Abstract
microRNAs (miRNAs) are small noncoding RNAs that modulate gene expression at the posttranscriptional level, playing an important role in many diseases. However, reports concerning the role of miRNA in hepatitis B virus (HBV) infection are limited. miRNA chips were used to investigate miRNA changes during HBV infection in vitro. Bioinformatics analysis was used to explore possible miRNA and target genes during HBV infection. The expression of miR-125b and its potential target gene, sodium channel, non-voltage-gated 1 alpha (SCNN1A), was further analyzed. A total of 136 miRNAs were analyzed in an HBV transient transfection model (HepG2-HBV1.3), and 78 miRNAs were differentially expressed in HepG2.2.15 cells compared with HepG2 cells. miR-125b expression was decreased in both HepG2-HBV1.3 and HepG2.2.15 cells, and ectopic expression of miR-125b inhibited HBV DNA intermediates and secretion of HBsAg and HBeAg. miR-125b also inhibited the mRNA and protein levels of SCNN1A. Using a dual luciferase reporter system, we found that SCNN1A was one of the targets of miR-125b. In this study, we found that miR-125b inhibits HBV expression in vitro by regulating SCNN1A expression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatitis B virus (HBV) is a hepatotropic, non-cytopathic virus with a 3.2-kb partially double-stranded DNA genome that causes acute and chronic hepatitis in humans [1]. Although the proteins encoded by the HBV genome have been identified, the molecular mechanism by which chronic HBV infection causes liver damage and carcinogenesis remains elusive.
The control of viral replication is one of the major strategies to reduce the morbidity and mortality associated with chronic HBV infection. At present, immunomodulatory therapy using IFN-α and direct antiviral therapy using nucleoside or nucleotide analogs are the two major strategies for targeting the life cycle of hepatitis B, but these therapies are associated with low efficacy and drug resistance, respectively [2]. Recently, some medicinal plants were shown to have potential antiviral properties. Pei et al. found that pu-erh tea extracts have anti-HBV properties in the HepG2.2.15 cell line [3], and Liu et al. reported that Dioscin can decrease the secretion of HBsAg and HBeAg in HepG2.2.15 cells [4], shedding a new light on HBV treatment. Therefore, elucidation of the viral and host factors responsible for HBV infection, replication and dissemination will be useful for the future development of anti-HBV therapeutics.
MicroRNAs (miRNAs) are approximately 22-nucleotide-long non-coding RNAs that modulate gene expression at the posttranscriptional level by targeting mRNAs for degradation or by inhibiting translation [5]. miRNAs have been shown to play a prevalent role in cell proliferation, differentiation, cell death and carcinogenesis [6, 7]. Recent reports have indicated that host miRNAs are involved in HBV infection [8]. The expression of many miRNAs is dysregulated in HBV-infected cells or liver tissues, and some of these miRNAs are able to regulate HBV at the transcription level, either by targeting transcription factors required for HBV gene expression or by directly binding to HBV transcripts [9]. Has-miR-125a-5p was found to repress HBV surface antigen expression by acting on nt 3037-3065 of the HBV genome [10]. miR-122a, which was downregulated in an HBV-infected patient, repressed HBV expression by targeting the cyclin G1 and Wnt/beta-catenin pathways [11]. Another study also showed that miR-122a inhibited HBV replication and cell proliferation by targeting N-myc downstream-regulated gene (NDRG) [12]. In addition, Hu and colleagues found that miR-141 targeted peroxisome proliferator-activated receptor alpha (PPARA) to reduce HBV promoter activity, ultimately finally suppressed HBV replication [13]. On the other hand, some miRNAs appear to be involved in HBV-associated hepatocellular carcinoma. microRNA-152 (miR-152) is frequently downregulated in HBV-related HCC tissues and probably functions as a tumor repressor by decreasing global DNA methylation [14]. However, our understanding how the host profile is altered by HBV infection and the direct or indirect effect of cellular miRNA on HBV replication is limited. As an important host defense mechanism, it is important to achieve a global view of both miRNA and target gene expression profiles after HBV infection.
