Abstract
Ghrelin is a 28-residue peptide acylated with an n-octanoyl group on the Ser 3 residue, predominantly produced by the stomach. Ghrelin displays strong growth hormone (GH) releasing activity, which is mediated by the activation of the so-called GH secretagogue receptor type 1a (GHS-R1a). Given the wide spectrum of biological activities of Ghrelin in neuroendocrine and metabolic pathways, many research groups, including our group, developed synthetic peptide, and nonpeptide GHS-R1a ligands, acting as agonists, partial agonists, antagonists, or inverse agonists. In this highlight article, we will focus on the discovery of a GHS-R1a antagonist compound, JMV 2959, which has been extensively studied in different in vitro and in vivo models. We will first describe the peptidomimetic approach that led us to discover this compound. Then we will review the results obtained with this compound in different studies in the fields of food intake and obesity, addictive behaviors, hyperactivity and retinopathy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ghrelin is a 28-residue peptide acylated with an n-octanoyl group on the Ser 3 residue and is predominantly produced by the stomach (Kojima et al. 1999) (Fig. 1).
Ghrelin displays strong growth hormone (GH)-releasing activity, which is mediated by the activation of the so-called GH secretagogue receptor type 1a (GHS-R1a) (Howard et al. 1996). GHS-R1a is concentrated in the hypothalamus–pituitary unit, but is also distributed in other central and peripheral tissues (Howard et al. 1996; Guan et al. 1997; Yokote et al. 1998; Gnanapavan et al. 2002; Dass et al. 2003). Indeed, apart from stimulating GH secretion, ghrelin exhibits hypothalamic activities that result in the stimulation of prolactin (PRL) and adrenocorticotropic hormone (ACTH) secretion (Arvat et al. 2001; Broglio et al. 2003). It effects a negative feedback on the pituitary–gonadal axis (Furuta et al. 2001; Fernandez-Fernandez et al. 2004), stimulates appetite and a positive energy balance (Tschop et al. 2000; Wren et al. 2000; Inui 2001; Nakazato et al. 2001; Tschop et al. 2001; Akamizu et al. 2004), influences sleep and behavior (Asakawa et al. 2001a, b; Carlini et al. 2002, 2004; Tolle et al. 2002; Weikel et al. 2003), controls gastric motility and acid secretion (Masuda et al. 2000; Asakawa et al. 2001a, b; Fujino et al. 2003; Peeters 2003; Inui et al. 2004), modulates pancreatic exocrine and endocrine function, and affects glucose levels (Broglio et al. 2001, 2003; Adeghate and Ponery 2002; Date et al. 2002; Murata et al. 2002; Ukkola 2003; Salehi et al. 2004). Ghrelin has an influence on the cardiovascular system (Nagaya et al. 2001; Enomoto et al. 2003; Nagaya and Kangawa 2003) and has been shown to modulate the proliferation of tumor cells (Jeffery et al. 2002; Duxbury et al. 2003; Volante et al. 2003; Cassoni et al. 2004).
Given this wide spectrum of biological activities, it is evident that the discovery of ghrelin and its receptor has opened up many avenues for neuroendocrine and metabolic research. Furthermore, many research groups, including our group, developed synthetic peptide, and nonpeptide GHS-R1a ligands, acting as agonists, partial agonists, antagonists, or inverse agonists (Moulin et al. 2007b).
In this highlight article, we will focus on the discovery of a GHS-R1a antagonist compound, JMV 2959, which has been extensively studied in different in vitro and in vivo models.
We will first describe the process that led us to discover this compound, thanks to a peptidomimetic approach. Then we will review the results obtained with this compound in different studies in the fields of food intake and obesity, addictive behaviors, hyperactivity and retinopathy.
Development of JMV 2959: from peptide to peptidomimetics
First lead: EP 51389
The story started in our laboratory in collaboration with the Europeptides Company.
Starting from GHRP-6, the first synthetic growth hormone secretagogue active in vitro and in vivo discovered by Bowers in 1984 (Bowers et al. 1984), scientists from Mediolanum Farmaceutici synthesized an analog compound, named Hexarelin (Deghenghi et al. 1994), which differs with GHRP-6 by the introduction of (D)-2-methyltryptophan in place of (D)-tryptophan, which confers a better stability and a reduced toxicity to the molecule, compared to GHRP-6.
Starting from this result, Europeptides worked at the reduction of Hexarelin size to obtain compounds with a better oral bioavailability. Their studies led to the discovery of tripeptide EP 51389 (Deghenghi 1999). Collaboration started between Europeptides and our laboratory, with the aim to design an original family of growth hormone secretagogues derived from EP 51389 (Fig. 2).
From peptide to pseudo-peptide: JMV 1843 (ARD-07, AEZS-130)
Compound EP 51389 was modified at its C-terminal part: a gem-diamino tryptophane residue was incorporated, the amine function was then formylated to give compound JMV 1843 (Guerlavais et al. 2003) (Fig. 3).
The idea of introducing this modification was inspired by results obtained in our laboratory concerning studies on Bombesin analogs (Azay et al. unpublished results). Bombesin is a 14-residue peptide hormone from the large family of neuropeptides of the gastro-intestinal tract. Indeed, structure–activity relationship studies showed that the C-terminal nonapeptide of Bombesin was sufficient to have the total biological activities of the hormone. The importance of specific residues as well as the importance of C-terminal dipeptide was also observed according to a general strategy that we developed for gastrin (Rodriguez et al. 1987): the most potent Bombesin antagonists were obtained by modifying this C-terminal dipeptide. In our laboratory, among all the modifications introduced in the C-terminal dipeptide of bombesin, the substitution of the amide function of the C-terminal by a formylated amine function led to a potent bombesin receptor agonist. Interestingly, this compound showed remarkable in vivo activity. This modification was applied to compound EP 51389 to give compound JMV 1843.
From pseudo-peptide to peptidomimetics: JMV 2215
It was then discovered that the C-terminal part moiety was not necessary for binding to the receptor. Suppression of this part of the molecule was suggested from Novo-Nordisk studies (Peschke et al. 2000) concerning NN 703 derivatives, displaying a very strong in vitro activity on growth hormone release (Fig. 4).
Indeed, the corresponding compound, named JMV 2215, displays a GHSR-1a binding affinity similar to that of compound JMV 1843. Moreover, this compound does not induce any growth hormone secretion in rat per subcutaneous route.
