Abstract
Microtubule components α- and β-tubulin undergo a number of posttranslational modifications that modulate their dynamics and cellular functions. These modifications include polyamination and covalent crosslinking by transglutaminase enzymes. We have demonstrated previously that the less dynamic and more stable tubulin form—detyrosinated Glu-tubulin—is found in high molecular weight, oligomeric complexes in bone-forming osteoblasts during differentiation and along with deposition of collagenous extracellular matrix. In this study, we report that oligomeric Glu-tubulin has high nocodazole tolerance, indicating further increased stability. We show that α-tubulin, which gives rise to Glu-tubulin, is a transglutaminase substrate in in vitro assays and that it is crosslinked into oligomers (dimers, trimers and tetramers) by transglutaminase 2 and Factor XIIIA; β-tubulin was not crosslinked by transglutaminase activity. The oligomeric Glu-tubulin was specifically localized to the plasma membrane of osteoblasts as analyzed by subcellular fractionation, cell surface biotinylation experiments and total internal reflection fluorescence (TIRF) microscopy. Glu- and α-tubulin co-localized with cellular Factor XIIIA as analyzed by conventional and TIRF microscopy. The Factor XIIIA-specific substrate peptide bF11 co-localized with α-tubulin and acted as a competitive inhibitor to oligomerization of Glu-tubulin, attenuating its formation in cells. This was associated with significantly decreased type I collagen deposition and decreased secretory activity as measured by synaptotagmin VII levels on the osteoblast plasma membrane. Our results suggest that Glu-tubulin may exist as covalently stabilized form which may be linked to the secretion and elaboration of collagenous extracellular matrix.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Microtubules (MTs) are dynamic cytoskeletal proteins that are essential for a number of cellular functions such as mitosis, motility and intracellular transport (Wloga and Gaertig 2010; Garnham and Roll-Mecak 2012). MTs are comprised of heterodimeric α-and β-tubulin units that polymerize and grow into molecular rods through a GTP-powered process. MT growth and shrinkage are highly dynamic and occurs rapidly by polymerization–depolymerization events. MTs are stabilized and blocked from depolymerization during various cellular functions including secretion and differentiation, and this occurs initially through posttranslational modifications that alter the ability of tubulin to bind other proteins (Garnham and Roll-Mecak 2012). Perhaps the best characterized and understood stabilizing modification is the enzymatic removal of the C-terminal tyrosine residue (detyrosination) on α-tubulin which creates a new C-terminal end having two glutamic acid residues (Liao and Gundersen 1998). This form is referred to as Glu-tubulin and is used as a marker for MT stability (Westermann and Weber 2003). Although detyrosination itself does not stabilize MTs, the process precedes further stabilization where Glu-tubulin has an improved ability to recruit stabilizing factors, such as MT-associated proteins (MAPs) and Tau, as well as cargo-carrying motor proteins such as kinesin-1 (Liao and Gundersen 1998; Peris et al. 2006, 2009). Both α-and β-tubulin undergo a number of other posttranslational modifications that create subpopulations of tubulins with different properties that appear to fine tune MT function in various cellular processes (Westermann and Weber 2003; Janke and Kneussel 2010; Janke and Bulinski 2011; Song et al. 2013). In addition to detyrosination/tyrosination, α-tubulin undergoes acetylation and polyglutamylation which also increases the ability of these modified MTs to recruit motor proteins (Maas et al. 2009). Polyglycylation of α-tubulin and β-tubulin has been linked to regulation of cell growth (Xia et al. 2000). β-tubulin can be also glycosylated, glutamylated, and phosphorylated at a serine and a tyrosine residue, of which the latter modification has been suggested to improve tubulin interaction with cellular membranes (Hargreaves et al. 1986; Audebert et al. 1993; Garnham and Roll-Mecak 2012). The different posttranslational modifications of tubulin are reversible and can occur in various combinations (Eddé et al. 1991; Janke and Kneussel 2010; Garnham and Roll-Mecak 2012).
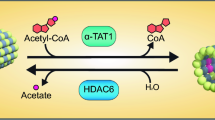
We and others have recently reported that tubulin can be also posttranslationally modified by transglutaminase (TG) enzymes and can form covalent high molecular weight (HMW) oligomers (Del Duca et al. 2009, 2013; Di Sandro et al. 2010; Al-Jallad et al. 2011; Song et al. 2013). TGs are a family of protein-crosslinking enzymes capable of creating an isopeptide bond between a glutamine (Q) residue and a lysine (K) residue or between a glutamine (Q) residue and primary amines such as putrescine, spermine, and spermidine (Williams-Ashman and Canellakis 1980; Lorand and Graham 2003; Iismaa et al. 2009). Formation of covalent isopeptide bonds between proteins leads to the formation of oligomers or polymers, whereas primary amine incorporation does not; however, both modifications have been shown to change the chemical properties of proteins as well as their biological functions (Truong et al. 2004; Lai et al. 2004; Lorand 2007). TG-crosslinking activity has been associated with stabilization of protein networks in the extracellular matrix and of intracellular protein systems because crosslinked protein complexes typically resist proteolytic degradation (Iismaa et al. 2009). The TG family contains currently 9 different enzymes—TG1-7, Factor XIIIA (FXIIIA) and band 4.2 (inactive enzyme). TG enzymes are expressed in a wide variety of tissues and in different cellular compartments, sometimes working in combinations of two or more (Nurminskaya and Kaartinen 2006; Al-Jallad et al. 2011), where they participate in a variety of cellular functions ranging from tissue stabilization to cell signaling (Lorand 2007; Iismaa et al. 2009; Park et al. 2010). Although many TG substrates are extracellular proteins (Kaartinen et al. 2002, 2005; Esposito and Caputo 2005; Beninati et al. 2009; Cui et al. 2014), they have been also shown to stabilize cytoskeletal and intermediate filament components such as actin, β-tubulin, myosin and vimentin (Maccioni and Seeds 1986; Safer et al. 1997; Nemes et al. 1997; Clément et al. 1998; Tseng et al. 2002; Esposito and Caputo 2005; Baumgartner and Weth 2007; Del Duca et al. 2009, 2013; Song et al. 2013). In recent studies, neuronal tubulin was shown to undergo TG-mediated polyamination, namely incorporation of putrescine, spermidine and spermine into its structure (Song et al. 2013); the modification was required for stabilization of MTs during neurite growth (Song et al. 2013). TG activity has also been reported to covalently modify actin and tubulin into HMW oligomers during pear pollen tube growth (Del Duca et al. 2009, 2013; Di Sandro et al. 2010). In our previous work, we demonstrated that bone-forming osteoblasts also form HMW, oligomeric Glu-tubulin upon expression of TG activity (Al-Jallad et al. 2011). This HMW form of Glu-tubulin was present specifically in membrane preparations of differentiating and secretory osteoblasts, and we suggested at that time that the Glu-tubulin oligomerization was linked to stabilization of MT tracks to the plasma membrane during secretion of type I collagen (COL I). In the present study, we have further examined the formation of oligomeric Glu-tubulin in osteoblasts in vitro. We report that the covalent crosslinking by TG creates plasma membrane-associated Glu-tubulin with increased stability. This form co-localizes with FXIIIA transglutaminase, and its presence correlates with secretory activity of osteoblasts.
