Abstract
Receptor–receptor interactions within receptor heterodimers and receptor mosaics formed by different types of GPCRs represent an important integrative mechanism for signaling in brain networks at the level of the plasma membrane. The malfunction of special heterodimers and receptor mosaics in the ventral striatum containing D2 receptors and 5-HT2A receptors in cortical networks may contribute to disturbances of key pathways involving ventral striato-pallidal GABA neurons and mediodorsal thalamic prefrontal glutamate neurons that may lead to the development of schizophrenia. The ventral striatum transmits emotional information to the cerebral cortex through a D2 regulated accumbal–ventral pallidal–mediodorsal–prefrontal circuit which is of special interest to schizophrenia in view of the reduced number of glutamate mediodorsal–prefrontal projections associated with this disease. This circuit is especially vulnerable to D2 receptor activity in the nucleus accumbens, since it produces a reduction in the prefrontal glutamate drive from the mediodorsal nucleus. The following D2 receptor containing heterodimers/receptor mosaics are of special interest to schizophrenia: A2A–D2, mGluR5–D2, CB1–D2, NTS1–D2 and D2–D3 and are discussed in this review. They may have a differential distribution pattern in the local circuits of the ventral striato-pallidal GABA pathway, predominantly located extrasynaptically. Specifically, trimeric receptor mosaics consisting of A2A–D2–mGluR5 and CB1–D2–A2A may also exist in these local circuits and are discussed. The integration of receptor signaling within assembled heterodimers/receptor mosaics is brought about by agonists and allosteric modulators. These cause the intramembrane receptor–receptor interactions, via allosteric mechanisms, to produce conformational changes that pass over the receptor interfaces. Exogenous and endogenous cooperativity is discussed as well as the role of the cortical mGluR2–5-HT2A heterodimer/receptor mosaic in schizophrenia (Gonzalez-Maeso et al. 2008). Receptor–receptor interactions within receptor heterodimer/receptor mosaics of different receptors in the ventral striatum and cerebral cortex give novel strategies for treatment of schizophrenia involving, e.g., monotherapy with either A2A, mGluR5, CB1 or NTS1 agonists or combined therapies with some of these agonists combined with D2-like antagonists that specifically target the ventral striatum. In addition, a combined targeting of receptor mosaics in the ventral striatum and in the cerebral cortex should also be considered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Receptor–receptor interactions within receptor heterodimers and receptor mosaics of different types of G protein coupled receptors (GPCRs, high order heteromers) represent an important integrative mechanism for signaling that already occurs at the level of the plasma membrane (Agnati et al. 2003, 2007b; Carriba et al. 2008; Fuxe et al. 2003a, 2007a; Gozes 2005; Guo et al. 2008; Marshall 2001, 2005; Maurel et al. 2008; Milligan and Smith 2007)]. During this integrative process, transmitters act at their orthosteric binding sites and induce conformational changes in other receptors through allosteric mechanisms. This integrative process can involve cooperative allosteric interactions when receptor subtypes that recognize the same ligand are involved (Agnati et al. 2007b, 2008; Fuxe et al. 2007a, 2008). In addition, allosteric modulators that act at allosteric modulatory sites of one receptor may also participate in this integrative process of heterodimer and receptor mosaic signaling (Agnati et al. 2006, 2007a; Fuxe et al. 2007a; Milligan and Smith 2007). The latter has been elegantly illustrated through works on homocysteine (Agnati et al. 2006, 2007b). Homocysteine acts as a negative allosteric modulator of dopamine D2 receptors (D2) and binds noncovalently to two arginine-rich epitopes of its third intracellular loop through an eletrostatic interaction between arginine and thiol groups of homocysteine (Agnati et al. 2006, 2007b).
In the present review, we will discuss how a dysfunction in special heterodimers and receptor mosaics in the ventral striatum and cortical networks may contribute to malfunction of key pathways involving ventral striato-pallidal γ-aminobutyric acid (GABA) neurons and prefrontal cortical glutamate projections to the ventral tegmental area (VTA). In the VTA, the dopamine (DA) A10 cell groups are located and project into the ventral striatum and the prefrontal and cortical limbic regions (Dahlstroem and Fuxe 1964; Anden et al. 1966; Berger et al. 1976). Such neuronal systems appear to participate in schizophrenia in view of the meso-limbic DA hyperfunction hypothesis as well as the N-methyl-d-aspartic acid (NMDA) glutamate receptor hypofunction hypotheses of schizophrenia in which striatal D2 receptors play a major role and are targeted in treatment therapies by antipsychotic drugs (Carlsson and Lindqvist 1963; Carlsson 1988; Svensson 2000; Seeman et al. 2006; Fuxe et al. 2007b; Stahl 2007a). D2 containing heterodimers and receptor mosaics located within such pathways and networks may therefore become important novel targets for treatment of schizophrenia once these are fully understood (Fuxe et al. 2005, 2007a, 2008.
Ventral striatum
The ventral striatum is an important interface between the limbic and motor system (Mogenson et al. 1980; Groenewegen et al. 1996; Groenewegen and Trimble 2007) in which disturbances in this interface may contribute to the development of schizophrenia (Fuxe 1970, Grace 2000, Heimer 2000, Fuxe et al. 2007b). The ventral striatum receives inputs from regions of the prefrontal cortex, the amygdala, and the hippocampus belonging to the limbic system and the midline thalamus. It is also densely innervated by the meso-limbic DA system that originates in the VTA and is involved in the motivational aspects of behavior and in the gating of the flow of emotional information to the cerebral cortex, specifically the prefrontal cortex (Dahlstroem and Fuxe 1964; Fuxe 1965; Anden et al. 1966; Schultz 2002; Fuxe et al. 2007b). A dense DA innervation exists in the majority of the ventral striatum including the nucleus accumbens core and shell, as well as the olfactory tubercle (Fuxe 1965; Fuxe et al. 1979). All of the subregions are rich in both dopamine D1 receptor (D1) and D2 receptors; however, dopamine D3 receptors (D3) are specifically found within the nucleus accumbens shell and the islands of Calleja (Joyce and Gurevich 1999; Schwartz et al. 2000).
The efferent projections from the nucleus accumbens core are complex. They reach the subcomissural ventral pallidum as well as the medial part of the globus pallidus interna (GPi) and the pars reticulata of the substantia nigra. The ventral pallidum connects to the subthalamic nucleus becoming part of the indirect pathway from the dorsal striatum (Groenewegen et al. 1993). It is of particular interest that the medial parts of GPi and pars reticulata project back to the medial and orbital prefrontal regions via thalamic relay stations, especially the mediodorsal thalamic nucleus (MD). This completes one accumbal–thalamocortical circuit, since these prefrontal regions project into the nucleus accumbens core (Alexander et al. 1990; Groenewegen et al. 1996).
Instead, the nucleus accumbens shell projects into the ventral and medial parts of the ventral pallidum and the lateral preoptic area. It also innervates the VTA and the dorsal tier of the zona compacta of the substantia nigra, all with high densities of DA cell bodies. In view of nigral DA projections to the dorsal striatum, it illustrates that a spiraling circuitry of ventral striato-nigrostriatal pathways can arise from the nucleus accumbens shell to the dorsolateral striatum (Haber et al. 2000). In fact, cocaine-seeking habits rely on DA-dependent serial connectivity from the ventral striatum to the dorsal striatum for their development (Belin and Everitt 2008). The nucleus accumbens takes control over the dorsal striatal processes via the spiraling striato-nigrostriatal circuitry.
We believe this pathological neuronal mechanism may also exist in schizophrenia where obsessive-compulsive symptoms may develop (Sturm et al. 2003; van Kuyck et al. 2007). In fact, an increase in meso-limbic DA activity is postulated to exist in schizophrenia that subsequently leads to the increased activation of DA receptor subtypes in the nucleus accumbens (Fuxe 1970). Hence, D2 receptors are the major target for antipsychotic drugs (Seeman et al. 2006). Furthermore, the NMDA receptor hypofunction hypothesis of schizophrenia also exists and is based on the fact that the NMDA receptor antagonist phencylidine can mimic the positive as well as the negative symptoms of schizophrenia (Stahl 2007a). This indicates that many glutamate synapses are dysfunctional with reduced informational processing including those of the prefrontal–nucleus accumbens glutamate system. Thus, the prefrontal cortex can no longer exert its proper executive function over the nucleus accumbens and this deficit will allow the ventral striatum, with the nucleus accumbens being its major structure, to take over control of behavior via its integrative role in emotions and motivation (mainly nucleus accumbens shell) and strong link to the motor systems (mainly nucleus accumbens core). The NMDA receptor hypofunction hypothesis is also supported by observations that the genetics of schizophrenia appear to converge on the NMDA glutamate receptor (Stahl 2007b).
Another major nucleus when discussing the neuroanatomy of schizophrenia is the MD nucleus since a loss of neurons in this nucleus has been reported in those who suffer from schizophrenia (Pakkenberg 1990; Popken et al. 2000; Young et al. 2000). In the study of (Popken et al. (2000), it is of interest to note their discovery of a specific subnucleus loss of nerve cells in MD nucleus with significant reductions in the total neuron number only in the parvocellular (pc) and densocellular (dc) subnuclei. The pc receives inputs especially from the ventral pallidum and sends its glutamate outputs to the dorsal and lateral areas of the prefrontal cortex, which are affected in schizophrenia, showing hypoactivity. These findings are not in agreement with the work of (Danos et al. (2005), showing a reduction in the volume of the MD thalamic nucleus, associated with a lack of reduction in the total neuron number and neuron density. Volume reductions were also observed in another association thalamic nucleus, the medial pulvinar nucleus and in the whole thalamus in schizophrenia (Danos et al. 2003; Danos 2004). Deficiency in other limbic circuits most likely exist in schizophrenia since there is a reduction in the paralbumin positive glutamate/aspartate containing neurons of the mammillary bodies projecting into the anterior thalamus in schizophrenia (Bernstein et al. 2007). It should be noticed, however, that other groups have failed to observe any reductions in the number of MD neurons or in the volume of this nucleus (Cullen et al. 2003; Dorph-Petersen et al. 2004).
Thus, the strength of the MD glutamate projections into the prefrontal cortex may be reduced in schizophrenia. This will bring down the glutamate drive in this region and add to the postulated NMDA receptor hypofunction hypothesis. The D2 regulated accumbal–ventral pallidal–MD–prefrontal circuit therefore becomes a circuit of special interest in schizophrenia in view of the reduced number and/or activity of glutamate MD–prefrontal projections making this circuit especially vulnerable to D2 receptor activity in the nucleus accumbens. Taking this into consideration, D2 receptor activity within the nucleus accumbens will result in a further reduction in the activity of the MD–prefrontal glutamate projections and exacerbate schizophrenic symptoms. However, there is the possibility that certain subpopulations with schizophrenia may not show this neuropathology.
D2 receptor containing heterodimers/receptor mosaics of different types of receptors in the ventral striatum
A large number of different types of D2 receptor heterodimers/receptor mosaics appear to exist in the ventral striato-pallidal GABA neurons at the dendritic, terminal and collateral levels (Fuxe et al. 2007a, 2008). Within their local circuits, such heteromers can be found inter alia in the dendritic spines of the striato-pallidal GABA neurons, their GABA collateral terminals and in the cortical glutamate terminals. In the present review, we will deal with the D2 receptor heterodimers/receptor mosaics that are of special interest in schizophrenia: adenosine A2A receptor (A2A)–D2, metabotropic glutamate receptor 5 (mGluR5)-D2, cannabinoid receptor 1 (CB1)–D2, neurotensin receptor 1 (NTS1)–D2 and D2–D3,, which may have a differential distribution pattern in the local circuits of the ventral striato-pallidal GABA pathway mainly located extrasynaptically (Agnati et al. 2003; Maggio et al. 2005; Ferre et al. 2007; Fuxe et al. 2007a, 2008; Ferraro et al. 2008). The existence of trimeric receptor mosaics of A2A–D2–mGluR5 mainly located extrasynaptically in the dendritic spines of these local circuits has also been proposed (Ferre et al. 2002; Fuxe et al. 2003a, 2007a, 2008; Schwarzschild et al. 2006).