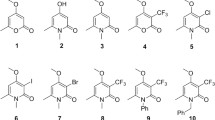
Compound JMV 2215 was chosen as a lead compound because of the simplicity of its structure. As ghrelin and its implication in food intake stimulation were discovered at that time, the interest for the discovery of receptor antagonists prompted us to adopt a classical medicinal chemistry approach. (Hruby and Balse 2000) As peptidic structures present several disadvantages such as limited stability toward proteolysis, poor transport properties and inherent flexibility, we decided to rigidify the structure by introducing various heterocycles bearing the needed side chain groups for receptor binding (Fig. 5, unpublished results).
These original heterocyclic structures were supposed to present a better selectivity and stability compared to their peptidic counterparts. Among all these molecules, several presented interesting binding affinities toward the ghrelin receptor, and particularly those belonging to the triazole family.
First triazole antagonist: JMV 2760
We started to work on the triazole family by the end of 2004, in collaboration with Æterna-Zentaris GmbH, with the following aims:
-
To find new ghrelin receptor ligands displaying a binding affinity lower than 10 nM.
-
To look for ghrelin receptor antagonists to develop a compound able to be tested in feeding behavior.
-
To synthesize molecules having a molecular weight in the 500–600 g/mol range.
-
The synthetic scheme leading to these compounds has to be easy to handle and modular.
We chose to work on the 1,2,4-triazole moiety, for the following reasons:
-
Interesting results were preliminary obtained with this family in our laboratory.
-
The 1,2,4-triazole moiety presents a strategic interest because no patent claimed this scaffold as ghrelin receptor ligand.
-
This scaffold is well known in medicinal chemistry for various biological properties: antifungal (Collin et al. 2003), antimicrobial (Papakonstantinou-Garoufalias et al. 2002), antiviral (De Clercq 2004), antiasthmatic (Naito et al. 1996) and hypotonic activities (Hester et al. 1971). 1,2,4-triazoles are also used as amide bond isostere for the design of peptide ligands with the aim of enhancing their pharmacological properties (Boyd et al. 1994; Thompson et al. 1994), or to mimic the cis configuration of the amide bond, which is present in some peptides (Hitotsuyanagi et al. 2002) (Fig. 6).
The 1,2,4-triazole moiety presents 3 potential points of diversity in positions 3, 4 and 5. An aminoalkyl group in position 5 will allow a fourth point of diversity. When the amino-alkyl is branched, the molecule displays an asymmetric center. The presence of these sites of diversity is essential when a structure–activity relationship study is considered (Fig. 7).
Once chosen the general scaffold, we then had to choose the first lead compound. For this purpose, we carefully examined the results previously obtained in our laboratory with the triazole family.
Starting from compound JMV 2215, a first target was compound JMV 2683, in which amide bond was replaced by the triazole scaffold (Fig. 8).
The synthetic scheme started from a primary thioamide, which was anticipated to cyclize as described by Hitotsuyanagi et al. (2002). Unfortunately, the primary thioamide spontaneously degraded into nitrile (Avalos et al. 1997) in the presence of mercury (II) acetate (Scheme 1).
It was then considered to protect the primary amide by an o,p-dimethoxybenzyl group, cleavable in acidic media (Scheme 2).
Both the amino-protected and unprotected compounds were tested to determine their binding affinity toward GHS-1a receptor. It was found that the N-protected triazole presented a better binding affinity for the GHR-R1a (i.e. compound JMV 2684 vs. JMV 2683, Fig. 9).
Several other triazole compounds were synthesized, and two of them retained our attention, compounds JMV 2570 and JMV 2604 (Fig. 10).
Indeed, by introducing an additional carbon atom between the triazole ring and the indole moiety, the binding affinity of the molecule was significantly improved.
By combining these two observations:
-
Trisubstituted triazole with o,p-dimethoxybenzyl group in position 4;
-
2 carbon atoms between the triazole scaffold and the indol moiety;
we considered synthesizing the corresponding compound, which was named JMV 2760 (Fig. 11).
Compound 2760 was tested (Demange et al. 2007) to determine its ability to inhibit 125I-[His9] ghrelin radioligand binding on hGHS-1a receptor transiently expressed on LLC-PK1 cells. The obtained inhibition curve indicated an inhibitory constant IC50 of 108 ± 17 nM. This binding affinity was far better from that obtained with JMV 2684 and JMV 2604 (IC50 783 and 580 nM, respectively) (Fig. 12).
The biological activity of compound JMV 2760 was then determined. For this purpose, the percentage of activation of intracellular calcium caused by the compound in saturating conditions (concentration of 10 μM) was measured. Compound JMV 2760 did not induce any intracellular calcium mobilization by itself. It was then tested at various concentrations on ghrelin-stimulated [Ca++]i mobilization. The dissociation constant of the receptor/JMV 2760 complex was determined by the Schild method (Fig. 13).
This experiment revealed a dissociation constant Kb of 14 ± 5 nM.
Compound JMV 2760 presented interesting binding affinity toward GHS-R1a, and behave as a ghrelin receptor antagonist on the [Ca++]i mobilization. This compound was the starting point of a structure–activity relationship study for searching ghrelin receptor antagonists.
Structure–activity relationship studies on the triazole series: discovery of compound JMV 2959 (AEZS-123)
Starting from this lead compound, extensive structure–activity relationship studies were performed (Demange et al. 2007; Moulin et al. 2007a, 2008a, b) (Fig. 14).
Variation of the R1 moiety was performed: the nature of the aromatic group and the carbon chain length was tested. For the R2 position, various groups, with diverse steric hindrance and substitutions, were tested. In R3 position, the nature of the aromatic group was modified, as well as the configuration of the carbon atom. We also studied the R4 part of the molecule: on the scheme below are displayed several carboxylic acids that were introduced. By this mean, more than 300 compounds were synthesized. The structure–activity relationship study allowed to rationalize, at least in part, the binding affinity of compounds toward the ghrelin receptor.
This study led to privilege a CH2–CH2–indole or a CH2–CH2–phenyl group in R1 position. In R2 position, a p-methoxy or o,p-dimethoxybenzyl group was preferred. It also clearly appeared that a (D)-tryptophan precursor was preferred at the R3 position. Concerning the R4 position, it appeared that to obtain an antagonist compound with high affinity, an aliphatic or aromatic nitrogen atom in position 2 relative to the amide carbonyl function was necessary.