In this study, an miRNA microarray was used to investigate the miRNA expression pattern during HBV infection in vitro. miR-125b expression was decreased in both HepG2-HBV1.3 (a HepG2 cell line transiently transfected with an HBV expression plasmid) and HepG2.2.15 cells, and ectopic expression of miR-125b inhibited HBV DNA intermediates and secretion of HBsAg and HBeAg. Furthermore, miR-125b inhibited the mRNA and protein levels of SCNN1A. Using a dual luciferase assay, SCNN1A was shown to be one of the targets of miR-125b. We show that miR-125b inhibits HBV expression by targeting the SCNN1A gene, suggesting a potential role of miRNA in HBV infection.
Materials and methods
Plasmid construction
pCDNA3.1-SCNN1A was constructed by in-frame insertion of full-length SCNN1A into the pcDNA3.1.HBV expression vector pGEM-HBV1.3, which was obtained from Dr. Protzer (University of Heidelberg, Heidelberg, Germany).
Cell culture and transfection
HepG2 and HepG2.2.15 (stably HBV-transfected HepG2 cells) cells were maintained in modified Eagle’s medium (MEM) containing 10 % fetal calf serum. Transfection of pGEM-HBV1.3 into the HepG2 cells was carried out using Lipofectamine 2000 (Invitrogen). miR-125b mimics and its mutants were purchased from GenePharma (Shanghai). si-SCNN1A and control siRNA were purchased from Ambion (Silencer Select siRNAs).
miRNA microarrays
miRNA expression profiles were determined using mammalian miRNA arrays (miRCURYTM Array Microarray Kit, Exiqon 8.1) that were designed based on miRBase release 10.0 and contained 546 probes from humans, mice and rats. An miRNA was considered differentially expressed if its expression changed by more than twofold.
RNA extraction and quantitative RT-PCR
Total RNA was extracted from cultured cells using TRIzol Reagent (Invitrogen), and miR-125b expression was evaluated by quantitative real-time PCR (qPCR). Relative quantification was performed using SYBR Green assays for the target genes together with U6 mRNA as endogenous control. Expression values of target genes were calculated using the 2−∆∆Ct method. SCNN1A expression was determined by the same method, using PCR primers and GAPDH as an internal control.
Detection of HBsAg, HBeAg and HBV viral DNA
The levels of HBV surface antigen (HBsAg) and HBV envelope antigen (HBeAg) in culture medium and cell extracts were determined using an enzyme-linked immunosorbent assay (ELISA) following the manufacturer’s protocol (Kehua Biotech Inc., Shanghai, China). HBV viral DNA was detected using an HBV DNA PCR Fluorescence Quantitative Diagnostic Kit (Kehua Biotech Inc., Shanghai, China). Each experiment was performed in triplicate and independently repeated three times.
Southern blot analysis
HBV replicative intermediates were obtained as follows. Cells from one 35-mm-diameter dish were lysed with 0.5 ml of lysis buffer containing 10 mM Tris-HCl (pH 8.0), 1 mM EDTA, 1 % NP-40, and 2 % sucrose at 37 °C for 10 min. Cell debris and nuclei were removed by centrifugation, and the supernatant was mixed with 130 μl of 35 % polyethylene glycol (PEG) 8000 containing 1.5 M NaCl. After a 1-h incubation on ice, viral nucleocapsids were pelleted by centrifugation at 10,000g for 5 min at 4 °C, followed by a 1-h digestion at 37 °C in 400 μl of digestion buffer containing 0.5 mg pronase per ml (Calbiochem), 0.5 % sodium dodecyl sulfate (SDS), 150 mM NaCl, 25 mM Tris-HCl (pH 8.0), and 10 mM EDTA. The digestion mixture was extracted twice with phenol, and DNA was precipitated with ethanol, dissolved in TE buffer (10 mM Tris-HCl, pH 8.0, 1 mM EDTA) and separated on 0.8 % agarose gels. DNA samples were transferred to nylon membranes (Roche, Germany). After ultraviolet cross-linking and prehybridization, the membranes were hybridized with a DIG-labeled HBV-specific probe generated using a random-primed labeling kit (Roche,Germany). The signal was detected by exposing an X-ray film, which was scanned using a VersaDoc Imaging system (Bio-Rad).
