitive effects of antipsychotic drugs in first-episode schizophrenia and schizophreniform disorder: a randomized, open-label clinical trial (EUFEST). Am J Psychiatry 166(6):675–682. https://doi.org/10.1176/appi.ajp.2008.08060806
van der Werf M, Hanssen M, Köhler S, Verkaaik M, Verhey FR, Investigators R, van Winkel R, van Os J, Allardyce J (2014) Systematic review and collaborative recalculation of 133,693 incident cases of schizophrenia. Psychol Med 44(1):9–16. https://doi.org/10.1017/s0033291712002796
Di Forti M, Sallis H, Allegri F, Trotta A, Ferraro L, Stilo SA, Marconi A, La Cascia C, Reis Marques T, Pariante C, Dazzan P, Mondelli V, Paparelli A, Kolliakou A, Prata D, Gaughran F, David AS, Morgan C, Stahl D, Khondoker M, MacCabe JH, Murray RM (2014) Daily use, especially of high-potency cannabis, drives the earlier onset of psychosis in cannabis users. Schizophr Bull 40(6):1509–1517. https://doi.org/10.1093/schbul/sbt181
Duggal HS, Muddasani S, Keshavan MS (2005) Insular volumes in first-episode schizophrenia: gender effect. Schizophr Res 73(1):113–120. https://doi.org/10.1016/j.schres.2004.08.027
Egloff L, Lenz C, Studerus E, Harrisberger F, Simieskova R, Schmidt A, Huber C, Simon A, Lang UE, Riecher-Rössler A, Borgwardt S (2018) Sexually dimorphic subcortical brain volumes in emerging psychosis. Schizophr Res. https://doi.org/10.1016/j.schres.2018.03.034
Eranti SV, MacCabe JH, Bundy H, Murray RM (2013) Gender difference in age at onset of schizophrenia: a meta-analysis. Psychol Med 43(1):155–167. https://doi.org/10.1017/S003329171200089X
Esterberg ML, Trotman HD, Holtzman C, Compton MT, Walker EF (2010) The impact of a family history of psychosis on age-at-onset and positive and negative symptoms of schizophrenia: a meta-analysis. Schizophr Res 120(1-3):121–130. https://doi.org/10.1016/j.schres.2010.01.011
EU Report on Promoting Gender Equality in Mental Health and Clinical Research (2016/2096(INI)) by the Committee on Women’s Rights and Gender Equality (2016). http://www.europarl.europa.eu/sides/getDoc.do?pubRef=-a//EP//TEXT+REPORT+A8-2016-0380+0+DOC+XML+Vo//EN
Falkenburg J, Tracy DK (2014) Sex and schizophrenia: a review of gender differences. Psychosis 6(1):61–69. https://doi.org/10.1080/17522439.2012.733405
Fatouros-Bergman H, Cervenka S, Flyckt L, Edman G, Farde L (2014) Meta-analysis of cognitive performance in drug-naive patients with schizophrenia. Schizophr Res 158(1-3):156–162. https://doi.org/10.1016/j.schres.2014.06.034
Ferrari M, Flora N, Anderson KK, Haughton A, Tuck A, Archie S, Kidd S, McKenzie K, Team ACEP (2016) Gender differences in pathways to care for early psychosis. Early Interv Psychiatry. doi:https://doi.org/10.1111/eip.12324
Filatova S, Marttila R, Koivumaa-Honkanen H, Nordstrom T, Veijola J, Maki P, Khandaker GM, Isohanni M, Jaaskelainen E, Moilanen K, Miettunen J (2017) A comparison of the cumulative incidence and early risk factors for psychotic disorder in young adults in the Northern Finland Birth Cohorts 1966 and 1986. Epidemiol Psychiatr Sci 26(3):314–324. https://doi.org/10.1017/S2045796016000123
Fischer B, Gleason C, Asthana S (2014) Effects of hormone therapy on cognition and mood. Fertility and Sterility 101 (4):898–904.
Frederikse M, Lu A, Aylward E, Barta P, Sharma T, Pearlson G (2000) Sex differences in inferior parietal lobule volume in schizophrenia. Am J Psychiatry 157(3):422–427. https://doi.org/10.1176/appi.ajp.157.3.422
Fridgen GJ, Aston J, Gschwandtner U, Pflueger M, Zimmermann R, Studerus E, Stieglitz RD, Riecher-Rössler A (2013) Help-seeking and pathways to care in the early stages of psychosis. Soc Psychiatry Psychiatr Epidemiol 48:1033–1043. https://doi.org/10.1007/s00127-012-0628-0
Fusar-Poli P, Bonoldi I, Yung AR, Borgwardt S, Kempton MJ, Valmaggia L, Barale F, Caverzasi E, McGuire P (2012a) Predicting psychosis: meta-analysis of transition outcomes in individuals at high clinical risk. Arch Gen Psychiatry 69(3):220–229. https://doi.org/10.1001/archgenpsychiatry.2011.1472
Fusar-Poli P, McGuire P, Borgwardt S (2012b) Mapping prodromal psychosis: a critical review of neuroimaging studies. Eur Psychiatry 27(3):181–191. https://doi.org/10.1016/j.eurpsy.2011.06.006
Fusar-Poli P, Rutigliano G, Stahl D, Davies C, Bonoldi I, Reilly T, McGuire P (2017) Development and validation of a clinically based risk calculator for the transdiagnostic prediction of psychosis. JAMA Psychiatry 74(5):493–500. https://doi.org/10.1001/jamapsychiatry.2017.0284
Galderisi S, Bucci P, Ucok A, Peuskens J (2012) No gender differences in social outcome in patients suffering from schizophrenia. Eur Psychiatry 27(6):406–408. https://doi.org/10.1016/j.eurpsy.2011.01.011
Garcia M, Montalvo I, Creus M, Cabezas A, Sole M, Algora MJ, Moreno I, Gutierrez-Zotes A, Labad J (2016) Sex differences in the effect of childhood trauma on the clinical expression of early psychosis. Compr Psychiatry 68:86–96. https://doi.org/10.1016/j.comppsych.2016.04.004
Gibson LE, Anglin DM, Klugman JT, Reeves LE, Fineberg AM, Maxwell SD, Kerns CM, Ellman LM (2014) Stress sensitivity mediates the relationship between traumatic life events and attenuated positive psychotic symptoms differentially by gender in a college population sample. J Psychiatr Res 53(Supplement C):111–118. https://doi.org/10.1016/j.jpsychires.2014.02.020