One of these compounds JMV 2959 (Fig. 15) was chosen for further investigation.
In vitro characterization of compound JMV 2959
This compound was tested (Moulin et al. 2007a) to determine its ability to inhibit 125I-[His9] ghrelin radioligand binding on hGHS-1a receptor transiently expressed on LLC-PK1 cells (IC50 32 ± 3 nM).
Compound JMV 2959 did not induce any intracellular calcium mobilization by itself. The dissociation constant of the receptor/JMV 2959 complex was determined by the Schild method. This experiment revealed a dissociation constant Kb of 19 ± 6 nM (Figs. 16, 17).
The aqueous solubility of the hydrochloride salt of JMV 2959 was determined to be 5.0 mg/mL, and the clogP = 2.67.
First in vivo properties of compound JMV 2959
This compound was extensively studied in vivo by several research groups and for several different potential applications.
In vivo effects on food intake and fat accumulation
Ghrelin, first isolated from the stomach (Kojima et al. 1999), has emerged as an important gut-brain signal for the regulation of food intake (Wren et al. 2000; Nakazato et al. 2001) and fat mass (Tschop et al. 2000). Circulating ghrelin levels increase preprandially in healthy subjects (Cummings et al. 2001), and this finding is consistent with a role for ghrelin in food-seeking behavior and meal initiation.
Indeed, the central ghrelin signaling system receives considerable interest as a potential therapeutic target for the regulation of appetite and fat mass (Vincent and Le Roux 2007). A number of studies have shown that suppressed ghrelin signaling has beneficial effects to prevent/reverse obesity in animal studies (Asakawa et al. 2003; Esler et al. 2007).
Compound JMV 2959, as a ghrelin receptor antagonist, can be of great interest for this type of studies. Compound JMV 2959 was evaluated for in vivo effects on food intake and obesity (Moulin et al. 2007a). JMV 2959 was tested in feeding behavior in rats. It was first evaluated alone for its effect on food intake and compared to hexarelin, and then for its ability to inhibit hexarelin-stimulated food intake. As expected, when administered alone, JMV 2959 was without effect, it did not increase food intake. When inhibition of food intake induced by hexarelin was evaluated, JMV 2959 was found to totally suppress food intake induced by hexarelin administration [hexarelin (80 μg/kg, cumulative food intake (g of food/100 g of body weight) at 6 h by acute administration (sc) of compound JMV 2959 160 μg/kg)] (Fig. 18).
A dose–response study was performed for this compound. It showed a well-correlated progressive inhibition of hexarelin-stimulated cumulative food intake with increasing doses (20, 80, and 160 μg/kg). Almost total inhibition was observed at a dose of 160 μg/kg. Higher doses did not improve the inhibition (Fig. 19).
JMV 2959 was also evaluated for its activity on GH secretion in infant rats after sc administration, in the presence or not of hexarelin. Indeed, it is known that in the baby rats the pulsatility of the GH secretion is not yet activated at the hypothalamic level, and therefore, a constant GH blood level is measured in these young animals. As expected, when administered alone, JMV 2959 did not significantly stimulate GH release. Unexpectedly, it was unable to antagonize hexarelin-stimulated GH secretion.
No straightforward correlation could be drawn between in vitro results and in vivo experiments on GH secretion and food intake. JMV 2959 defined as an in vitro GHS-R1a antagonist had no effect on GH secretion or food intake in rats when administered alone. However, it was able to totally suppress hexarelin-induced food intake in rats, while it was unable to inhibit GH secretion elicited by hexarelin. All these findings strongly suggested the existence of either ghrelin receptor subtypes or a particular signalisation pathway of the ghrelin receptor correlated with GH secretion on one side and food intake on the other side. It is a possibility that different signaling pathways could be activated according to the interaction of the ghrelin receptor with another specific receptor present in the same tissue.
The first description of the central acute effects of JMV 2959 to suppress food intake induced by exogenous ghrelin administration and also by fasting-induced food intake was provided by Salomé et al. (2009).
Central (i.c.v.) injection of JMV 2959 to rats suppressed food intake induced by i.c.v. ghrelin injection (1 μg) in a dose-dependent manner with a total blockade at a 8 μg dose. JMV 2959 also reduced fasting-induced food intake in rats (i.e. the amount of food eaten during the first hour of food exposure after 16 h fast).
At the single cell level, the effects of JMV 2959 to suppress ghrelin (0.5 μM)-induced changes in electrical activity of arcuate nucleus cells recorded extracellularly in a slice preparation was also explored: preincubation with ghrelin followed by perfusion with JMV 2959 suppressed the responsiveness of arcuate cells to ghrelin.
Thus, JMV 2959 suppresses ghrelin-induced and fasting-induced food intake at the level of the central nervous system. This appeared to be mediated, at least in part, by a modulation of the activity of ghrelin-responsive arcuate nucleus cells.
In another study (Salome et al. 2009), the central nervous system mechanism underlying the chronic central effects of ghrelin, with respect to increasing body weight and body fat, was explored. JMV 2959 was used to investigate the role of GHS-R1a in mediating the effects of ghrelin on energy balance and on hypothalamic gene expression.
As expected, in adult male rats, chronic central treatment with ghrelin for 14 days, when compared to vehicle-treated control rats, resulted in an increased body weight, lean mass and fat mass (assessed by dual X-ray absorptiometry), dissected white fat pad weight, cumulative food intake, food efficiency, respiratory exchange ratio and a decrease of energy expenditure. Co-administration of JMV 2959 suppressed the majority of these effects, with the notable exception of ghrelin-induced food intake and food efficiency.
This effect of chronic JMV 2959 on food intake was difficult to interpret because, even though the antagonist appears to suppress ghrelin-induced food intake back to the same level as the control animals (ghrelin + JMV 2959 group vs. control), Salomé et al. could not detect a suppression of ghrelin-induced food intake by the antagonist (ghrelin + JMV 2959 vs. ghrelin). Similar results were obtained for the food efficiency. Thus, these data suggest that JMV 2959 did not completely block ghrelin’s effects of chronic central ghrelin administration on food intake, although the trends in the data would make it difficult to conclude that ghrelin-induced food intake is independent of GHS-R1a. Such effects could be explained by additional ghrelin receptor types (Yokote et al. 1998).