Western blot analysis of HBc and SCNN1A expression
To monitor HBc expression, total proteins (30 μg) were separated by electrophoresis on a 15 % SDS polyacrylamide gel and transferred to polyvinylidenefluoride membranes (Millipore, Massachusetts, USA). The membranes were incubated with rabbit anti-core antibody (Dako Cytomation, Glostrup, Denmark) or mouse anti-GAPDH antibody (Jiamay, China). The immunoblot signals were detected using enhanced chemiluminescence reagent (Pierce, USA). To detect SCNN1A expression, 30 μg of total protein from HepG2.2.15 cells was separated using a 12 % SDS polyacrylamide gel and transferred onto polyvinylidene fluoride membranes. The membrane was incubated with rabbit anti-SCNN1A polyclonal antibody (Epitomics, USA). The secondary antibody for HBVcore protein and SCNN1NA was goat-anti rabbit HRP, and for GAPDH, it was rabbit anti-mouse HRP (Zhongshan Jinqiao, Beijing).
Luciferase assay
pGL3-SCNN1A was constructed by inserting the 3′UTR of SCNN1A downstream of pGL3-control using XbaI (Promega, USA). HEK293 cells were cotransfected with the plasmid and miR-125b or its mutant. At 36 h post transfection, cells were collected for luciferase activity using a Dual-Luciferase Reporter Assay System (Promega, USA).
Detection of cell viability
miRNA-125b and control RNA were introduced by transfection into both HepG2 and HepG2.2.15 cells, and 48 h posttransfection, an MTS assay (Promega, USA) was carried out according to the manufacturer’s instructions.
Statistical analysis
The raw miRNA expression data were quantile-normalized to correct for between-sample variations. An miRNA was considered differentially expressed if its expression change was more than 2.0-fold, and it was identified as significantly changed using the Significance Analysis of Microarrays method with FDR <0.05. Statistical analysis was done using one-way ANOVA for comparison of three groups, followed by LSD analysis for pairwise comparison, and differences with P < 0.05 were considered statistically significant.
Results
Effect of HBV replication on miRNA expression in HepG2 cells
The global miRNA expression profiles in HBV-transfected cells (HepG2-HBV1.3, HepG2 cells transfected with pGEM-HBV1.3) and HepG2.2.15 were compared with that of the parent HepG2 cell line using miRNA arrays. A total of 546 human mature miRNAs were analyzed in the arrays, of which 136 and 78 were differentially expressed in HepG2-HBV1.3 and HepG2.2.15 cells, respectively (Table 1, Supplementary Data 1, Supplementary Data 2). In HepG2-HBV1.3 cells, these included 114 upregulated and 22 downregulated miRNAs, and in HepG2.2.15 cells, 28 unregulated and 50 downregulated miRNAs were identified. Among these miRNAs, 35 showed similar differences in both HepG2-HBV1.3 and HepG2.2.15 cells, with 26 miRNA unregulated and nine downregulated (Table 1).
miR-125b is downregulated in HBV-infected HepG2 cells
We next examined miR-125b expression in both HepG2-HBV1.3 and HepG2.2.15 cells. Consistent with the microarray results, miR-125b was downregulated in both HepG2-HBV1.3 cells and HepG2.2.15 cells (Fig. 1). This result indicated that miR-125b might be involved in HBV infection.