Gibson LE, Alloy LB, Ellman LM (2016) Trauma and the psychosis spectrum: a review of symptom specificity and explanatory mechanisms. Clin Psychol Rev 49:92–105. https://doi.org/10.1016/j.cpr.2016.08.003
Gillies GE, McArthur S (2010) Estrogen actions in the brain and the basis for differential action in men and women: a case for sex-specific medicines. Pharmacol Rev 62(2):155–198. https://doi.org/10.1124/pr.109.002071
Goel N, Workman JL, Lee TT, Innala L, Viau V (2014) Sex differences in the HPA axis. Compr Physiol 4(3):1121–1155. https://doi.org/10.1002/cphy.c130054
Gogos A, Sbisa AM, Sun J, Gibbons A, Udawela M, Dean B (2015) A role for estrogen in schizophrenia: clinical and preclinical findings. Int J Endocrinol 2015:16. https://doi.org/10.1155/2015/615356
Goldstein JM, Seidman LJ, O'Brien LM, Horton NJ, Kennedy DN, Makris N, Caviness VS Jr, Faraone SV, Tsuang MT (2002) Impact of normal sexual dimorphisms on sex differences in structural brain abnormalities in schizophrenia assessed by magnetic resonance imaging. Arch Gen Psychiatry 59(2):154–164
Goldstein JM, Seidman LJ, Makris N, Ahern T, O'Brien LM, Caviness VS Jr, Kennedy DN, Faraone SV, Tsuang MT (2007) Hypothalamic abnormalities in schizophrenia: sex effects and genetic vulnerability. Biol Psychiatry 61(8):935–945. https://doi.org/10.1016/j.biopsych.2006.06.027
Goldstein JM, Jerram M, Abbs B, Whitfield-Gabrieli S, Makris N (2010) Sex differences in stress response circuitry activation dependent on female hormonal cycle. J Neurosci 30(2):431–438. https://doi.org/10.1523/jneurosci.3021-09.2010
Goldstein JM, Cherkerzian S, Seidman LJ, Petryshen TL, Fitzmaurice G, Tsuang MT, Buka SL (2011) Sex-specific rates of transmission of psychosis in the New England high-risk family study. Schizophr Res 128(1-3):150–155. https://doi.org/10.1016/j.schres.2011.01.019
Goldstein JM, Cherkerzian S, Tsuang MT, Petryshen TL (2013) Sex differences in the genetic risk for schizophrenia: history of the evidence for sex-specific and sex-dependent effects. Am J Med Genet B Neuropsychiatr Genet 162B(7):698–710. https://doi.org/10.1002/ajmg.b.32159
Gonzalez-Blanco L, Greenhalgh AM, Garcia-Rizo C, Fernandez-Egea E, Miller BJ, Kirkpatrick B (2016) Prolactin concentrations in antipsychotic-naive patients with schizophrenia and related disorders: a meta-analysis. Schizophr Res 174(1-3):156–160. https://doi.org/10.1016/j.schres.2016.03.018
González-Rodríguez A, Studerus E, Spitz A, Bugra H, Aston J, Borgwardt S, Rapp C, Riecher-Rössler A (2014) Gender differences in the psychopathology of emerging psychosis. Isr J Psychiatry Relat Sci 51(2):85–93
Gur RE, Cowell PE, Latshaw A, Turetsky BI, Grossman RI, Arnold SE, Bilker WB, Gur RC (2000) Reduced dorsal and orbital prefrontal gray matter volumes in schizophrenia. Arch Gen Psychiatry 57(8):761–768
Gur RE, Kohler C, Turetsky BI, Siegel SJ, Kanes SJ, Bilker WB, Brennan AR, Gur RC (2004) A sexually dimorphic ratio of orbitofrontal to amygdala volume is altered in schizophrenia. Biol Psychiatry 55(5):512–517. https://doi.org/10.1016/j.biopsych.2003.10.009
Haarmans M (2015) Improving our science in psychosis research with a sex- and gender-based analysis. In: Sáenz-Herrero M (ed) Psychopathology in women: incorporating gender perspective into descriptive psychopathology. Springer International Publishing, Cham, pp 83–110. https://doi.org/10.1007/978-3-319-05870-2_5
Häfner H, Riecher A, Maurer K, Löffler W, Munk-Jorgensen P, Stromgren E (1989) How does gender influence age at first hospitalization for schizophrenia? A transnational case register study. Psychol Med 19(4):903–918
Häfner H, Riecher-Rössler A, Fätkenheuer B, Hambrecht M, Löffler W, An der Heiden W (1991a) Sex differences in schizophrenia. Psychiatr Fenn 22:123–156
Häfner H, Riecher A, Maurer K, Fatkenheuer B, Löffler W, an der Heiden W, Munk-Jorgensen P, Stromgren E (1991b) [Sex differences in schizophrenic diseases] ([Sex differences in schizophrenic diseases]). Fortschr Neurol Psychiatr 59(9):343–360
Häfner H, Riecher-Rössler A, Maurer K, Fatkenheuer B, Löffler W (1992) First onset and early symptomatology of schizophrenia. A chapter of epidemiological and neurobiological research into age and sex differences. Eur Arch Psychiatry Clin Neurosci 242(2-3):109–118
Häfner H, Maurer K, Löffler W, Riecher-Rössler A (1993) The influence of age and sex on the onset and early course of schizophrenia. Br J Psychiatry 162:80–86
Häfner H, Maurer K, Löffler W, Fatkenheuer B, an der Heiden W, Riecher-Rössler A, Behrens S, Gattaz WF (1994) The epidemiology of early schizophrenia. Influence of age and gender on onset and early course. Br J Psychiatry Suppl (23):29-38
Heidari S, Babor TF, De Castro P, Tort S, Curno M (2016) Sex and gender equity in research: rationale for the SAGER guidelines and recommended use. Res Integr Peer Rev 1(1):2. https://doi.org/10.1186/s41073-016-0007-6
Heitz U, Papmeyer M, Menghini-Müller S, Egloff L, Ittig S, Navarra A, Studerus E, Riecher-Rössler A (2017) Gender differences in first self-perceived signs and symptoms in patients with an at-risk mental state and first episode psychosis. Early Interv Psychiatry. doi:https://doi.org/10.1111/eip.12528
Heringa SM, Begemann MJ, Goverde AJ, Sommer IE (2015) Sex hormones and oxytocin augmentation strategies in schizophrenia: a quantitative review. Schizophr Res 168(3):603–613. https://doi.org/10.1016/j.schres.2015.04.002