By contrast to the feeding data, the ghrelin-induced weight gain was totally blocked by JMV 2959. Both fat mass and lean mass were significantly increased by i.c.v. ghrelin treatment, but only the effect on fat mass was blocked by the antagonist. These data suggest that ghrelin is able to exert these beneficial effects on lean mass by a direct CNS action that does not only involve GHS-R1a (i.e. co-administration with JMV 2959 did not block these effects).
To further explore the dynamic changes in gene expression of hypothalamic peptide systems in rats chronically administered ghrelin (with/without JMV 2959), that have a positive energy balance, high throughput RT-PCR analysis of dissected hypothalamic tissue was performed, exploring a large number of candidate genes that may mediate the metabolic effects of ghrelin. It was found that central ghrelin infusion increased the gene expression of various hypothalamic peptides and their precursors (NPY, CART, prodynorphin, proenkephalin, prolactin-releasing hormone, orexin A and somatostatin), signaling molecules involved in GABA and glutamate signaling (e.g GAD1 and Vglut2) and UCP2 as well as various receptors (CRH-R1, CRH-R2, GHS-R1a, GLP-1R, insulin receptor, leptin receptor, and MC3R). Because ghrelin induces a positive energy balance and activates the hypothalamic-pituitary growth axis, it was impossible to distinguish between those changes that are a direct consequence of ghrelin action (and may be directly involved in ghrelin-induced changes in fat utilization) as opposed to those that are secondary to the adiposity or other endocrine changes (e.g. circulating adipokines).
Some of the hypothalamic gene expression which had increased after 2 weeks of ghrelin treatment also showed an increased expression even in rats in which the ghrelin was co-infused with JMV 2959 (and that did not have increased adiposity), namely the genes for CRH-R2, GAD1, GHS-R1a, GLP-1R, insulin receptor, NPY, orexin A, prodynorphin, prolactin-releasing hormone, Vglut2, somatostatin and UCP-2. These genes are regulated by chronic central ghrelin treatment, but this does not appear to involve signaling via GHS-R1a alone.
Co-administration of JMV 2959 was able to suppress some of the genes that were up-regulated by ghrelin. These included the genes for CART, MC3R and proenkephalin.
Although the effects of ghrelin on gene expression of the orexigenic peptide AgRP did not reach statistical significance, it was found a suppression of AgRP gene expression when ghrelin was co-administered with JMV 2959, consistent with the established literature that AgRP may be an important hypothalamic target for ghrelin (Kamegai et al. 2001; Tschop et al. 2002).
Regarding the reported effects of ghrelin that were not blocked by JMV 2959, including effects on hypothalamic gene expression, the authors suggested that these may be mediated by unknown ghrelin receptors (including receptor subtypes). They also pointed out the possibility that these effects were mediated by desacyl ghrelin, the unacylaed form of ghrelin that does not bind to GHS-R1a and has anorexigenic properties (Asakawa et al. 2005). The extent to which desacylation of exogenous ghrelin occurs in the brain remains to be determined, because the available evidence to date indicates that key circulating enzymes involved in desacylation do not gain access to the CNS (Duysen and Lockridge 2008). However, GHS-R1a interaction with other receptors expressed in the same tissues may also result in different intracellular pathways that could explain these behavioral differences.
In vivo effects on addictive behavior
A variety of human studies suggests that common neurobiological mechanisms underly different forms of addictive behaviors, including compulsive overeating, pathological gambling, alcoholism, nicotine dependence, and other forms of chemical addiction (Holderness et al. 1994; Volkow and Wise 2005). Given the hyperghrelinemia associated with certain forms of compulsive overeating (Cummings et al. 2002) and also with alcohol dependence (Kaur 2005; Kim et al. 2005), it was hypothesized that a common mechanism, involving the central ghrelin signaling system, underlies the pathophysiology of these diseases. Indeed, GHS-R1a antagonists such as JMV 2959 may have therapeutic potential in drug dependence disorders.
The first report concerning JMV 2959 and addictive behavior was performed by Jerlhag et al. (2009). They provide evidence that the central ghrelin signaling system is required for alcohol reward. Central ghrelin administration (to brain ventricles or to tegmental areas involved in reward) increased alcohol intake in a 2-bottle (alcohol/water) free choice limited access paradigm in mice. By contrast, central or peripheral administration of JMV 2959 suppressed alcohol intake in this model. Alcohol-induced locomotor stimulation, accumbal dopamine release and conditioned place preference were abolished in models of suppressed central ghrelin signaling: GHS-R1a KO mice and mice treated with JMV 2959.
As the target circuits for ghrelin in the brain include a mesolimbic reward pathway that is intimately associated with reward-seeking behavior, the same authors further sought to determine whether the central ghrelin signaling system is required for reward from drugs of abuse other than alcohol, namely cocaine or amphetamine (Jerlhag et al. 2010).
They found that amphetamine as well as cocaine-induced locomotor stimulation and accumbal dopamine release were reduced in mice treated with JMV 2959. Moreover, the ability of these drugs to condition a place preference was also attenuated by JMV 2959.
In another study (Clifford et al. 2011) it was examined the development of cocaine locomotor sensitization in rats, by pharmacologic antagonism by compound JMV 2959. During 7 consecutive days, adult male rats were injected per i.p. route with either 0.3 or 6.0 mg/kg JMV 2959, 20 min later, they were injected per i.p. route with either vehicle or 10 mg/kg cocaine HCl. Rats pretreated with JMV 2959 showed significantly attenuated cocaine-induced hyperlocomotion.
Collectively, these findings raised important questions regarding the physiological role of ghrelin influencing not only food intake and appetite, as described earlier, but also clearly having a broader role in reward induced by addictive drugs such as alcohol, amphetamine, and cocaine.
These results were enlarged by another study, where the effect of peripheral administration of JMV 2959 on the nicotine-induced locomotor stimulation, accumbal dopamine release and conditioned place preference was investigated (Jerlhag and Engel 2011).
It was found that the ability of nicotine to increase the locomotor activity, accumbal dopamine release and to condition place preference was reduced in mice treated with JMV 2959.
Thus GHS-R1a appeared to be required not only for alcohol, cocaine and amphetamine-induced reward, but also for reward induced by nicotine.
