Abstract
Background
In microvascular decompression (MVD) procedures for hemifacial spasm (HFS), surgeons often encounter a rhomboid lip which may obscure the root exit zone (REZ) of the facial nerve. This study aims to explore the anatomical variations of rhomboid lips and their surgical implications to improve safety and effectiveness in MVD surgeries.
Methods
A retrospective analysis was conducted on 111 patients treated for HFS between April 2021 and March 2023. The presence of a rhomboid lip was assessed through operative video records, and its characteristics, dissection methods, and impact on nerve decompression outcomes were further examined. Preoperative magnetic resonance imaging (MRI) scans were reviewed for detectability of the rhomboid lip.
Results
Rhomboid lips were identified in 33% of the patients undergoing MVD, with a higher prevalence in females and predominantly on the left side. Two distinct types of rhomboid lips were observed: membranous and cystic variations. The membranous type was noted for its smaller size and position ventral to the choroid plexus. In contrast, the cystic variation was distinguished by its larger size and a thin membrane that envelops the choroid plexus. Preoperative MRI successfully identified rhomboid lips in only 21% of the patients who were later confirmed to have them in the surgical procedures. Surgical approaches primarily involved incisions on the dorsal wall and along the glossopharyngeal nerve root, with only limited need for extensive dissection from lower cranial nerves. Immediate spasm relief was observed in 97% of the patients. One case exhibited a lower cranial nerve deficit accompanied by brainstem infarction, which was caused by the dissection from the lower cranial nerves.
Conclusions
Recognizing the two variations of the rhomboid lip and understanding their anatomical structures are essential for reducing lower cranial nerve injuries and ensuring effective nerve decompression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The rhomboid lip is a sheetlike neural structure that extends from the floor of the fourth ventricle to the lateral recess, forming the ventral wall of the foramen of Luschka [8, 12, 13]. Understanding the anatomy surrounding the foramen of Luschka is crucial for performing safe surgery in the cerebellopontine angle. Despite being described microanatomy by Rhoton [12, 13], knowledge of the rhomboid lip remains limited. Its embryological development is not well known, and its function as a neural tissue remains unclear [1, 3, 6, 11]. Although histologically distinct from the arachnoid membrane, its appearance is similar, which may lead to it being ignored or dissected without recognition during surgery. The size and appearance of the rhomboid lip that needs to be dissected during microvascular decompression (MVD) can vary. Smaller rhomboid lips are situated ventrally to the choroid plexus, while larger ones may reach toward the jugular foramen, encasing the choroid plexus and attaching to the lower cranial nerves [1, 4, 6]. A large rhomboid lip can hinder the clear visualization of the root exit zone (REZ) of the facial nerve during MVD for hemifacial spasm (HFS) [1, 4, 6, 11]. Extensive dissection near the lower cranial nerves poses a risk of cranial nerve palsy, potentially leading to hoarseness or dysphagia [2]. In contrast, inadequate dissection of the rhomboid lip may result in insufficient exposure of the REZ, increasing the failed surgery due to either insufficient nerve decompression or missing the offending vessels. Although rhomboid lips are rarely encountered during MVD, they may be frequently overlooked due to their similarity to thick arachnoid membrane. Failing to recognize the presence of the rhomboid lip and its relationships with the adjacent structures can lead to unnecessary dissection, which increases the risk of neural damage and vascular injury [4, 6]. Comprehensive understanding of the anatomical structures at the surgical site is crucial to performing safe and effective surgeries. Despite its significance, there is a scarcity of literature that addresses the clinical implications and surgical strategies regarding the rhomboid lip. This study aims to delineate the anatomical characteristics of the rhomboid lip to enhance the safety of surgical interventions.
Methods
We retrospectively analyzed 111 patients treated with HFS between April 2021 and March 2023. Recorded operative videos were scrutinized to ascertain the presence of the rhomboid lip within the surgical fields. Among the 101 patients who underwent initial MVD, the rhomboid lip was identified in the surgical videos of 33 patients (Fig. 1). For these cases, further analyses were conducted on the characteristics of the rhomboid lips, dissection methods, the offending arteries, and the techniques utilized for nerve decompression. Additionally, preoperative magnetic resonance imaging (MRI) scans were retrospectively examined to assess the detectability of the rhomboid lip before surgery.