Furthermore, novel evidence inter alia with the recently developed sequential bioluminescence resonance energy transfer (BRET) and fluorescence resonance energy transfer (FRET) techniques indicate the existence of trimeric A2A–D2–CB1 receptor mosaics (Carriba et al. 2008; Marcellino et al. 2008), which may be located mainly extracellularly in the dendritic spines of the ventral striato-pallidal GABA neurons, cortico-accumbal glutamate terminals and the collateral GABA terminals of the local circuits of these neurons as well as in the GABA terminals of the external globus pallidus belonging to the ventral striato-pallidal GABA pathway (Andersson et al. 2005a; Pickel et al. 2006).
The D2-long isoform of the D2 receptor is mainly located in the dendrites of the striato-pallidal GABA neurons, while the D2-short isoform represents the D2 autoreceptor on DA terminals inhibiting DA release (Khan et al. 1998). Also, the D2-mediated presynaptic inhibition of striatal glutamate transmission mainly involves the D2-short receptor, while the presynaptic inhibition of the striatal GABA transmission involves both D2 isoforms (Centonze et al. 2004). Such differences in distribution of these two D2 isoforms may contribute to differences in the receptor heterodimer and receptor mosaic assembly and their receptor–receptor interactions depending on their location in the elements of the local circuits and thus in their physiology and pharmacology.
It should be considered that endogenous cooperativity exists in the heterodimer/receptor mosaic assembly process based on the allosteric interactions between the receptor protein monomers as they bind to each other via the receptor interfaces (Agnati et al. 2007b; Fuxe et al. 2008). Cooperativity in macromolecular assembly has recently been discussed and represents a thermodynamic process to drive the macromolecular complex formation and make it more stable than the sum of its components (Williamson 2008). An endogenous cooperativity can explain the constitutive changes in receptor recognition, G protein coupling and selection, and receptor trafficking of the receptors participating in the heterodimer/receptor mosaics in the absence of transmitter ligands and allosteric modulators (Fuxe et al. 2008).
It is therefore clear that D2 receptors in different constitutive D2 receptor heterodimers/receptor mosaics can have different functional and pharmacological properties even if they contain the same D2 isoform. It should be considered that the D2 partial agonist aripiprazole may be an antipsychotic drug (Tamminga and Carlsson 2002; Novi et al. 2007; Carlsson and Carlsson 2008; Stahl 2008), since it mainly targets the D2 autoreceptor heterodimer/receptor mosaic on the DA nerve terminals as an agonist. The postjunctional extrasynaptic D2 heterodimer/receptor mosaics on the terminals and dendrites of the local circuits may be less affected. At these locations, this compound may exert antagonistic actions by its partial agonist activity on these receptor mosaics. Based on this theory, the development of novel antipsychotic D2 antagonists could also be based on targeting the different postjunctional extrasynaptic D2 containing heterodimers/receptor mosaics in the local circuits of the ventral striato-pallidal GABA neurons. This may reduce the positive symptoms of schizophrenia with reduced extrapyramidal side effects and cognitive deficits related to blockade of dorsal striatal and cortical D2 receptors, respectively (Tamminga and Carlsson 2002; Del Arco et al. 2007; Stahl 2007a). The endogenous cooperativity in the receptor mosaic should however not only be discussed in terms of allosteric cooperativity, but also in terms of configurational cooperativity (Whitty 2008). The receptor proteins may be regarded as polyvalent ligands, which contain multiple binding epitopes, similar or different, binding the other receptor. As discussed by (Whitty (2008) the first binding interaction makes the subsequent binding site interactions more easily performed if the receptor geometries are suitable for an interaction. If so, an enhanced binding is observed since the initial binding interaction pre-organizes the other binding sites for receptor protein interactions by reducing the number of inefficient configurations, making possible binding interactions at reduced entropic cost. The multiple interactions between the two receptor proteins may also cooperatively increase the enthalpic stability of all the binding interactions between the receptor proteins (Williams et al. 2004).
The integration of receptor signaling in the assembled heterodimer and receptor mosaic of different types of GPCRs is instead brought about by exogenous agonist ligands and allosteric modulators not belonging to the receptor protein. This causes the intramembrane receptor–receptor interactions via allosteric mechanisms, with conformational changes passing over the receptor interfaces. Exogenous cooperativity develops when similar subtypes of receptors having the same transmitter directly interact (Agnati et al. 2007b; Fuxe et al. 2007a, 2008; Agnati et al. 2008). The functional outcome of the integrative process with emergent function is determined by the stoichiometry, topology, agonist concentrations and receptor recognition properties determining the rank order of receptor activation and how this process becomes altered by allosteric modulators and the microenvironment (Agnati et al. 2007b, 2008, Fuxe et al. 2007a, 2008).
The D2–D3 heterodimer/receptor mosaic
D2–D3 heterodimers have been discovered in cellular models (Scarselli et al. 2001; Maggio et al. 2003) and are of particular interest for schizophrenia since they are colocated in ventral striato-pallidal GABA neurons, especially in the nucleus accumbens shell and in limbic DA terminals (Surmeier et al. 1996; Gurevich and Joyce 1999; Joyce and Gurevich 1999; Diaz et al. 2000; Schwartz et al. 2000). It is likely that in DA terminals, the D3 and the D2-short autoreceptor form a heterodimer/receptor mosaic and together modulate DA release (Diaz et al. 2000; Millan et al. 2000; Sokoloff et al. 2006). Instead, in ventral striatal nerve cells, D2L–D3 heterodimers/receptor mosaics may be formed. Specific D3 antagonists have also been developed and proposed to be antipsychotic drugs (Millan et al. 2000; Schwartz et al. 2000; Joyce and Millan 2005).
The actions of the partial D2 agonist antipsychotic aripiprazole as well as the partial D2 agonist candidate antipschotics including S33592, bifeprunox, N-desmethylclozapine, and preclamol have recently been characterized with regard to potential D2L–D3 heterodimer/receptor mosaics in cellular models (Novi et al. 2007). An interesting finding was obtained that the partial D2 agonist actions of these compounds on D2L receptors were counteracted in the D2L–D3 heterodimer/receptor mosaics due to a reduced coupling efficiency in the D2L receptor brought about by the allosteric interaction in the D2–D3 interface. Instead, they behaved as D2 antagonists at the D2L–D3 heterodimer/receptor mosaic. This analysis was made possible by the use of COS-7 cells co-transfected with a D3 receptor-insensitive, chimeric adenylate cyclase (AC)-V/VI (Novi et al. 2007). These results indicate that one reason for the putative antipsychotic effects of the partial D2 agonists may be that in the ventral striatum, they exert mainly antagonist action at the D2L receptor due to the substantial existence of postjunctional D2L–D3 heterodimers/receptor mosaics canceling the partial D2 agonist actions of these candidate antipsychotics. Instead in the dorsal striatum, such heterodimers/receptor mosaics hardly exist, and therefore the partial D2 agonist effects can be exerted at the postjunctional D2 receptors, leading to reduced extrapyramidal side effects due to improved motor function via increases in the D2 receptor activity.
The A2A–D2 heterodimer/receptor mosaic
The A2A–D2 heterodimer/receptor mosaic was first indicated from the demonstration of antagonistic intramembrane receptor–receptor interactions through biochemical binding techniques in striatal membranes (Ferre et al. 1991; Fuxe et al. 1993). Further evidence for its existence were demonstrated using resonance energy transfer techniques (BRET and FRET) and co-immunoprecipitation experiments (Hillion et al. 2002; Canals et al. 2003; Kamiya et al. 2003). The zones of receptor interactions were mapped and modeled and important epitope–epitope electrostatic interactions between negatively charged epitopes of the A2A (specifically involving a phosphorylated serine in its C terminal tail) and positively charged epitopes (rich in arginine residues) in the intracellular loop (IC) 3 of the D2 receptor were discovered (Ciruela et al. 2004). For reviews, see Fuxe et al. (2005, 2007a, 2008).
The recent discovery of higher order oligomers of D2 receptors in living mammalian cells at physiological expression levels is highly interesting. These were demonstrated through the use of bioluminescence/fluorescence complementation together with resonance energy transfer (Guo et al. 2008). Likewise, higher order A2A receptor oligomers have been observed using combined BRET and bimolecular fluorescence complementation techniques (Gandia et al. 2008). Therefore, A2A–D2 heterodimers that display antagonistic interactions should be considered with D2 coupled to Gi or Gq/11 to regulate AC and phospholipase C (PLC), linked to inhibition of L-type voltage-dependent calcium channels (VDCC) (Ferre et al. 2007, Fuxe et al. 2007a, Fuxe et al. 2007d, Fuxe et al. 2008). Receptor mosaics of A2A and D2 receptors with an unknown stoichiometry and topology, where A2A may antagonize D2 signaling to Gi and Gq/11, should also be considered. In such a receptor mosaic the D2 receptors via Gi in turn inhibit the A2A-activated AC keeping the A2A signaling at a low basal level.
The A2A–D2 heterodimer/receptor mosaic is mainly located extrasynaptically on the dendritic spines of the local circuits of the ventral and dorsal striato-pallidal GABA neurons. These receptor mosaics may also exist on either glutamate terminals and/or collateral GABA terminals within these local circuits [for reviews, see Ferre et al. (2007), Fuxe et al. 2007a, 2007d, 2008]. Recently, further studies have been performed to obtain a physiological correlate to the antagonistic A2A–D2 receptor interactions in this receptor mosaic by pairing afferent stimulation with postsynaptic spikes in a burst mode (Shen et al. 2008). In D2 positive striato-pallidal neurons, long-term potentiation (LTP) was induced when spiking was induced 5 ms after the synaptic stimulation, while long-term depression (LTD) developed when postsynaptic spiking was induced prior to synaptic stimulation. The D2 antagonist sulpiride blocked LTD underlining the importance of D2 receptors for LTD. In contrast, the A2A antagonist SCH58261 counteracted the introduction of LTP in the D2 positive striato-pallidal nerve cells (Shen et al. 2008). This may be at least in part explained by the removal of the tonic A2A reduction of postjunctional D2 signaling through the A2A/D2 receptor mosaic (Fuxe et al. 2007d). The increased D2 activity will not allow the increased excitability to be maintained via its gating effects on currents over the voltage-dependent calcium channels (Cav), inward rectifier potassium channels (Kir), a glutamate-gated ion channel that is permeable to Na+ and K+ (AMPA) and voltage-dependent sodium channels (Nav), favoring the silencing of the D2 striato-pallidal neurons (Surmeier et al. 2007).
In line with these results, the D2 agonist quinpirole transformed the normal LTP development into LTD, and when the A2A agonist CGS 221680 and quipirole were co-administered LTP was restored (Shen et al. 2008). These results can also be explained by the antagonistic A2A–D2 receptor interaction in the A2A–D2 receptor mosaic, markedly reducing D2 signaling and setting free the A2A signaling by removal of the inhibitory tone of D2 via Gi on the A2A activated AC mediated via Golf (Fuxe et al. 2007c). It seems likely that the resulting A2A-mediated activation of protein kinase A (PKA) contributes to the excitability and upstate (depolarized plateau potential favoring the elicitation of action potentials) of this neuron system and restoration of LTP by phosphorylation of L-type voltage-dependent calcium channels, dopamine and cyclic AMP-regulated phosphoprotein with molecular weight 32 kDa (DARPP-32) at threonine 34 and of GluR1–AMPA receptors playing an important role in synaptic plasticity (Hernandez-Lopez et al. 2000, Hakansson et al. 2006, Bateup et al. 2008). The strength of the A2A agonist action in inducing LTP is evident by its ability to do so in the presence of a D2 receptor antagonist using a protocol that should not result in LTP (postsynaptic spiking prior to synaptic activation) (Shen et al. 2008). These results by (Shen et al. 2008) therefore indicate that the A2A–D2 receptor–receptor interactions in receptor mosaics play an important role in striatal synaptic plasticity, contributing to making it bidirectional and Hebbian in the striato-pallidal GABA neurons.
