Abstract
Diabetes is a chronic metabolic disease associated with oxidative stress, damage to biomolecules such as DNA, and neuroinflammation. Taurine, a sulfur-containing amino acid widespread in the brain, has neuroprotective properties that might prevent tissue injury and DNA damage induced by chronic hyperglycemia. We evaluated the effects of chronic taurine treatment on oxidative stress parameters, DNA damage and inflammatory markers in the frontal cortex, and hippocampus of streptozotocin-induced diabetic rats. Diabetic rats displayed increased levels of reactive oxygen species (ROS) and DNA damage in both areas, evidencing the pro-oxidant effects of diabetes in the brain. Moreover, this condition increased levels of several inflammatory mediators, such as IL-6, IL-12, TNF-γ, and IFN-α, more pronouncedly in the hippocampus. Supporting our hypothesis, taurine treatment reduced ROS, DNA damage, and inflammatory cytokine levels, providing evidence of its beneficial effects against genotoxicity and neuroinflammation associated with diabetes. Our data endorse the necessary clinical trials to evaluate the efficacy and safety of taurine supplementation in the prevention and treatment of neurochemical and metabolic alterations related to diabetes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In diabetic individuals, poor glycemic control is related to microvascular (retinopathy, nephropathy, and neuropathy) and macrovascular (cardiovascular ischemia, stroke, and peripheral vascular disease) complications (Cade 2008). Chronic hyperglycemia also induces metabolic and vascular alterations in the central nervous system (CNS), elevating the risk of cognitive decline, dementia, and mood disorders (Gispen and Biessels 2000; Anderson et al. 2001).
The neuropathological changes observed in the brain of diabetic individuals have been associated with an unbalance between pro- and antioxidant systems—which results in oxidative stress—and nonenzymatic glycation and glycoxidation of proteins—generating advanced glycation end products (AGEs) (Yamagishi and Matsui 2010; Giacco and Brownlee 2010). Oxidative stress and the consequent overproduction of reactive oxygen species (ROS) by the mitochondrial electron transport chain may lead to irreversible damage to lipids, proteins, and DNA (Nishikawa et al. 2000; Brownlee 2001), which is potentiated by the presence of AGEs (Lee and Chan 2015). The brain is sensitive to oxidative damage, and alterations in the redox status have been linked to cognitive deficits and mood disorders in diabetic patients (Floyd 1999; Malkov et al. 2014).
Another consequence of ROS overproduction in the CNS is microglial activation and sustained release of pro-inflammatory cytokines, leading to a state of chronic neuroinflammation (Leszek et al. 2016). Endogenous defenses, including antioxidant enzymes such as superoxide dismutase (SOD) and catalase (CAT), or exogenous defenses such as ascorbic acid, α-tocopherol, and polyphenols, can prevent, attenuate, or interrupt the pro-oxidant and pro-inflammatory cycle (Rajendran et al. 2014).
Taurine is a sulfur-containing amino acid with osmoregulatory, antioxidant, and neuroprotective properties (Jong et al. 2012; Lambert et al. 2015). Studies have shown that taurine improves learning and memory in aged mice (El Idrissi 2008b) and decreases depressive-like behaviors in diabetic and non-diabetic rats (Caletti et al. 2012; Toyoda and Iio 2013). Acute taurine administration also exerts anxiolytic-like effects in mice and in zebrafish (El Idrissi et al. 2009; Mezzomo et al. 2016), which may be explained by its property of enhancing GABAergic transmission (Jia et al. 2008; L’Amoreaux et al. 2010). Our group has also shown that taurine increases GABAA receptor α2 subunit and BDNF mRNA expression in the hippocampus of diabetic rats (Caletti et al. 2015). In addition, taurine has been found to improve whole body glucose control, lower triglyceride and cholesterol levels, and control blood pressure (Chen et al. 2016).
Considering its neuroprotective effects and its ability to ameliorate cognitive and behavioral deficits in conditions associated with oxidative stress and neuroinflammation, we hypothesized that taurine counteracts the deleterious effects of chronic hyperglycemia in relevant brain regions of diabetic rats. To answer this question, we evaluated the effects of chronic taurine treatment on oxidative stress parameters, DNA damage, and inflammatory markers in the frontal cortex and hippocampus of streptozotocin-induced diabetic rats.
Materials and methods
Animals
Adult male Wistar rats (270–300 g) were born and reared in the animal facility of Universidade Federal do Rio Grande do Sul (UFRGS), Brazil. Animals were housed 4 per cage and kept under controlled environmental conditions (12-h light/dark cycle, 22 ± 1 °C) with free access to food and water. All experiments had been previously approved by the university Ethics Committee for Animal Use (CEUA-UFRGS #26303) and followed the International Institute of Health Guide for the Care and Use of Laboratory Animals and the guidelines from Conselho Nacional de Controle de Experimentação Animal (CONCEA).