Verification of miR-125b expression in HepG2-HBV and HepG2.2.15 cells. Total RNA was extracted from HepG2, HepG2-HBV and HepG2.2.15 cells. miRNA expression levels in HepG2 were set as 1. The relative miRNA expression level in HepG2-HBV and HepG2.2.15 was calculated. Asterisks indicate statistical differences between HepG2-HBV and HepG2.2.15 cells. The experiment was done in triplicate
miR-125b downregulates HBV expression in vitro
miR-125b has a negative regulatory effect on inflammation and tumor genesis. However, its role in HBV infection has not been reported. To examine first whether miR-125b could affect cell viability, an MTS assay was carried out using HepG2 and HepG2.215 cells. The results showed that ectopic expression of miR-125b had no significant effect on cell viability in either of these cell lines (Fig. 2a). To understand better the biological functions of miR-125b in HBV infection, exogenous miR-125b was introduced into HepG2.2.15 cells by transfection, and HBV viral DNA and HBV protein expression (including HBsAg, HBeAg, and HBc) were analyzed. Extopic expression of miR-125b inhibited HBV intermediates, as shown both real-time PCR and Southern blot analysis. miR-125b also inhibited HBV core protein expression as well as HBsAg and HBeAg secretion. The inhibitory effect of miR-125b on HBV replication was counteracted when an miR-125b inhibitor was introduced into HepG2.2.15 cells (Fig. 2b, c, and d). This indicates that miR-125b inhibits HBV expression in vitro.
miR-125b inhibits HBV expression in HepG2.2.15 cells. a) Effect of ectopic expression of miR-125b on cell viability. HepG2 and HepG2.2.15 cells were transfected with 50 pmol of miR-125b and control RNA. Forty-eight hours after transfection, an MTS assay was carried to determine cell viability. Cell viability in the control group was set as 1. b) miR-125b inhibits HBV intermediate expression. HepG2.2.15 cells were cotransfected with 30 pmol of miR-125b and 30 pmol of control RNA or inhibitor. HBV viral particles were extracted 72 h post-transfection and subjected to qPCR and Southern blot analysis. HepG2.2.15 cells transfected with 60 pmol of control RNA were used as a control. c, d) HBV surface antigen (HBsAg), HBV envelope antigen (HBeAg) and HBV core protein (HBc) were inhibited by miR-125b. HepG2.2.15 cells were cotransfected with 30 pmol of miR-125b mimic and 30 pmol of control RNA or miR-125b inhibitor, and supernatant was collected for ELISA and western blot 48 h post-transfection. Asterisks indicate statistical difference between groups
miR-125b targets the 3′UTR of SCNN1A
Based on the gene expression profile, one potential target gene associated with miR-125b, SCNN1A, was predicted. It was found that nt 927-933 of the SCNN1A 3′UTR matched the seed sequence of miR-125b (Fig. 3a). We further analyzed SCNN1A expression by quantitative PCR and western blot in cells overexpressing miR-125b. Overexpression of miR-125b downregulated both mRNA and protein levels of SCNN1A in HepG2.2.15 cells (Fig. 3b and c), suggesting that SCNN1A might be one of the targets of miR-125b. We then cotransfected HepG2 cells with an miR-125b mimic or its mutants and then plasmid construct pGL3-SCNN1A, which contained the 3′UTR of SCNN1A fused to a luciferase gene. Using a dual luciferase system, we found that the luciferase activity was inhibited when miR-125b was overexpressed, but the luciferase activity was restored when the seed sequence of miR-125b was mutated (Fig. 3d).
miR-125b targets SCNN1A in vitro. a) Bioinformatics prediction of miR-125b-SCNN1A interaction. b, c) miR-125b inhibits SCNN1A mRNA and protein expression in vitro. SCNN1A mRNA and protein expression were determined by qPCR and western blot after transfection of HepG2.2.15 cells with miR -125b. d) miR-125b targets the 3′UTR of SCNN1A. HEK293 cells were cotransfected with miR-125b mimics or miR-125b mutants (miR-125bM) and pGL3-SCNN1A. The luciferase activity was determined 36 h after transfection. The histogram shows the normalized firefly/Renilla luciferase activities as relative values compared to the negative control. Asterisks indicate statistical differences between the miR-125b and mutant groups
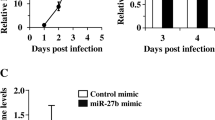
miR-125b inhibits HBV expression by regulating SCNN1A expression
To verify that miR125b regulates HBV expression by targeting the SCNN1A gene, HepG2.2.15 cells were cotransfected with an miR-125b mimic or its mutant (miR-125b M) and a plasmid expressing SCNN1A (pCDNA3.1-SCNN1A). The HBV DNA level as well as HBV protein expression decreased after transfection with miR-125b and SCNN1A, but the HBV expression level recovered when the miR-125b mutant was introduced (Fig. 4a-d). The effect of miR-125b on HBV expression decreased further when HepG2.2.15 cells were cotransfected with siRNA targeting SCNN1A (si-SCNN1A) and miR-125b (Fig. 5). This indicated that miR-125b regulates HBV expression by targeting the SCNN1A gene.