Surgical interventions for all patients were performed using the infrafloccular approach in a lateral position. The morphological characteristics of the rhomboid lips observed during these procedures were classified into two types: the membranous type and the cystic type, as depicted in the figure (Fig. 2). The membranous type is characterized as a small, thick membranous structure situated ventrally to the choroid plexus. In contrast, the cystic type is clearly distinguished from the membranous type by encapsulating the choroid plexus. Larger ones of the cystic type tend to extend towards the jugular foramen, showing cystic formation.
Anatomical variations of the rhomboid lip. a Illustration at the level of the Foramen Luschka elucidating their distinct anatomical configurations. Two variants of the rhomboid lip, the membranous type (blue line) and the cystic type (black line) are demonstrated. b Membranous type of rhomboid lip on the right. Characterized as a small, membranous structure situated ventrally to the choroid plexus and dorsally to the lower cranial nerves. c Cystic type of rhomboid lip on the right. Distinguished by its encapsulation of the choroid plexus, extending towards the jugular foramen with cystic formation
The dissection strategies employed were categorized based on three distinct procedures (Fig. 3). These included the 'Dorsal Incision,' which involved an incision on the dorsal membrane of the rhomboid lip; the 'Longitudinal Incision,' an extensive incision on the ventral membrane along the glossopharyngeal nerve root; and the 'Extensive Dissection,' which meticulously detached the rhomboid lip from the lower cranial nerves. The offending arteries and the nerve decompression techniques were documented by reviewing operative records and video recordings. Preoperative MRI scans were retrospectively analyzed for patients whose rhomboid lips were identified during the surgery to ascertain whether these anatomical structures were detectable before the surgery. The efficacy of MVDs was assessed by recording the spasm-free rates immediately one year after the surgery. Any postoperative neurological complications were systematically investigated.
Surgical dissection for the rhomboid lip (Right Side). Strategic incisions are employed in the surgical dissection of the rhomboid lip. The "Dorsal Incision" (dashed red line) is made on the dorsal membrane of the rhomboid lip. The "Longitudinal Incision" (dashed blue line) runs parallel to the glossopharyngeal nerve root. The "Extensive Dissection" (black arrow) meticulously separates the rhomboid lip from the lower cranial nerves
In analyzing demographic characteristics, p-values were derived using linear regression for continuous variables, and chi-squared tests or Mantel–Haenszel tests for categorical variables. Significance for each statistical test was established at a two-sided P-value of < 0.05. All statistical analyses were performed using SAS software (version 9.4, SAS Institute, Inc., Cary, North Carolina).
Results
Incidence of the rhomboid lip
Rhomboid lips were identified in the operative field in 33 of the 101 patients (33%) who underwent initial MVD for HFS. Of these, 15 patients were classified as having the membranous type, while 18 were classified as having the cystic type (Fig. 1). The mean age of these patients was 53 years, ranging from 28 to 78 years. A higher prevalence of rhomboid lips was observed in females, with 22 patients (67%) compared to males, and more frequently on the left side, with 19 patients (58%), than on the right. No statistically significant differences were observed in age, sex, and affected side when comparing patients with intraoperatively identified rhomboid lips to those without. Preoperative MRI successfully identified the cystic type of rhomboid lips in 7 patients prior to surgery (Fig. 4). These cases account for 7% of the total 101 initial MVD cases in this series and 21% of the instances where rhomboid lips were confirmed during the surgery. In contrast, no cases of the membranous type rhomboid lip were detected, demonstrating a statistically significant difference (p = 0.0009) (Table 1).