Materials and methods
Peptides, proteins and antibodies
Biotinylated peptides (bF11: Biotin-DQMMLPWPAVAL, bF11QN: Biotin-DNMMLPWPAVAL) were synthesized by Biologica Co. (Nagoya, Japan) and by Biomatik Corp (Wilmington, DE, USA). Bovine tubulin protein (α/β-tubulin) was purchased from Cytoskeleton Inc. (Denver, CO, USA); pre-activated human FXIIIA enzyme was from Zedira (Darmstadt, Germany); and paclitaxel was from Cell Signaling (Danvers, MA, USA) and nocodazole was from Sigma (St. Louis, MO, USA). Mouse monoclonal anti-α-tubulin antibody and rabbit anti-synaptotagmin VII were from Sigma (St. Louis, MO, USA), and anti-Glu-tubulin (rabbit polyclonal antibody) was from Millipore (Temecula, CA, USA). Anti-dansyl antibody was purchased from Molecular Probes (Eugene, OR, USA). Polyclonal antibody against mouse FXIIIA was designed and generated by GenScript (Piscataway, NJ, USA) (Al-Jallad et al. 2011) Anti-biotin antibody (rabbit polyclonal) was from Rockland Immunochemicals (Gilbertsville PA, USA); anti-fibronectin from (Millipore, Temecula, CA, USA); and mouse mAb 6-11B-1 specific for acetylated tubulin and rabbit pan-cadherin antibody from Abcam (Cambridge, MA, USA). Horseradish peroxidase linked anti-rabbit IgG and anti-mouse IgG were from Cell Signaling (Whitby, ON, Canada) and GE Healthcare Life Sciences (Baie d’Urfe, QC, Canada), respectively. The AlexaFluor® secondary antibodies, DAPI, EZ-link sulfo-NHS-biotin and protein BCA assay kit were from Thermo Scientific (Waltham, MA, USA). All other reagents, if not specified below, were purchased from Sigma or Fisher Scientific.
Cell culture
Mouse calvarial pre-osteoblasts (MC3T3-E1) subclone 14 were (originally a generous gift from Dr. Renny T. Franceschi, University of Michigan, School of Dentistry, Ann Arbor, MI, USA) (Wang et al. 1999) were cultured in a humidified 37 °C incubator at 5 % CO2 in modified alpha minimum essential medium (α-MEM) minus l-glutamine and l-aspartic acid (Gibco, Burlington, ON, Canada), supplemented with 10 % fetal bovine serum (Hyclone), 1 % penicillin–streptomycin antibiotics, l-glutamine and l-aspartic acid. All treatments were initiated 24 h after adhesion (Day 0), and cells were plated at 50,000 cells per cm2 unless otherwise specified. Differentiation into mature osteoblasts was induced by supplementing the medium with 50 μg/ml ascorbic acid (AA), and mineralization was induced by adding 50 μg/ml AA plus 10 mM β-glycerophosphate (βGP) as described previously (Al-Jallad et al. 2006). This medium was referred to as differentiating medium (DM). Control cells were treated with medium only (referred to as M). Media were changed every second day, and TG activity was inhibited by using the irreversible inhibitor N-α-carbobenzyloxy-N-ε-acryloyl-l-lysine (2-(2-dansylaminoethoxy) ethoxy) ethanamide (NC9) (Keillor et al. 2008), which was used at 25 μM as before (Al-Jallad et al. 2011). The end point of all experiments was day 5. For immunofluorescence visualization of the bF11 and bF11QN inhibitors, a 1 μM concentration was used and peptides were administered to cells at day 4, and cells were fixed on day 5 for analysis. For inhibition of COL I deposition, bF11 was administered to cells at a 25–100 μM concentration from day 0 to day 6. The effect of bF11 and bF11QN peptides on cell viability was assessed by MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) tetrazolium assay (Sigma). Peptides were not toxic to cells at any concentration (Online Resource 2). Plasma fibronectin-depleted serum was prepared as described previously (Cui et al. 2014). Paclitaxel and nocodazole treatments (1–5 μM) were started on day 2 and continued for 48 h.
Transglutaminase-activity assays
TG-activity assays were performed according to our previously published method (Al-Jallad et al. 2006). Briefly, samples were incubated for 2 h at 37 °C with different concentrations of 5-(biotinamido) pentylamine (bPA) (Pierce/Thermo Scientific), 10 mM dithiothreitol (DTT) and 1 μg α/β-tubulin mix and pre-activated FXIIIA in a reaction buffer containing 3 mM CaCl2 in Tris-buffered saline (TBS) at pH 8.0. After incubation, samples were processed for SDS-PAGE and Western blotting as below.
Preparation of protein extracts, subcellular fractions and cell surface proteins
Total cellular protein preparations were obtained using RIPA buffer (150 mM NaCl, 10 mM Tris–HCl (pH 7.2), 5 mM EDTA, 0.1 % Sodium dodecyl sulfate (SDS), 1 % Triton X-100, 1 % Na-Deoxycholate). Cell extracts were homogenized by ultrasonication directly after extraction and centrifuged at 14,000×g for 15 min at 4 °C. The supernatant was collected and hereafter is referred to as total protein extract. Subcellular protein fractions where prepared using ProteoExtract® Subcellular Proteome Extraction Kit (S-PEK) from Calbiochem (Gibbstown, NJ, USA), following the manufacturer’s instructions. Cytoplasmic (Cy) plasma membranous (Me) preparations were used for this study. Proteins presented on the cell surface were isolated using EZ-link sulfo-NHS-biotin (Thermo Scientific). Protein concentrations of all preparations were determined with a bicinchoninic acid (BCA) protein assay kit (Thermo Scientific).
SDS-PAGE and Western blotting
Twenty-five (25) μg of each sample was boiled in Laemmli buffer for 5 min, followed by electrophoretic separation of proteins by SDS-PAGE. Following electrophoresis, gels were transferred to PVDF membranes (Bio-Rad) and blocked for 30 min in 5 % nonfat dry milk in TBS-Tween (TBS-T) and then incubated at 4 °C overnight in primary antibody diluted in TBS-T. Following incubation with primary antibody, membranes were rinsed in TBS-T and then incubated with secondary antibody conjugated with horseradish peroxidase at room temperature. Secondary antibodies used were sheep anti-mouse (Invitrogen) and goat anti-rabbit (Cell Signaling). Bands were visualized using the ECL Plus kit (GE Healthcare), and chemiluminescence was detected using Kodak Biomax film.
Immunofluorescence microscopy
Cells were seeded on Nunc® Lab-Tek®chamber slides (Fisher) and cultured as described above. On day 5, cells were fixed with 3.7 % formaldehyde in phosphate-buffered saline (PBS) for 10 min at room temperature. Slides were washed three times with PBS and blocked with 2 % bovine serum albumin (BSA) in PBS. This was followed by primary antibody incubation for 2 h at room temperature, and a washing step with 0.1 % BSA in PBS and incubation with AlexaFluor® secondary antibody conjugates. Nuclei were stained by DAPI (4′,6-diamidino-2-phenylindole). Samples were mounted with Prolong Gold Anti-Fade medium (Invitrogen) and dried overnight at room temperature. Cells were imaged using an Axioskop 2 upright fluorescence microscope equipped with an AxioCam MRm camera and AxioVision 4.8 imaging software from Zeiss. For supplemental experiments, some slides were permeabilized with a 10-min incubation of 0.25 % Triton-X100 in PBS, or fixed in methanol at −20 °C.
Total internal reflection fluorescence microscopy
MC3T3-E1 cells were plated and cultured (as above) on the FluoroDish™ plates (World Precision Instruments, Inc, Sarasota, FL, USA) coated with 1 μg/ml fibronectin (Sigma). On day 5, cells were fixed with 3.7 % formaldehyde in PBS for 10 min at room temperature. Immunofluorescence staining of the cells was done by following the same protocol as for conventional immunofluorescence microscopy (as above). After the final wash of DAPI staining, samples were covered with PBS and kept in the dark at 4 °C prior to analysis. Samples were observed and visualized with an incident angle of 68° using a Zeiss Axio Observer Z1 microscope in the multi-color TIRF illumination mode.
Collagen staining and quantification
Staining for COL I in vitro was performed by the Picrosirius method as described previously (Tullberg-Reinert and Hundt 1999). Briefly, cell layers were washed twice with PBS (137 mM NaCl, 2.7 mM KCl, 4.3 mM Na2HPO4, 1.47 mM KH2PO4, pH 7.4), and then fixed in Bouin’s Fluid (75 % saturated aqueous picric acid, 3.7 % formaldehyde, 5 % glacial acetic acid) for 1 h at room temperature on an orbital shaker. Following fixation, cell layers were washed for 15 min, then twice for 1 min, in distilled water. COL I was stained by incubating in Sirius Red staining solution (100 mg/ml Sirius Red (Sigma) in saturated aqueous picric acid) for 1 h at room temperature with gentle shaking. Unbound dye was removed by washing twice for 1 min with 0.01 M HCl. Stain was then dissolved in 0.1 N NaOH, diluted in PBS, and quantified by spectrophotometry at 562 nm in triplicates. Serial dilutions of COL I from calf skin was applied to 96-well plates, dried overnight, stained as described above, and used to generate standard curves.