In animal models of Parkinson’s disease (PD) with severe degeneration of DA terminals, abnormal striatal plasticity was observed, since with the protocol normally inducing LTD, LTP was observed (spiking prior to synaptic activation) (Shen et al. 2008). This LTP was blocked by A2A antagonists underlining the view of a dominance of A2A over D2 signaling in the A2A–D2 receptor mosaic in PD (Fuxe et al. 2007c). The impact of D2 for LTD was again demonstrated in the PD model by recruiting LTD with a D2 agonist. The results underline the value of introducing A2A antagonists as antiparkinsonian drugs (Schwarzschild et al. 2006; Fuxe et al. 2007d, 2008).
On the basis of the existence of the antagonistic A2A–D2 receptor interactions in the ventral striato-pallidal GABA pathway, A2A agonists were early on proposed to be atypical antipsychotic drugs (Ferre et al. 1994, Fuxe et al. 2007a, 2008). In fact, A2A agonists show an atypical antipsychotic profile in the rat amphetamine and phencyclidine model of schizophrenia (Rimondini et al. 1997) and in the Cebus apella monkey model of schizophrenia (Andersen et al. 2002). A glutamate releasing action in the nucleus accumbens may also contribute to its atypical antipsychotic profile (Fuxe et al. 2008). Recently, evidence has been obtained that the antagonistic A2A–D2 receptor interactions importantly modulate the information flow in the neuronal circuit from the nucleus accumbens to the prefrontal cortex via the ventral pallidum and the mediodorsal thalamic nucleus. The antipsychotic activity of A2A agonists appears to mainly rely on the ability of these compounds to counteract the D2 receptor-induced reduction of the glutamate drive from the mediodorsal thalamic nucleus to the prefrontal cortex via their reduction of D2 signaling in the nucleus accumbens (Fuxe et al. 2008). It brings the A2A agonists targeting the A2A–D2 receptor mosaic into the center of the D2 and NMDA hypothesis of schizophrenia where combined treatment with low doses of A2A and D2 antagonists may be an optimal treatment to avoid collateral effects (Fuxe et al. 2008).
A2A–D3 heterodimers/receptor mosaics and putative A2A–D2–D3 receptor mosaics
A2A–D3 heterodimers/receptor mosaics have been demonstrated in cellular models and exhibit an antagonistic receptor interaction where A2A agonists reduce both D3 receptor agonist binding and D3 receptor signaling (Torvinen et al. 2005). It is therefore possible that such receptor complexes exist in the ventral striatum where A2A and D3 receptors are co-distributed, especially in the nucleus accumbens. A2A agonists may therefore exert their antipsychotic effects in animal models of schizophrenia by targeting these receptor mosaics and producing a reduction in D3 receptor signaling (Fuxe et al. 2008), since D3 antagonists may have antipsychotic actions (Schwartz et al. 2000; Joyce and Millan 2005). D3 tetramers have been found in the brain (Nimchinsky et al. 1997), opening up the possibility for the existence of A2A/D3 receptor mosaics in the ventral striatum.
In view of the likely existence of D2–D3 heterodimer/receptor mosaic in the ventral striatum, it seems possible that A2A–D2–D3 receptor mosaics exist in the ventral striatum, especially in the nucleus accumbens, modulating the local circuits of the ventral striato-pallidal GABA pathway, mainly originating in the nucleus accumbens shell and core (Fuxe et al. 2008). It will be of interest to evaluate if in fact such complex receptor mosaics may be a target of antischizophrenic drugs such as D2 antagonists and of antipsychotic candidates such as D3 antagonists and A2A agonists.
Putative A2A–D2–mGluR5 receptor mosaics
The first indications for the existence of glutamate receptor–D2 receptor complexes was obtained in 1984 through the demonstration that L-glutamate could reduce the affinity of the D2 agonist binding sites in striatal membrane preparations (Fuxe et al. 1984). Later on, mGluR5 was demonstrated as the glutamate receptor involved in mediating this antagonistic receptor–receptor interaction in putative mGluR5–D2 receptor heterodimer/receptor mosaics (Ferre et al. 1999; Popoli et al. 2001). Furthermore, combined activation of A2A and mGluR5 receptors enhanced the reduction of the affinity of the D2 agonist binding sites (Popoli et al. 2001) and coimmunoprecipitation experiments showed the existence of A2A–mGluR5 heteromeric complexes (Ferre et al. 2002; Fuxe et al. 2003a). Together with the chemical anatomical analysis (Fuxe et al. 2003a, Ferre et al. 2004, Conn et al. 2005), these results indicated the existence of extrasynaptic A2A–D2–mGluR5 receptor mosaics located mainly not only on the dendritic spines of the local circuits of the ventral and dorsal striato-pallidal GABA neurons, but also on the cortico-striatal glutamate terminals (Fig. 1).
Illustration of the possible existence of CB1–D2–A2A and A2A–D2–mGluR5 receptor mosaics in different local circuits of the accumbal-pallidal GABA neurons projecting into the ventral pallidum reached by volume transmission signals. The extrasynaptic CB1–D2–A2A receptor mosaic is inter alia located on the dendritic spines of these neurons and on the incoming synaptic glutamate terminals to these spines. Activation of the CB1 receptors with CB1 agonists in this receptor mosaic leads to inhibition D2 recognition and signaling and removal of D2–Gi-mediated inhibition of A2A activated adenylate cyclase with a release of its brake on A2A signaling as shown in the upper left (1). The postulated extrasynaptic A2A–D2–mGluR5 receptor mosaic is illustrated in another local circuit of the same neurons and mainly in the dendritic spines, but may also be located in the same local circuit as you find the CB1–D2–A2A receptor mosaic. Combined activation of the A2A and mGluR5 receptors in this receptor mosaic leads to synergistic inhibition of D2 recognition and signaling as illustrated in the upper right (2)
In this receptor mosaic, A2A and mGluR5 co-activation appears to synergistically increase c-fos expression as well as extracellular signal-regulated kinase (ERK) and DARPP-32 phosphorylation (Ferre et al. 2002; Nishi et al. 2003). A2A and mGluR5 co-activation counteracts D2 recognition and signaling, probably resulting in an activation of the ventral and dorsal striato-pallidal GABA pathways. This has in fact been shown with dual-probe microdialysis showing that coactivation of mGluR5 and A2A receptors in the nucleus accumbens leads to a synergistic rise of GABA release in the ventral pallidum (Diaz-Cabiale et al. 2002b). Behavioral evidence also exists that the A2A agonist CGS21680 and the mGluR5 agonist (RS)-2-chloro-5-hydroxy-phenylglycine (CHPG) synergize in counteracting phencylidine-induced motor activity (Ferre et al. 2002). Based on this work it was proposed that combined treatment with low doses of A2A and mGluR5 agonists with or without treatment with low doses of D2 antagonists may be an interesting new strategy for treatment of schizophrenia (Fuxe et al. 2008). The finding that LTD in striato-pallidal GABA nerve cells highly dependent on D2 receptors is antagonized by mGluR5 antagonists (Shen et al. 2008) can, however, not be explained on the basis of this hypothesis, but probably is caused by a reduction of retrograde endocannabinoid signaling being enhanced by mGluR5 coupled to Gq/11 (Uchigashima et al. 2007).
Parallel to this work, it has been shown that mGluR5 activation enhances NMDA currents (Conn et al. 2005). In view of the NMDA hypofunction hypothesis of schizophrenia, it has therefore been suggested that mGluR5 agonists and positive allosteric modulators produce antipsychotic actions by enhancing synaptic NMDA signaling (Kinney et al. 2003, 2005; Conn et al. 2005). It has been shown that mGluR5 agonist counteracts the amphetamine-induced reduction in prepulse inhibition and the mGluR5 antagonist 2-methyl-6-(phenylethynyl)-pyridine (MPEP) enhances the phencyclidine (PCP)-induced disruption of prepulse inhibition (Kinney et al. 2003).
Taken together, it seems likely that the mechanism underlying the antipsychotic-like actions of mGluR5 agonists and modulators involves in part an inhibition of D2 signaling in the extrasynaptic A2A–D2–mGluR5 receptor mosaics located in the ventral striato-pallidal GABA neurons. However, it also involves an enhancement of synaptic NMDA signaling via indirect mGluR5–NMDA receptor interactions in the postsynaptic density in several brain regions, including the ventral striatum and the prefrontal cortex.
Receptor mosaic of D2 and NMDA receptors
A direct interaction between the N-terminal portion of the third intracellular loop of the D2 receptor and a C-terminal region of the NR2B subunit occurs and takes place within the microdomains of the postsynaptic densities of striatal glutamate synapses (Liu et al. 2006). This receptor interaction appears to be increased through the activation of the D2 receptors and subsequently leads to reduced NMDA receptor signaling by a reduction in the phosphorylation of NR2B through the counteraction of Ca2+/calmodulin-dependent protein kinase II binding to the NR2B receptor. Thus, D2 receptors at glutamate synapses on ventral striato-pallidal GABA neurons may assist in silencing these neurons through direct interactions with NR2B containing NMDA receptors. This receptor mosaic represents an interesting novel target for antischizophrenic drugs including D2 antagonists and/or partial D2 agonists. It is possible that synaptic mGluR5 receptors may, in part, increase NR2B–NMDA signaling through its antagonistic interaction with D2 receptors [see above and Fuxe et al. (2008)]. It should also be noted that timing-dependent LTP in the striato-pallidal GABA neurons is blocked by NMDA antagonists and the antagonistic D2–NR2B–NMDA interaction helps understand the crucial role of D2 receptors for the development of LTD in these neurons (Shen et al. 2008).
CB1–D2 heterodimer/receptor mosaics and CB1–D2–A2A receptor mosaics
Indications for the existence of CB1–D2 heterodimers/receptor mosaics were first obtained in 2003 (Fuxe et al. 2003b). In 2005, coimmunoprecipitation of CB1 and D2 receptor was found in cellular models (Kearn et al. 2005) and resonance energy transfer (FRET) tecniques gave further evidence for the existence of CB1–D2 receptor heterodimers/receptor mosaics in cell lines in 2008 (Marcellino et al. 2008). Antagonistic CB1–D2 receptor interactions were demonstrated at the level of D2 recognition, where reduced D2 agonist affinity in ventral and dorsal striatum was found upon CB1 stimulation (Marcellino et al. 2008). It is of special interest that CB1 signaling appears to switch from a Gi-mediated inhibition of AC to a Gs/Golf-mediated activation of AC upon concurrent activation of both CB1 and D2 receptors in cellular models (Glass and Felder 1997; Kearn et al. 2005). In the ventral striatum, CB1 and D2 receptors are colocated in dendrites, terminals and local collaterals of the ventral striato-pallidal GABA neurons as well as in the cortico-striatal glutamate terminals (Pickel et al. 2006; Uchigashima et al. 2007). In the dorsal striatum, their colocation is mainly found in the terminals and local collaterals of dorsal striato-pallidal GABA neurons.
The antagonistic CB1–D2 receptor interaction may exist in CB1–D2 heterodimer/receptor mosaics located in different regions of the striato-pallidal GABA neurons (Maneuf et al. 1997). This antagonistic interaction may be part of an inhibitory feedback mechanism aimed to counteract strong D2 signaling. Evidence for this includes a marked increase in extracellular levels of anandamide following D2 agonist administration as well as D2 regulation of 2-arachidonoyl-glycerol (2-AG) signaling (Giuffrida et al. 1999; Piomelli 2003; Uchigashima et al. 2007). Therefore, the two major endocannabinoids are increased by D2 receptor activation. Via volume transmission and the antagonistic CB1–D2 receptor interaction, these increases in endocannabinoids makes possible the counteraction of excessive or aberrant D2 signaling, thus restoring the activity of striato-pallidal GABA neurons and reducing motor activation (Rodriguez de Fonseca et al. 1998; Fuxe et al. 2008; Marcellino et al. 2008).