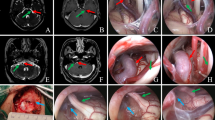
Imaging study of the cystic type rhomboid lip (Right Side). a Axial magnetic resonance imaging (MRI) indicates the presence of the cystic type rhomboid lip at the level of the foramen Luschka. The cyst membrane surrounds the choroid plexus and causes a ventral displacement of the lower cranial nerves. b An upper slice shows the neurovascular compression by the AICA at the root entry zone of the facial nerve. c Three-dimensional GammaPlan surgical view providing a perspective on the relationships between the rhomboid lip and adjacent neurovascular structures. d A ventral view of the surgical field elucidating the anatomical location of the rhomboid lip. AICA; anterior inferior cerebellar artery; CP, choroid plexus; RL, rhomboid lip
Appearance of the rhomboid lip
Rhomboid lips are classified into two distinct types. The membranous type, observed in 15 patients (45%), is characterized by its smaller size and positioning between the choroid plexus and the lower cranial nerves, extending from the floor of the fourth ventricle (Fig. 5). This type exhibits a white, thick membrane composed of a fibrous layer reminiscent of onion skin, which can be feasibly differentiated from the arachnoid membrane. The membranous type tends to adhere tightly to the lower cranial nerves. In contrast, the cystic type observed in 18 patients (55%), is typically larger than the membranous type and, as a distinct characteristic, encases the choroid plexus within its structure (Figs. 6 and 7). The surface of the cystic type is notably thin, complicating its differentiation from the normal arachnoid membrane. Consequently, unrecognized dissection occurred more frequently with the cystic type, affecting 5 patients (28%), compared to the membranous type, which involved only one patient (7%). Small veins are frequently observed on the surface of a rhomboid lip (Fig. 7a). The size of the cystic type varies, ranging from the area around the root exits of the lower cranial nerves to extensions towards the jugular foramen, accompanied by cyst-like formation (Figs. 4a and 6a). The cyst cavity is not merely an isolated pooling of cerebrospinal fluid; rather, it is continuous from the 4th ventricle (Fig. 7d). Exceptionally, the choroid plexus was observed penetrating the thin rhomboid lip membrane through a natural foramen, protruding into the lateral cerebellomedullary cistern in one patient (Fig. 8). The cystic type of rhomboid lips typically exhibits moderate adhesions to the lower cranial nerves, though these adhesions are not more severe than those observed with the membranous type.
Membranous type rhomboid lip (Left Side). a Exposure of the membranous type rhomboid lip locating ventral to the choroid plexus (black asterisk), adhering to lower cranial nerves. PICA, posterior inferior cerebellar artery. b Surgical incisions applied to the rhomboid lip. A longitudinal incision along the glossopharyngeal nerve (dashed blue line) and extensive dissection from lower cranial nerves (black dashed line), with a vascular injury from a tiny perforator noted during dissection. c Neurovascular compression by the PICA is shown (white asterisk) via the longitudinal incision. The decompression procedure was performed through this incision. The extensive dissection was unnecessary. d Postoperative MRI shows a brainstem infarction in the medulla (white arrowhead) following a perforator injury
Large-sized cystic type rhomboid lip with thin membrane (Left Side). a Preoperative MRI shows a higher intensity area in the cistern, suggesting the cystic type rhomboid lip with dislocated lower cranial nerves. The cyst membrane is undetectable on MRI, and the cyst extends to the jugular foramen. b Initial exposure shows the cystic type rhomboid lip after arachnoid dissection, reaching the jugular foramen. An incision on the dorsal wall of the rhomboid lip is indicated (red dashed line). c The choroid plexus was found within the rhomboid lip after the incision on the dorsal wall. A cystic portion located laterally. A subsequent longitudinal incision along the glossopharyngeal nerve (blue dashed line) was followed on the ventral wall. d Neurovascular compression by AICA (white asterisk) was identified via the rhomboid lip with the choroid plexus retracted medially. The extensive dissection from the lower cranial nerves was not applied in this case