Herting MM, Maxwell EC, Irvine C, Nagel BJ (2012) The impact of sex, puberty, and hormones on white matter microstructure in adolescents. Cereb Cortex 22(9):1979–1992. https://doi.org/10.1093/cercor/bhr246
Hill RA (2016) Sex differences in animal models of schizophrenia shed light on the underlying pathophysiology. Neurosci Biobehav Rev 67:41–56. https://doi.org/10.1016/j.neubiorev.2015.10.014
Höfer P, Lanzenberger R, Kasper S (2013) Testosterone in the brain: neuroimaging findings and the potential role for neuropsychopharmacology. Eur Neuropsychopharmacol 23(2):79–88. https://doi.org/10.1016/j.euroneuro.2012.04.013
Hoff AL, Wieneke M, Faustman WO, Horon R, Sakuma M, Blankfeld H, Espinoza S, DeLisi LE (1998) Sex differences in neuropsychological functioning of first-episode and chronically ill schizophrenic patients. Am J Psychiatry 155(10):1437–1439. https://doi.org/10.1176/ajp.155.10.1437
Hoff AL, Kremen WS, Wieneke MH, Lauriello J, Blankfeld HM, Faustman WO, Csernansky JG, Nordahl TE (2001) Association of estrogen levels with neuropsychological performance in women with schizophrenia. Am J Psychiatry 158(7):1134–1139
Holtzman CW, Larson MK, Addington J, Cadenhead K, Cannon TD, Cornblatt B, Heinssen R, McGlashan T, Perkins D, Seidman LJ, Tsuang M, Woods SW, Walker EF (2010) Poster: sex differences in symptom presentation in individuals at risk for psychosis. Schizophr Res 117(2):304–305. https://doi.org/10.1016/j.schres.2010.02.508
Howard LM, Ehrlich AM, Gamlen F, Oram S (2017) Gender-neutral mental health research is sex and gender biased. Lancet Psychiatry 4(1):9–11. https://doi.org/10.1016/S2215-0366(16)30209-7
Howes OD, Kapur S (2009) The dopamine hypothesis of schizophrenia: version III—the final common pathway. Schizophr Bull 35(3):549–562. https://doi.org/10.1093/schbul/sbp006
Huber TJ, Tettenborn C, Leifke E, Emrich HM (2005) Sex hormones in psychotic men. Psychoneuroendocrinology 30(1):111–114. https://doi.org/10.1016/j.psyneuen.2004.05.010
Hui CL, Leung CM, Chang WC, Chan SK, Lee EH, Chen EY (2016) Examining gender difference in adult-onset psychosis in Hong Kong. Early Interv Psychiatry 10(4):324–333. https://doi.org/10.1111/eip.12167
Ingalhalikar M, Smith A, Parker D, Satterthwaite TD, Elliott MA, Ruparel K, Hakonarson H, Gur RE, Gur RC, Verma R (2014) Sex differences in the structural connectome of the human brain. Proc Natl Acad Sci U S A 111(2):823–828. https://doi.org/10.1073/pnas.1316909110
Irani F, Seligman S, Kamath V, Kohler C, Gur RC (2012) A meta-analysis of emotion perception and functional outcomes in schizophrenia. Schizophr Res 137(1-3):203–211. https://doi.org/10.1016/j.schres.2012.01.023
Irle E, Lange C, Ruhleder M, Exner C, Siemerkus J, Weniger G (2011) Hippocampal size in women but not men with schizophrenia relates to disorder duration. Psychiatry Res 192(3):133–139. https://doi.org/10.1016/j.pscychresns.2010.12.009
Ittig S, Studerus E, Papmeyer M, Uttinger M, Koranyi S, Ramyead A, Riecher-Rössler A (2015) Sex differences in cognitive functioning in at-risk mental state for psychosis, first episode psychosis and healthy control subjects. Eur Psychiatry 30:242–250. https://doi.org/10.1016/j.eurpsy.2014.11.006
Ittig S, Studerus E, Heitz U, Menghini-Müller S, Beck K, Egloff L, Leanza L, Andreou C, Riecher-Rössler A (2017) Sex differences in prolactin levels in emerging psychosis: indication for enhanced stress reactivity in women. Schizophr Res 189:111–116. https://doi.org/10.1016/j.schres.2017.02.010
Jääskelainen E, Juola P, Hirvonen N, McGrath JJ, Saha S, Isohanni M, Veijola J, Miettunen J (2013) A systematic review and meta-analysis of recovery in schizophrenia. Schizophr Bull 39(6):1296–1306. https://doi.org/10.1093/schbul/sbs130
Jablensky A, Sartorius N, Ernberg G, Anker M, Korten A, Cooper JE, Day R, Bertelsen A (1992) Schizophrenia: manifestations, incidence and course in different cultures. A World Health Organization ten-country study. Psychol Med Monogr Suppl 20:1–97
Jimenez JA, Mancini-Marie A, Lakis N, Rinaldi M, Mendrek A (2010) Disturbed sexual dimorphism of brain activation during mental rotation in schizophrenia. Schizophr Res 122(1-3):53–62. https://doi.org/10.1016/j.schres.2010.03.011
Kelly DL, Rowland LM, Patchan KM, Sullivan K, Earl A, Raley H, Liu F, Feldman S, McMahon RP (2016) Schizophrenia clinical symptom differences in women vs. men with and without a history of childhood physical abuse. Child Adolesc Psychiatry Ment Health 10:5. https://doi.org/10.1186/s13034-016-0092-9
Khan SS, Secades-Villa R, Okuda M, Wang S, Perez-Fuentes G, Kerridge BT, Blanco C (2013) Gender differences in cannabis use disorders: results from the National Epidemiologic Survey of Alcohol and Related Conditions. Drug Alcohol Depend 130(1-3):101–108. https://doi.org/10.1016/j.drugalcdep.2012.10.015
Kirkbride JB, Errazuriz A, Croudace TJ, Morgan C, Jackson D, Boydell J, Murray RM, Jones PB (2012) Incidence of schizophrenia and other psychoses in England, 1950–2009: a systematic review and meta-analyses. PLoS One 7(3):e31660. https://doi.org/10.1371/journal.pone.0031660
Koskinen J, Lohonen J, Koponen H, Isohanni M, Miettunen J (2010) Rate of cannabis use disorders in clinical samples of patients with schizophrenia: a meta-analysis. Schizophr Bull 36(6):1115–1130. https://doi.org/10.1093/schbul/sbp031
Koster A, Lajer M, Lindhardt A, Rosenbaum B (2008) Gender differences in first episode psychosis. Soc Psychiatry Psychiatr Epidemiol 43(12):940–946. https://doi.org/10.1007/s00127-008-0384-3