Paul Wellman research team also examined the role of ghrelin receptor in the behavioral sensitizing effects of nicotine (Wellman et al. 2011). For this purpose, adult male rats were injected with either 0.3 or 6.0 mg/kg of JMV 2959 per i.p. route and 20 min later with either vehicle or 0.4 mg/kg nicotine hydrogen tartrate per sc route, on each of 7 consecutive days.
It could be observed that rats treated with nicotine alone showed robust locomotor sensitization, as expected, whereas rats pretreated with JMV 2959 showed significantly attenuated nicotine-induced hyperlocomotion.
Skibicka et al. (2011) sought to determine whether ghrelin and its receptors are important for reinforcing motivation for natural sugar reward by examining the role of ghrelin receptor stimulation and blockade for sucrose progressive ratio operant conditioning, a procedure used to measure motivational drive to obtain a reward.
Peripherally and centrally administered ghrelin significantly increased operant responding and therefore, incentive motivation for sucrose. Utilizing JMV 2959, it was demonstrated that blockade of GHS-R1a signaling significantly decreased operant responding for sucrose. These findings suggested that ghrelin antagonists, such as JMV 2959, have therapeutic potential to suppress the overconsumption of sweet food.
These data were confirmed by Landgren et al. (Landgren et al. 2011). They present a rodent study where a group of alcohol-consuming individuals selected from a population cohort was investigated for genetic variants of the ghrelin signaling system in relation to both their alcohol and sucrose consumption. Moreover, the effect of JMV 2959 on voluntary sucrose intake and operant self administration, as well as saccharin intake was investigated. It was found associations with the ghrelin gene haplotypes and increased sucrose consumption, and a trend for the same association was seen in the high alcohol consumers. The preclinical data show that JMV 2959 reduces the intake and self-administration of sucrose in rats as well as saccharin intake in mice. Collectively, the data provided a clear indication that GHS-R1a such as JMV 2959 reduces the intake of rewarding substances.
Egecioglu et al. (2011) also showed that mice with a disrupted gene encoding the ghrelin receptor (GHS-R1a) and rats treated peripherally with JMV 2959 both show suppressed intake of rewarding food in a free choice (chow/rewarding food) paradigm. The ability of rewarding food to condition a place preference was suppressed by JMV 2959 in rats. These data supported the hypothesis that central ghrelin signaling at the level of the ventral tegmental area is important for the reward system. Indeed, the neurocircuity underpinning food-motivated behavior involves, in particular, the dopamine cells of the ventral tegmental area (VTA) that project to the nucleus accumbens (Nacc).
Skibicka et al. (2011) further sought to determine if ghrelin acts directly within these mesolimbic reward areas to increase food reward/motivation in studies that combine feeding behavior, pharmacology and neuroanatomy. It was found that motivated behavior for a sucrose reward, assessed in an operant conditioning paradigm in rats, was increased when ghrelin was microinjected directly into the VTA but not into the NAcc. By contrast, ghrelin administration to both areas increased the free feeding of chow. Importantly, in a state of overnight food restriction, where endogenous levels of ghrelin are increased, ghrelin receptor blockade by JMV 2959 in the VTA was sufficient to decrease the motivation to work for a sugar reward. Blockade of GHS-R1a in VTA or NAcc was not sufficient to reduce fasting-induced chow hyperphagia. Taken together these data identified the VTA but not the NAcc as a direct, necessary and sufficient, target site for ghrelin’s action on food motivation.
In vivo effects on hyperactivity
In patients suffering from anorexia nervosa, total plasma ghrelin concentrations of underweight subjects are increased and tend to normalize with the recovery of body weight (Otto et al. 2001). It has been reported by Misra et al. (2005) that high plasma levels of total ghrelin induced by fasting in humans are negatively associated with the percentage body fat and with low levels of leptin and insulin, which might play an important role in the pathophysiology of anorexia nervosa. Important characteristics of this disease include, in particular, increased locomotor activity and reduced food consumption (Routtenberg and Kuznesof 1967), together with similar endocrine abnormalities (de Rijke et al. 2005).
Studies in GHS-R1a KO mice have implicated the central ghrelin system in food anticipatory activity (Blum et al. 2009; LeSauter et al. 2009). Therefore, it was envisaged to use GHS-R1a antagonists, such as JMV 2959, to suppress anorexia-induced hyperlocomotor activity.
Verhagen et al. (2011) demonstrated that the central ghrelin signaling system, involving GHS-R1a, is required for food anticipation, measured in the ABA model (activity-based anorexia, an animal model of anorexia nervosa). Thus, food anticipatory activity was attenuated both in chronic models of suppressed ghrelin signaling (GHS-R1a KO mice and mice chronically treated with JMV 2959) and in an acute model (rats given an acute central injection of JMV 2959). Collectively these data suggest that the gut–brain signal provided by ghrelin is important for food anticipation and that GHS-R1a antagonists such as JMV 2959 provide a potential therapy for suppressing food anticipatory hyperlocomotor activity independently of food intake.
Anorectic patients often display abnormally high physical activity levels (Kron et al. 1978), which hinder the process of recovery (Kaye et al. 1988; Holtkamp et al. 2004). Thus, reducing hyperactivity in severely ill patients suffering from anorexia nervosa could be beneficial for therapeutic outcome.
In vivo effects on retinopathy
Vascular degeneration and the ensuing abnormal vascular proliferation are central to proliferative retinopathies, consisting of neovascularization of the retina extending into the vitreous body. Given the metabolic discordance associated with these diseases, Zaniolo et al. (2011) explored the role of ghrelin and GHS-R1a in proliferative retinopathy.
In a rat model of oxygen-induced retinopathy, the contribution of ghrelin and GHS-R1a was investigated using stable ghrelin agonists and antagonists, including JMV 2959.
This study allowed disclosing new role for the ghrelin-GHS-R1a pathway in the preservation of retinal vasculature during the vaso-obliterative phase of OIR and during the angiogenic phase of OIR. These findings suggest that the ghrelin-GHS-R1a pathway can exert opposing effects on retinal vasculature, depending on the phase of retinopathy, and thus holds therapeutic potential for proliferative retinopathies.