In the glutamate terminals, our hypothesis is that CB1 receptor homodimers (Mackie 2005) may dominate over CB1–D2 receptor heteromers and lead to CB1-mediated inhibition of glutamate release (Piomelli 2003). In fact, in D2 containing striato-pallidal nerve cells, timing-dependent LTD is not able to develop after the blockade of CB1 receptors on the glutamate terminals, demonstrating that these receptors are required for the reduction of glutamate release (Shen et al. 2008). These CB1 receptors mediate the retrograde endocannabinoid signaling through a postsynaptic release step (Adermark and Lovinger 2007). In PD models, it has recently been shown that endocannabinoids can rescue striatal LTD in the indirect pathway demonstrated through the use of inhibitors of endocannabinoid degradation (Kreitzer and Malenka 2007). It was also found that combined treatment with D2 agonists and such inhibitors rescued motor deficits in the PD models used.
One explanation for these findings is that CB1 receptors mainly exist as homomers on the glutamate terminals and act to reduce glutamate release, thereby enhancing motor function when activated. Thus, CB1 may preferentially heteromerize with D2-long since D2-short are found on glutamate terminals (Centonze et al. 2004). Alternatively, the CB1 receptor in the heterodimer/receptor mosaic may have a lower affinity than CB1 homodimers. These are possible explanations for the indicated dominance of the CB1 homomer signaling on the glutamate terminals with inhibition of glutamate release and induction of LTD in the striato-pallidal GABA neurons.
The antagonistic CB1–D2 receptor interaction may also occur at the postjunctional level in the striato-pallidal GABA neurons where the CB1–D2 heterodimer/receptor mosaic may exist especially at the terminal level. This inhibitory feedback may only take place in the presence of a highly exaggerated D2 signaling resulting in a higher release of endocannabinoids. Such events may take place due to the postulated reduced affinity of the CB1 receptor in the heteromer versus the homomer. This inhibitory feedback may become effective not only by reducing D2 recognition and signaling, but also because the CB1 receptor in the CB1–D2 heterodimer/receptor mosaic may be coupled to Golf. This will further help switch the indirect pathway towards excitation, which can also involve increased glutamate release (Fuxe et al. 2008).
In recent years, indications have also been obtained for the existence of possible CB1–A2A–D2 receptor mosaics in the terminal parts of the dorsal striato-pallidal GABA neurons and in the dendritic regions of the ventral striato-pallidal GABA neurons and in cortico-striatal glutamate terminals (Rosin et al. 1998; Shindou et al. 2002; Pickel et al. 2006; Simola et al. 2006; Fuxe et al. 2008). In striatal slices, CB1 agonists can produce an increase in PKA-mediated DARPP-32 phosphorylation through activation of A2A receptors (Andersson et al. 2005b; Borgkvist et al. 2007). A2A–CB1 heterodimer/receptor mosaics have been demonstrated in cell lines in which CB1 signaling depends on A2A signaling (Carriba et al. 2007) and A2A antagonists can counteract the ability of CB1 agonists to antagonize the D2 agonist-induced motor activation (Marcellino et al. 2008). Furthermore, in the brain there exists a high molecular weight form of CB1 devoid of G proteins, which may represent a trimeric CB1–A2A–D2 receptor mosaic (Mukhopadhyay et al. 2000). Using sequential BRET–FRET, Franco et al. (Carriba et al. 2008) have this year in fact identified trimeric receptor mosaics of cannabinoid CB1, dopamine D2 and adenosine A2A receptors in living cells (Fig. 1).
Based on these findings, the hypothesis has been introduced that the molecular basis for the motor inhibition produced by CB1 agonists is through the specific target of these trimeric receptor mosaics. Within these receptor mosaics, you can set free the A2A signaling to AC from D2 inhibition via the antagonistic CB1–D2 receptor interactions reducing D2 signaling over Gi (Marcellino et al. 2008). Also in this trimeric receptor mosaic, the CB1 receptor may be coupled to Golf and not to Gi. These receptor mosaics probably represent important integrators of adenosine, DA and endocannabinoid signals and probably exist also in the cortico-striatal glutamate terminals.
The ventral striato-pallidal GABA pathway is of special interest, since here the CB1 receptors have been demonstrated also in the dendrites including the dendritic spines where they are colocated with A2A and D2 receptors (Pickel et al. 2006). Thus, CB agonists may more effectively inhibit D2 signaling in the ventral striato-pallidal GABA pathway than in the dorsal striato-pallidal GABA pathway, giving them a potential atypical antipsychotic profile. However, the CB1 agonists should preferentially target the CB1/D2 heterodimer/receptor mosaic and the trimeric A2A–D2–CB1 receptor mosaic in the ventral striato-pallidal GABA pathway and the cortico-striatal glutamate terminals, which probably exhibit a special CB1 pharmacology versus the CB1 homodimers/receptor mosaics. The CB1 agonist delta-9-tetrahydrocannabinol (Δ9-THC) may exacerbate psychotic symptoms in schizophrenia (D’Souza et al. 2005) because of a high affinity for CB1 homodimers/receptor mosaics. This would result in a reduction of glutamate release inter alia in the prefrontal cortex and the nucleus accumbens and reduced activity in the ventral striato-pallidal GABA pathway. Instead, cannabidiol, a weak CB1 antagonist appears to be an antipsychotic drug (Zuardi et al. 2006a, 2006b. Based on the present findings, it is postulated that this action of cannabidiol is produced by its ability to act as a preferential CB1 agonist at CB1/D2 heterodimers/receptor mosaics and at trimeric A2A–D2–CB1 receptor mosaics. In line with this hypothesis, it has been reported that in schizophrenic patients the anandamide cerebrospinal fluid (CSF) levels are inversely correlated to psychotic symptoms, probably due to the activation of the CB1 receptors in the mentioned D2 containing receptor mosaics (Leweke et al. 2007). For further discussion, see Fuxe et al. (2008).
Based on the likely existence of the CB1–D2–A2A receptor mosaic in the ventral striatum, it may be suggested that combined treatment with A2A agonists and CB1 agonists preferentially acting on this receptor mosaic may be an interesting novel strategy for treatment of schizophrenia, especially in combination with low doses of typical and atypical D2-like antagonists.
Putative NTS1–D2 heterodimers/receptor mosaics
In 1980, it was proposed that Neurotensin (NT) may be an endogenous antipsychotic based on antatomical and neurochemical evidence of NT/DA interactions (Nemeroff 1980). In agreement, low CSF NT concentrations have been found in a subset of drug-free schizophrenic patients (Breslin et al. 1994; Sharma et al. 1997). Furthermore, clinical improvement was associated with normalization of CSF NT, and low CSF NT concentrations were positively correlated with severity of thought disorder, deficit symptoms, etc. (Caceda et al. 2006). Also NT receptor agonists, similar to known antipsychotic drugs, prevent amphetamine and dizocilpine-induced disruption of prepulse inhibition of the startle response in the rat (Feifel et al. 1999).
Discovered antagonistic NTS1–D2 receptor interactions in postulated NTS1–D2 heterodimers/receptor mosaics in the ventral striatum have been repeatedly proposed to be the molecular mechanism involved in the postulated antipsychotic effects of NT (Agnati et al. 1983; Tanganelli et al. 1989; Fuxe et al. 1992; Diaz-Cabiale et al. 2002a; Antonelli et al. 2007; Ferraro et al. 2007). It should be noted, however, that NT shows antipsychotic-like behavioral effects in the nucleus accumbens, but stimulant-like effects in the VTA (Kalivas et al. 1981, 1984. The mechanism for such dual actions can be explained by the probable existence of antagonistic postjunctional NTS1–D2 interactions in the nucleus accumbens that reduce postjunctional D2–mediated signaling and antagonistic NTS1–D2 autoreceptor interactions on DA nerve cells in the VTA that increase the firing of meso-limbic DA neurons. This regional difference can also explain why systemic NTS1 receptor antagonists demonstrate antipsychotic-like effects, namely by preferentially blocking the NTS1–D2 autoreceptor interaction. This will in turn lead to an increased D2 autoreceptor function and reduced activity of meso-limbic DA neurons (Dobner et al. 2003; Ferraro et al. 2007)]. The antagonistic NTS1–D2 receptor interaction was first shown by the reduction of D2 receptor agonist affinity in striatal membrane preparations (Agnati et al. 1983; von Euler 1991) and in striatal sections (Li et al. 1994).
An in vivo functional correlate to the antagonistic NT effects on D2 recognition was obtained from microdialysis studies (Tanganelli et al. 1989, 1994; Fuxe et al. 1992; Antonelli et al. 2007, Ferraro et al. 2007). These experiments indicated for the first time the existence of a D2 autoreceptor heteromer on DA nerve terminals in the dorsal striatum, namely the NTS1–D2 autoreceptor heterodimer/receptor mosaic, where NT was able to restore DA release after D2 autoreceptor activation (Tanganelli et al. 1989; Diaz-Cabiale et al. 2002a). On the other hand, the postjunctional antagonistic NTS1/D2 receptor interaction in the dorsal striatum predominantly takes place in cortico-striatal glutamate terminals and results in an increase in glutamate release. The enhancement of glutamate transmission may be responsible for the subsequent activation of the dorsal striato-pallidal GABA neurons thus producing an increase in GABA outflow (Fuxe et al. 1992; Antonelli et al. 2007) and may contribute to the motor inhibition produced by NT treatment. This fact may underlie the use of NTS1 antagonists as a novel strategy for the treatment of PD (Antonelli et al. 2007). The D1 receptors are not modulated by the NT peptides and therefore a switch towards D1-mediated DA transmission is obtained, which is facilitated by the antagonistic NTS1–D2 autoreceptor interaction favoring DA release (Fuxe et al. 1992, Antonelli et al. 2007).
In contrast to the dorsal striatum, accumbal DA terminals did not exhibit a NTS1–D2 autoreceptor interaction (Tanganelli et al. 1994). Rather in the nucleus accumbens, the major postjunctional antagonistic NTS1–D2 receptor interaction is again linked to the glutamate terminals and leads to an enhancement of glutamate release in view of the inhibitory role D2 receptors play on glutamate release (Ferraro et al. 2007). This increase in glutamate outflow will thereby activate the ventral striato-pallidal GABA pathway and increase GABA outflow from terminals and collaterals that will reduce accumbal DA release (Tanganelli et al. 1994). In this way, NT agonists will more strongly reduce D2-mediated DA transmission in the nucleus accumbens, which will give them an atypical antipsychotic profile. The increase in glutamate release can also explain why NT peptides can block the D2 agonist-induced reduction of GABA release (Ferraro et al. 2007).
The mGluR2–5-HT2A heterodimer/receptor mosaic in the cerebral cortex
In 1968–1974, we published a series of papers demonstrating that d-lysergic acid diethylamide (d-LSD), hallucinogenic drugs of the indolalkylamine type, and hallucinogenic phenylethylamines produced reductions of 5-hydroxytryptamine (5-HT) turnover. This reduction of 5-HT turnover was associated with an increase in the extensor hind limb reflex activity of the acutely spinalized rat. The reflex activity was known to be induced through a postjunctional 5-HT receptor (Anden et al. 1968; Anden et al. 1971, 1974; Fuxe et al. 1972). In the pharmacological analysis, all of these hallucinogenic drugs were determined to be postsynaptic 5-HT receptor agonists. We proposed that the hallucinogenic actions of these compounds were produced via a postsynaptic activation of a 5-HT receptor in the brain, which produced a compensatory reduction in the firing of the 5-HT raphe neuron systems that in turn led to the reduced 5-HT turnover. These effects were blocked by methergoline, a putative 5-HT receptor antagonist (Fuxe et al. 1976).