Kotlicka-Antczak M, Pawelczyk T, Podgorski M, Zurner N, Karbownik MS, Pawelczyk A (2016) Polish individuals with an at-risk mental state: demographic and clinical characteristics. Early Interv Psychiatry. https://doi.org/10.1111/eip.12333
Kraan TC, Velthorst E, Themmen M, Valmaggia L, Kempton MJ, McGuire P, van Os J, Rutten BPF, Smit F, de Haan L, van der Gaag M (2018) Child maltreatment and clinical outcome in individuals at ultra-high risk for psychosis in the EU-GEI high risk study. Schizophr Bull 44(3):584-592. doi:https://doi.org/10.1093/schbul/sbw162
Kring AM, Gordon AH (1998) Sex differences in emotion: expression, experience, and physiology. J Pers Soc Psychol 74(3):686–703. https://doi.org/10.1037/0022-3514.74.3.686
Kudielka BM, Kirschbaum C (2005) Sex differences in HPA axis responses to stress: a review. Biol Psychol 69(1):113–132. https://doi.org/10.1016/j.biopsycho.2004.11.009
Kühl JOG, Laursen TM, Thorup A, Nordentoft M (2016) The incidence of schizophrenia and schizophrenia spectrum disorders in Denmark in the period 2000–2012. A register-based study. Schizophr Res 176(2-3):533–539. https://doi.org/10.1016/j.schres.2016.06.023
Labad J, Stojanovic-Perez A, Montalvo I, Sole M, Cabezas A, Ortega L, Moreno I, Vilella E, Martorell L, Reynolds RM, Gutierrez-Zotes A (2015) Stress biomarkers as predictors of transition to psychosis in at-risk mental states: roles for cortisol, prolactin and albumin. J Psychiatr Res 60:163–169. https://doi.org/10.1016/j.jpsychires.2014.10.011
Lally J, Ajnakina O, Stubbs B, Williams HR, Colizzi M, Carra E, Fraietta S, Gardner-Sood P, Greenwood KE, Atakan Z, Mondelli V, Ismail K, Howes O, Taylor DM, Smith S, Hopkins D, Murray RM, Gaughran F (2017) Hyperprolactinaemia in first episode psychosis—a longitudinal assessment. Schizophr Res 189:117-125. doi:https://doi.org/10.1016/j.schres.2017.07.037
Lange EH, Nesvåg R, Ringen PA, Hartberg CB, Haukvik UK, Andreassen OA, Melle I, Agartz I (2014) One year follow-up of alcohol and illicit substance use in first-episode psychosis: does gender matter? Compr Psychiatry 55(2):274–282. https://doi.org/10.1016/j.comppsych.2013.08.018
Large M, Sharma S, Compton MT, Slade T, Nielssen O (2011) Cannabis use and earlier onset of psychosis: a systematic meta-analysis. Arch Gen Psychiatry 68(6):555–561. https://doi.org/10.1001/archgenpsychiatry.2011.5
Lennartsson AK, Jonsdottir IH (2011) Prolactin in response to acute psychosocial stress in healthy men and women. Psychoneuroendocrinology 36(10):1530–1539. https://doi.org/10.1016/j.psyneuen.2011.04.007
Leung MDDA, Chue MRC, Psych DP (2000) Sex differences in schizophrenia, a review of the literature. Acta Psychiatr Scand 101(401):3–38. https://doi.org/10.1111/j.0065-1591.2000.0ap25.x
Longenecker J, Genderson J, Dickinson D, Malley J, Elvevåg B, Weinberger DR, Gold J (2010) Where have all the women gone?: participant gender in epidemiological and non-epidemiological research of schizophrenia. Schizophr Res 119(1):240–245. https://doi.org/10.1016/j.schres.2010.03.023
Low M (2016) Chapter 7—neuroendocrinology. In: Melmed S, Polonsky K, Laresen P, Kronenberg H (eds) Williams textbook of endocrinology, 13th edn. W.B. Saunders Co, Philadelphia, pp 109–175. https://doi.org/10.1016/B978-0-323-29738-7.00007-1
MacMaster FP, Keshavan M, Mirza Y, Carrey N, Upadhyaya AR, El-Sheikh R, Buhagiar CJ, Taormina SP, Boyd C, Lynch M, Rose M, Ivey J, Moore GJ, Rosenberg DR (2007) Development and sexual dimorphism of the pituitary gland. Life Sci 80(10):940–944. https://doi.org/10.1016/j.lfs.2006.11.040
Maki PM, Dumas J (2009) Mechanisms of action of estrogen in the brain: insights from human neuroimaging and psychopharmacologic studies. Semin Reprod Med 27(3):250–259. https://doi.org/10.1055/s-0029-1216278
Marchbanks RM, Ryan M, Day IN, Owen M, McGuffin P, Whatley SA (2003) A mitochondrial DNA sequence variant associated with schizophrenia and oxidative stress. Schizophr Res 65(1):33–38
Maric N, Krabbendam L, Vollebergh W, de Graaf R, van Os J (2003) Sex differences in symptoms of psychosis in a non-selected, general population sample. Schizophr Res 63(1-2):89–95
Maric N, Popovic V, Jasovic-Gasic M, Pilipovic N, van Os J (2005) Cumulative exposure to estrogen and psychosis: a peak bone mass, case-control study in first-episode psychosis. Schizophr Res 73(2-3):351–355. https://doi.org/10.1016/j.schres.2004.07.016
Maric NP, Raballo A, Rojnic Kuzman M, Andric Petrovic S, Klosterkötter J, Riecher-Rössler A (2017) European status and perspectives on early detection and intervention in at-risk mental state and first episode psychosis: viewpoint from the EPA section for prevention of mental disorders. Eur Psychiatry 46(Supplement C):48–50. https://doi.org/10.1016/j.eurpsy.2017.08.003
Markham JA (2012) Sex steroids and schizophrenia. Rev Endocr Metab Disord 13(3):187–207. https://doi.org/10.1007/s11154-011-9184-2
Mayo D, Corey S, Kelly LH, Yohannes S, Youngquist AL, Stuart BK, Niendam TA, Loewy RL (2017) The role of trauma and stressful life events among individuals at clinical high risk for psychosis: a review. Front Psychiatry 8:55. https://doi.org/10.3389/fpsyt.2017.00055
McCarthy MM (2008) Estradiol and the developing brain. Physiol Rev 88(1):91–124. https://doi.org/10.1152/physrev.00010.2007
McCarthy MM (2015) Incorporating sex as a variable in preclinical neuropsychiatric research. Schizophr Bull 41(5):1016–1020. https://doi.org/10.1093/schbul/sbv077