Perspectives
We described in this paper the process that led us to design ghrelin receptor antagonist JMV 2959. A first very interesting agonist compound, JMV 1843 (ARD-07) was published in 2003. In 2007, Scottish drugmaker Ardana has initiated a US registrational study of this compound, which is being developed as a treatment for growth hormone deficiency in adults. Earlier the same year, JMV 1843 was granted Orphan Drug status by the US Food and Drug Administration (http://www.thepharmaletter.com/file/46317/ardana-begins-us-study-of-ard-07-.html).
Further extensive structure–activity relationship studies led us to the discovery of a second very interesting compound, named JMV 2959 (AEZ-123), a ghrelin receptor antagonist, structure of which was published in 2007. As reviewed in the second part of this paper, this compound turned out to be an interesting pharmacological tool allowing researchers to better understand the way ghrelin and its receptor are involved in food intake and obesity, addictive behaviors, hyperactivity and retinopathy. This compound is also claimed in AeternaZentaris preclinical pipeline for the treatment of obesity and related pathologies (http://www.aeternazentaris.com/en/page.php?p=32&prod=28). We believe this compound will follow the same successful runway as compound JMV 1843, to rapidly reach clinical development.
References
Adeghate E, Ponery AS (2002) Ghrelin stimulates insulin secretion from the pancreas of normal and diabetic rats. J Neuroendocrinol 14(7):555–560
Akamizu T, Takaya K et al (2004) Pharmacokinetics, safety, and endocrine and appetite effects of ghrelin administration in young healthy subjects. Eur J Endocrinol 150(4):447–455
Arvat E, Maccario M et al (2001) Endocrine activities of ghrelin, a natural growth hormone secretagogue (GHS), in humans: comparison and interactions with hexarelin, a nonnatural peptidyl GHS, and GH-releasing hormone. J Clin Endocrinol Metab 86(3):1169–1174
Asakawa A, Inui A et al (2001a) A role of ghrelin in neuroendocrine and behavioral responses to stress in mice. Neuroendocrinology 74(3):143–147
Asakawa A, Inui A et al (2001b) Ghrelin is an appetite-stimulatory signal from stomach with structural resemblance to motilin. Gastroenterology 120(2):337–345
Asakawa A, Inui A et al (2003) Antagonism of ghrelin receptor reduces food intake and body weight gain in mice. Gut 52(7):947–952
Asakawa A, Inui A et al (2005) Stomach regulates energy balance via acylated ghrelin and desacyl ghrelin. Gut 54(1):18–24
Avalos M, Babiano R et al (1997) Reactions of thioamides with metal carboxylates in organic media. Tetrahedron 53(42):14463–14480
Blum ID, Patterson Z et al (2009) Reduced anticipatory locomotor responses to scheduled meals in ghrelin receptor deficient mice. Neuroscience 164(2):351–359
Bowers CY, Momany FA et al (1984) On the in vitro and in vivo activity of a new synthetic hexapeptide that acts on the pituitary to specifically release growth hormone. Endocrinology 114(5):1537–1545
Boyd SA, Fung AKL et al (1994) Nonpeptide renin inhibitors with good intraduodenal bioavailability and efficacy in dog. J Med Chem 37(19):2991–3007
Broglio F, Arvat E et al (2001) Ghrelin, a natural GH secretagogue produced by the stomach, induces hyperglycemia and reduces insulin secretion in humans. J Clin Endocrinol Metab 86(10):5083–5086
Broglio F, Benso A et al (2003a) The endocrine response to ghrelin as a function of gender in humans in young and elderly subjects. J Clin Endocrinol Metab 88(4):1537–1542
Broglio F, Gottero C et al (2003b) Ghrelin and the endocrine pancreas. Endocrine 22(1):19–24
Carlini VP, Monzon ME et al (2002) Ghrelin increases anxiety-like behavior and memory retention in rats. Biochem Biophys Res Commun 299(5):739–743
Carlini VP, Varas MM et al (2004) Differential role of the hippocampus, amygdala, and dorsal raphe nucleus in regulating feeding, memory, and anxiety-like behavioral responses to ghrelin. Biochem Biophys Res Commun 313(3):635–641
Cassoni P, Ghe C et al (2004) Expression of ghrelin and biological activity of specific receptors for ghrelin and des-acyl ghrelin in human prostate neoplasms and related cell lines. Eur J Endocrinol 150(2):173–184
Clifford PS, Rodriguez J, Schul D, Hughes S, Kniffin T, Hart N, Eitan S, Brunel L, Fehrentz J.-A, Martinez J, Wellman PJ (2011) Attenuation of cocaine induced locomotor sensitization in rats sustaining genetic or pharmacologic antagonism of ghrelin receptors. Addict Biol. doi:10.1111/j.1369.2011.00339.x
Collin X, Sauleau A et al (2003) 1,2,4-triazolo mercapto and aminonitriles as potent antifungal agents. Bioorg Med Chem Lett 13(15):2601–2605
Cummings DE, Clement K et al (2002) Elevated plasma ghrelin levels in Prader-Willi syndrome. Nat Med 8(7):643–644
Cummings DE, Purnell JQ et al (2001) A preprandial rise in plasma ghrelin levels suggests a role in meal initiation in humans. Diabetes 50(8):1714–1719
Dass NB, Munonyara M et al (2003) Growth hormone secretagogue receptors in rat and human gastrointestinal tract and the effects of ghrelin. Neuroscience 120(2):443–453
Date Y, Nakazato M et al (2002) Ghrelin is present in pancreatic α-cells of humans and rats and stimulates insulin secretion. Diabetes 51(1):124–129
De Clercq E (2004) Antiviral drugs in current clinical use. J Clin Virol 30(2):115–133
de Rijke CE, Hillebrand JJG et al (2005) Hypothalamic neuropeptide expression following chronic food restriction in sedentary and wheel-running rats. J Mol Endocrinol 35(2):381–390
Deghenghi R (1999) Impervious peptides as GH secretagogues. In: Ghigo E, Boghen M, Casanueva FF, Dieguez C (eds) Growth hormone secretagogues, 1st ed. Elsevier Science, Lausanne