Experimental procedure
Diabetes was induced by a single intraperitoneal (i.p.) injection of streptozotocin (STZ, 50 mg/kg, Sigma, St. Louis, MO, USA), which was dissolved in citrate buffer, pH 4.3 (n = 12). Control (CTR) animals received a vehicle i.p. injection at a volume of 1 mL/kg (n = 12). 48 h later, a blood drop was drawn from a superficial puncture in the distal tail. Blood glucose was instantly measured with a glucometer (Accu-Check Active monitoring system, Roche Diagnostics, Rotkreuz, Switzerland). Only animals with glucose levels higher than 200 mg/dL were kept in the study. After diabetes confirmation, rats were randomly allocated to receive taurine (TAU, 100 mg/kg, i.p.) or saline, once a day for 28 days (n = 5–6/group). The dose of TAU was chosen based on the previous studies from our group (Caletti et al. 2012, 2015). Body weight was measured weekly throughout the experimental period. After the end of treatment, animals were euthanized and the frontal cortex and hippocampi were dissected and stored at −80 °C for neurochemical analyses. These brain regions were chosen, because they are likely involved in the deleterious consequences of hyperglycemia and oxidative stress, and have a prominent role in the functions known to be affected by diabetes.
Oxidative stress parameters: SOD, CAT, and DCFH-DA assays
Brain tissue was homogenized in phosphate-buffered saline (pH 7.4) using a homogenizer, and then centrifuged for 5 min. The supernatant was used for the assays, and all procedures were performed under cold conditions.
The DCFH-DA assay is a reliable method for measuring intracellular reactive oxygen species (ROS) such as hydrogen peroxide (H2O2), hydroxyl radical (OH·), and hydroperoxides (ROOH). The method is based on the deacetylation of the DCFH-DA probe, and its subsequent oxidation by ROS into a highly fluorescent compound (2′,7′-dichlorofluorescein; DCF) (Halliwell and Gutteridge 2007). For this assay, phosphate-buffered saline (pH 7.4), 500 µM DCFH-DA, and 5 µL of tissue suspension were incubated in 96-well dark plates at 37 °C for 30 min. Fluorescence was measured using a spectrofluorometer (SpectraMax, Molecular Devices, Sunnyvale, CA, USA). Excitation and emission wavelengths were 490 nm and 525 nm, respectively (Ko et al. 2005). All experiments were carried out in a dark room to prevent the oxidation of DCHF-DA. The results were expressed as intensity of fluorescence from DCF per mg of protein.
SOD activity was determined according to Misra and Fridovich (Misra and Fridovich 1972), and the results were expressed as SOD units per mg of protein. CAT activity was determined by the H2O2 decomposition rate as described by Aebi (1984) and was expressed as CAT units per mg of protein.
DNA damage: comet assay
In this assay, fragmented DNA migrates through permeabilized nuclear and cytoplasmic membranes, producing a “tail” from the nuclear head. Single- and double-strand breaks and alkali-labile sites were measured by the alkaline version of the comet assay, performed according to the method described by Hartmann et al. (2003). Briefly, brain tissue samples were placed in microtubes filled with 1 mL phosphate-buffered saline, 20 mM EDTA, and 10% dimethylsulphoxide (DMSO), and then chopped with a scissor. The pieces were allowed to settle down and the supernatant containing single cells was collected. The isolated cells were counted in a Neubauer chamber to determine cell concentration and survival by trypan blue exclusion assay in accordance with Uliasz and Hewett (2000).
The single-cell suspension (104 cells/mL) was dissolved in 0.75% low-melting point agarose, and spreads onto a glass microscope slide pre-coated with a layer of agarose. Slides were then incubated in ice-cold lysis solution (2.5 M NaCl, 10 mM Tris, 100 mM EDTA, 1% Triton X-100, and 10% DMSO, pH 10.0) at 4 °C for 24 h to remove cell membranes, leaving DNA as “nucleoids”. Slides were placed in a horizontal electrophoresis unit and incubated with fresh buffer solution (300 mM NaOH, 1 mM EDTA, pH 13.0) at 4 °C for 15 min to allow DNA unwinding and the expression of alkali-labile sites. Electrophoresis was conducted for 15 min at 25 V and 300 mA (94 V/cm). Slides were then neutralized (0.4 M Tris, pH 7.5) and stained using the silver-staining method (Nadin et al. 2001). From each sample, 100 cells were selected and analyzed for DNA migration under a light microscope. These cells were visually scored according to tail length into class 0: undamaged, without a tail; class 1: with a tail shorter than the diameter of the head nucleus; class 2: with a tail length 1–2 times the diameter of the head; class 3: with a tail longer than 2 times the diameter of the head; and class 4: comets with no heads. Each sample was assigned a value of damage index, which is the summation of cell scores and thus may range from 0 to 400 (Burlinson et al. 2007). All steps were performed under yellow light to prevent additional DNA damage.