miR-125b regulates HBV expression by targeting SCNN1A. a) miR-125b inhibits HBV intermediate expression. HepG2.2.15 cells were co-transfected with pcDNA-SCNN1A and 50 pmol of miR-125b, miR-125b mutant (miR-125bM) or control RNA, and HBV viral particles were extracted 72 h post-transfection and subjected to qPCR. c, d) HBV surface antigen (HBsAg) and HBV envelope antigen (HBeAg) were inhibited when cells were co-transfected with miR-125b and SCNN1A. HepG2.2.15 cells were transfected with 50 pmol of miR-125b mimic, miR-125b mutant or control RNA, and the supernatant was collected for ELISA 48 h post-transfection. Asterisks indicate statistical differences between the three groups
Gene silencing of SCNN1A aggravates the inhibitory effect of miR-125b on HBV replication. Cells were co-transfected with 30 pmol of miR-125b and si-SCNN1A or siControl. HBV viral DNA was detected by qPCR and Southern blot (a, b), and the HBV core protein expression level was determined by western blot (c)
Discussion
MicroRNAs are important small non-coding RNAs that primarily mediate posttranscriptional gene regulation. Recent evidence has shown that several miRNAs are involved in HBV infection. Our microarray profiling analysis of miRNAs during HBV infection showed that a significant number of miRNAs are differentially expressed in both HepG-HBV and HepG2.2.15 cells, suggesting that some common mechanisms may be involved in acute and chronic infection at the miRNA level. Furthermore, most of these miRNA are predicted to target several genes involved in the signaling pathways of angiogenesis, apoptosis, p53, Wnt, JAK-STAT and tumorigenesis. These findings are consistent with previous studies that suggest that HBV replication modulates the process of carcinogenesis, apoptosis and inflammation.
Recently, increasing evidence has suggested that there is a complex relationship between cellular miRNAs and HBV genes, suggesting that important regulatory networks exist between the virus, host miRNAs and their respective target genes. To examine the reliability of our expression dataset, we compared our results with those of others. Pan et al. found that 223 miRNAs were differentially expressed between the HepG2.2.15 and HepG2 cells. Among them, miR-29a, miR-16, miR-146a, miR-96, miR-15a, miR-195 were upregulated in HepG2.2.15 cells, which was consistent with our results. It has been reported that downregulation of miR-122a in HBV-infected cells and in patients suppresses HBV in vitro [15]. In our study, we also found that miR-122a was downregulated in HepG2.2.15 cells, which might be related to chronic HBV infection and tumorigenesis. Using an mRNA array, we found that four predicted target genes of miR-122 (GRAMD3, GNPDA2, ZBTB4 and EFHA2) showed decreased expression in HepG2.2.15 cells (data not shown). One of these four genes, ZBTB4, is a novel tumor suppressor that is a critical determinant of the cellular response to p53 [16]. In addition, Su et al. reported that miR-155 could mildly inhibit HBV infection in HepG2 cells. They also found that miR-155 could enhance innate antiviral immunity by promoting the JAK/STAT signaling pathway by targeting SOCS1 [17]. Consistent with that study, miR-155 was also upregulated in HepG2-HBV cells, but not in HepG2.2.15 cells (Table 1). On the other hand, there were some discrepancies in our microarray data when compared to previous studies. miR-602 has been found to be overexpressed in chronic HBV hepatitis, HBV-positive cirrhotic liver, and HBV-positive HCC when compared to normal paratumorous livers (NT) [18]. miR-602 plays a procarcinogenic role in HBV-related hepatocarcinogenesis by inhibiting RASSF1A expression. However, miR-602 expression was downregulated in HepG2-HBV and HepG2.2.15 cells. It is possible that this is due to differences in miRNA expression in vitro and in vivo.