Instead, Aghajanian et al. (1968) proposed that the hallucinogenic effects of d-LSD was produced by the activation of a presynaptic 5-HT receptor on the raphe nerve cells. The receptor was very sensitive to d-LSD and other hallucinogens, and thereby caused a reduction in the firing of the 5-HT neuron systems that mediated the hallucinogenic effects. The doses of hallucinogens we used to produce postjunctional 5-HT receptor activation were considerably higher. In line with these results, we observed, with Dr. Everitt, biphasic dose response curves with d-LSD and other hallucinogens on lordosis behavior of estrogen-primed ovariectomized rats (Fuxe et al. 1976). The ascending 5-HT neuron systems play an inhibitory role in sexual behavior (Everitt et al. 1975). Therefore, as expected, a low dose (5–20 μg/kg) of d-LSD was associated with an increase in sexual behavior, indicating a presynaptic 5-HT receptor activation. Inhibition was observed with a higher dose (40 μg/kg) indicating postsynaptic 5-HT receptor activation (Fuxe et al. 1976). However, no evidence was obtained to indicate that the hallucinogenic effects were abolished with increasing doses of hallucinogens. Hence the postsynaptic 5-HT receptor hypothesis was therefore maintained, especially since antidepressants were also shown to reduce the firing of the ascending 5-HT neuron system.
Today, the postjunctional 5-HT receptor has been identified as the 5-hydroxytrypamine receptor 2A (5-HT2A) receptor (Lieberman et al. 1998) and high densities of these binding sites have been found all over the cerebral cortex, especially in layer IV where the sensory inputs terminate (Palacios 1983; Cummins et al. 1987). Immunohistochemistry of 5-HT2A has indicated that 5-HT2A receptors are located extrasynaptically in large populations of pyramidal nerve cells, especially along the apical dendrites, and also in GABA interneurons distributed over the cerebral cortex. They are reached by 5-HT through volume transmission with a minimal distance of 7 μm between the 5-HT varicosities and the 5-HT2A receptors located on the apical dendrites of the pyramidal cells (Jansson et al. 2001).
Certain antipsychotic drugs, such as risperidone, have now been identified by their high affinity for the 5-HT2A receptor that results in a blockade of 5-HT2A activity (Lieberman et al. 1998, Colpaert 2003, Miyamoto et al. 2005). Psilocybine induces schizophrenia-like psychosis in humans through the activation of 5-HT2A receptors (Vollenweider et al. 1998). The effects of d-LSD and psilocybine and other hallucinogenic drugs appear to resemble core symptoms of schizophrenia (Colpaert 2003). Evidence indicates that hallucinogens act by recruiting specific cortical 5-HT2A receptor-mediated signaling pathways (Gonzalez-Maeso et al. 2007), which non-hallucinogenic 5-HT2A agonists cannot activate. This can also explain the observations that you can distinguish between hallucinogenic and non-hallucinogenic 5-HT2A agonists by transcriptome fingerprints (Gonzalez-Maeso et al. 2003).
It is a major discovery that a cortical mGluR2–5-HT2A heterodimer/receptor mosaic may have been identified and implicated in psychosis (Gonzalez-Maeso et al. 2008). In fact, metabotropic glutamate 2/3 receptors have been regarded as targets for antischizophrenic drugs (Aghajanian and Marek 2000; Marek 2004). In addition, a positive allosteric modulator of mGluR2, biphenyl-indanone A is effective in a hallucinogenic drug model of psychosis (Benneyworth et al. 2007). Furthermore, a randomized phase II clinical trial in schizophrenia using a mGluR2/3 agonist indicates their therapeutic potential in this disease (Patil et al. 2007).
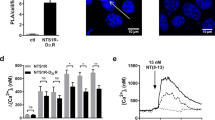
Fluorescent in situ hybridization (FISH) has demonstrated colocation of 5-HT2A/mGluR2 mRNA expression in nerve cell bodies of mouse somatosensory cortex and mouse cortical primary cultures. Also, specific 5-HT2A and mGluR2 heteromerization has been found in HEK-293 cells using bioluminescence resonance energy transfer (BRET2) techniques (Gonzalez-Maeso et al. 2008). The interface in the mGluR2–5-HT2A heteromer model introduced involves the TM4 and TM5 helices of the two receptors. It is of substantial interest that the hallucinogenic 2,5-dimethoxy-4-iodoamphetamine (DOI) stimulated [35S]GTPγS binding in primary cortical membranes when linked to either Gαi1, Gαi2 or Gαi3 is strongly reduced by the mGluR2/3 agonist LY379268 as is the hallucinogen-specific induction of egr-2 in mouse cortex (Gonzalez-Maeso et al. 2008). In contrast, the DOI-stimulated [35S]GTPγS binding when linked to Gαq/11 is only weakly affected by the mGluR2/3 agonist.
Thus, the mGluR2/3 agonist may produce their antipsychotic effects by targeting the mGluR2–5-HT2A heterodimer/receptor mosaic probably located in distinct pyramidal and granular cells and reduce the hallucinogen-specific Gi/o signaling via allosteric interactions over the receptor interface (Gonzalez-Maeso et al. 2008). The receptor–receptor interaction is also found at the agonist recognition level in this receptor mosaic. mGluR2/3 agonists increase the agonist affinity of the 5-HT2A receptor. This may be part of a complex allosteric mechanism within this receptor–receptor interaction, which increases 5-HT2A recognition and reduces its coupling to Gi/o.
In this exciting paper (Gonzalez-Maeso et al. 2008), it was also found that 5-HT2A receptor expression is increased in schizophrenia, a rise that is blocked by antipsychotic treatment. In parallel, the mGluR2 is reduced in schizophrenia and not affected by the antipsychotic treatment. These results clearly indicate that the disruption of sensory processing in schizophrenia may be related in part to pathological disturbances in the mGluR2–5-HT2A receptor mosaic in the cerebral cortex. Alterations in its receptor–receptor interactions may lead to increases in hallucinogen-specific signaling (Fig. 2).
Illustration of the possible preferential location of the mGluR2–5-HT2A heterodimer/receptor mosaic on the shafts of the apical dendrites of pyramidal nerve cells of the cerebral cortex. This receptor assembly may mainly have an extrasynaptic location and is reached by both glutamate and 5-HT through volume transmission within the extracellular space originating from the synaptic glutamate nerve terminals and from the varicosities of the 5-HT nerve terminal plexus. No 5-HT2A receptors exist on the dendritic spines of the pyramidal nerve cells (see Jansson et al. 2001). In the upper part, the hallucinogenic signaling of d-LSD is indicated as it targets the mGluR2–5-HT2A heterodimer/receptor mosaic. d-LSD can activate not only the Gq/11 but also the Gi/o-mediated hallucinogenic signaling of the 5-HT2A receptors (Gonzalez-Maeso et al. 2008). Via the inhibitory 5-HT2A–mGluR2 receptor interaction in the receptor assembly, the signaling of the mGluR2 is also reduced by d-LSD (Gonzalez-Maeso et al. 2008). The type of G protein involved in the mGluR2 signaling in this assembly is not known. Through glutamate activation of the mGluR2 receptor within this receptor assembly, the d-LSD-mediated hallucinogenic signaling over the Gi/o in the 5-HT2A receptor becomes blocked through an inhibitory mGluR2–5-HT2A receptor–receptor interaction at the G protein coupling level. The receptor interaction is complex, since at the same time the affinity of the 5-HT2A receptor becomes increased upon the activation of the mGluR2 (Gonzalez-Maeso et al. 2008) suggesting a major conformational change in the 5-HT2A receptor that results in altered G protein selection and an enhancement of 5-HT2A recognition
Conclusions
Receptor–receptor interactions within receptor heterodimer/receptor mosaics of different receptors give novel strategies for treatment of schizophrenia. One key region is the ventral striatum where the discovery of different types of D2 containing heterodimers/receptor mosaics offer new therapeutic possibilities to increase activity in the ventral striato-pallidal GABA pathway. This will help and restore the glutamate drive from the mediodorsal thalamic nucleus to the prefrontal cortex and other cortical regions apart from the present use of D2 antagonists/partial agonists. Thus, the existence of antagonistic A2A–D2, mGluR5–D2, CB1–D2 and NTS1–D2 receptor interactions in the corresponding heterodimers/receptor mosaics in the local circuits of the ventral striato-pallidal GABA neurons suggests the use of A2A, mGluR5, CB1 and NTS1 agonists as novel strategies for the treatment of schizophrenia. This may involve combined use of such agonists in low doses to antagonize D2 receptor function especially in view of the likely existence also of trimeric A2A–D2–CB1 and A2A–D2–mGluR5 receptor mosaics in these local circuits. This should reduce collateral effects, which may also be the case if also very low doses of D2 antagonists are added to the agonist treatments.
Different primary disturbances may exist in subpopulations of schizophrenic patients in these D2-containing receptor mosaics, modulating the activity of the ventral striato-pallidal GABA pathways. Therefore, the different agonists may be differentially active in subgroups of schizophrenic patients.
An important consequence of restoring the glutamate drive to the prefrontal cortex may be the increased activation of mGluR2 in the 5-HT2A–mGluR2 heterodimer/receptor mosaic in cortical neurons. This will reduce the hallucinogenic-specific Gi/o signaling and behavior over the 5-HT2A receptor with a reduction of primary disturbances in cortical sensory processing (Gonzalez-Maeso et al. 2008). In certain groups of patients, the primary disturbance may be in this receptor mosaic and therefore these schizophrenic patients may optimally respond to mGluR2 agonists and/or 5-HT2A antagonists for antipsychotic activity. Other groups of schizophrenic patients may show optimal therapeutic responses by targeting both the malfunctioning D2 receptor containing receptor mosaic in the ventral striatum and the 5-HT2A–mGluR2 heterodimer/receptor mosaic in the cerebral cortex.
The field of receptor mosaics of different types of receptors and their receptor–receptor interactions in networks of the ventral striatum and the prefrontal cortex offer novel strategies for treatment of different forms of schizophrenia.