Inflammatory parameters: cytokine levels
Interleukin-6 (IL-6), interleukin-10 (IL-10), interleukin-12p70 (IL-12p70), tumor necrosis factor alpha (TNF-α), interferon gamma (IFN-γ), and monocyte chemoattractant protein-1 (MCP-1) levels were quantified in brain homogenates using a commercial kit (Cytometric Bead Array Mouse Inflammation Kit, BD Biosciences, San Diego, CA, USA). Briefly, 50 μL of samples or known concentrations of the standard samples (0–5000 pg/mL) were added to a mixture of 50 μL each of capture antibody bead reagent and phycoerythrin (PE)-conjugated detection antibody. The mixture was incubated for 2 h at room temperature and washed to remove unbound antibodies. Data were acquired using a FACS Aria III flow cytometer (BD Biosciences) and analyzed using the FCAP Array v2.0 software (BD Biosciences).
Statistical analysis
Data normality was assessed by Shapiro–Wilk test. Data were analyzed by two-way ANOVA with diabetes condition (STZ) and taurine treatment (TAU) as factors, followed by Tukey’s post hoc test when appropriate. Significance was set at P < 0.05. Results were presented as mean + standard error (SEM).
Results
Oxidative profile
Figure 1a shows that taurine (TAU) was able to counteract the increased SOD activity induced by streptozotocin (STZ) in the hippocampus; there was a significant interaction between STZ × TAU (P = 0.0054). Regarding CAT activity, TAU counteracted its increase in the hippocampus of diabetic rats (Fig. 1b); there were significant main effects of both STZ (P = 0.0162) and TAU (P = 0.0266). No significant changes in antioxidant enzymes activity were observed in the frontal cortex.
Effects of taurine (TAU) treatment (100 mg/kg, i.p.) on oxidative stress parameters in the frontal cortex and hippocampus of control (CTR) and streptozotocin-induced diabetic (STZ) rats. Antioxidant enzyme activity of a superoxide dismutase (SOD) and b catalase (CAT); c DCF fluorescence represents reactive oxygen species levels. Two-way ANOVA followed by Tukey’s post hoc test. *P < 0.05, **P < 0.01, post hoc comparisons; § P < 0.05, main effect of streptozotocin treatment; + P < 0.05, main effect of taurine treatment. Data presented as mean + SEM
ROS levels, as measured by DCF fluorescence, were increased in the frontal cortex and hippocampus of STZ rats, an effect also blocked by TAU (Fig. 1c). Two-way ANOVA revealed a significant main effect of TAU in the frontal cortex (P = 0.0082), as well as a significant main effect of STZ (P = 0.0034) and an interaction effect (P = 0.0216) in the hippocampus.
DNA damage
The neuropathological effects of chronic hyperglycemia were also evidenced by increased DNA damage in both areas of the brain. TAU partially protected brain cells from this loss of DNA integrity (Fig. 2b). Significant interactions between STZ × TAU were observed in the frontal cortex (P = 0.01) and hippocampus (P = 0.0002).
Effects of taurine (TAU) treatment (100 mg/kg, i.p.) on DNA damage in the frontal cortex and hippocampus of control (CTR) and streptozotocin-induced diabetic (STZ) rats. a Representative images of cell nuclei, comet assay. b Quantification of DNA damage. Two-way ANOVA followed by Tukey’s post hoc test. *P < 0.05, **P < 0.01, ***P < 0.001, post hoc comparisons. Data presented as mean + SEM
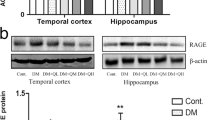
Inflammatory profile
In the frontal cortex, diabetic rats displayed increased levels of IL-6 and TNF-α; IL-6 levels were restored by TAU. In addition, TAU decreased the levels of IL-6, IL-12, IFN-γ, and MCP-1 in both control (CTRL) and STZ animals, indicating a generalized anti-inflammatory action in this brain area (Figs. 3, 4).