Medium-sized cystic type rhomboid lip with thick membrane (Right Side, Video available). Operative photos and an operative video from the case in Fig. 4. a Initial exposure displays the cystic type rhomboid lip featuring a thick membrane, with small veins visible on the surface (white arrowhead). This thick membrane correlates with findings from MRI (Fig. 4a). The rhomboid lip hinders access to the root exit zone (REZ) of the facial nerve due to adhesion to the lower cranial nerves. b An incision on the dorsal wall of the rhomboid lip (red dashed line) unveils the choroid plexus while preserving the arachnoid between the rhomboid lip and the lower cranial nerves. c A longitudinal incision along the glossopharyngeal nerve (blue dashed line) facilitates access to the REZ of the facial nerve, with the choroid plexus retracted medially. Extensive dissection from the lower cranial nerves was avoided. d Neurovascular compression by the AICA is revealed (white asterisk). A lateral view shows the floor of the 4th ventricle (black asterisk) continuing to the ventral wall of the rhomboid lip
Exceptional natural foramen in the rhomboid lip (Left Side). a After incising the dorsal wall, the choroid plexus within the cystic rhomboid lip is exposed, partially protruding into the lateral medullary cistern (black arrowhead) through a natural foramen on the ventral wall of the rhomboid lip (white dashed line). b Retraction of the choroid plexus reveals the subarachnoid space ventral to the rhomboid lip through the foramen's margin (white arrowhead)
Surgical manipulation
Surgical dissection of the rhomboid lip was categorized into three distinct procedures. The incision on the dorsal wall of the rhomboid lip was performed in all cases (100%) of the cystic type to expose the choroid plexus, which is enveloped by the rhomboid lip (Figs. 6c and 7b). In contrast, for the membranous type, this incision was not utilized for the same purpose because the choroid plexus is located outside the rhomboid lip. This incision was employed in three cases of the membranous type specifically to visualize the ventral area of the lower cranial nerves. For the remaining 12 cases (80%) of the membranous type, the dorsal incision was either deemed unnecessary or was avoided due to its small size and tight adhesion to the lower cranial nerves. A statistically significant difference in the use of the dorsal incision between the cystic and membranous types was observed (p < 0.001).
The longitudinal incision along the glossopharyngeal nerve root was utilized to visualize the REZ of the facial nerve in 20 patients (60%) in total. Although there was no statistical significance in the frequency of longitudinal incision between the two types, it was performed more often in the cystic type (13 patients, 71%) than in the membranous type (7 patients, 47%) (Fig. 5b), attributed to the larger size of the cystic type. In most cases, the incision was necessary to reach the REZ of the facial nerve (Figs. 5b and 6c). There was one case where the floor of the 4th ventricle was exposed after this incision (Fig. 7d). When the offending vessel was the anterior inferior cerebellar artery (AICA) or the common trunk of the anterior and inferior cerebellar arteries (APC), the dorsal and longitudinal incisions were sufficient to perform transposition of the offending vessel in most cases (23 patients, 69%).
Extensive dissection was performed exclusively in cases requiring manipulation in the ventral area of the lower cranial nerves. This surgical dissection was conducted in only 5 patients (15%) in total, mainly for those involving the posterior inferior cerebellar artery (PICA, 11 patients, 33%) or the vertebral artery (7 patients, 21%), due to the significant risks associated with this procedure. These risks included potential damage to the lower cranial nerves and brainstem, resulting from either direct or vascular injury. Predominantly, this procedure was performed in patients with the cystic type (4 patients, 22%) compared to the membranous type (one patient, 7%), where dysphagia was observed postoperatively (Fig. 5).
In all patients, the arteries causing compression were successfully transposed away from the REZ of the facial nerve following the specified incisions and dissection of the rhomboid lips. In this series, the insertion of a prosthesis at the REZ was not performed.