References
Adermark L, Lovinger DM (2007) Retrograde endocannabinoid signaling at striatal synapses requires a regulated postsynaptic release step. Proc Natl Acad Sci USA 104:20564–20569
Aghajanian GK, Marek GJ (2000) Serotonin model of schizophrenia: emerging role of glutamate mechanisms. Brain Res Brain Res Rev 31:302–312
Aghajanian GK, Foote WE, Sheard MH (1968) Lysergic acid diethylamide: sensitive neuronal units in the midbrain raphe. Science 161:706–708
Agnati LF, Fuxe K, Benfenati F, Battistini N (1983) Neurotensin in vitro markedly reduces the affinity in subcortical limbic 3H-N-propylnorapomorphine binding sites. Acta Physiol Scand 119:459–461
Agnati LF, Ferre S, Lluis C, Franco R, Fuxe K (2003) Molecular mechanisms and therapeutical implications of intramembrane receptor/receptor interactions among heptahelical receptors with examples from the striatopallidal GABA neurons. Pharmacol Rev 55:509–550
Agnati LF, Ferre S, Genedani S et al (2006) Allosteric modulation of dopamine D2 receptors by homocysteine. J Proteome Res 5:3077–3083
Agnati L, Guidolin D, Genedani S, Arhem P, Forni A, Andreoli N, Fuxe K (2007a) Role of cooperativity in protein folding and protein mosaic assemblage: relevance for protein conformational diseases. Curr Protein Pept Sci 8:460–470
Agnati LF, Guidolin D, Leo G, Fuxe K (2007b) A boolean network modelling of receptor mosaics relevance of topology and cooperativity. J Neural Transm 114:77–92
Agnati LF, Leo G, Genedani S, Andreoli N, Marcellino D, Woods A, Piron L, Guidolin D, Fuxe K (2008) Structural plasticity in G-protein coupled receptors as demonstrated by the allosteric actions of homocysteine and computer-assisted analysis of disordered domains. Brain Res Rev 58:459–474
Alexander GE, Crutcher MD, DeLong MR (1990) Basal ganglia–thalamocortical circuits: parallel substrates for motor, oculomotor, “prefrontal” and “limbic” functions. Prog Brain Res 85:119–146
Anden NE, Dahlstroem A, Fuxe K, Larsson K, Olson L, Ungerstedt U (1966) Ascending monoamine neurons to the telencephalon and diencephalon. Acta Physiol Scand 67:313–326
Anden NE, Corrodi H, Fuxe K, Hokfelt T (1968) Evidence for a central 5-hydroxytryptamine receptor stimulation by lysergic acid diethylamide. Br J Pharmacol 34:1–7
Anden NE, Corrodi H, Fuxe K (1971) Hallucinogenic drugs of the indolealkylamine type and central monoamine neurons. J Pharmacol Exp Ther 179:236–249
Anden NE, Corrodi H, Fuxe K, Meek JL (1974) Hallucinogenic phenylethylamines: interactions with serotonin turnover and receptors. Eur J Pharmacol 25:176–184
Andersen MB, Fuxe K, Werge T, Gerlach J (2002) The adenosine A2A receptor agonist CGS 21680 exhibits antipsychotic-like activity in Cebus apella monkeys. Behav Pharmacol 13:639–644
Andersson M, Terasmaa A, Fuxe K, Stromberg I (2005a) Subchronic haloperidol increases CB(1) receptor binding and G protein coupling in discrete regions of the basal ganglia. J Neurosci Res 82:264–272
Andersson M, Usiello A, Borgkvist A et al (2005b) Cannabinoid action depends on phosphorylation of dopamine- and cAMP-regulated phosphoprotein of 32 kDa at the protein kinase A site in striatal projection neurons. J Neurosci 25:8432–8438
Antonelli T, Fuxe K, Tomasini MC, Mazzoni E, Agnati LF, Tanganelli S, Ferraro L (2007) Neurotensin receptor mechanisms and its modulation of glutamate transmission in the brain: relevance for neurodegenerative diseases and their treatment. Prog Neurobiol 83:92–109
Bateup HS, Svenningsson P, Kuroiwa M, Gong S, Nishi A, Heintz N, Greengard P (2008) Cell type-specific regulation of DARPP-32 phosphorylation by psychostimulant and antipsychotic drugs. Nat Neurosci 11:932–939
Belin D, Everitt BJ (2008) Cocaine seeking habits depend upon dopamine-dependent serial connectivity linking the ventral with the dorsal striatum. Neuron 57:432–441
Benneyworth MA, Xiang Z, Smith RL, Garcia EE, Conn PJ, Sanders-Bush E (2007) A selective positive allosteric modulator of metabotropic glutamate receptor subtype 2 blocks a hallucinogenic drug model of psychosis. Mol Pharmacol 72:477–484
Berger B, Thierry AM, Tassin JP, Moyne MA (1976) Dopaminergic innervation of the rat prefrontal cortex: a fluorescence histochemical study. Brain Res 106:133–145
Bernstein HG, Krause S, Krell D et al (2007) Strongly reduced number of parvalbumin-immunoreactive projection neurons in the mammillary bodies in schizophrenia: further evidence for limbic neuropathology. Ann N Y Acad Sci 1096:120–127
Borgkvist A, Marcellino D, Fuxe K, Greengard P, Fisone G (2008) Regulation of DARPP-32 phosphorylation by Delta(9)-tetrahydrocannabinol. Neuropharmacology 54(1):31–35
Breslin NA, Suddath RL, Bissette G, Nemeroff CB, Lowrimore P, Weinberger DR (1994) CSF concentrations of neurotensin in schizophrenia: an investigation of clinical and biochemical correlates. Schizophr Res 12:35–41
Caceda R, Kinkead B, Nemeroff CB (2006) Neurotensin: role in psychiatric and neurological diseases. Peptides 27:2385–2404
Canals M, Marcellino D, Fanelli F et al (2003) Adenosine A2A-dopamine D2 receptor-receptor heteromerization: qualitative and quantitative assessment by fluorescence and bioluminescence energy transfer. J Biol Chem 278:46741–46749
Carlsson A (1988) The current status of the dopamine hypothesis of schizophrenia. Neuropsychopharmacology 1:179–186
Carlsson A, Carlsson ML (2008) Adaptive properties and heterogeneity of dopamine D(2) receptors: pharmacological implications. Brain Res Rev 58:374–378
Carlsson A, Lindqvist M (1963) Effect Of chlorpromazine or haloperidol on formation of 3 methoxytyramine and normetanephrine in mouse brain. Acta Pharmacol Toxicol (Copenh) 20:140–144
Carriba P, Ortiz O, Patkar K et al (2007) Striatal adenosine A(2A) and cannabinoid CB(1) receptors form functional heteromeric complexes that mediate the motor effects of cannabinoids. Neuropsychopharmacology 32(11):2249–2259
Carriba P, Navarro G, Ciruela F et al (2008) Detection of heteromerization of more than two proteins by sequential BRET–FRET. Nat Methods 5:727–733
Centonze D, Battista N, Rossi S, Mercuri NB, Finazzi-Agro A, Bernardi G, Calabresi P, Maccarrone M (2004) A critical interaction between dopamine D2 receptors and endocannabinoids mediates the effects of cocaine on striatal gabaergic transmission. Neuropsychopharmacology 29:1488–1497
Ciruela F, Burgueno J, Casado V et al (2004) Combining mass spectrometry and pull-down techniques for the study of receptor heteromerization: dDirect epitope–epitope electrostatic interactions between adenosine A2A and dopamine D2 receptors. Anal Chem 76:5354–5363
Colpaert FC (2003) Discovering risperidone: the LSD model of psychopathology. Nat Rev Drug Discov 2:315–320
Conn PJ, Battaglia G, Marino MJ, Nicoletti F (2005) Metabotropic glutamate receptors in the basal ganglia motor circuit. Nat Rev Neurosci 6:787–798
Cullen TJ, Walker MA, Parkinson N, Craven R, Crow TJ, Esiri MM, Harrison PJ (2003) A postmortem study of the mediodorsal nucleus of the thalamus in schizophrenia. Schizophr Res 60:157–166
Cummins JT, von Euler G, Fuxe K, Ogren SO, Agnati LF (1987) Chronic imipramine treatment reduces (+)2-[125I]iodolysergic acid, diethylamide but not 125I-neuropeptide Y binding in layer IV of rat cerebral cortex. Neurosci Lett 75:152–156
D’Souza DC, Abi-Saab WM, Madonick S, Forselius-Bielen K, Doersch A, Braley G, Gueorguieva R, Cooper TB, Krystal JH (2005) Delta-9-tetrahydrocannabinol effects in schizophrenia: implications for cognition, psychosis, and addiction. Biol Psychiatry 57:594–608
Dahlstroem A, Fuxe K (1964) Evidence for the existence of monoamine-containing neurons in the central nervous system. I. Demonstration of monoamines in the cell bodies of brain stem neurons. Acta Physiol Scand Suppl Suppl 232:231–255
Danos P (2004) Pathology of the thalamus and schizophrenia: an overview. Fortschr Neurol Psychiatr 72:621–634
Danos P, Baumann B, Kramer A, Bernstein HG, Stauch R, Krell D, Falkai P, Bogerts B (2003) Volumes of association thalamic nuclei in schizophrenia: a postmortem study. Schizophr Res 60:141–155
Danos P, Schmidt A, Baumann B, Bernstein HG, Northoff G, Stauch R, Krell D, Bogerts B (2005) Volume and neuron number of the mediodorsal thalamic nucleus in schizophrenia: a replication study. Psychiatry Res 140:281–289
Del Arco A, Mora F, Mohammed AH, Fuxe K (2007) Stimulation of D2 receptors in the prefrontal cortex reduces PCP-induced hyperactivity, acetylcholine release and dopamine metabolism in the nucleus accumbens. J Neural Transm 114:185–193
Diaz J, Pilon C, Le Foll B, Gros C, Triller A, Schwartz JC, Sokoloff P (2000) Dopamine D3 receptors expressed by all mesencephalic dopamine neurons. J Neurosci 20:8677–8684
Diaz-Cabiale Z, Fuxe K, Narvaez JA, Finetti S, Antonelli T, Tanganelli S, Ferraro L (2002a) Neurotensin-induced modulation of dopamine D2 receptors and their function in rat striatum: counteraction by a NTR1-like receptor antagonist. Neuroreport 13:763–766
Diaz-Cabiale Z, Vivo M, Del Arco A et al (2002b) Metabotropic glutamate mGlu5 receptor-mediated modulation of the ventral striopallidal GABA pathway in rats: interactions with adenosine A(2A) and dopamine D(2) receptors. Neurosci Lett 324:154–158
Dobner PR, Deutch AY, Fadel J (2003) Neurotensin: dual roles in psychostimulant and antipsychotic drug responses. Life Sci 73:801–811
Dorph-Petersen KA, Pierri JN, Sun Z, Sampson AR, Lewis DA (2004) Stereological analysis of the mediodorsal thalamic nucleus in schizophrenia: volume, neuron number, and cell types. J Comp Neurol 472:449–462
Everitt BJ, Fuxe K, Hokfelt FT, Jonsson G (1975) Role of monoamines in the control by hormones of sexual receptivity in the female rat. J Comp Physiol Psychol 89:556–572
Feifel D, Reza TL, Wustrow DJ, Davis MD (1999) Novel antipsychotic-like effects on prepulse inhibition of startle produced by a neurotensin agonist. J Pharmacol Exp Ther 288:710–713
Ferraro L, Tomasini MC, Fuxe K, Agnati LF, Mazza R, Tanganelli S, Antonelli T (2007) Mesolimbic dopamine and cortico-accumbens glutamate afferents as major targets for the regulation of the ventral striato-pallidal GABA pathways by neurotensin peptides. Brain Res Rev 55:144–154
Ferraro L, Tomasini MC, Mazza R, Fuxe K, Fournier J, Tanganelli S, Antonelli T (2008) Neurotensin receptors as modulators of glutamatergic transmission. Brain Res Rev 58:365–373
Ferre S, von Euler G, Johansson B, Fredholm BB, Fuxe K (1991) Stimulation of high-affinity adenosine A2 receptors decreases the affinity of dopamine D2 receptors in rat striatal membranes. Proc Natl Acad Sci USA 88:7238–7241
Ferre S, O’Connor WT, Snaprud P, Ungerstedt U, Fuxe K (1994) Antagonistic interaction between adenosine A2A receptors and dopamine D2 receptors in the ventral striopallidal system: implications for the treatment of schizophrenia. Neuroscience 63:765–773