Effects of taurine (TAU) treatment (100 mg/kg, i.p.) on interleukin levels in the frontal cortex and hippocampus of control (CTR) and streptozotocin-induced diabetic (STZ) rats. a IL-6, b IL-10, and c IL-12 levels. Two-way ANOVA followed by Tukey’s post hoc test. *P < 0.05, **P < 0.01, post hoc comparisons; § P < 0.05, main effect of streptozotocin treatment; + P < 0.05, main effect of taurine treatment. Data presented as mean + SEM
Effects of taurine (TAU) treatment (100 mg/kg, i.p.) on inflammatory parameters in the frontal cortex and hippocampus of control (CTR) and streptozotocin-induced diabetic (STZ) rats. a Tumor necrosis factor alpha (TNF-α), b interferon gamma (IFNγ), and c monocyte chemoattractant protein-1 (MCP-1) levels. Two-way ANOVA followed by Tukey’s post hoc test. *P < 0.05, **P < 0.01, post hoc comparisons; § P < 0.05, main effect of streptozotocin treatment; + P < 0.05, main effect of taurine treatment. Data presented as mean + SEM
In the hippocampus, STZ increased the levels of IL-6, IL-12, TNF-α, and IFN-γ, all of which was counteracted by TAU. Especially, for IL-12 and IFN-γ, although TAU protected STZ animals from the increase in these inflammatory markers, it increased their levels in CTR animals. MCP-1 levels in the hippocampus were decreased in STZ groups (Figs. 3, 4).
The anti-inflammatory interleukin IL-10 was the only cytokine not significantly altered by either STZ or TAU in any of the brain regions (Fig. 3b). The results of statistical analyses are summarized in detail in supplementary Table S1.
Discussion
In the present study, we showed that diabetes increased ROS generation and DNA damage in the frontal cortex and hippocampus of rats; SOD and CAT activities were increased only in the hippocampus. Diabetes also increased several inflammatory mediators, most notably in the hippocampus than in the frontal cortex. Taurine blocked the increase in ROS, as indicated by DCF fluorescence restored to control group levels, and attenuated DNA damage in both brain regions of diabetic rats. Taurine also maintained SOD and CAT activities at control levels in the hippocampus, and decreased several inflammatory cytokines in both brain regions. Therefore, this set of results provides novel insights on the neuroprotective effects of taurine against oxidative stress, DNA damage, and inflammation in the brain of diabetic rats.
In a pro-oxidant environment, antioxidant enzymes are recruited in an attempt to scavenge free radicals and thus protect cells from injury (Biswas 2016). This compensatory mechanism explains the up-regulatory effect of the antioxidant enzymes SOD and CAT that we observed in the hippocampus of diabetic rats. SOD protects cells against the toxic effects of superoxide anion (O ·─2 ) by catalyzing its dismutation to hydrogen peroxide (H2O2) and water. CAT, in its turn, neutralizes the resulting H2O2 to avoid its reaction with metal ions such as iron and copper and the formation of the highly toxic hydroxyl radical (OH·) (Devasagayam et al. 2004). Despite the observed increase in antioxidant enzymes activity, chronic hyperglycemia led to DNA damage in both frontal cortex and hippocampus, as assessed by the comet assay.
Taurine is present at high concentrations in the CNS and plays an important role as an endogenous antioxidant (Schaffer et al. 2009). It is synthesized by astrocytes and accumulated by neurons from the extracellular medium (Brand et al. 1993). In diabetic rats, chronic hyperglycemia increases the expression of taurine transporters in the brain, which is counteracted by insulin administration (Trachtman et al. 1992). Our study confirms the antioxidant properties of taurine, since it neutralized oxidative stress and genotoxicity in the brain of diabetic rats. Beneficial antioxidant effects of taurine have already been reported in the testes of STZ-induced diabetic animals (Tsounapi et al. 2012; Abd El-Twab et al. 2016); however, our study is, to the best of our knowledge, the first to provide evidence that chronic taurine treatment reduces ROS and DNA damage in the brain of diabetic rats. There is some evidence that taurine can scavenge the superoxide anion in vitro, at physiological concentrations (Oliveira et al. 2010). Its action as a ROS scavenger may explain the decrease in DCFH-DA oxidation, enabling the restoration of SOD and CAT to normal levels and, consequently, reducing DNA damage. It can also be the case, however, that the antioxidant properties of taurine are due to a regulatory effect on mitochondrial function that boosts electron transport chain activity, maintaining a normal flow of electrons and avoiding their diversion to generate free radicals (Schaffer et al. 2009; Jong et al. 2010, 2012). The effects of taurine in regulating calcium homeostasis may also be related to its antioxidant activity, as this ion is an important regulator of several pathways implicated in oxidative stress (El Idrissi 2008a). The exact mechanism underlying taurine antioxidant actions is yet to be determined.
Chronic hyperglycemia increases the levels of inflammatory markers in patients with both type 1 and type 2 diabetes (Esposito 2002; Devaraj et al. 2006). In our study, we found that diabetes induced more pronounced pro-inflammatory effects in the hippocampus, increasing almost all the cytokines that we measured in this region. Indeed, the hippocampus is one of the most sensitive and responsive brain regions to changes in glucose homeostasis (Magariños and McEwen 2000; Pamidi and Satheesha Nayak 2012) and, therefore, is more vulnerable to inflammation resulting from hyperglycemia. Moreover, pro-inflammatory effects have been reported in different experimental protocols of diabetes, showing that a short period of hyperglycemia is sufficient to induce neuroinflammation (Giribabu et al. 2014; Datusalia and Sharma 2014; Liu et al. 2015).