miR-125b has been shown to suppress virus infection as well as tumorigenesis. Nuovo and coworkers discovered that miR-125b could target sequences in the 3′ end of HIV-1 RNA, thus silencing viral messengers [20]. Neutralizing miR-125b in T4 cells from patients with HIV under highly active antiretroviral therapy increased the in vitro efficiency of virus isolation [19]. Moreover, miR-125b regulated the replication of human papillomavirus [20]. In terms of tumorigenesis, miR-125b is downregulated in hepatocellular carcinoma (HCC) tissues and HCC cell lines, suggesting potential tumor suppression by target host genes [21]. So far, we have not found any reports about miR-125b and HBV infection. In our study, we found that miR-125b was downregulated in both HepG2-HBV and HepG2.2.15 cells, indicating a possible role of miR-125b in HBV infection. Using an mRNA array, one potential miR-125b-targeted gene, SCNN1A, was upregulated in HepG2.2.15 cells. SCNN1A controls fluid and electrolyte transport across epithelia in many organs [22, 23], and mutations in this gene have been associated with pseudohypoaldosteronism type 1 (PHA1) [24]. Importantly, ectopic expression of miR-125b inhibited HBV replication and SCNN1A expression, providing evidence that miR125b regulates HBV replication by targeting SNN1A. However, the role of miR-125b and SCNN1A in HBV infection needs further investigation.
Conclusion
In this study, we explored the miRNA expression pattern during HBV infection in a cell model and found that miR-125b was downregulated in both an HBV transient expression model and a cell line stably expressing HBV. Further investigation showed that miR-125b regulates HBV expression by targeting the SCNN1A gene. Future studies should be devoted to understanding how SCNN1A impinges on HBV expression and to exploring further if miR-125b could be an anti-HBV therapeutic target.
References
Andreas S, Philippe G, Stephan U (2007) Hepatitis B virus infection initiates with a large surface protein-dependent binding to heparin sulfate proteoglycans. Hepatology 46:1759–1768
Zoulim F, Locarnini S (2009) Hepatitis B virus resistance to nucleos(t)ide analogues. Gastroenterology 137(5):1593–1608
Pei S, Zhang Y, Xu H, Chen X, Chen S (2011) Inhibition of the replication of hepatitis B virus in vitro by pu-erh tea extracts. J Agric Food Chem 59:9927–9934
Liu C, Wang Y, Wu C, Pei R, Song J, Chen S, Chen X (2013) Dioscin’s antiviral effect in vitro. Virus Res 172:9–14
Bartel DP (2004) MicroRNAs: genomics, biogenesis, mechanism, and function. Cell 116:281–297
Berkhout B, Jeang KT (2007) RISCy business: MicroRNAs, pathogenesis, and viruses. J Biol Chem 282:26641–26645
Ambros V (2004) The functions of animal microRNAs. Nature 431:350–355
Sendi H (2012) Dual role of miR-122 in molecular pathogenesis of viral hepatitis. Hepat Mon 12(5):312–314
Pan Xiao-Ben, Ma Hui, Jin Qian, Wei Lai (2012) Characterization of microRNA expression profiles associated with hepatitis B virus replication and clearance in vivo and in vitro. J Gastroenterol Hepatol 27:805–812
Jin W, Wang Y, Chen L, Wu E, Ye X, Gao GF, Wang F, Chen Y, Duan Z, Meng S (2012) Loss of microRNA122 expression in patients with hepatitis B enhances hepatitis B virus replication through cyclin G(1) -modulated P53 activity. Hepatology 55(3):730–741
Fan CG, Wang CM, Tian C, Wang Y, Li L, Sun WS, Li RF, Liu YG (2011) miR-122 inhibits viral replication and cell proliferation in hepatitis B virus-related hepatocellular carcinoma and targets NDRG3. Oncol Rep 26(5):1281–1286