Statistical analysis
Error bars represent standard error of the mean (SEM) from three separate samples or experiments. Statistical significance was determined by the Student’s t test.
Results
TG activity in osteoblasts creates a membrane-associated, 150 kDa Glu-tubulin with increased stability
To investigate TG-mediated oligomerization of tubulin, we first examined the formation of 150 kDa Glu-tubulin in differentiating MC3T3-E1 osteoblast cultures. As evident from Western blotting conducted after SDS-PAGE under reducing conditions, Glu-tubulin is detected in the cells in two forms, as a 50 kDa monomer and as a 150 kDa HMW form which was specifically found in the membrane preparations (Me) of osteoblasts (Fig. 1a). Inhibition of TG activity in osteoblasts using the irreversible TG inhibitor NC9 (Keillor et al. 2008; Al-Jallad et al. 2011), decreased levels of the 150 kDa Glu-tubulin showing that its formation is dependent on TG activity (Fig. 1a) similarly as we have shown before (Al-Jallad et al. 2011). This covalent modification did not occur in acetylated tubulin (Ac-tub), another posttranslationally stabilized form of α-tubulin (Garnham and Roll-Mecak 2012) which was found only in its monomeric 50 kDa form in osteoblasts (Fig. 1b). To examine whether 150 kDa Glu-tubulin responds to chemical modulators of MT dynamics, MC3T3-E1 osteoblasts were treated with different concentrations of nocodazole (destabilizer) or paclitaxel (stabilizer) during their differentiation. As seen in Fig. 1c, nocodazole treatment of the cells rapidly and dose dependently destabilized all of the 50 kDa Glu-tubulin. Nocodazole also affected levels of 150 kDa Glu-tubulin dose dependently; however, the oligomeric form was considerably more resistant to destabilization. Conversely, paclitaxel dose dependently increased formation of 50 kDa Glu-tubulin, but had no effect on the formation of 150 kDa Glu-tubulin, strongly indicating that there is an additional rate-limiting step in the formation of 150 kDa Glu-tubulin. To investigate whether the formation of 150 kDa Glu-tubulin might involve a plasma membrane TG activity, we detected the presence of the activity in the membrane fractions of non-differentiating and differentiating osteoblasts inhibited by NC9 which incorporates covalently and irreversibly into active TG enzymes and can be detected via its dansyl group. As seen in Fig. 1d, detection of the dansyl group of NC9 in cytoskeletal and membrane fractions of osteoblasts by Western blotting showed that the inhibitor was specifically in the membrane fraction of both non-differentiating (medium only treated, M) cells and differentiating (differentiation medium, DM) cells and bound to a 68 kDa enzyme. This molecular weight (MW) corresponds to the MW of cellular FXIIIA in the mouse osteoblast culture system (Al-Jallad et al. 2011). In summary, Glu-tubulin appears to undergo a specific TG-mediated stabilization step in osteoblasts that results in the formation of membrane-associated, oligomeric 150 kDa Glu-tubulin that has increased stability compared with 50 kDa Glu-tubulin.
TG activity on the osteoblast cell membrane creates a high molecular weight, membrane-associated, 150 kDa Glu-tubulin with increased resistance to destabilization. a Western blot analysis of Glu-tubulin (Glu-tub) in cytosolic (Cy) and membrane (Me) fractions of differentiating MC3T3-E1 osteoblasts (DM). Glu-tubulin is found in two forms, as a 50 kDa monomer in the cytosolic fraction and as a 150 kDa high molecular weight form in the membrane fraction. The TG inhibitor NC9 decreases the levels of 150 kDa Glu-tubulin. b Acetylated tubulin (Ac-tub) is not found as a high molecular weight form as analyzed by Western blotting—only the 50 kDa form is detected. c The 150 kDa Glu-tubulin has increased stability, since nocodazole treatment of differentiating osteoblasts causes a destabilization and disappearance of the 50 kDa Glu-tubulin, whereas the 150 kDa Glu-tubulin shows increased resistance to this destabilization. Paclitaxel, a microtubule stabilizer, causes a dose-dependent increase in the levels of 50 kDa Glu-tubulin, whereas the 150 kDa Glu-tubulin does not respond to paclitaxel treatment suggesting an additional mechanism for the formation of the 150 kDa Glu-tubulin. α-Tubulin was used as a loading control. d Western blot analysis of the dansyl group of NC9 (a TG inhibitor) shows its specific incorporation into the membrane fraction of osteoblasts indicating the presence of the enzyme on the plasma membrane. Pan-cadherin (Pan-cad) was used as loading control. NC9 labeled a TG enzyme with a MW of 68 kDa
α-Tubulin is a specific TG substrate and can be crosslinked into HMW forms of 100, 150 and 250 kDa (dimers, trimers and polymers) in vitro
As demonstrated, differentiating MC3T3-E1 osteoblasts have oligomeric Glu-tubulin whose formation is dependent on TG activity. We next examined if tubulin serves as a crosslinking substrate in vitro and investigated whether this modification is specific to α-tubulin, which is known to give rise to Glu-tubulin (β-tubulin has a different C-terminus and is not detyrosinated). This was tested by an established TG-substrate assay involving protein incubation with a TG enzyme and 5-(biotinamido) pentylamine (bPA) (Al-Jallad et al. 2006). In this reaction bPA replaces lysine residues in crosslink formation and incorporates into TG-reactive glutamine residues of a substrate protein in the presence of a TG enzyme (Iismaa et al. 2009). We have previously shown that osteoblasts express two TGs—TG2 and FXIIIA—the latter being the main crosslinking enzyme in osteoblasts (Al-Jallad et al. 2006, 2011; Piercy-Kotb et al. 2012; Cui et al. 2014); thus, FXIIIA was the chosen enzyme for this assay. Incubation of an α/β-tubulin mix with a pre-activated human FXIIIA and increasing amounts of bPA resulted in a dose-dependent, strong labeling as well as formation of covalent (SDS-resistant) oligomeric tubulin forms as analyzed by Western blotting and detection by biotin antibody for bPA label (Fig. 2a). α/β-Tubulin mix formed dimers, trimers, tetramers and pentamers all of which were also labeled with bPA, this being indicative of the existence of several TG-reactive Q residues (Fig. 2a). A negative control without α/β-tubulin was used to confirm that the biotin-labeled bands were from tubulin and do not result from bPA incorporation into FXIIIA enzyme. We further incubated the α/β-tubulin mix with FXIIIA or TG2 enzyme alone without bPA, and detected the samples with specific α-tubulin and β-tubulin antibodies to investigate whether the modification was specific to FXIIIA and crosslinking of α-tubulin. As evident from Fig. 2b, the modification was not specific to FXIIIA; the TG2 enzyme was capable of creating α-tubulin oligomers. Crosslinking of the α/β-tubulin mix with FXIIIA and detection with both α-tubulin and β-tubulin antibodies (Fig. 2c) showed strong and specific polymerization of the α-tubulin, while β-tubulin did not form any oligomers. Furthermore, the observation that the pure α/β-tubulin preparations contained also oligomerized α-tubulin, but no oligomers of β-tubulin (Fig. 2c), supported the finding and indicated that the α-tubulin is more prone to forming oligomers.