Deghenghi R, Cananzi MM et al (1994) GH-releasing activity of hexarelin, a new growth hormone releasing peptide, in infant and adult rats. Life Sci 54(18):1321–1328
Demange L, Boeglin D et al (2007) Synthesis and pharmacological in vitro and in vivo evaluations of novel triazole derivatives as ligands of the ghrelin receptor 1. J Med Chem 50(8):1939–1957
Duxbury MS, Waseem T et al (2003) Ghrelin promotes pancreatic adenocarcinoma cellular proliferation and invasiveness. Biochem Biophys Res Commun 309(2):464–468
Duysen EG, Lockridge O (2008) Whole body and tissue imaging of the butyrylcholinesterase knockout mouse injected with near infrared dye labeled butyrylcholinesterase. Chem Biol Interact 175(1–3):119–124
Egecioglu E, Jerlhag E et al (2011) Ghrelin increases intake of rewarding food in rodents. Addict Biol 15(3):304–311
Enomoto M, Nagaya N et al (2003) Cardiovascular and hormonal effects of subcutaneous administration of ghrelin, a novel growth hormone-releasing peptide, in healthy humans. Clin Sci 105(4):431–435
Esler WP, Rudolph J et al (2007) Small-molecule ghrelin receptor antagonists improve glucose tolerance, suppress appetite, and promote weight loss. Endocrinology 148(11):5175–5185
Fernandez-Fernandez R, Tena-Sempere M et al (2004) Ghrelin effects on gonadotropin secretion in male and female rats. Neurosci Lett 362(2):103–107
Fujino K, Inui A et al (2003) Ghrelin induces fasted motor activity of the gastrointestinal tract in conscious fed rats. J Physiol 550(1):227–240
Furuta M, Funabashi T et al (2001) Intracerebroventricular administration of ghrelin rapidly suppresses pulsatile luteinizing hormone secretion in ovariectomized rats. Biochem Biophys Res Commun 288(4):780–785
Gnanapavan S, Kola B et al (2002) The tissue distribution of the mRNA of ghrelin and subtypes of its receptor GHS-R, in humans. J Clin Endocrinol Metab 87(6):2988–2991
Guan X-M, Yu H et al (1997) Distribution of mRNA encoding the growth hormone secretagogue receptor in brain and peripheral tissues. Mol Brain Res 48(1):23–29
Guerlavais V, Boeglin D et al (2003) New active series of growth hormone secretagogues. J Med Chem 46(7):1191–1203
Hester JB Jr, Rudzik AD et al (1971) 6-Phenyl-4H-s-triazolo[4,3-a][1,4]benzodiazepines which have central nervous system depressant activity. J Med Chem 14(11):1078–1081
Hitotsuyanagi Y, Motegi S et al (2002) A cis Amide Bond Surrogate Incorporating 1,2,4-Triazole. J Org Chem 67(10):3266–3271
Holderness CC, Brooks-Gunn J et al (1994) Co-morbidity of eating disorders and substance abuse review of the literature. Int J Eat Disord 16(1):1–34
Holtkamp K, Hebebrand J et al (2004) The contribution of anxiety and food restriction on physical activity levels in acute anorexia nervosa. Int J Eat Disord 36(2):163–171
Howard AD, Feighner SD et al (1996) A receptor in pituitary and hypothalamus that functions in growth hormone release. Science (Washington, DC) 273(5277):974–977
Hruby VJ, Balse PM (2000) Conformational and topographical considerations in designing agonist peptidomimetics from peptide leads. Curr Med Chem 7(9):945–970
Inui A (2001) Ghrelin: an orexigenic and somatotrophic signal from the stomach. Nat Rev Neurosci 2(8):551–560
Inui A, Asakawa A et al (2004) Ghrelin, appetite, and gastric motility: the emerging role of the stomach as an endocrine organ. FASEB J 18(3):439–456
Jeffery PL, Herington AC et al (2002) Expression and action of the growth hormone releasing peptide ghrelin and its receptor in prostate cancer cell lines. J Endocrinol 172(3):R7–R11
Jerlhag E, Egecioglu E et al (2010) Ghrelin receptor antagonism attenuates cocaine- and amphetamine-induced locomotor stimulation, accumbal dopamine release, and conditioned place preference. Psychopharmacology 211(4):415–422
Jerlhag E, Engel JA (2011) Ghrelin receptor antagonism attenuates nicotine-induced locomotor stimulation, accumbal dopamine release and conditioned place preference in mice. Drug Alcohol Depend 117(2–3):126–131
Jerlhag E, Egecioglu E et al (2009) Requirement of central ghrelin signaling for alcohol reward. Proc Natl Acad Sci USA 106(27):11318–11323
Kamegai J, Tamura H et al (2001) Chronic central infusion of ghrelin increases hypothalamic neuropeptide Y and agouti-related protein mRNA levels and body weight in rats. Diabetes 50(11):2438–2443
Kaur S, Ryabinin AE (2005) Ghrelin receptor antagonism decreases alcohol consumption and activation of perioculomotor urocortin-containing neurons. Alcohol Clin Exp Res 34(9):1525–1534
Kaye WH, Gwirtsman HE et al (1988) Relative importance of calorie intake needed to gain weight and level of physical activity in anorexia nervosa. Am J Clin Nutr 47(6):989–994
Kim D.-J., Yoon S.-J. et al (2005) Increased fasting plasma Ghrelin levels during alcohol abstinence. Alcohol Alcohol 40(1):76–79
Kojima M, Hosoda H et al (1999) Ghrelin is a growth-hormone-releasing acylated peptide from stomach. Nature 402(6762):656–660
Kron L, Katz JL et al (1978) Hyperactivity in anorexia nervosa: a fundamental clinical feature. Compr Psychiatry 19(5):433–440
Landgren S, Simms JA et al (2011) The ghrelin signalling system is involved in the consumption of sweets. PLoS One 6(3):e18170
LeSauter J, Hoque N et al (2009) Stomach ghrelin-secreting cells as food-entrainable circadian clocks. Proc Natl Acad Sci USA 106:13582–13587
Masuda Y, Tanaka T et al (2000) Ghrelin stimulates gastric acid secretion and motility in rats. Biochem Biophys Res Commun 276(3):905–908
Misra M, Miller KK et al (2005) Secretory dynamics of ghrelin in adolescent girls with anorexia nervosa and healthy adolescents. Am J Physiol 289(2):E347–E356
Moulin A, Demange L et al (2007a) Toward potent ghrelin receptor ligands based on trisubstituted 1,2,4-triazole structure. 2. synthesis and pharmacological in vitro and in vivo evaluations. J Med Chem 50(23):5790–5806