Surgical outcomes and complications
Immediate relief from spasms was achieved in 32 patients (97%) in total. Although fluctuations in spasms and delayed relief were noted in 5 patients (15%), 32 patients (97%) achieved spasm-free status one year after surgery. There were no statistical differences between the two types of rhomboid lips regarding surgical outcomes. Persistent neurological deficits one year after surgery included facial nerve palsy (House-Brackmann grade 2) in one patient and lower cranial nerve palsy, accompanied by brainstem infarction presenting as Wallenberg syndrome, in another (Fig. 5d). No cases of hearing impairment were noted at one year postoperatively (Table 1).
Discussion
The rhomboid lip frequently presents a challenge in MVD for HFS by obstructing the clear visualization of the REZ of the facial nerve [1, 2, 4, 6, 9, 11]. Its appearance varies significantly in terms of size, wall thickness, and cystic formation. Akiyama et al. observed rhomboid lips in cadaveric specimens, categorizing them into three types based on lateral expansion relative to the choroid plexus [1]. They found that the most common type, present in 75% of specimens, is small-sized and located medially to the choroid plexus's lateral edge. Conversely, rhomboid lips that extend beyond the choroid plexus's edge were observed in 25% of specimens, including a rare variation that reaches the jugular foramen in 5% of cases. Nakahara et al. explored the encounter rate and detectability of the rhomboid lip in 34 clinical patients with HFS [11]. Among these, rhomboid lips were identified in 9 (26.5%) cases, with only 3 (8.8%) detected in preoperative MRI. They advocated the awareness of the rhomboid lip's presence during MVD for HFS due to its potential to hinder facial nerve exposure and increase the risk of lower cranial nerve deficits from improper dissection. In this study, we identified distinct variations in the appearance of the rhomboid lip. The smaller-sized rhomboid lip does not encase the choroid plexus, whereas the larger variations tend to envelop it. These differences may stem from variations in embryonic development. Our observations support the hypothesis proposed by Barany et al. that the development of the choroid plexus in relation to the rhomboid lip leads to the formation of a cystic variation [3]. During its development, the choroid plexus, encapsulated by the rhomboid lip, may undergo expansion, resulting in the thinning of the encapsulating rhomboid lip. This thinning process can be exacerbated by the secretion of cerebrospinal fluid (CSF) from the choroid plexus within this cystic structure, which is associated with primary obstruction of the foramen of Luschka. In instances where CSF flow is compromised from the covering rhomboid lip, a large cyst can be formed, extending towards the jugular foramen. We observed that larger rhomboid lips often have thinner walls, resembling the arachnoid membrane, potentially leading to misidentification or oversight during MVD procedures. Careful analysis of preoperative MRI can assist in predicting the presence of the cystic type of rhomboid lip based on its CSF retention, although detectability remains limited. In contrast, the membranous type of the rhomboid lip is so small that it cannot be detected by MRI, necessitating the determination of a surgical strategy for this variant intraoperatively.
Lower cranial nerve deficits, reported at a rate of 2.8% in MVD procedures for HFS, represent significant risks that should be avoided [7]. The dissection of the rhomboid lip from the lower cranial nerves has been linked to complications such as hoarseness and dysphagia, with it often adhering to these nerves [2, 11]. Although Amagasaki et al. reported no significant correlation between this dissection and neurological deficits, such complications can severely impact patients' postoperative quality of life [2]. Hence, neurosurgeons are advised to exercise utmost caution during the dissection at this region. Our own experience includes an instance of lower cranial nerve palsy with brainstem infarction resulting from minor vascular injuries during this dissection. The infrafloccular approach, preferred for its reduced risk of hearing loss, conversely increases encountering rate with the rhomboid lip due to its direction of approach from beneath the glossopharyngeal nerve. This study demonstrates that extensive dissection from the lower cranial nerves is often unnecessary. Adequate exposure for facial nerve decompression can be achieved through precise incisions on its dorsal wall and along the glossopharyngeal nerve root. In cases involving the posterior inferior cerebellar artery (PICA) or vertebral artery (VA) as the offending vessel, meticulous separation of the rhomboid lip from the REZ of the lower cranial nerves is often essential. During such procedures, preserving the medullary branches of the VA and perforators from the lateral medullary segment of the PICA is crucial to prevent lower cranial nerve deficits and brainstem infarction [5, 10]. The cisternal segment of the nerve roots often exhibits severe adhesions with the rhomboid lip. If necessary, it is safer to incise the ventral wall parallel to the lower cranial nerve roots than attempting to detach the entire adherent membrane from the nerve roots.