α-Tubulin, but not β-tubulin, is a TG substrate and can be crosslinked into high molecular weight forms of 100, 150 and 250 kDa (dimers, trimers and pentamers). a TG-substrate assay of α/β-tubulin mix was performed by using 5-(biotinamido) pentylamine (bPA) (increasing concentrations of 2, 4 and 8 mM) which incorporates into Q residues of TG substrates in the presence of TG enzyme(s). Western blot analysis using biotin antibody shows that bPA label incorporates into 50 kDa tubulin as well as into complexes of tubulin. Dimers, trimers and other-sized polymers are readily detected. b Tubulin can act as substrate for both TG2 and Factor XIIIA as demonstrated by the formation of high molecular weight forms of α-tubulin upon incubation with both enzymes. Western blot detection was done for α-tubulin. c α-Tubulin is a specific substrate for FXIIIA as demonstrated by the formation of high molecular weight complexes in the presence of the enzyme. β-Tubulin does not form complexes and is thus not a FXIIIA substrate
α-Tubulin and Glu-tubulin are found on the plasma membrane and co-localize with FXIIIA
The observation that 150 kDa Glu-tubulin specifically associated with membrane fractions in MC3T3-E1 osteoblast cultures suggests that it may be associated with the plasma membrane of the cells and possibly also found on the cell surface. Although it is well established that tubulin links to the inner leaflet of the plasma membrane via linker molecules [microtubule plus-end tracking proteins (TIPs)] such as EB1 (Ligon et al. 2003; Dixit et al. 2009), it has been suggested, although not yet fully established, that tubulin alone can associate with the plasma membrane and even penetrate the plasma membrane to extrude to the cell surface (Zisapel and Littauer 1979; Rubin et al. 1982; Quillen et al. 1985; Wolff 2009). It has been suggested that modifications such as phosphorylation may promote tubulin insertion into membranes (Hargreaves et al. 1986; Atashi et al. 1992). The concept that tubulin is on the outer leaflet of the osteoblast plasma membrane is central to the concept that it undergoes crosslinking by FXIIIA since FXIIIA is generally considered only to catalyze the crosslinking reaction within the high Ca2+ environment outside the cell, and because we have demonstrated in our previous work that FXIIIA (and TG2) are not active inside osteoblasts, but are found on the cell surface (Al-Jallad et al. 2011). Therefore, we examined whether α- and Glu-tubulin were associated with the osteoblast plasma membrane and whether they are found on the cell surface, and if they co-localize there with FXIIIA. To do this, we used Total Internal Reflection Fluorescence (TIRF) microscopy which is a specialized technique to study cell surface and plasma membrane-associated molecules (Axelrod 2001; Jaiswal and Simon 2007; Mattheyses et al. 2010; Simons and Gerl 2010). TIRF microscope only excites fluorophores in a restricted region of the specimen immediately adjacent to the bottom of the microscope slide upon which cells are examined using this method, which allows the study of molecules on the plasma membrane (Mattheyses et al. 2010). As seen in Fig. 3a, TIRF microscopy using a 68° angle and penetration depth of less than 80 nm into the plasma membrane shows clear α-tubulin staining where it appears close to the plasma membrane in ~5–7 μm patches. Analysis of α-tubulin, Glu-tubulin and FXIIIA with TIRF microscopy shows co-localization of both forms of tubulins with FXIIIA in these structures (Fig. 3b). We have previously published co-localization of FXIIIA and tubulin in similar structures using a conventional IF microscope where specimens were prepared by only fixing with formaldehyde (not permeabilized with Triton-X100) (Al-Jallad et al. 2011). In these experiments, we assigned the patchy staining pattern to tubulin at the periphery of the osteoblasts. Here the α-tubulin visualization with TIRF microscopy resembles these images obtained with conventional IF microscopy of cells fixed with only formaldehyde showing filamentous α-tubulin patches (Online Resource 1a). This suggests that the formaldehyde-fixation method may be also used to visualize tubulin at the cell periphery. As seen in Online Resource 1a-c, formaldehyde fixing blocks visualization of the intracellular tubulin network which can be seen only after Triton-X100 permeabilization or after methanol fixation at −20 °C. Conversely, the two methods do not show patchy tubulin staining suggesting that the detergent treatment interferes with detection of tubulin patches, possibly by abolishing critical lipid components from the cell membrane (Online Resource 1).
α- and Glu-tubulin are found on the plasma membrane and cell surface of osteoblasts where both co-localize with Factor XIIIA. a TIRF microscopy of α-tubulin (green, Alexa Fluor® 488) and DAPI (blue) (visualized in EPI mode) in formaldehyde-fixed and non-permeabilized osteoblasts on day 5. Analysis shows α-tubulin in 5–7 μm patches at the periphery of the cells. Visualization was done with an incident angle of 68° reaching to a depth of 80 nm. b TIRF microscopy co-localization (yellow) of FXIIIA (red, Alexa Fluor® 568) and α-tubulin and Glu-tubulin (green, Alexa Fluor® 488) in differentiating osteoblasts. c Both α- and Glu-tubulin are detected on the cell surface as determined by Western blotting of cell surface biotinylated protein extracts. A non-cell permeable biotinylation reagent was used for preparing and purifying the cell surface material. Differentiating osteoblasts (DM) have more high molecular weight Glu-tubulin on the cell surface compared with non-differentiated osteoblasts treated with medium only (M). Inhibition of TG activity with NC9 results in a decrease in the high molecular weight Glu-tubulin on the cell surface. β1-Integrin was used as the loading control for cell surface material (color figure online)
Since the plasma membrane is on average 7 nm thick, visualizing through a depth of 80 nm with TIRF microscopy is not a bone fide demonstration of the presence of a protein on the outer leaflet of the plasma membrane. Thus, we further examined the possibility of the Glu-tubulin being on the outer leaflet of the osteoblast membrane by cell surface biotinylation experiments. For this, cell surface-specific biotinylation and subsequent pull-down experiments were done using cell-impermeable sulfo-NHS-biotin. Western blotting of α- and Glu-tubulin from this cell surface biotinylated material showed clearly that both Glu-tubulin and α-tubulin are found on the surface of the osteoblast but that the presence of Glu-tubulin (both 50 and 150 kDa forms) on the cell surface is specific to the differentiated and COL I-depositing cells producing extracellular matrix (Fig. 3c). The presence of oligomeric Glu-tubulin on the cell surface is dependent on TG activity since inhibitor NC9 abolishes the 150 kDa Glu-tubulin while the 50 kDa form appears largely unaffected. This suggests that Glu-tubulin first localizes to the cell surface and is subsequently crosslinked upon co-localizing with FXIIIA. Immunodetection of cell surface β1-integrin was used as a positive control for Western blotting using the same biotinylated material (Fig. 3c). We conclude that Glu-tubulin (α-tubulin) can be found on the outer leaflet of the plasma membrane (on the cell surface) where it appears to acts as a substrate for FXIIIA.
The specific FXIIIA substrate peptide bF11 co-localizes with α-tubulin in osteoblasts and attenuates α-tubulin crosslinking in vitro
To further confirm that the α-tubulin (and thus Glu-tubulin) is crosslinked by FXIIIA in osteoblast cultures, we used the FXIIIA-specific substrate peptide bF11 to examine whether it co-localizes with α-tubulin. This isozyme-specific Q-donor substrate probe was developed from a phage-display random peptide library (Sugimura et al. 2006; Watanabe et al. 2013) and it specifically incorporates into substrates of FXIIIA. The peptide bears a biotin label in the N-terminus for antibody detection. Immunofluorescence staining of non-permeabilized osteoblasts and their analysis by conventional IF microscopy shows co-localization of the bF11 peptide with α-tubulin in rounded patches (Fig. 4a). Use of control bF11QN peptide where a Q residue has been changed to an N residue (which eliminates its reactivity to FXIIIA) showed no staining. TIRF microscopy confirmed the co-localization of bF11 and α-tubulin on the osteoblast plasma membrane (Fig. 4b). We next tested the ability of the bF11 peptide to covalently integrate into α-tubulin using an in vitro TG-activity assay. In this assay, bF11 incorporated into α-tubulin as did bPA. It also acted as a competitive inhibitor to decrease the oligomerization of α-tubulin in vitro when applied at a high concentration (100 μM) (Fig. 4c, last lane). bPA-labeled α-tubulin is detected at 50 and 150 kDa. The 75 kDa band here arises from labeling of the pre-activated human FXIIIA added in the mixtures. The results demonstrate that α-tubulin has both TG-reactive Q residues and TG-reactive K residues that are capable of covalently reacting and incorporating bPA and bF11, respectively.