Ferre S, Popoli P, Rimondini R, Reggio R, Kehr J, Fuxe K (1999) Adenosine A2A and group I metabotropic glutamate receptors synergistically modulate the binding characteristics of dopamine D2 receptors in the rat striatum. Neuropharmacology 38:129–140
Ferre S, Karcz-Kubicha M, Hope BT et al (2002) Synergistic interaction between adenosine A2A and glutamate mGlu5 receptors: implications for striatal neuronal function. Proc Natl Acad Sci USA 99:11940–11945
Ferre S, Ciruela F, Canals M et al (2004) Adenosine A2A-dopamine D2 receptor-receptor heteromers: targets for neuro-psychiatric disorders. Parkinsonism Relat Disord 10:265–271
Ferre S, Agnati LF, Ciruela F, Lluis C, Woods AS, Fuxe K, Franco R (2007) Neurotransmitter receptor heteromers and their integrative role in ‘local modules’: The striatal spine module. Brain Res Rev 55:55–67
Fuxe K (1965) Evidence for the existence of monoamine neurons in the central nervous system. IV. Distribution of monoamine nerve terminals in the central nervous system. Acta Physiol Scand Suppl Suppl 247:237
Fuxe K (1970) Biological and pharmacological theories. In: Bobon DP, Janssen PAJ, Bobon J (eds) The neuroleptics. S. Karger, Basel, pp 121–122
Fuxe K, Holmstedt B, Jonsson G (1972) Effects of 5-methoxy-N, N-dimethyltryptamine on central monoamine neurons. Eur J Pharmacol 19:25–34
Fuxe K, Everitt BJ, Agnati L, Fredholm BB, Jonsson G (1976) On the biochemistry and pharmacology of hallucinogens. In: Kemali D, Bartholini G, Richter D (eds) Schizophrenia today. Pergamon, Oxford, pp 135–157
Fuxe K, Andersson K, Schwarcz R (1979) Studies on different types of DA nerve terminals in the forebrain and their possible interactions with hormones and with neurons containing GABA, glutamate and opiod peptides. In: Poirier LJ, Sourkes TL, Bedard PJ et al (eds) Advances in neurology, vol 24. Raven, New York, pp 199–214
Fuxe K, Celani MF, Martire M, Zini I, Zoli M, Agnati LF (1984) l-Glutamate reduces the affinity of [3H]N-propylnorapomorphine binding sites in striatal membranes. Eur J Pharmacol 100:127–130
Fuxe K, O’Connor WT, Antonelli T, Osborne PG, Tanganelli S, Agnati LF, Ungerstedt U (1992) Evidence for a substrate of neuronal plasticity based on pre- and postsynaptic neurotensin–dopamine receptor interactions in the neostriatum. Proc Natl Acad Sci USA 89:5591–5595
Fuxe K, Ferre S, Snaprud P, von Euler G, Johansson B, Fredholm BB (1993) Antagonistic A2A/D2 receptor interactions as a basis for adenosine/dopamine interactionns in the central nervous system. Drug Dev Res 28:374–380
Fuxe K, Agnati LF, Jacobsen K et al (2003a) Receptor heteromerization in adenosine A2A receptor signaling: relevance for striatal function and Parkinson’s disease. Neurology 61:S19–S23
Fuxe K, Ferre S, Woods A, Rivera A, Hoistad M, Franco R, Kehr J, Agnati L (2003b) Novel strategies for the treatment of Parkinson’s disease: focus on receptor–receptor interactions in the basal ganglia. In: Kehr J, Fuxe K, Ungerstedt U, Svensson T (eds) Monitoring molecules in neuroscience. Karolinska University Press, Stockholm, pp 199–202
Fuxe K, Ferre S, Canals M et al (2005) Adenosine A2A and dopamine D2 heteromeric receptor complexes and their function. J Mol Neurosci 26:209–220
Fuxe K, Canals M, Torvinen M et al (2007a) Intramembrane receptor–receptor interactions: a novel principle in molecular medicine. J Neural Transm 114:49–75
Fuxe K, Dahlstrom A, Hoistad M et al (2007b) From the Golgi-Cajal mapping to the transmitter-based characterization of the neuronal networks leading to two modes of brain communication: wiring and volume transmission. Brain Res Rev 55:17–54
Fuxe K, Ferre S, Genedani S, Franco R, Agnati LF (2007c) Adenosine receptor–dopamine receptor interactions in the basal ganglia and their relevance for brain function. Physiol Behav 92:210–217
Fuxe K, Marcellino D, Genedani S, Agnati L (2007d) Adenosine A(2A) receptors, dopamine D(2) receptors and their interactions in Parkinson’s disease. Mov Disord 22:1990–2017
Fuxe K, Marcellino D, Rivera A et al (2008) Receptor–receptor interactions within receptor mosaics: impact on neuropsychopharmacology. Brain Res Rev 58:415–452
Gandia J, Galino J, Amaral OB, Soriano A, Lluis C, Franco R, Ciruela F (2008) Detection of higher-order G protein-coupled receptor oligomers by a combined BRET–BiFC technique. FEBS Lett 582:2979–2984
Giuffrida A, Parsons LH, Kerr TM, Rodriguez de Fonseca F, Navarro M, Piomelli D (1999) Dopamine activation of endogenous cannabinoid signaling in dorsal striatum. Nat Neurosci 2:358–363
Glass M, Felder CC (1997) Concurrent stimulation of cannabinoid CB1 and dopamine D2 receptors augments cAMP accumulation in striatal neurons: evidence for a Gs linkage to the CB1 receptor. J Neurosci 17:5327–5333
Gonzalez-Maeso J, Yuen T, Ebersole BJ et al (2003) Transcriptome fingerprints distinguish hallucinogenic and nonhallucinogenic 5-hydroxytryptamine 2A receptor agonist effects in mouse somatosensory cortex. J Neurosci 23:8836–8843
Gonzalez-Maeso J, Weisstaub NV, Zhou M et al (2007) Hallucinogens recruit specific cortical 5-HT(2A) receptor-mediated signaling pathways to affect behavior. Neuron 53:439–452
Gonzalez-Maeso J, Ang RL, Yuen T et al (2008) Identification of a serotonin/glutamate receptor complex implicated in psychosis. Nature 452:93–97
Gozes I (2005) Receptor–receptor interactions among heptaspanning membrane receptors: from structure to function. In: Wenner-Gren Foundation symposium on receptor–receptor interactions among heptaspanning membrane receptors: from structure to function, vol, special issue of J Mol Neurosci 26 (Nos. 2, 3). Humana press, Stockholm, pp 109–305
Grace AA (2000) Gating of information flow within the limbic system and the pathophysiology of schizophrenia. Brain Res Brain Res Rev 31:330–341
Groenewegen HJ, Trimble M (2007) The ventral striatum as an interface between the limbic and motor systems. CNS Spectr 12:887–892
Groenewegen HJ, Berendse HW, Haber SN (1993) Organization of the output of the ventral striatopallidal system in the rat: ventral pallidal efferents. Neuroscience 57:113–142
Groenewegen HJ, Wright CI, Beijer AV (1996) The nucleus accumbens: gateway for limbic structures to reach the motor system? Prog Brain Res 107:485–511
Guo W, Urizar E, Kralikova M, Mobarec JC, Shi L, Filizola M, Javitch JA (2008) Dopamine D2 receptors form higher order oligomers at physiological expression levels. EMBO J 27:2293–2304
Gurevich EV, Joyce JN (1999) Distribution of dopamine D3 receptor expressing neurons in the human forebrain: comparison with D2 receptor expressing neurons. Neuropsychopharmacology 20:60–80
Haber SN, Fudge JL, McFarland NR (2000) Striatonigrostriatal pathways in primates form an ascending spiral from the shell to the dorsolateral striatum. J Neurosci 20:2369–2382
Hakansson K, Galdi S, Hendrick J, Snyder G, Greengard P, Fisone G (2006) Regulation of phosphorylation of the GluR1 AMPA receptor by dopamine D2 receptors. J Neurochem 96:482–488
Heimer L (2000) Basal forebrain in the context of schizophrenia. Brain Res Brain Res Rev 31:205–235
Hernandez-Lopez S, Tkatch T, Perez-Garci E, Galarraga E, Bargas J, Hamm H, Surmeier DJ (2000) D2 dopamine receptors in striatal medium spiny neurons reduce L-type Ca2+ currents and excitability via a novel PLC[beta]1-IP3-calcineurin-signaling cascade. J Neurosci 20:8987–8995
Hillion J, Canals M, Torvinen M et al (2002) Coaggregation, cointernalization, and codesensitization of adenosine A2A receptors and dopamine D2 receptors. J Biol Chem 277:18091–18097
Jansson A, Tinner B, Bancila M, Verge D, Steinbusch HW, Agnati LF, Fuxe K (2001) Relationships of 5-hydroxytryptamine immunoreactive terminal-like varicosities to 5-hydroxytryptamine-2A receptor-immunoreactive neuronal processes in the rat forebrain. J Chem Neuroanat 22:185–203
Joyce JN, Gurevich EV (1999) D3 receptors and the actions of neuroleptics in the ventral striatopallidal system of schizophrenics. Ann N Y Acad Sci 877:595–613
Joyce JN, Millan MJ (2005) Dopamine D3 receptor antagonists as therapeutic agents. Drug Discov Today 10:917–925
Kalivas PW, Nemeroff CB, Prange AJ Jr (1981) Increase in spontaneous motor activity following infusion of neurotensin into the ventral tegmental area. Brain Res 229:525–529
Kalivas PW, Nemeroff CB, Prange AJ Jr (1984) Neurotensin microinjection into the nucleus accumbens antagonizes dopamine-induced increase in locomotion and rearing. Neuroscience 11:919–930
Kamiya T, Saitoh O, Yoshioka K, Nakata H (2003) Oligomerization of adenosine A2A and dopamine D2 receptors in living cells. Biochem Biophys Res Commun 306:544–549
Kearn CS, Blake-Palmer K, Daniel E, Mackie K, Glass M (2005) Concurrent stimulation of cannabinoid CB1 and dopamine D2 receptors enhances heterodimer formation: a mechanism for receptor cross-talk? Mol Pharmacol 67:1697–1704
Khan ZU, Mrzljak L, Gutierrez A, de la Calle A, Goldman-Rakic PS (1998) Prominence of the dopamine D2 short isoform in dopaminergic pathways. Proc Natl Acad Sci USA 95:7731–7736
Kinney GG, Burno M, Campbell UC, Hernandez LM, Rodriguez D, Bristow LJ, Conn PJ (2003) Metabotropic glutamate subtype 5 receptors modulate locomotor activity and sensorimotor gating in rodents. J Pharmacol Exp Ther 306:116–123
Kinney GG, O’Brien JA, Lemaire W et al (2005) A novel selective positive allosteric modulator of metabotropic glutamate receptor subtype 5 has in vivo activity and antipsychotic-like effects in rat behavioral models. J Pharmacol Exp Ther 313:199–206
Kreitzer AC, Malenka RC (2007) Endocannabinoid-mediated rescue of striatal LTD and motor deficits in Parkinson’s disease models. Nature 445:643–647
Leweke FM, Giuffrida A, Koethe D et al (2007) Anandamide levels in cerebrospinal fluid of first-episode schizophrenic patients: impact of cannabis use. Schizophr Res 94:29–36
Li XM, Hedlund PB, Fuxe K (1994) Strong effects of NT/NN peptides on DA D2 receptors in rat neostriatal sections. Neuroreport 5:1621–1624
Lieberman JA, Mailman RB, Duncan G, Sikich L, Chakos M, Nichols DE, Kraus JE (1998) Serotonergic basis of antipsychotic drug effects in schizophrenia. Biol Psychiatry 44:1099–1117
Liu XY, Chu XP, Mao LM et al (2006) Modulation of D2R–NR2B interactions in response to cocaine. Neuron 52:897–909
Mackie K (2005) Cannabinoid receptor homo- and heterodimerization. Life Sci 77:1667–1673
Maggio R, Scarselli M, Novi F, Millan MJ, Corsini GU (2003) Potent activation of dopamine D3/D2 heterodimers by the antiparkinsonian agents, S32504, pramipexole and ropinirole. J Neurochem 87:631–641