Persistent activation of the nuclear factor kappa B (NF-κB) possibly mediates the neuroinflammatory effects observed in diabetic rats (Alvarez-Nölting et al. 2012), and is involved in oxidative stress and cell death (Biswas 2016). The anti-inflammatory effects of taurine may also be explained by modulation of the NF-κB pathway. Support for this hypothesis stems from the findings of Agca and colleagues (2014), who reported that taurine orally administered for 8 weeks blunts the increase in NF-κB expression in the brain of STZ-induced diabetic rats (Agca et al. 2014). In addition to anti-inflammatory effects in diabetic rats, we observed that taurine decreased IL-6, IL-12, IFN-γ, and MCP-1 in the frontal cortex of control rats. On the other hand, although it prevented STZ effects, taurine increased IL-12 and IFN-γ in the hippocampus of controls. This indicates that taurine may exert opposite effects depending on the glycemic status and the brain region. Moreover, treatment duration is known to dictate the neurochemical and behavioral effects of taurine. For example, acute taurine administration is anxiolytic, whereas chronic taurine supplementation is anxiogenic in non-diabetic mice (El Idrissi et al. 2009). Although speculative, the increase on hippocampal pro-inflammatory cytokines that we observed in control rats may explain this report of increased anxiety levels following chronic taurine treatment. It remains to be elucidated whether acute taurine would result in a differential effect on cytokine levels in control animals.
There is an important link between oxidative stress and inflammation, since the presence of one triggers the other and vice versa. Immune-activated cells release reactive species at the site of inflammation, leading to oxidative stress. On the other hand, ROS can initiate and potentiate intracellular signaling cascades that promote pro-inflammatory gene expression. This cycle elicits a series of intracellular events leading to cell dysfunction and apoptosis. Imbalance between the formation of ROS and antioxidant defenses further aggravates this process, contributing to the onset of diabetic complications. This pro-oxidant and pro-inflammatory environment is highly toxic to the CNS, and thus impairs neuronal transmission (Patel 2016). The hippocampus is a brain region particularly susceptible to oxidative and inflammatory injuries—this vulnerability is probably inherent to its singular neurochemical and metabolic characteristics (Rivas-Arancibia et al. 2010; Wang and Michaelis 2010). Indeed, in vivo proton nuclear magnetic resonance (1H-NMR) spectroscopy studies show that among three brain areas investigated (total cortex, striatum, and hippocampus), chronic hyperglycemia increases taurine levels only in the hippocampus of STZ-induced diabetic rats (Duarte et al. 2009; Zhang et al. 2015). The authors suggest that in this brain area, the osmoregulatory effect of taurine avoids ion-induced perturbation in protein function after 4 weeks of chronic hyperglycemia. Duarte and colleagues (2009) have shown that caffeine administration increases taurine levels and prevents synaptic degeneration and astrogliosis in the hippocampus of diabetic rats, evidencing a neuroprotective mechanism associated with osmolarity regulation (Duarte et al. 2009).
The vulnerability of the hippocampus is further evidenced by the increased risk of major depression and Alzheimer’s disease in diabetic patients, since hippocampal atrophy is linked to both conditions (Joko et al. 2016; De Winter et al. 2017). Interestingly, we have previously demonstrated that the same dose of taurine used here has antidepressant-like effects in STZ-induced diabetic rats (Caletti et al. 2012). It is likely that the antioxidant and anti-inflammatory actions of taurine play a role in its antidepressant effect. Furthermore, anti-inflammatory and antioxidant properties of taurine were also observed in the cortex and hippocampus of cognitively impaired rats after intracerebroventricular STZ injection (Reeta et al. 2017). Paralleling our findings, the authors have shown that the chronic oral doses of 120 mg/kg taurine decreased TNF-α and IL-1β in the hippocampus and total cortex, reversing the cognitive deficits in those rats (Reeta et al. 2017).
In summary, chronic taurine administration reduced ROS and DNA damage and decreased inflammatory markers in the diabetic rat brain. These effects may be due to the ROS scavenger properties of taurine and/or to its regulatory effects on the electron transport chain, decreasing free radicals generation and restoring antioxidant enzymes activity. In agreement with other studies, we found a more consistent response of taurine in the hippocampus of diabetic rats. This area-specific response may reflect the particular vulnerability of the hippocampus against a chronic hyperglycemia insult. The specific and more robust effect of taurine in diabetic rats may reflect increased expression of taurine transporters in the brain of these rats. We hypothesize that higher doses of taurine would present similar effects in non-diabetic rats.