The Factor XIIIA-specific substrate peptide bF11 co-localizes with α-tubulin and inhibits α-tubulin crosslinking in vitro. a Immunofluorescence microscopy of bF11 incorporation into osteoblast cell cultures and co-localization with α-tubulin. bF11 was detected with anti-biotin antibody (red, Alexa Fluor® 568) co-localized (yellow) with α-tubulin (green, Alexa Fluor® 488). bF11QN control peptide does not incorporate into osteoblast cultures and no signal is detected. b TIRF microscopy co-localization (yellow) of bF11 (biotin) (red, Alexa Fluor® 568) with α-tubulin and Glu-tubulin (green, Alexa Fluor® 488) in differentiating osteoblasts (DM) on day 5 in formaldehyde-fixed, non-permeabilized cells. c Western blot analysis of bF11 peptide incorporation into α-tubulin in the presence of FXIIIA (last lane). bF11 incorporates into α-tubulin in a manner similar to 5-(biotinamido) pentylamine (bPA), but is more efficient in blocking the formation of high molecular weight complexes of α-tubulin. The 75 kDa band arises from bPA-labeled FXIIIA. Since bF11 incorporates into the K residues of TG substrates and bPA into the Q residues, these results show that α-tubulin can provide both K and Q residues for crosslinking (color figure online)
bF11 peptide inhibits Glu-tubulin crosslinking and COL I deposition in osteoblast cultures
We have previously linked FXIIIA activity in osteoblast cultures to COL I extracellular matrix deposition via mechanisms that involve (1) promotion of COL I-containing secretory vesicle trafficking to the plasma membrane via microtubule tracks and Glu-tubulin crosslinking to stabilize the secretory process (Al-Jallad et al. 2011), and (2) the stabilization of a fibronectin matrix scaffold for COL I deposition into the extracellular space (Cui et al. 2014). To examine if the bF11 peptide was able to also block COL I secretion and deposition, we used bF11 in osteoblast cultures at a high dose where it would be expected to act as a competitive inhibitor and attenuate the formation of oligomeric 150 kDa Glu-tubulin. Firstly, as seen in Fig. 5a, 100 μM bF11 decreased the formation of 150 kDa Glu-tubulin similarly as NC9 as evident from Western blots of cytosolic and membrane fractions of differentiating osteoblasts. Examination of the effect of bF11 on COL I matrix accumulation in osteoblast cultures showed that it inhibited the process in a concentration-dependent manner when the inhibitory peptide was applied to the cell cultures for 6 days (25–100 μM concentrations were tested). Quantification of Picrosirius Red staining (which stains extracellular fibrillar COL I) in the cultures showed significant (−39 and −63 %) decreases in COL I levels at 50 and 100 μM bF11 concentration, respectively (Fig. 5b). An unexplained slight but significant increase in COL I deposition was observed when using bF11 at the 25 μM concentration and bF11QN at the 100 μM concentration. bF11 treatments did not affect cell viability (Online Resource 2).
The Factor XIIIA-specific substrate peptide bF11 attenuates levels of the 150 kDa Glu-tubulin in osteoblasts and inhibits COL I extracellular matrix accumulation. a Western blot analysis of 150 kDa Glu-tubulin cytosolic (Cy) and membrane (Me) fractions of differentiating osteoblasts upon bF11 treatment. NC9 treatment was used here as a positive control to demonstrate successful inhibition. bF11 (100 μM) treatment results in a decrease in 150 kDa HMW Glu-tubulin levels in membrane fractions similar to that seen after treatment with NC9. b COL I deposition in osteoblast cultures upon bF11 treatment (25–100 μM). COL I levels were quantified by Picrosirius red staining. The COL I levels of non-differentiating (and thus non-COL I depositing) osteoblasts was subtracted as background (0 %). COL I levels in differentiating osteoblasts (DM) were set at 100 %. bF11 treatment results in a dose-dependent and significant decrease in COL I deposition at concentrations of 50 and 100 μM (−39 and −63 %, respectively). A slight, but significant increase in COL I deposition is observed at 25 μM of bF11 (+7 %) and at 100 μM of bF11QN (+11 %). Data are presented as mean values ± SEM. **p ≤ 0.01; ***p ≤ 0.001. Student’s t test relative to control (DM). c Western blot analysis of synaptotagmin VII (Syt VII) levels in cytosolic (Cy) and membrane (Me) fractions of differentiating osteoblasts upon bF11 treatment. Differentiating treatment (DM) results in an appearance of Syt VII in the membrane fraction as an indicator of successful exocytosis of proteins related to osteoblast differentiation and the elaboration of a collagenous extracellular matrix. bF11 treatment decreases Syt VII levels in the membrane fraction by 29 %, suggesting that the secretory process was impaired. Pan-cadherin was used as the loading control
To examine whether the secretory process was defective in bF11-treated cells, we analyzed synaptotagmin VII (Syt VII) levels in the membrane fractions. It has been shown that Syt VII becomes part of the cell membrane during successful exocytose making Syt VII detectable at the cell surface of secretory cells (Chapman 2002). As seen also in Fig. 5c, Syt VII levels were decreased (−29 %) in membrane fractions of bF11-treated cells, supporting the notion that secretory vesicle transport to the cell membrane is impaired following this inhibition. Of importance here is also the observation that Syt VII is found on the plasma membrane of osteoblasts only in differentiating (COL I-synthesizing) osteoblasts. Non-differentiating medium-treated osteoblasts retained Syt VII in the cytosolic compartment (Fig. 5c).
As outlined above, we have shown before that inhibition of FXIIIA with bF11 in osteoblast cultures interferes with plasma FN (pFN) assembly (Cui et al. 2014) as also seen in Online Resource 2a. Thus, as a control experiment, we examined whether the lack of a pFN network affects oligomerization of Glu-tubulin. This was done by culturing osteoblasts in pFN-depleted serum. As seen in Online Resource 2b, pFN depletion from serum did not affect the formation of oligomeric 150 kDa Glu-tubulin. This demonstrates that Glu-tubulin crosslinking and pFN matrix stabilization are two separate functions of FXIIIA. In summary, formation of 150 kDa Glu-tubulin is associated with FXIIIA activity on the cell surface and COL I secretion in osteoblasts.
Discussion
Both α-and β-tubulin undergo a number of posttranslational modifications which influence MT function and dynamics in many cell types. In this study, we describe details of a FXIIIA-mediated covalent oligomerization of Glu-tubulin in osteoblasts. We report that this oligomerization, which creates a 150 kDa Glu-tubulin form, is specific to α- and Glu-tubulin. This HMW Glu-tubulin appears associated with the plasma membrane and found on the outer leaflet of osteoblast cells where it co-localizes with FXIIIA. Oligomerization appears to create a more stable form of Glu-tubulin whose function is likely linked to highly specialized COL I trafficking in osteoblasts to produce an extracellular matrix. While our studies are the first to link HMW Glu-tubulin formation to COL I secretion, the role of detyrosination and the formation of Glu-tubulin has been linked to the secretory process in other studies. It has been speculated that Glu-tubulin binds kinesin motor protein(s) with high affinity during cell polarization, differentiation and secretory vesicle trafficking (Liao and Gundersen 1998). It has also been shown that Glu-tubulin slows down the velocity of the kinesin protein while it moves along MT tracks. This change in velocity has been suggested to allow more ‘consistent delivery of cargo’ or ‘asymmetric’ secretion in the cell (Garnham and Roll-Mecak 2012). Indeed, COL I secretory activity in osteoblasts is consistent with such a concept. COL I is the most abundant protein in vertebrates and constitutes approximately 30 % of the weight of bone (Feng and McDonald 2011). Its biosynthesis is a highly complex process involving important extracellular processing steps where it is carefully assembled into long fibrils and then fibers (Kadler et al. 1996). In bone, osteoblasts are thus a cell type responsible for a high level of continuous, polarized secretory activity from the apical cell membrane that occurs over weeks while the cell resides at the bone tissue surface (Long 2012). Thus, an extra step to stabilize MT tracks radiating to the cell membrane involving covalent oligomerization of tubulin may be required to achieve this extensive and stable secretion.