Potenza Nicoletta, Papa Umberto, Mosca Nicola, Zerbini Francesca, Nobile Valentina, Russo Aniello (2011) Human microRNA hsa-miR-125a-5p interferes with expression of hepatitis B virus surface antigen. Nucleic Acids Res 39:5157–5163
Hu W, Wang X, Ding X, Li Y, Zhang X, Xie P, Yang J, Wang S (2012) MicroRNA-141 represses HBV replication by targeting PPARA. PLoS One 7(3):e34165
Huang Jinfeng, Wang Yue, Guo Yingjun, Sun Shuhan (2010) Down-regulated MicroRNA-152 induces aberrant DNA methylation in hepatitis B virus-related hepatocellular carcinoma by targeting DNA methyltransferase 1. Hepatology 52:1
Weber A, Marquardt J, Elzi D, Forster N, Starke S, Glaum A, Yamada D, Defossez PA, Delrow J, Eisenman RN, Christiansen H, Eilers M (2008) Zbtb4 represses transcription of P21CIP1 and controls the cellular response to p53 activation. EMBO J 27(11):1563–1574
Kim K, Chadalapaka G, Pathi SS, Jin UH, Lee JS, Park YY, Cho SG, Chintharlapalli S, Safe S (2012) Induction of the transcriptional repressor ZBTB4 in prostate cancer cells by drug-induced targeting of MicroRNA-17-92/106b-25 clusters. Mol Cancer Ther 11(9):1852–1862
Chenhe Su, Hou Zhaohua, Zhang Cai, Tian Zhigang, Zhang Jian (2011) Ectopic expression of microRNA-155 enhances innate antiviral immunity against HBV infection in human hepatoma cells. Virology 8:354
Yang Lian, Ma Zhaolong, Wang Dongdong, Zhao Wenyue, Chen Libo, Wang Guobin (2010) MicroRNA-602 regulating tumor suppressive gene RASSF1A is over-expressed in hepatitis B virus-infected liver and hepatocellular carcinoma. Cancer Biol Ther 9(10):803–808
Huang J, Wang F, Argyris E, Chen K, Liang Z, Tian H, Huang W, Squires K, Verlinghieri G, Zhang H (2007) Cellular microRNAs contribute to HIV-1 latency in resting primary CD4+T lymphocytes. Nat. Med 13:1241–1247
Nuovo GJ, Wu X, Volinia S, Yan F, di Leva G, Chin N, Nicol AF, Jiang J, Otterson G, Schmittgen TD, Croce C (2010) Strong inverse correlation between microRNA-125b and human papillomavirus DNA in productive infection. Diagn Mol Pathol 19:135–143
Jia HY, Wang YX, Yan WT, Li HY, Tian YZ, Wang SM, Zhao HL (2012) MicroRNA-125b functions as a tumor suppressor in hepatocellular carcinoma cells. Int J Mol Sci 13(7):8762–8774
Donaldson SH, Boucher RC (2007) Sodium channels and cystic fibrosis. Chest 132:1631–1636
Kellenberger S, Schild L (2002) Epithelial sodium channel/degenerin family of ion channels: a variety of functions for a shared structure. Physiol Rev 82:735–767
Dirlewanger M, Huser D, Zennaro MC, Girardin E, Schild L, Schwitzgebel VM (2011) A homozygous missense mutation in SCNN1A is responsible for a transient neonatal form of pseudohypoaldosteronism type 1. Am J Physiol Endocrinol, Meta 301(3):467–473
Acknowledgments
The reported work was supported by the National Natural Science Foundation of China (81201282), Chongqing Science Technology Commitment Project (cstc2012jiA10047).
Author information
Authors and Affiliations
Corresponding author
Additional information
Z. Zhang, J. Chen, and Y. He contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhang, Z., Chen, J., He, Y. et al. miR-125b inhibits hepatitis B virus expression in vitro through targeting of the SCNN1A gene. Arch Virol 159, 3335–3343 (2014). https://doi.org/10.1007/s00705-014-2208-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00705-014-2208-y