The therapeutic potential of taurine is further supported by the fact that its endogenous concentrations are reduced in the plasma of rats and humans with diabetes (Goodman and Shihabi 1990; Franconi et al. 1995; De Luca et al. 2001). Therefore, supplementation of this amino acid may be important to restore its concentration to normal values and preserve physiological functions impaired by chronic hyperglycemia. The data reported here endorse the necessary clinical trials to evaluate the efficacy and safety of taurine supplementation in the prevention and treatment of neurochemical and metabolic alterations related to diabetes.
References
Abd El-Twab SM, Mohamed HM, Mahmoud AM (2016) Taurine and pioglitazone attenuate diabetes-induced testicular damage by abrogation of oxidative stress and up-regulation of the pituitary-gonadal axis. Can J Physiol Pharmacol 94:651–661. doi:10.1139/cjpp-2015-0503
Aebi H (1984) Catalase in vitro. Methods Enzymol 105:121–126
Agca CA, Tuzcu M, Hayirli A, Sahin K (2014) Taurine ameliorates neuropathy via regulating NF-κB and Nrf2/HO-1 signaling cascades in diabetic rats. Food Chem Toxicol 71:116–121. doi:10.1016/j.fct.2014.05.023
Alvarez-Nölting R, Arnal E, Barcia JM et al (2012) Protection by DHA of early hippocampal changes in diabetes: possible role of CREB and NF-κB. Neurochem Res 37:105–115. doi:10.1007/s11064-011-0588-x
Anderson RJ, Freedland KE, Clouse RE, Lustman PJ (2001) The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care 24:1069–1078. doi:10.2337/diacare.24.6.1069
Biswas SK (2016) Does the interdependence between oxidative stress and inflammation explain the antioxidant paradox? Oxid Med Cell Longev 2016:1–9. doi:10.1155/2016/5698931
Brand A, Richter-Landsberg C, Leibfritz D (1993) Multinuclear NMR studies on the energy metabolism of glial and neuronal cells. Dev Neurosci 15:289–298
Brownlee M (2001) Biochemistry and molecular cell biology of diabetic complications. Nature 414:813–820. doi:10.1038/414813a
Burlinson B, Tice RR, Speit G et al (2007) Fourth International Workgroup on Genotoxicity testing: results of the in vivo Comet assay workgroup. Mutat Res 627:31–35. doi:10.1016/j.mrgentox.2006.08.011
Cade WT (2008) Diabetes-related microvascular and macrovascular diseases in the physical therapy setting. Phys Ther 88:1322–1335. doi:10.2522/ptj.20080008
Caletti G, Olguins DB, Pedrollo EF et al (2012) Antidepressant effect of taurine in diabetic rats. Amino Acids 43:1525–1533. doi:10.1007/s00726-012-1226-x
Caletti G, Almeida FB, Agnes G et al (2015) Antidepressant dose of taurine increases mRNA expression of GABAA receptor α2 subunit and BDNF in the hippocampus of diabetic rats. Behav Brain Res 283:11–15. doi:10.1016/j.bbr.2015.01.018
Chen W, Guo J, Zhang Y, Zhang J (2016) The beneficial effects of taurine in preventing metabolic syndrome. Food Funct 7:1849–1863. doi:10.1039/C5FO01295C
Datusalia AK, Sharma SS (2014) Amelioration of diabetes-induced cognitive deficits by GSK-3β inhibition is attributed to modulation of neurotransmitters and neuroinflammation. Mol Neurobiol 50:390–405. doi:10.1007/s12035-014-8632-x
De Luca G, Calpona PR, Caponetti A et al (2001) Taurine and osmoregulation: platelet taurine content, uptake, and release in type 2 diabetic patients. Metabolism 50:60–64. doi:10.1053/meta.2001.19432
De Winter F-L, Emsell L, Bouckaert F et al (2017) No association of lower hippocampal volume with alzheimer’s disease pathology in late-life depression. Am J Psychiatry 174:237–245. doi:10.1176/appi.ajp.2016.16030319
Devaraj S, Glaser N, Griffen S et al (2006) Increased monocytic activity and biomarkers of inflammation in patients with type 1 diabetes. Diabetes 55:774–779
Devasagayam TPA, Tilak JC, Boloor KK et al (2004) Free radicals and antioxidants in human health: current status and future prospects. J Assoc Physicians India 52:794–804
Duarte JMN, Carvalho RA, Cunha RA, Gruetter R (2009) Caffeine consumption attenuates neurochemical modifications in the hippocampus of streptozotocin-induced diabetic rats. J Neurochem 111:368–379. doi:10.1111/j.1471-4159.2009.06349.x
El Idrissi A (2008a) Taurine increases mitochondrial buffering of calcium: role in neuroprotection. Amino Acids 34:321–328. doi:10.1007/s00726-006-0396-9