In the present study, we describe that the oligomeric 150 kDa Glu-tubulin form is plasma membrane associated, since it is found only in membrane fractions as assessed by subcellular protein analysis. While the mechanism by which this oligomerization might promote Glu-tubulin association with the plasma membrane remains unknown, it is possible that the crosslinking results in complexation with another protein that is capable of penetrating the phospholipid layer. Another intriguing possibility is that oligomerization of Glu-tubulin changes tubulin solubility to lipids which may promote its association with membranes in a manner similar to that which has been described for phosphorylated β-tubulin and its association with vesicle lipid bilayers (Hargreaves et al. 1986). It is known that solubility changes are fairly common upon covalent crosslinking by TGs (Lai et al. 2004; Shin et al. 2008).
We also report that both 50 and 150 kDa Glu-tubulin/α-tubulin are found on the cell surface where we believe the covalent crosslinking and oligomerization occurs. While the presence of tubulin on the cell surface remains a concept that needs further evidence, it is not a completely novel idea. The existence of cell surface tubulin was first shown in 1976 with an approach involving labeling of the surface of pigeon erythrocytes (known to contain tubulin, unlike human erythrocytes) with colchicine/Sepharose beads which bind to β- and α-tubulin (Zenner and Pfeuffer 1976). The authors of this study concluded that since colchicine extends at most 11–12 Å into the membrane that it binds to material on the cell surface. Further evidence of the existence of cell surface tubulin comes from studies of malignant cells where it has been reported for neuroblastoma cells (Zisapel and Littauer 1979), for transformed lymphocytes (Bachvaroff et al. 1980) and for a lymphoblast line (Quillen et al. 1985). In addition to that occurring in lymphocytes, tubulin penetration to the outer leaflet of the plasma membrane has been shown via surface labeling of intact cells in a human cultured monocyte-like cell line, U937 (Por et al. 1991). In this study, the authors used an indirect staining procedure based on a biotinylated anti-mouse IgG antibody, and flow cytometry using antibodies to actin and tubulin which detected both these proteins on the cell surface in U937 cells. The role of cell surface tubulin is not known in any of the above cell types; however, the authors of these studies suggested that it may be linked with malignancy and leukemic transformation. Our work provides further evidence of the potential existence of cell surface tubulin in another, nonmalignant cell type (osteoblasts), and suggests that it may represent a form of tubulin that can be modified and further stabilized by TGs on the cell surface.
Evidence that tubulin is a substrate for TG in mammalian cells was first introduced in 1986 by Maccioni and Seeds using clonal mouse neuroblastoma N18 cells (Maccioni and Seeds 1986). The authors of this study suggested that this modification could mediate covalent crosslinking of microtubules to other cellular components. To date, most studies regarding tubulin suggest that TGs stabilize this MT protein, or regulate the interactions between tubulin and membrane-associated or cytoskeletal proteins, to facilitate biological events such as cell secretion, placental development, and axonal growth and maintenance (Robinson et al. 2007; Del Duca et al. 2009; Al-Jallad et al. 2011; Song et al. 2013). The latest report on neural cells has shown that tubulin can be polyaminated by TG2 in the intracellular space in a process that regulates axon growth (Song et al. 2013). TGs require a fairly high Ca2+-concentration for activation which induces a significant conformational change in the enzymes that expose their active site (Pinkas et al. 2007). This knowledge has been at the center of a debate on whether TGs can act as crosslinking enzymes in the intracellular compartment where Ca2+-concentration is relatively low. With regard to this, strong evidence exists showing that monoamination (serotonylation, histaminylation, dopaminylation of Q residues) (Vowinckel et al. 2012) and polyamination (incorporation of spermine, spermidine, putrescine into Q residues) occurs in the intracellular compartment (Seiler and Deckardt 1976; Cooper et al. 1997; Jeon et al. 2003; Song et al. 2013). It thus seems reasonable to consider that TGs may be activated inside the cell via Ca2+ oscillations or that binding of other small proteins to intracellular TGs could induce conformational change and activation. In our system, the active TG enzyme appears to be FXIIIA (Al-Jallad et al. 2006, 2011; Piercy-Kotb et al. 2012; Cui et al. 2014) which has not heretofore been reported to catalyze crosslinking reactions inside cells. Although FXIIIA is found inside osteoblasts, where it may have functions in cell signaling, its crosslinking activity is only found on the plasma membrane outer leaflet of the cells as well as in the extracellular matrix. Thus, for FXIIIA-mediated oligomerization of tubulin to occur, it would be required to be outside the cells. One intriguing possibility related to this discussion is that tubulin may be monoaminated and/or polyaminated by TG2 inside certain cells, and oligomerized by FXIIIA outside the cells, thus providing two modes of stabilization depending on the cell type and function of MTs related to the function of the respective cell.
In summary, in differentiating osteoblasts, Glu-tubulin can act as a substrate for FXIIIA transglutaminase which creates oligomeric Glu-tubulin with increased stability. This form of Glu-tubulin is membrane associated, where its presence is linked with COL I secretion and deposition during osteoblast differentiation and the associated elaboration of a collagenous extracellular matrix.
Abbreviations
- FXIIIA:
-
Factor XIIIA
- TG:
-
Transglutaminase
- MTs:
-
Microtubules
- bPA:
-
5-(Biotinamido) pentylamine
- COL I:
-
Collagen type I
- Syt VII:
-
Synaptotagmin VII
- pFN:
-
Plasma FN
- TIRF:
-
Total internal reflection fluorescence
References
Al-Jallad HF, Nakano Y, Chen JLY, McMillan E, Lefebvre C, Kaartinen MT (2006) Transglutaminase activity regulates osteoblast differentiation and matrix mineralization in MC3T3-E1 osteoblast cultures. Matrix Bio 25(3):135–148. doi:10.1016/j.matbio.2005.11.001
Al-Jallad HF, Myneni VD, Piercy-Kotb SA, Chabot N, Mulani A, Keillor JW, Kaartinen MT (2011) Plasma membrane factor XIIIA transglutaminase activity regulates osteoblast matrix secretion and deposition by affecting microtubule dynamics. PLoS ONE 6(1):e15893. doi:10.1371/journal.pone.0015893
Atashi JR, Klinz SG, Ingraham CA, Matten WT, Schachner M, Maness PF (1992) Neural cell adhesion molecules modulate tyrosine phosphorylation of tubulin in nerve growth cone membranes. Neuron 8(5):831–842. doi:10.1016/0896-6273(92)90197-L
Audebert S, Desbruyères E, Gruszczynski C, Koulakoff A, Gros F, Denoulet P, Eddé B (1993) Reversible polyglutamylation of alpha- and beta-tubulin and microtubule dynamics in mouse brain neurons. Mol Biol Cell 4(6):615–626. doi:10.1091/mbc.4.6.615