Maggio R, Novi F, Scarselli M, Corsini GU (2005) The impact of G-protein-coupled receptor hetero-oligomerization on function and pharmacology. FEBS J 272:2939–2946
Maneuf YP, Crossman AR, Brotchie JM (1997) The cannabinoid receptor agonist WIN 55, 212–2 reduces D2, but not D1, dopamine receptor-mediated alleviation of akinesia in the reserpine-treated rat model of Parkinson’s disease. Exp Neurol 148:265–270
Marcellino D, Carriba P, Filip M et al (2008) Antagonistic cannabinoid CB1/dopamine D2 receptor interactions in striatal CB1/D2 heteromers: a combined neurochemical and behavioral analysis. Neuropharmacology 54:815–823
Marek GJ (2004) Metabotropic glutamate 2/3 receptors as drug targets. Curr Opin Pharmacol 4:18–22
Marshall FH (2001) Heterodimerization of G-protein-coupled receptors in the CNS. Curr Opin Pharmacol 1:40–44
Marshall FH (2005) Is the GABA B heterodimer a good drug target? J Mol Neurosci 26:169–176
Maurel D, Comps-Agrar L, Brock C et al (2008) Cell-surface protein–protein interaction analysis with time-resolved FRET and snap-tag technologies: application to GPCR oligomerization. Nat Methods 5:561–567
Millan MJ, Gobert A, Newman-Tancredi A, Lejeune F, Cussac D, Rivet JM, Audinot V, Dubuffet T, Lavielle G (2000) S33084, a novel, potent, selective, and competitive antagonist at dopamine D(3)-receptors: I. Receptorial, electrophysiological and neurochemical profile compared with GR218, 231 and L741, 626. J Pharmacol Exp Ther 293:1048–1062
Milligan G, Smith NJ (2007) Allosteric modulation of heterodimeric G-protein-coupled receptors. Trends Pharmacol Sci 28:615–620
Miyamoto S, Duncan GE, Marx CE, Lieberman JA (2005) Treatments for schizophrenia: a critical review of pharmacology and mechanisms of action of antipsychotic drugs. Mol Psychiatry 10:79–104
Mogenson GJ, Jones DL, Yim CY (1980) From motivation to action: functional interface between the limbic system and the motor system. Prog Neurobiol 14:69–97
Mukhopadhyay S, McIntosh HH, Houston DB, Howlett AC (2000) The CB(1) cannabinoid receptor juxtamembrane C-terminal peptide confers activation to specific G proteins in brain. Mol Pharmacol 57:162–170
Nemeroff CB (1980) Neurotensin: perchance an endogenous neuroleptic? Biol Psychiatry 15:283–302
Nimchinsky EA, Hof PR, Janssen WG, Morrison JH, Schmauss C (1997) Expression of dopamine D3 receptor dimers and tetramers in brain and in transfected cells. J Biol Chem 272:29229–29237
Nishi A, Liu F, Matsuyama S, Hamada M, Higashi H, Nairn AC, Greengard P (2003) Metabotropic mGlu5 receptors regulate adenosine A2A receptor signaling. Proc Natl Acad Sci USA 100:1322–1327
Novi F, Millan MJ, Corsini GU, Maggio R (2007) Partial agonist actions of aripiprazole and the candidate antipsychotics S33592, bifeprunox, N-desmethylclozapine and preclamol at dopamine D(2L) receptors are modified by co-transfection of D(3) receptors: potential role of heterodimer formation. J Neurochem 102:1410–1424
Pakkenberg B (1990) Pronounced reduction of total neuron number in mediodorsal thalamic nucleus and nucleus accumbens in schizophrenics. Arch Gen Psychiatry 47:1023–1028
Palacios JM (1983) Quantitative receptor autoradiography: application to the study of multiple serotonin receptors in rat cortex. Adv Biochem Psychopharmacol 37:455–463
Patil ST, Zhang L, Martenyi F et al (2007) Activation of mGlu2/3 receptors as a new approach to treat schizophrenia: a randomized Phase 2 clinical trial. Nat Med 13:1102–1107
Pickel VM, Chan J, Kearn CS, Mackie K (2006) Targeting dopamine D2 and cannabinoid-1 (CB1) receptors in rat nucleus accumbens. J Comp Neurol 495:299–313
Piomelli D (2003) The molecular logic of endocannabinoid signalling. Nat Rev Neurosci 4:873–884
Popken GJ, Bunney WE Jr, Potkin SG, Jones EG (2000) Subnucleus-specific loss of neurons in medial thalamus of schizophrenics. Proc Natl Acad Sci USA 97:9276–9280
Popoli P, Pezzola A, Torvinen M, Reggio R, Pintor A, Scarchilli L, Fuxe K, Ferre S (2001) The selective mGlu(5) receptor agonist CHPG inhibits quinpirole-induced turning in 6-hydroxydopamine-lesioned rats and modulates the binding characteristics of dopamine D(2) receptors in the rat striatum: interactions with adenosine A(2a) receptors. Neuropsychopharmacology 25:505–513
Rimondini R, Ferre S, Ogren SO, Fuxe K (1997) Adenosine A2A agonists: a potential new type of atypical antipsychotic. Neuropsychopharmacology 17:82–91
Rodriguez de Fonseca F, Del Arco I, Martin-Calderon JL, Gorriti MA, Navarro M (1998) Role of the endogenous cannabinoid system in the regulation of motor activity. Neurobiol Dis 5:483–501
Rosin DL, Robeva A, Woodard RL, Guyenet PG, Linden J (1998) Immunohistochemical localization of adenosine A2A receptors in the rat central nervous system. J Comp Neurol 401:163–186
Scarselli M, Novi F, Schallmach E et al (2001) D2/D3 dopamine receptor heterodimers exhibit unique functional properties. J Biol Chem 276:30308–30314
Schultz W (2002) Getting formal with dopamine and reward. Neuron 36:241–263
Schwartz JC, Diaz J, Pilon C, Sokoloff P (2000) Possible implications of the dopamine D(3) receptor in schizophrenia and in antipsychotic drug actions. Brain Res Brain Res Rev 31:277–287
Schwarzschild MA, Agnati L, Fuxe K, Chen JF, Morelli M (2006) Targeting adenosine A(2A) receptors in Parkinson’s disease. Trends Neurosci 29:647–654
Seeman P, Schwarz J, Chen JF et al (2006) Psychosis pathways converge via D2high dopamine receptors. Synapse 60:319–346
Sharma RP, Janicak PG, Bissette G, Nemeroff CB (1997) CSF neurotensin concentrations and antipsychotic treatment in schizophrenia and schizoaffective disorder. Am J Psychiatry 154:1019–1021
Shen W, Flajolet M, Greengard P, Surmeier DJ (2008) Dichotomous dopaminergic control of striatal synaptic plasticity. Science 321:848–851
Shindou T, Nonaka H, Richardson PJ, Mori A, Kase H, Ichimura M (2002) Presynaptic adenosine A2A receptors enhance GABAergic synaptic transmission via a cyclic AMP dependent mechanism in the rat globus pallidus. Br J Pharmacol 136:296–302
Simola N, Fenu S, Baraldi PG, Tabrizi MA, Morelli M (2006) Involvement of globus pallidus in the antiparkinsonian effects of adenosine A(2A) receptor antagonists. Exp Neurol 202:255–257
Sokoloff P, Diaz J, Le Foll B, Guillin O, Leriche L, Bezard E, Gross C (2006) The dopamine D3 receptor: a therapeutic target for the treatment of neuropsychiatric disorders. CNS Neurol Disord Drug Targets 5:25–43
Stahl SM (2007a) Beyond the dopamine hypothesis to the NMDA glutamate receptor hypofunction hypothesis of schizophrenia. CNS Spectr 12:265–268
Stahl SM (2007b) The genetics of schizophrenia converge upon the NMDA glutamate receptor. CNS Spectr 12:583–588
Stahl SM (2008) Do dopamine partial agonists have partial efficacy as antipsychotics? CNS Spectr 13:279–282
Sturm V, Lenartz D, Koulousakis A, Treuer H, Herholz K, Klein JC, Klosterkotter J (2003) The nucleus accumbens: a target for deep brain stimulation in obsessive-compulsive- and anxiety-disorders. J Chem Neuroanat 26:293–299
Surmeier DJ, Song WJ, Yan Z (1996) Coordinated expression of dopamine receptors in neostriatal medium spiny neurons. J Neurosci 16:6579–6591
Surmeier DJ, Ding J, Day M, Wang Z, Shen W (2007) D1 and D2 dopamine-receptor modulation of striatal glutamatergic signaling in striatal medium spiny neurons. Trends Neurosci 30:228–235
Svensson TH (2000) Dysfunctional brain dopamine systems induced by psychotomimetic NMDA-receptor antagonists and the effects of antipsychotic drugs. Brain Res Brain Res Rev 31:320–329
Tamminga CA, Carlsson A (2002) Partial dopamine agonists and dopaminergic stabilizers, in the treatment of psychosis. Curr Drug Targets CNS Neurol Disord 1:141–147
Tanganelli S, von Euler G, Fuxe K, Agnati LF, Ungerstedt U (1989) Neurotensin counteracts apomorphine-induced inhibition of dopamine release as studied by microdialysis in rat neostriatum. Brain Res 502:319–324
Tanganelli S, O’Connor WT, Ferraro L, Bianchi C, Beani L, Ungerstedt U, Fuxe K (1994) Facilitation of GABA release by neurotensin is associated with a reduction of dopamine release in rat nucleus accumbens. Neuroscience 60:649–657
Torvinen M, Marcellino D, Canals M, Agnati LF, Lluis C, Franco R, Fuxe K (2005) Adenosine A2A receptor and dopamine D3 receptor interactions: evidence of functional A2A/D3 heteromeric complexes. Mol Pharmacol 67:400–407
Uchigashima M, Narushima M, Fukaya M, Katona I, Kano M, Watanabe M (2007) Subcellular arrangement of molecules for 2-arachidonoyl-glycerol-mediated retrograde signaling and its physiological contribution to synaptic modulation in the striatum. J Neurosci 27:3663–3676
van Kuyck K, Gabriels L, Cosyns P, Arckens L, Sturm V, Rasmussen S, Nuttin B (2007) Behavioural and physiological effects of electrical stimulation in the nucleus accumbens: a review. Acta Neurochir Suppl 97:375–391
Vollenweider FX, Vollenweider-Scherpenhuyzen MF, Babler A, Vogel H, Hell D (1998) Psilocybin induces schizophrenia-like psychosis in humans via a serotonin-2 agonist action. Neuroreport 9:3897–3902
von Euler G (1991) Biochemical characterization of the intramembrane interaction between neurotensin and dopamine D2 receptors in the rat brain. Brain Res 561:93–98
Whitty A (2008) Cooperativity and biological complexity. Nat Chem Biol 4:435–439
Williams DH, Stephens E, O’Brien DP, Zhou M (2004) Understanding noncovalent interactions: ligand binding energy and catalytic efficiency from ligand-induced reductions in motion within receptors and enzymes. Angew Chem Int Ed Engl 43:6596–6616
Williamson JR (2008) Cooperativity in macromolecular assembly. Nat Chem Biol 4:458–465
Young KA, Manaye KF, Liang C, Hicks PB, German DC (2000) Reduced number of mediodorsal and anterior thalamic neurons in schizophrenia. Biol Psychiatry 47:944–953
Zuardi AW, Crippa JA, Hallak JE, Moreira FA, Guimaraes FS (2006a) Cannabidiol, a Cannabis sativa constituent, as an antipsychotic drug. Braz J Med Biol Res 39:421–429
Zuardi AW, Hallak JE, Dursun SM, Morais SL, Sanches RF, Musty RE, Crippa JA (2006b) Cannabidiol monotherapy for treatment-resistant schizophrenia. J Psychopharmacol 20:683–686
Acknowledgment
This work was supported by the Swedish Research Council.
Author information
Authors and Affiliations
Corresponding author
Additional information
This review is dedicated to the special issue “Brain plasticity: aging and neuropsychiatric disorders”.
Rights and permissions
About this article
Cite this article
Fuxe, K., Marcellino, D., Woods, A.S. et al. Integrated signaling in heterodimers and receptor mosaics of different types of GPCRs of the forebrain: relevance for schizophrenia. J Neural Transm 116, 923–939 (2009). https://doi.org/10.1007/s00702-008-0174-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-008-0174-9