McEwen BS, Milner TA (2017) Understanding the broad influence of sex hormones and sex differences in the brain. J Neurosci Res 95(1-2):24–39. https://doi.org/10.1002/jnr.23809
McGrath J, Saha S, Chant D, Welham J (2008) Schizophrenia: a concise overview of incidence, prevalence, and mortality. Epidemiol Rev 30:67–76. https://doi.org/10.1093/epirev/mxn001
Melcangi RC, Panzica G, Garcia-Segura LM (2011) Neuroactive steroids: focus on human brain. Neuroscience 191:1–5. https://doi.org/10.1016/j.neuroscience.2011.06.024
Mendrek A (2007) Reversal of normal cerebral sexual dimorphism in schizophrenia: evidence and speculations. Med Hypotheses 69(4):896–902. https://doi.org/10.1016/j.mehy.2007.01.064
Mendrek A, Stip E (2011) Sexual dimorphism in schizophrenia: is there a need for gender-based protocols? Expert Rev Neurother 11(7):951–959. https://doi.org/10.1586/ern.11.78
Mendrek A, Mancini-Marie A, Fahim C, Stip E (2007) Sex differences in the cerebral function associated with processing of aversive stimuli by schizophrenia patients. Aust N Z J Psychiatry 41(2):136–141. https://doi.org/10.1080/00048670601109907
Menghini-Müller S, Studerus E, Heitz U, Egloff L, Ittig S, Riecher-Rössler A (2016) Gender differences in the symptomatology of patients at-risk for psychosis—results from the EU-GEI study. In: 5th Biennial SIRS Conference, Florence, Italy, 2–6 April 2016. vol 2. npj Schizophrenia, pp 19–20
Moore L, Kyaw M, Vercammen A, Lenroot R, Kulkarni J, Curtis J, O’Donnell M, Carr VJ, Shannon Weickert C, Weickert TW (2013) Serum testosterone levels are related to cognitive function in men with schizophrenia. Psychoneuroendocrinology 38(9):1717–1728. https://doi.org/10.1016/j.psyneuen.2013.02.007
Morris RW, Purves-Tyson TD, Weickert CS, Rothmond D, Lenroot R, Weickert TW (2015) Testosterone and reward prediction-errors in healthy men and men with schizophrenia. Schizophr Res 168(3):649-660. doi:https://doi.org/10.1016/j.schres.2015.06.030
Murray RM, Quigley H, Quattrone D, Englund A, Di Forti M (2016) Traditional marijuana, high-potency cannabis and synthetic cannabinoids: increasing risk for psychosis. World Psychiatry 15(3):195–204. https://doi.org/10.1002/wps.20341
Myin-Germeys I, Krabbendam L, Delespaul PA, van Os J (2004) Sex differences in emotional reactivity to daily life stress in psychosis. J Clin Psychiatry 65(6):805–809
Narr KL, Bilder RM, Kim S, Thompson PM, Szeszko P, Robinson D, Luders E, Toga AW (2004) Abnormal gyral complexity in first-episode schizophrenia. Biol Psychiatry 55(8):859–867. https://doi.org/10.1016/j.biopsych.2003.12.027
Newhouse P, Albert K (2015) Estrogen, stress, and depression: a neurocognitive model. JAMA Psychiatry 72(7):727–729. https://doi.org/10.1001/jamapsychiatry.2015.0487
Newman SC, Bland RC, Thompson AH (2012) Long-term course and outcome in schizophrenia: a 34-year follow-up study in Alberta, Canada. Psychol Med 42(10):2137–2143. https://doi.org/10.1017/S0033291712000177
Ngun TC, Ghahramani N, Sanchez FJ, Bocklandt S, Vilain E (2011) The genetics of sex differences in brain and behavior. Front Neuroendocrinol 32(2):227–246. https://doi.org/10.1016/j.yfrne.2010.10.001
Nordholm D, Krogh J, Mondelli V, Dazzan P, Pariante C, Nordentoft M (2013) Pituitary gland volume in patients with schizophrenia, subjects at ultra high-risk of developing psychosis and healthy controls: a systematic review and meta-analysis. Psychoneuroendocrinology 38(11):2394–2404. https://doi.org/10.1016/j.psyneuen.2013.06.030
Novick D, Haro JM, Hong J, Brugnoli R, Lepine JP, Bertsch J, Karagianis J, Dossenbach M, Alvarez E (2012) Regional differences in treatment response and three year course of schizophrenia across the world. J Psychiatr Res 46(7):856–864. https://doi.org/10.1016/j.jpsychires.2012.03.017
Nunez C, Ochoa S, Huerta-Ramos E, Banos I, Barajas A, Dolz M, Sanchez B, Del Cacho N, Group G, Usall J (2016) Differential effects of sex on substance use between first episode psychosis patients and healthy people. Compr Psychiatry 69:169–178. https://doi.org/10.1016/j.comppsych.2016.05.017
O’Leary DS, Flaum M, Kesler ML, Flashman LA, Arndt S, Andreasen NC (2000) Cognitive correlates of the negative, disorganized, and psychotic symptom dimensions of schizophrenia. J Neuropsychiatr Clin Neurosci 12(1):4–15. https://doi.org/10.1176/jnp.12.1.4
Ochoa S, Usall J, Cobo J, Labad X, Kulkarni J (2012) Gender differences in schizophrenia and first-episode psychosis: a comprehensive literature review. Schizophr Res Treat 2012:916198. https://doi.org/10.1155/2012/916198
van Os J, EU-GEI-Study-Group (2014) European Network of National Networks studying Gene–Environment Interactions in Schizophrenia: identifying gene–environment interactions in schizophrenia: contemporary challenges for integrated, large-scale investigations. Schizophr Bull 40(4):729–736. https://doi.org/10.1093/schbul/sbu069
Petrikis P, Tigas S, Tzallas AT, Archimandriti DT, Skapinakis P, Mavreas V (2016) Prolactin levels in drug-naive patients with schizophrenia and other psychotic disorders. Int J Psychiatry Clin Pract 20(3):165–169. https://doi.org/10.1080/13651501.2016.1197274
Pinkham AE, Kelsven S, Kouros C, Harvey PD, Penn DL (2017) The effect of age, race, and sex on social cognitive performance in individuals with schizophrenia. J Nerv Ment Dis 205(5):346–352. https://doi.org/10.1097/NMD.0000000000000654