Axelrod D (2001) Total internal reflection fluorescence microscopy in cell biology. Traffic 2(11):764–774. doi:10.1034/j.1600-0854.2001.21104.x
Bachvaroff RJ, Miller F, Rapaport FT (1980) Appearance of cytoskeletal components on the surface of leukemia cells and of lymphocytes transformed by mitogens and epstein-barr virus. Proc Natl Acad Sci U S A 77(8):4979–4983
Baumgartner W, Weth A (2007) Transglutaminase 1 stabilizes β-actin in endothelial cells correlating with a stabilization of intercellular junctions. J Vasc Res 44(3):234–240
Beninati S, Bergamini C, Piacentini M (2009) An overview of the first 50 years of transglutaminase research. Amino Acids 36(4):591–598. doi:10.1007/s00726-008-0211-x
Chapman ER (2002) Synaptotagmin: a Ca2+ sensor that triggers exocytosis? Nat Rev Mol Cell Biol 3(7):498–508
Clément S, Velasco PT, Murthy SNP, Wilson JH, Lukas TJ, Goldman RD, Lorand L (1998) The intermediate filament protein, vimentin, in the lens is a target for cross-linking by transglutaminase. J Biol Chem 273(13):7604–7609. doi:10.1074/jbc.273.13.7604
Cooper AJL, Sheu K-FR, Burke JR, Onodera O, Strittmatter WJ, Roses AD, Blass JP (1997) Polyglutamine domains are substrates of tissue transglutaminase: does transglutaminase play a role in expanded CAG/poly-Q neurodegenerative diseases? J Neurochem 69(1):431–434. doi:10.1046/j.1471-4159.1997.69010431.x
Cui C, Wang S, Myneni VD, Hitomi K, Kaartinen MT (2014) Transglutaminase activity arising from Factor XIIIA is required for stabilization and conversion of plasma fibronectin into matrix in osteoblast cultures. Bone 59:127–138. doi:10.1016/j.bone.2013.11.006
Del Duca S, Serafini-Fracassini D, Bonner P, Cresti M, Cai G (2009) Effects of post-translational modifications catalysed by pollen transglutaminase on the functional properties of microtubules and actin filaments. Biochem J 418(3):651–664. doi:10.1042/bj20081781
Del Duca S, Faleri C, Iorio RA, Cresti M, Serafini-Fracassini D, Cai G (2013) Distribution of transglutaminase in pear pollen tubes in relation to cytoskeleton and membrane dynamics. Plant Physiol 161(4):1706–1721
Di Sandro A, Del Duca S, Verderio E, Hargreaves AJ, Scarpellini A, Cai G, Cresti M, Faleri C, Iorio RA, Hirose S, Furutani Y, Coutts IGC, Griffin M, Bonner PLR, Serafini-Fracassini D (2010) An extracellular transglutaminase is required for apple pollen tube growth. Biocheml J 429(2):261–271. doi:10.1042/bj20100291
Dixit R, Barnett B, Lazarus JE, Tokito M, Goldman YE, Holzbaur ELF (2009) Microtubule plus-end tracking by CLIP-170 requires EB1. Proc Natl Acad Sci U S A 106(2):492–497. doi:10.1073/pnas.0807614106
Eddé B, Rossier J, Caer J-PL, Berwald-Netter Y, Koulakoff A, Gros F, Denoulet P (1991) A combination of posttranslational modifications is responsible for the production of neuronal α-tubulin heterogeneity. J Cell Biol 46(2):134–142. doi:10.1002/jcb.240460207
Esposito C, Caputo I (2005) Mammalian transglutaminases. FEBS J 272(3):615–631. doi:10.1111/j.1742-4658.2004.04476.x
Feng X, McDonald JM (2011) Disorders of bone remodeling. Annu Rev Pathol 6(1):121–145. doi:10.1146/annurev-pathol-011110-130203
Garnham CP, Roll-Mecak A (2012) The chemical complexity of cellular microtubules: tubulin post-translational modification enzymes and their roles in tuning microtubule functions. Cytoskeleton 69(7):442–463. doi:10.1002/cm.21027
Hargreaves AJ, Wandosell F, Avila J (1986) Phosphorylation of tubulin enhances its interaction with membranes. Nature 323(6091):827–828
Iismaa SE, Mearns BM, Lorand L, Graham RM (2009) Transglutaminases and disease: lessons from genetically engineered mouse models and inherited disorders. Physiol Rev 89(3):991–1023. doi:10.1152/physrev.00044.2008
Jaiswal JK, Simon SM (2007) Imaging single events at the cell membrane. Nat Chem Biol 3(2):92–98
Janke C, Bulinski JC (2011) Post-translational regulation of the microtubule cytoskeleton: mechanisms and functions. Nat Rev Mol Cell Biol 12(12):773–786
Janke C, Kneussel M (2010) Tubulin post-translational modifications: encoding functions on the neuronal microtubule cytoskeleton. Trends Neurosci 33(8):362–372
Jeon J-H, Choi K-H, Cho S-Y, Kim C-W, Shin D-M, Kwon J-C, Song K-Y, Park S-C, Kim I-G (2003) Transglutaminase 2 inhibits Rb binding of human papillomavirus E7 by incorporating polyamine. EMBO J 22(19):5273–5282. doi:10.1093/emboj/cdg495
Kaartinen MT, El-Maadawy S, Räsänen NH, McKee MD (2002) Tissue transglutaminase and its substrates in bone. J Bone Miner Res 17(12):2161–2173. doi:10.1359/jbmr.2002.17.12.2161
Kaartinen MT, Sun W, Kaipatur N, McKee MD (2005) Transglutaminase crosslinking of SIBLING proteins in teeth. J Dent Res 84(7):607–612. doi:10.1177/154405910508400705
Kadler KE, Holems DF, Trotter JA, Chapman JA (1996) Collagen fibril formation. J Biochem 316(Pt 1):1–11
Keillor JW, Chica RA, Chabot N, Vinci V, Pardin C, Fortin E, Gillet SMFG, Nakano Y, Kaartinen MT, Pelletier JN, Lubell WD (2008) The bioorganic chemistry of transglutaminase—from mechanism to inhibition and engineering. Can J Chem 86(4):271–276. doi:10.1139/v08-024
Lai TS, Tucker T, Burke JR, Strittmatter WJ, Greenberg CS (2004) Effect of tissue transglutaminase on the solubility of proteins containing expanded polyglutamine repeats. J Neurochem 88(5):1253–1260. doi:10.1046/j.1471-4159.2003.02249.x
Liao G, Gundersen GG (1998) Kinesin is a candidate for cross-bridging microtubules and intermediate filaments: selective binding of kinesin to detyrosinated tubulin and vimentin. J BiolChem 273(16):9797–9803. doi:10.1074/jbc.273.16.9797
Ligon LA, Shelly SS, Tokito M, Holzbaur ELF (2003) The microtubule plus-end proteins EB1 and dynactin have differential effects on microtubule polymerization. Mol Biol Cell 14(4):1405–1417. doi:10.1091/mbc.E02-03-0155
Long F (2012) Building strong bones: molecular regulation of the osteoblast lineage. Nat Rev Mol Cell Biol 13(1):27–38
Lorand L (2007) Crosslinks in blood: transglutaminase and beyond. FASEB J 21(8):1627–1632. doi:10.1091/mbc.E02-03-0155
Lorand L, Graham RM (2003) Transglutaminases: crosslinking enzymes with pleiotropic functions. Nat Rev Mol Cell Biol 4(2):140–156
Maas C, Belgardt D, Lee HK, Heisler FF, Lappe-Siefke C, Magiera MM, van Dijk J, Hausrat TJ, Janke C, Kneussel M (2009) Synaptic activation modifies microtubules underlying transport of postsynaptic cargo. Proc Natl Acad Sci U S A 106(21):8731–8736
Maccioni R, Seeds N (1986) Transglutaminase and neuronal differentiation. Mol Cell Biochem 69(2):161–168. doi:10.1007/BF00224763
Mattheyses AL, Simon SM, Rappoport JZ (2010) Imaging with total internal reflection fluorescence microscopy for the cell biologist. J Cell Sci 123(21):3621–3628. doi:10.1242/jcs.056218
Nemes Z, AdányR Balázs M, Boross P, Fésüs L (1997) Identification of cytoplasmic actin as an abundant glutaminyl substrate for tissue transglutaminase in HL-60 and U937 cells undergoing apoptosis. J Biol Chem 272(33):20577–20583. doi:10.1074/jbc.272.33.20577
Nurminskaya M, Kaartinen MT (2006) Transglutaminases in mineralized tissues. Front Biosci 11:1591–1606. doi:10.2741/1907
Park D, Choi S, Ha K-S (2010) Transglutaminase 2: a multi-functional protein in multiple subcellular compartments. Amino Acids 39(3):619–631. doi:10.1007/s00726-010-0500-z