El Idrissi A (2008b) Taurine improves learning and retention in aged mice. Neurosci Lett 436:19–22. doi:10.1016/j.neulet.2008.02.070
El Idrissi A, Boukarrou L, Heany W et al (2009) Effects of taurine on anxiety-like and locomotor behavior of mice. Adv Exp Med Biol 643:207–215
Esposito K (2002) Inflammatory cytokine concentrations are acutely increased by hyperglycemia in humans: role of oxidative stress. Circulation 106:2067–2072. doi:10.1161/01.CIR.0000034509.14906.AE
Floyd RA (1999) Antioxidants, oxidative stress, and degenerative neurological disorders. Proc Soc Exp Biol Med 222:236–245
Franconi F, Bennardini F, Mattana A et al (1995) Plasma and platelet taurine are reduced in subjects with insulin-dependent diabetes mellitus: effects of taurine supplementation. Am J Clin Nutr 61:1115–1119
Giacco F, Brownlee M (2010) Oxidative stress and diabetic complications. Circ Res 107:1058–1070. doi:10.1161/CIRCRESAHA.110.223545
Giribabu N, Srinivasarao N, Swapna Rekha S et al (2014) Centella asiatica attenuates diabetes induced hippocampal changes in experimental diabetic rats. Evid Based Complement Altern Med 2014:1–10. doi:10.1155/2014/592062
Gispen WH, Biessels GJ (2000) Cognition and synaptic plasticity in diabetes mellitus. Trends Neurosci 23:542–549
Goodman HO, Shihabi ZK (1990) Supplemental taurine in diabetic rats: effects on plasma glucose and triglycerides. Biochem Med Metab Biol 43:1–9
Halliwell B, Gutteridge JMC (2007) Free radicals in biology and medicine, 4th edn. Oxford University Press, Oxford
Hartmann A, Agurell E, Beevers C et al (2003) Recommendations for conducting the in vivo alkaline Comet assay. 4th International Comet Assay Workshop. Mutagenesis 18:45–51
Jia F, Yue M, Chandra D et al (2008) Taurine is a potent activator of extrasynaptic GABA(A) receptors in the thalamus. J Neurosci Off J Soc Neurosci 28:106–115. doi:10.1523/JNEUROSCI.3996-07.2008
Joko T, Washizuka S, Sasayama D et al (2016) Patterns of hippocampal atrophy differ among Alzheimer’s disease, amnestic mild cognitive impairment, and late-life depression. Psychogeriatr Off J Jpn Psychogeriatr Soc 16:355–361. doi:10.1111/psyg.12176
Jong CJ, Ito T, Mozaffari M et al (2010) Effect of β-alanine treatment on mitochondrial taurine level and 5-taurinomethyluridine content. J Biomed Sci 17:S25. doi:10.1186/1423-0127-17-S1-S25
Jong CJ, Azuma J, Schaffer S (2012) Mechanism underlying the antioxidant activity of taurine: prevention of mitochondrial oxidant production. Amino Acids 42:2223–2232. doi:10.1007/s00726-011-0962-7
Ko S-H, Choi S-W, Ye S-K et al (2005) Comparison of the antioxidant activities of nine different fruits in human plasma. J Med Food 8:41–46. doi:10.1089/jmf.2005.8.41
L’Amoreaux WJ, Marsillo A, El Idrissi A (2010) Pharmacological characterization of GABAA receptors in taurine-fed mice. J Biomed Sci 17:S14. doi:10.1186/1423-0127-17-S1-S14
Lambert IH, Kristensen DM, Holm JB, Mortensen OH (2015) Physiological role of taurine–from organism to organelle. Acta Physiol Oxf Engl 213:191–212. doi:10.1111/apha.12365
Lee SC, Chan JCN (2015) Evidence for DNA damage as a biological link between diabetes and cancer. Chin Med J (Engl) 128:1543–1548. doi:10.4103/0366-6999.157693
Leszek J, Barreto GE, Gąsiorowski K et al (2016) Inflammatory mechanisms and oxidative stress as key factors responsible for progression of neurodegeneration: role of brain innate immune system. CNS Neurol Disord: Drug Targets 15:329–336
Liu X, Mo Y, Gong J et al (2015) Puerarin ameliorates cognitive deficits in streptozotocin-induced diabetic rats. Metab Brain Dis. doi:10.1007/s11011-015-9779-5
Magariños AM, McEwen BS (2000) Experimental diabetes in rats causes hippocampal dendritic and synaptic reorganization and increased glucocorticoid reactivity to stress. Proc Natl Acad Sci U S A 97:11056–11061
Malkov A, Ivanov AI, Popova I et al (2014) Reactive oxygen species initiate a metabolic collapse in hippocampal slices: potential trigger of cortical spreading depression. J Cereb Blood Flow Metab Off J Int Soc Cereb Blood Flow Metab 34:1540–1549. doi:10.1038/jcbfm.2014.121