Pompili A, Arnone B, Gasbarri A (2012) Estrogens and memory in physiological and neuropathological conditions. Psychoneuroendocrinology 37(9):1379–1396. https://doi.org/10.1016/j.psyneuen.2012.01.007
Pruessner M, Lepage M, Collins DL, Pruessner JC, Joober R, Malla AK (2015) Reduced hippocampal volume and hypothalamus-pituitary-adrenal axis function in first episode psychosis: evidence for sex differences. Neuroimage Clin 7:195–202. https://doi.org/10.1016/j.nicl.2014.12.001
Pruessner M, Faridi K, Shah J, Rabinovitch M, Iyer S, Abadi S, Pawliuk N, Joober R, Malla AK (2017) The Clinic for Assessment of Youth at Risk (CAYR): 10 years of service delivery and research targeting the prevention of psychosis in Montreal, Canada. Early Interv Psychiatry 11(2):177–184. https://doi.org/10.1111/eip.12300
Resnick S, Driscoll I (2008) Sex differences in brain aging and Alzheimer’s disease. In: Becker J, Berkley K, Geary N (eds) Sex differences in the brain: from genes to behavior. Oxford University Press, Oxford, pp 427–454
Riecher-Rössler A (1994) Die Spätschizophrenie - eine valide Entität? Eine empirische Studie zu Risikofaktoren, Krankheitsbild und Verlauf. Habilitationsschrift. Fakultät für klinische Medizin Mannheim, Universität Heidelberg. Habilitationsschrift
Riecher-Rössler A (2003) Oestrogens and schizophrenia. Curr Opin Psychiatry 16:187–192
Riecher-Rössler A (2005) Estrogens and schizophrenia. In: Bergemann N, Riecher-Rössler A (eds) Estrogen effects in psychiatric disorders. Springer, Wien, pp 31–52
Riecher-Rössler A (2009) Psychotic disorders and menopause: the untold story. The menopausal transition—interface between gynecology and psychiatry. Karger, Basel
Riecher-Rössler A (2017) Oestrogens, prolactin, hypothalamic–pituitary–gonadal axis, and schizophrenic psychoses. Lancet Psychiatry 4(1):63–72. https://doi.org/10.1016/S2215-0366(16)30379-0
Riecher-Rössler A (in print) Vulnerability and protective factors for mental health: a rereading in gender perspective. In: Tarricone I, Riecher-Rössler A (eds) Health and gender. Resilience factors in the health of women in contemporary society. Springer International Publishing AG, Cham
Riecher-Rössler A, Häfner H (1993) Schizophrenia and oestrogens—is there an association? Eur Arch Psychiatry Clin Neurosci 242(6):323–328
Riecher-Rössler A, Häfner H (2000) Gender aspects in schizophrenia: bridging the border between social and biological psychiatry. Acta Psychiatr Scand Suppl 407:58–62
Riecher-Rössler A, Kulkarni J (2011) Estrogens and gonadal function in schizophrenia and related psychoses. Curr Top Behav Neurosci 8:155–171. https://doi.org/10.1007/7854_2010_100
Riecher-Rössler A, McGorry P (2016) Early detection and intervention in psychosis. State of the art and future perspectives. Key Issues Ment Health, vol 181. Karger, Basel
Riecher-Rössler A, Rössler W (1998) The course of schizophrenic psychoses: what do we really know? A selective review from an epidemiological perspective. Eur Arch Psychiatry Clin Neurosci 248(4):189–202
Riecher-Rössler A, Studerus E (2016) High time for a paradigm shift in psychiatry. World Psychiatry 15(2):131–133. https://doi.org/10.1002/wps.20329
Riecher-Rössler A, Studerus E (2017) Prediction of conversion to psychosis in individuals with an at-risk mental state: a brief update on recent developments. Curr Opin Psychiatry 30(3):209–219. https://doi.org/10.1097/YCO.0000000000000320
Riecher-Rössler A, Häfner H, Stumbaum M, Maurer K, Schmidt R (1994) Can estradiol modulate schizophrenic symptomatology? Schizophr Bull 20(1):203–214
Riecher-Rössler A, Löffler W, Munk-Jorgensen P (1997) What do we really know about late-onset schizophrenia? Eur Arch Psychiatry Clin Neurosci 247(4):195–208
Riecher-Rössler A, Pflueger MO, Aston J, Borgwardt SJ, Brewer WJ, Gschwandtner U, Stieglitz RD (2009) Efficacy of using cognitive status in predicting psychosis: a 7-year follow-up. Biol Psychiatry 66(11):1023–1030. https://doi.org/10.1016/j.biopsych.2009.07.020
Riecher-Rössler A, Pflueger MO, Borgwardt S (2010) Schizophrenia in women. In: Kohen D (ed) Oxford textbook of women and mental health. Oxford University Press, Oxford, pp 102–114
Riecher-Rössler A, Rybakowski JK, Pflueger MO, Beyrau R, Kahn RS, Malik P, Fleischhacker WW (2013) Hyperprolactinemia in antipsychotic-naive patients with first-episode psychosis. Psychol Med 43(12):2571–2582. https://doi.org/10.1017/S0033291713000226
Rietdijk J, Ising HK, Dragt S, Klaassen R, Nieman D, Wunderink L, Cuijpers P, Linszen D, van der Gaag M (2013) Depression and social anxiety in help-seeking patients with an ultra-high risk for developing psychosis. Psychiatry Res 209(3):309–313. https://doi.org/10.1016/j.psychres.2013.01.012
Rietschel L, Lambert M, Karow A, Zink M, Muller H, Heinz A, de Millas W, Janssen B, Gaebel W, Schneider F, Naber D, Juckel G, Kruger-Ozgurdal S, Wobrock T, Wagner M, Maier W, Klosterkotter J, Bechdolf A, group Ps (2017) Clinical high risk for psychosis: gender differences in symptoms and social functioning. Early Interv Psychiatry 11(4):306–313. https://doi.org/10.1111/eip.12240
van Rijn S, Aleman A, de Sonneville L, Sprong M, Ziermans T, Schothorst P, van Engeland H, Swaab H (2011) Neuroendocrine markers of high risk for psychosis: salivary testosterone in adolescent boys with prodromal symptoms. Psychol Med 41(9):1815–1822. https://doi.org/10.1017/S0033291710002576