Peris L, Thery M, Fauré J, Saoudi Y, Lafanechère L, Chilton JK, Gordon-Weeks P, Galjart N, Bornens M, Wordeman L, Wehland J, Andrieux A, Job D (2006) Tubulin tyrosination is a major factor affecting the recruitment of CAP-Gly proteins at microtubule plus ends. J Cell Biol 174(6):839–849. doi:10.1083/jcb.200512058
Peris L, Wagenbach M, Lafanechère L, Brocard J, Moore AT, Kozielski F, Job D, Wordeman L, Andrieux A (2009) Motor-dependent microtubule disassembly driven by tubulin tyrosination. J Cell Biol 185(7):1159–1166. doi:10.1083/jcb.200902142
Piercy-Kotb SA, Mousa A, Al-Jallad HF, Myneni VD, Chicatun F, Nazhat SN, Kaartinen MT (2012) Factor XIIIA transglutaminase expression and secretion by osteoblasts is regulated by extracellular matrix collagen and the MAP kinase signaling pathway. J Cell Physiol 227(7):2936–2946. doi:10.1002/jcp.23040
Pinkas DM, Strop P, Brunger AT, Khosla C (2007) Transglutaminase 2 undergoes a large conformational change upon activation. PLoS Biol 5(12):e327. doi:10.1371/journal.pbio.0050327
Por SB, Cooley MA, Breit SN, Penny R, French PW (1991) Antibodies to tubulin and actin bind to the surface of a human monocytic cell line, U937. J Histochem Cytochem 39(7):981–985. doi:10.1177/39.7.1865114
Quillen M, Castello C, Krishan A, Rubin RW (1985) Cell surface tubulin in leukemic cells: molecular structure, surface binding, turnover, cell cycle expression, and origin. J Cell Biol 101(6):2345–2354. doi:10.1083/jcb.101.6.2345
Robinson NJ, Baker PN, Jones CJP, Aplin JD (2007) A role for tissue transglutaminase in stabilization of membrane-cytoskeletal particles shed from the human placenta. Biol Reprod 77(4):648–657. doi:10.1095/biolreprod.107.061747
Rubin RW, Quillen M, Corcoran JJ, Ganapathi R, Krishan A (1982) Tubulin as a major cell surface protein in human lymphoid cells of leukemic origin. Cancer Res 42(4):1384–1389
Safer D, Sosnick TR, Elzinga M (1997) Thymosin β4 binds actin in an extended conformation and contacts both the barbed and pointed ends. Biochemistry 36(19):5806–5816. doi:10.1021/bi970185v
Seiler N, Deckardt K (1976) Association of putrescine, spermidine, spermine, and GABA with structural elements of brain cells. Neurochem Res 1(5):469–499. doi:10.1007/BF00964210
Shin D-M, Jeon J-H, Kim C-W, Cho S-Y, Lee H-J, Jang G-Y, Jeong EM, Lee D-S, Kang J-H, Melino G, Park S-C, Kim I-G (2008) TGFβ mediates activation of transglutaminase 2 in response to oxidative stress that leads to protein aggregation. FASEB J 22(7):2498–2507. doi:10.1096/fj.07-095455
Simons K, Gerl MJ (2010) Revitalizing membrane rafts: new tools and insights. Nat Rev Mol Cell Biol 11(10):688–699
Song Y, Kirkpatrick LL, Schilling AB, Helseth DL, Chabot N, Keillor JW, Johnson GV, Brady ST (2013) Transglutaminase and polyamination of tubulin: posttranslational modification for stabilizing axonal microtubules. Neuron 78(1):109–123
Sugimura Y, Hosono M, Wada F, Yoshimura T, Maki M, Hitomi K (2006) Screening for the preferred substrate sequence of transglutaminase using a phage-displayed peptide library: identification of peptide substrates for TGase 2 and factor XIIIA. J Biol Chem 281(26):17699–17706. doi:10.1074/jbc.M513538200
Truong V-D, Clare DA, Catignani GL, Swaisgood HE (2004) Cross-linking and rheological changes of whey proteins treated with microbial transglutaminase. J Agric Food Chem 52(5):1170–1176. doi:10.1021/jf034397c
Tseng T-F, Chen M-T, Liu D-C (2002) Purification of transglutaminase and its effects on myosin heavy chain and actin of spent hens. Meat Sci 60(3):267–270. doi:10.1016/S0309-1740(01)00132-2
Tullberg-Reinert H, Jundt G (1999) In situ measurement of collagen synthesis by human bone cells with a Sirius Red-based colorimetric microassay: effects of transforming growth factor β2 and ascorbic acid 2-phosphate. Histochemistry 112 (4):271–276. doi:10.1007/s004180050447
Vowinckel J, Stahlberg S, Paulmann N, Bluemlein K, Grohmann M, Ralser M, Walther DJ (2012) Histaminylation of glutamine residues is a novel posttranslational modification implicated in G-protein signaling. FEBS Lett 586(21):3819–3824. doi:10.1016/j.febslet.2012.09.027
Wang D, Christensen K, Chawla K, Xiao G, Krebsbach PH, Franceschi RT (1999) Isolation and characterization of MC3T3-E1 preosteoblast subclones with distinct in vitro and in vivo differentiation/mineralization potential. J Bone Miner Res 14(6):893–903. doi:10.1359/jbmr.1999.14.6.893
Watanabe K, Tsunoda K, Itoh M, Fukui M, Mori H, Hitomi K (2013) Transglutaminase 2 and factor XIII catalyze distinct substrates in differentiating osteoblastic cell line: utility of highly reactive substrate peptides. Amino Acids 44(1):209–214. doi:10.1007/s00726-011-1131-8
Westermann S, Weber K (2003) Post-translational modifications regulate microtubule function. Nat Rev Mol Cell Biol 4(12):938–948
Williams-Ashman HG, Canellakis ZN (1980) Transglutaminase-mediated covalent attachment of polyamines to proteins: mechanisms and potential physiological significance. Physiol Chem Phys 12(5):457–472
Wloga D, Gaertig J (2010) Post-translational modifications of microtubules. J Cell Sci 123(20):3447–3455. doi:10.1242/jcs.063727
Wolff J (2009) Plasma membrane tubulin. Biochim Biophys Acta 1788(7):1415–1433. doi:10.1016/j.bbamem.2009.03.013
Xia L, Hai B, Gao Y, Burnette D, Thazhath R, Duan J, Bré M-H, Levilliers N, Gorovsky MA, Gaertig J (2000) Polyglycylation of tubulin is essential and affects cell motility and division in tetrahymena thermophila. J Cell Biol 149(5):1097–1106. doi:10.1083/jcb.149.5.1097
Zenner HP, Pfeuffer T (1976) Microtubular proteins in pigeon erythrocyte membranes. Eur J Biochem 71(1):177–184. doi:10.1111/j.1432-1033.1976.tb11104.x
Zisapel N, Littauer UZ (1979) Expression of external-surface membrane proteins in differentiated and undifferentiated mouse neuroblastoma cells. Eur J Biochem 95(1):51–59. doi:10.1111/j.1432-1033.1979.tb12938.x
Acknowledgments
We would like to thank Mrs. Aisha Mousa for assistance in all phases of this study and Dr. Erika Wee of the Advanced BioImaging Facility (ABIF) of McGill University’s Life Science Complex for excellent assistance in using TIRF microscopy. This study was supported by grants to MTK from the Canadian Institutes of Health Research (CIHR) (MOP-119403), the CIHR Institute for Musculoskeletal Health and Arthritis (IMHA) (IMH-89827). KH was supported by a Grant-in-Aid for Scientific Research (B) (No. 23380200) from JSPS, Japan (KH). SW received studentship stipends from the China Scholarship Council (CSC) and Faculty of Dentistry, McGill University. CC received a studentship stipend from China the Scholarship Council (CSC).
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard
The manuscript does not contain clinical studies or patient data.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, S., Cui, C., Hitomi, K. et al. Detyrosinated Glu-tubulin is a substrate for cellular Factor XIIIA transglutaminase in differentiating osteoblasts. Amino Acids 46, 1513–1526 (2014). https://doi.org/10.1007/s00726-014-1719-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00726-014-1719-x