Moulin A, Ryan J et al (2007b) Recent developments in ghrelin receptor ligands. Chem Med Chem 2(9):1242–1259
Moulin A, Demange L et al (2008a) Trisubstituted 1,2,4-triazoles as ligands for the ghrelin receptor: on the significance of the orientation and substitution at position 3. Bioorg Med Chem Lett 18(1):164–168
Moulin A, Demange L et al (2008b) New trisubstituted 1,2,4-triazole derivatives as potent ghrelin receptor antagonists. Synthesis and pharmacological in vitro and in vivo evaluations. J Med Chem 51(3):689–693
Murata M, Okimura Y et al (2002) Ghrelin modulates the downstream molecules of insulin signaling in hepatoma cells. J Biol Chem 277(7):5667–5674
Nagaya N, Kangawa K (2003) Ghrelin, a novel growth hormone-releasing peptide, in the treatment of chronic heart failure. Regul Pept 114(2–3):71–77
Nagaya N, Miyatake K et al (2001) Hemodynamic, renal, and hormonal effects of ghrelin infusion in patients with chronic heart failure. J Clin Endocrinol Metab 86(12):5854–5859
Naito Y, Akahoshi F et al (1996) Synthesis and pharmacological activity of triazole derivatives inhibiting eosinophilia. J Med Chem 39(15):3019–3029
Nakazato M, Murakami N et al (2001) A role for ghrelin in the central regulation of feeding. Nature (London) 409(6817):194–198
Otto B, Cuntz U et al (2001) Weight gain decreases elevated plasma ghrelin concentrations of patients with anorexia nervosa. Eur J Endocrinol 145(5):R5–R9
Papakonstantinou-Garoufalias S, Pouli N et al (2002) Synthesis and antimicrobial and antifungal activity of some new 3-substituted derivatives of 4-(2,4-dichlorophenyl)-5-adamantyl-1H-1,2,4-triazole. Farmaco 57(12):973–977
Peeters TL (2003) Central and peripheral mechanisms by which ghrelin regulates gut motility. J Physiol Pharmacol Off J Pol Physiol Soc 54(Suppl 4):95–103
Peschke B, Ankersen M et al (2000) New highly potent dipeptidic growth hormone secretagogues with low molecular weight. Eur J Med Chem 35(6):599–618
Rodriguez M, Dubreuil P et al (1987) Synthesis and biological-activity of partially modified retro-inverso pseudopeptide derivatives of the C-terminal tetrapeptide of gastrin. J Med Chem 30(5):758–763
Routtenberg A, Kuznesof AW (1967) Self-starvation of rats living in activity wheels on a restricted feeding schedule. J Comp Physiol Psychol 64(3):414–421
Salehi A, Dornonville de la Cour C et al (2004) Effects of ghrelin on insulin and glucagon secretion: a study of isolated pancreatic islets and intact mice. Regul Pept 118(3):143–150
Salome N, Haage D et al (2009a) Anorexigenic and electrophysiological actions of novel ghrelin receptor (GHS-R1A) antagonists in rats. Eur J Pharmacol 612(1–3):167–173
Salome N, Hansson C et al (2009b) On the central mechanism underlying Ghrelin’s chronic pro-obesity effects in rats: new insights from studies exploiting a potent ghrelin receptor antagonist. J Neuroendocrinol 21(9):777–785
Skibicka KP, Hansson C et al (2011) Ghrelin directly targets the ventral tegmental area to increase food motivation. Neuroscience 180:129–137
Thompson SK, Eppley AM et al (1994) Synthesis and antiviral activity of a novel class of HIV-1 protease inhibitors containing a heterocyclic P1′–P2′ amide bond isostere. Bioorg Med Chem Lett 4(20):2441–2446
Tolle V, Bassant M-H et al (2002) Ultradian rhythmicity of ghrelin secretion in relation with GH, feeding behavior, and sleep-wake patterns in rats. Endocrinology 143(4):1353–1361
Tschop M, Smiley DL et al (2000) Ghrelin induces adiposity in rodents. Nature (London) 407(6806):908–913
Tschop M, Weyer C et al (2001) Circulating ghrelin levels are decreased in human obesity. Diabetes 50(4):707–709
Tschop M, Statnick MA et al (2002) GH-releasing peptide-2 increases fat mass in mice lacking NPY: indication for a crucial mediating role of hypothalamic agouti-related protein. Endocrinology 143(2):558–568
Ukkola O (2003) Ghrelin and insulin metabolism. Eur J Clin Invest 33(3):183–185
Verhagen LAW, Egecioglu E et al (2011) Acute and chronic suppression of the central ghrelin signaling system reveals a role in food anticipatory activity. Eur Neuropsychopharmacol 21(5):384–392
Vincent RP, Le Roux CW (2007) New agents in development for the management of obesity. Int J Clin Pract 61(12):2103–2112
Volante M, Allia E et al (2003) Ghrelin in fetal thyroid and follicular tumors and cell lines: expression and effects on tumor growth. Am J Pathol 162(2):645–654
Volkow ND, Wise RA (2005) How can drug addiction help us understand obesity? Nat Neurosci 8(5):555–560
Weikel JC, Wichniak A et al (2003) Ghrelin promotes slow-wave sleep in humans. Am J Physiol 284(2 Pt 1):E407–E415
Wellman PJ, Clifford PS et al (2011) Pharmacologic antagonism of ghrelin receptors attenuates development of nicotine induced locomotor sensitization in rats. Regul Pept 172(1–3):77–80
Wren AM, Small CJ et al (2000) The novel hypothalamic peptide ghrelin stimulates food intake and growth hormone secretion. Endocrinology 141(11):4325–4328
Yokote R, Sato M et al (1998) Molecular cloning and gene expression of growth hormone-releasing peptide receptor in rat tissues. Peptides (New York) 19(1):15–20
Zaniolo K, Sapieha P et al (2011) Ghrelin modulates physiologic and pathologic retinal angiogenesis through GHSR-1a. Invest Ophthalmol Vis Sci 52(8):5376–5386
Conflict of interest
The authors declare that they have no conflict of.interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Moulin, A., Brunel, L., Boeglin, D. et al. The 1,2,4-triazole as a scaffold for the design of ghrelin receptor ligands: development of JMV 2959, a potent antagonist. Amino Acids 44, 301–314 (2013). https://doi.org/10.1007/s00726-012-1355-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00726-012-1355-2