Ritsner MS (2011) The clinical and therapeutic potentials of dehydroepiandrosterone and pregnenolone in schizophrenia. Neuroscience 191:91–100. https://doi.org/10.1016/j.neuroscience.2011.04.017
Rubin LH, Carter CS, Drogos L, Pournajafi-Nazarloo H, Sweeney JA, Maki PM (2010) Peripheral oxytocin is associated with reduced symptom severity in schizophrenia. Schizophr Res 124(1-3):13–21. https://doi.org/10.1016/j.schres.2010.09.014
Saha S, Chant D, Welham J, McGrath J (2005) A systematic review of the prevalence of schizophrenia. PLoS Med 2(5):e141. https://doi.org/10.1371/journal.pmed.0020141
Salokangas RK, Stengard E (1990) Gender and short-term outcome in schizophrenia. Schizophr Res 3(5-6):333–345
Sanchez MG, Bourque M, Morissette M, Di Paolo T (2010) Steroids–dopamine interactions in the pathophysiology and treatment of CNS disorders. CNS Neurosci Ther 16(3):e43–e71. https://doi.org/10.1111/j.1755-5949.2010.00163.x
Seedat S, Scott KM, Angermeyer MC, Berglund P, Bromet EJ, Brugha TS, Demyttenaere K, de Girolamo G, Haro JM, Jin R, Karam EG, Kovess-Masfety V, Levinson D, Medina Mora ME, Ono Y, Ormel J, Pennell BE, Posada-Villa J, Sampson NA, Williams D, Kessler RC (2009) Cross-national associations between gender and mental disorders in the World Health Organization World Mental Health Surveys. Arch Gen Psychiatry 66(7):785–795. https://doi.org/10.1001/archgenpsychiatry.2009.36
Seeman MV (2013) Women and schizophrenia: new findings. Neuropsychiatry 3(4):423–431
Shibre T, Medhin G, Alem A, Kebede D, Teferra S, Jacobsson L, Kullgren G, Hanlon C, Fekadu A (2015) Long-term clinical course and outcome of schizophrenia in rural Ethiopia: 10-year follow-up of a population-based cohort. Schizophr Res 161(2-3):414–420. https://doi.org/10.1016/j.schres.2014.10.053
Shimamoto A, Rappeneau V (2017) Sex-dependent mental illnesses and mitochondria. Schizophr Res 187:38-46. doi:https://doi.org/10.1016/j.schres.2017.02.025
da Silva TL, Ravindran AV (2015) Contribution of sex hormones to gender differences in schizophrenia: a review. Asian J Psychiatr 18:2–14. https://doi.org/10.1016/j.ajp.2015.07.016
Smieskova R, Marmy J, Schmidt A, Bendfeldt K, Riecher-Rössler A, Walter M, Lang UE, Borgwardt S (2013) Do subjects at clinical high risk for psychosis differ from those with a genetic high risk?—a systematic review of structural and functional brain abnormalities. Curr Med Chem 20(3):467–481
Spitz A, Studerus E, Koranyi S, Rapp C, Ramyead A, Ittig S, Heitz U, Uttinger M, Riecher-Rössler A (2015) Correlations between self-rating and observer-rating of psychopathology in at-risk mental state and first-episode psychosis patients: influence of disease stage and gender. Early Interv Psychiatry 11:461-470. doi:https://doi.org/10.1111/eip.12270
Sun J, Walker AJ, Dean B, van den Buuse M, Gogos A (2016) Progesterone: the neglected hormone in schizophrenia? A focus on progesterone–dopamine interactions. Psychoneuroendocrinology 74:126–140. https://doi.org/10.1016/j.psyneuen.2016.08.019
Taherianfard M, Shariaty M (2004) Evaluation of serum steroid hormones in schizophrenic patients. Indian J Med Sci 58(1):3–9
Takahashi T, Kawasaki Y, Kurokawa K, Hagino H, Nohara S, Yamashita I, Nakamura K, Murata M, Matsui M, Suzuki M, Seto H, Kurachi M (2002) Lack of normal structural asymmetry of the anterior cingulate gyrus in female patients with schizophrenia: a volumetric magnetic resonance imaging study. Schizophr Res 55(1-2):69–81
Takahashi T, Nakamura K, Nishiyama S, Furuichi A, Ikeda E, Kido M, Nakamura Y, Kawasaki Y, Noguchi K, Seto H, Suzuki M (2013) Increased pituitary volume in subjects at risk for psychosis and patients with first-episode schizophrenia. Psychiatry Clin Neurosci 67(7):540–548. https://doi.org/10.1111/pcn.12093
Takayanagi Y, Takahashi T, Orikabe L, Mozue Y, Kawasaki Y, Nakamura K, Sato Y, Itokawa M, Yamasue H, Kasai K, Kurachi M, Okazaki Y, Suzuki M (2011) Classification of first-episode schizophrenia patients and healthy subjects by automated MRI measures of regional brain volume and cortical thickness. PLoS One 6(6):e21047. https://doi.org/10.1371/journal.pone.0021047
Taylor GT, Maloney S, Dearborn J, Weiss J (2009) Hormones in the mentally disturbed brain: steroids and peptides in the development and treatment of psychopathology. Cent Nerv Syst Agents Med Chem 9(4):331–360
Theodoridou A, Hengartner MP, Heekeren K, Dvorsky D, Schultze-Lutter F, Gerstenberg M, Walitza S, Rössler W (2017) Influence of demographic characteristics on attenuated positive psychotic symptoms in a young, help-seeking, at-risk population. Early Interv Psychiatry doi:https://doi.org/10.1111/eip.12444
Thorup A, Petersen L, Jeppesen P, Ohlenschlaeger J, Christensen T, Krarup G, Jorgensen P, Nordentoft M (2007) Gender differences in young adults with first-episode schizophrenia spectrum disorders at baseline in the Danish OPUS study. J Nerv Ment Dis 195(5):396–405. https://doi.org/10.1097/01.nmd.0000253784.59708.dd
Thorup A, Albert N, Bertelsen M, Petersen L, Jeppesen P, Le Quack P, Krarup G, Jorgensen P, Nordentoft M (2014) Gender differences in first-episode psychosis at 5-year follow-up—two different courses of disease? Results from the OPUS study at 5-year follow-up. Eur Psychiatry 29(1):44–51. https://doi.org/10.1016/j.eurpsy.2012.11.005
Toffol E, Heikinheimo O, Partonen T (2015) Hormone therapy and mood in perimenopausal and postmenopausal women: a narrative review. Menopause, 22(5), 564–578.