Mezzomo NJ, Silveira A, Giuliani GS et al (2016) The role of taurine on anxiety-like behaviors in zebrafish: a comparative study using the novel tank and the light-dark tasks. Neurosci Lett 613:19–24. doi:10.1016/j.neulet.2015.12.037
Misra HP, Fridovich I (1972) The role of superoxide anion in the autoxidation of epinephrine and a simple assay for superoxide dismutase. J Biol Chem 247:3170–3175
Nadin SB, Vargas-Roig LM, Ciocca DR (2001) A silver staining method for single-cell gel assay. J Histochem Cytochem Off J Histochem Soc 49:1183–1186
Nishikawa T, Edelstein D, Du XL et al (2000) Normalizing mitochondrial superoxide production blocks three pathways of hyperglycaemic damage. Nature 404:787–790. doi:10.1038/35008121
Oliveira MWS, Minotto JB, de Oliveira MR et al (2010) Scavenging and antioxidant potential of physiological taurine concentrations against different reactive oxygen/nitrogen species. Pharmacol Rep PR 62:185–193
Pamidi N, Satheesha Nayak BN (2012) Effect of streptozotocin induced diabetes on rat hippocampus. Bratisl Lekárske Listy 113:583–588
Patel M (2016) Targeting oxidative stress in central nervous system disorders. Trends Pharmacol Sci 37:768–778. doi:10.1016/j.tips.2016.06.007
Rajendran P, Nandakumar N, Rengarajan T et al (2014) Antioxidants and human diseases. Clin Chim Acta 436:332–347. doi:10.1016/j.cca.2014.06.004
Reeta KH, Singh D, Gupta YK (2017) Chronic treatment with taurine after intracerebroventricular streptozotocin injection improves cognitive dysfunction in rats by modulating oxidative stress, cholinergic functions and neuroinflammation. Neurochem Int 108:146–156. doi:10.1016/j.neuint.2017.03.006
Rivas-Arancibia S, Guevara-Guzmán R, López-Vidal Y et al (2010) Oxidative stress caused by ozone exposure induces loss of brain repair in the hippocampus of adult rats. Toxicol Sci Off J Soc Toxicol 113:187–197. doi:10.1093/toxsci/kfp252
Schaffer SW, Azuma J, Mozaffari M (2009) Role of antioxidant activity of taurine in diabetes. Can J Physiol Pharmacol 87:91–99. doi:10.1139/Y08-110
Toyoda A, Iio W (2013) Antidepressant-like effect of chronic taurine administration and its hippocampal signal transduction in rats. Adv Exp Med Biol 775:29–43. doi:10.1007/978-1-4614-6130-2_3
Trachtman H, Futterweit S, Sturman JA (1992) Cerebral taurine transport is increased during streptozocin-induced diabetes in rats. Diabetes 41:1130–1140
Tsounapi P, Saito M, Dimitriadis F et al (2012) Antioxidant treatment with edaravone or taurine ameliorates diabetes-induced testicular dysfunction in the rat. Mol Cell Biochem 369:195–204. doi:10.1007/s11010-012-1382-z
Uliasz TF, Hewett SJ (2000) A microtiter trypan blue absorbance assay for the quantitative determination of excitotoxic neuronal injury in cell culture. J Neurosci Methods 100:157–163
Wang X, Michaelis EK (2010) Selective neuronal vulnerability to oxidative stress in the brain. Front Aging Neurosci. doi:10.3389/fnagi.2010.00012
Yamagishi S, Matsui T (2010) Advanced glycation end products, oxidative stress and diabetic nephropathy. Oxid Med Cell Longev 3:101–108. doi:10.4161/oxim.3.2.11148
Zhang H, Huang M, Gao L, Lei H (2015) Region-specific cerebral metabolic alterations in streptozotocin-induced type 1 diabetic rats: an in vivo proton magnetic resonance spectroscopy study. J Cereb Blood Flow Metab Off J Int Soc Cereb Blood Flow Metab 35:1738–1745. doi:10.1038/jcbfm.2015.111
Acknowledgements
We thank Solange Bandiera and Alana W Hansen for their technical support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was supported by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Universidade Federal de Ciências da Saúde de Porto Alegre (UFCSPA) and Pró-Reitoria de Pesquisa, Universidade Federal do Rio Grande do Sul (UFRGS), Brazil.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All applicable international, national, and or institutional guidelines for the care and use of animals were followed.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Caletti, G., Herrmann, A.P., Pulcinelli, R.R. et al. Taurine counteracts the neurotoxic effects of streptozotocin-induced diabetes in rats. Amino Acids 50, 95–104 (2018). https://doi.org/10.1007/s00726-017-2495-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00726-017-2495-1