Trotman HD, Holtzman CW, Walker EF, Addington JM, Bearden CE, Cadenhead KS, Cannon TD, Cornblatt BA, Heinssen RK, Mathalon DH, Tsuang MT, Perkins DO, Seidman LJ, Woods SW, McGlashan TH (2014) Stress exposure and sensitivity in the clinical high-risk syndrome: initial findings from the North American Prodrome Longitudinal Study (NAPLS). Schizophr Res 160(1-3):104–109. https://doi.org/10.1016/j.schres.2014.09.017
Tseliou F, Johnson S, Major B, Rahaman N, Joyce J, Lawrence J, Mann F, Tapfumaneyi A, Chisholm B, Chamberlain-Kent N, Hinton MF, Fisher HL, MiData C (2017) Gender differences in one-year outcomes of first-presentation psychosis patients in inner-city UK Early Intervention Services. Early Interv Psychiatry 11(3):215–223. https://doi.org/10.1111/eip.12235
Vigod SN, Ross LE (2010) Epidemiology of psychotic symptoms during pregnancy and postpartum in women with schizophrenia. Curr Women’s Health Rev 6(1):17–21. https://doi.org/10.2174/157340410790979725
Vogeley K, Schneider-Axmann T, Pfeiffer U, Tepest R, Bayer TA, Bogerts B, Honer WG, Falkai P (2000) Disturbed gyrification of the prefrontal region in male schizophrenic patients: a morphometric postmortem study. Am J Psychiatry 157(1):34–39. https://doi.org/10.1176/ajp.157.1.34
Vuksan-Cusa B, Sagud M, Rados I (2016) The role of dehydroepiandrosterone (DHEA) in schizophrenia. Psychiatr Danub 28(1):30–33
Waford RN, MacDonald A, Goines K, Novacek DM, Trotman HD, Elaine FW, Addington J, Bearden CE, Cadenhead KS, Cannon TD, Cornblatt BA, Heinssen R, Mathalon DH, Tsuang MT, Perkins DO, Seidman LJ, Woods SW, McGlashan TH (2015) Demographic correlates of attenuated positive psychotic symptoms. Schizophr Res 166(1-3):31–36. https://doi.org/10.1016/j.schres.2015.04.035
Walder DJ, Mittal V, Trotman HD, McMillan AL, Walker EF (2008) Neurocognition and conversion to psychosis in adolescents at high-risk. Schizophr Res 101(1):161–168. https://doi.org/10.1016/j.schres.2007.12.477
Walder DJ, Holtzman CW, Addington J, Cadenhead K, Tsuang M, Cornblatt B, Cannon TD, McGlashan TH, Woods SW, Perkins DO, Seidman LJ, Heinssen R, Walker EF (2013) Sexual dimorphisms and prediction of conversion in the NAPLS psychosis prodrome. Schizophr Res 144(1-3):43–50. https://doi.org/10.1016/j.schres.2012.11.039
Walder DJ, Yaffe B, Ehrlich Y (2016) Chapter 5—sexual dimorphisms in psychosis risk: a neurodevelopmental perspective. In: Shansky RM (ed) Sex differences in the central nervous system. Academic Press, San Diego, pp 107–127. https://doi.org/10.1016/B978-0-12-802114-9.00005-6
Walker EF, Lewine RR (1993) Sampling biases in studies of gender and schizophrenia. Schizophr Bull 19(1):1–7 discussion 9–14
Walter A, Studerus E, Smieskova R, Tamagni C, Rapp C, Borgwardt SJ, Riecher-Rössler A (2015) Pituitary gland volume in at-risk mental state for psychosis: a longitudinal MRI analysis. CNS Spectr 20(2):122–129. https://doi.org/10.1017/S109285291400011X
Watson CS, Alyea RA, Cunningham KA, Jeng YJ (2010) Estrogens of multiple classes and their role in mental health disease mechanisms. Int J Womens Health 2:153–166
Weickert TW, Allen KM, Weickert CS (2016) Potential role of oestrogen modulation in the treatment of neurocognitive deficits in schizophrenia. CNS Drugs 30(2):125–133. https://doi.org/10.1007/s40263-016-0312-0
Wilson RP, Patel R, Bhattacharyya S (2017) Do fewer males present to clinical high-risk services for psychosis relative to first-episode services? Early Interv Psychiatry 11(5):429–435. https://doi.org/10.1111/eip.12311
Wing J, Cooper JE, Sartorius N (1973) Present State Examination (PSE). Deutsche Bearbeitung von M.v.Cranach 1978. Med Res Counc (GB)
Wing J, Cooper JE, Sartorius N (1974) Measurement and classification of psychiatric symptoms. An instruction manual for the PSE and Catego program. Cambridge University Press, London
Zubin J, Spring B (1977) Vulnerability—a new view of schizophrenia. J Abnorm Psychol 86(2):103–126
Zucker I, Beery AK (2010) Males still dominate animal studies. Nature 465(7299):690. https://doi.org/10.1038/465690a
Acknowledgment
We thank Claudine Pfister, MA, for her help in the preparation of the manuscript.
Funding
This research did not receive any specific grants or funding.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Riecher-Rössler, A., Butler, S. & Kulkarni, J. Sex and gender differences in schizophrenic psychoses—a critical review. Arch Womens Ment Health 21, 627–648 (2018). https://doi.org/10.1007/s00737-018-0847-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00737-018-0847-9