Conclusion
During microvascular decompression for hemifacial spasm, two variations of the rhomboid lip may be encountered. A clear understanding of the surrounding anatomical structures can reduce the risk of lower cranial nerve injuries by minimizing the need for extensive dissection.
Data availability
Data is available upon reasonable request.
Code availability
Not applicable.
References
Akiyama O, Kondo A, Arai H (2019) The rhomboid lip: Anatomy, pathology, and clinical consideration in neurosurgery. World Neurosurg 123:252–258
Amagasaki K, Kurita N, Watanabe S, Shono N, Hosono A, Naemura K, Nakaguchi H (2017) Lower cranial nerve palsy after the infrafloccular approach in microvascular decompression for hemifacial spasm. Surg Neurol Int 8:67
Barany L, Baksa G, Patonay L, Racz G, Ganslandt O, Buchfelder M, Kurucz P (2018) Primary obstruction of the foramen of luschka: Anatomy, histology, and clinical significance. World Neurosurg 112:288–297
Ding F, Li P, Zuo X, Song W, Xiao Y, Wang D, Geng L, Hu X, Yang K, Liu Y, Zou Y (2024) Case report: Significance of the large rhomboid lip in microvascular decompression: insights from two clinical cases. Front Neurol 14:1336273
Djukić B, Djukić-Macut N, Djulejić V, Boljanović J, Milić I, Marinković S, Blagojević M (2023) Medullary branches of the vertebral artery: microsurgical anatomy and clinical significance. Acta Neurochir (Wien) 165:1807–1819
Funaki T, Matsushima T, Masuoka J, Nakahara Y, Takase Y, Kawashima M (2010) Adhesion of rhomboid lip to lower cranial nerves as special consideration in microvascular decompression for hemifacial spasm: Report of two cases. Surg Neurol Int 1:71
Huh R, Han IB, Moon JY, Chang JW, Chung SS (2008) Microvascular decompression for hemifacial spasm: analyses of operative complications in 1582 consecutive patients. Surg Neurol 69:153–157
Jean WC, Abdel Aziz KM, Keller JT, van Loveren HR (2003) Subtonsillar approach to the foramen of Luschka: an anatomic and clinical study. Neurosurgery 52:860–866
Kasimu M, Tuersun M, Maimaitituerxun Y, Abulizi W, Li S, Fulati N (2024) Abnormal rhomboid lip and choroid plexus should be valued in microvascular decompression for vestibulocochlear diseases. World Neurosurg 181:607–614
Lui F, Tadi P, Anilkumar AC (2023) Wallenberg syndrome. In: StatPearls [Internet]. StatPearls Publishing, Treasure Island (FL)
Nakahara Y, Matsushima T, Hiraishi T, Takao T, Funaki T, Masuoka J, Kawashima M (2013) Importance of awareness of the rhomboid lip in microvascular decompression surgery for hemifacial spasm. J Neurosurg 119:1038–1042
Rhoton AL Jr (2000) The cerebellopontine angle and posterior fossa cranial nerves by the retrosigmoid approach. Neurosurgery 47:93–129
Rhoton AL Jr (2000) Cerebellum and fourth ventricle. Neurosurgery 47:7–27
Acknowledgements
We dedicate this paper to the memory of Professor Takanori Fukushima, whose lifetime dedication profoundly advanced neurosurgery.
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Contributions
Study concept and design: Takuro Inoue. Data collection and analysis: Takuro Inoue, Yukihiro Goto, and Peter Adidharma. Data interpretation: Takuro Inoue. Writing the manuscript: Takuro Inoue. Reviewing and editing: Takuro Inoue, Yukihiro Goto, Shunsuke Satoh, Ryan Keswani, Yasuaki Inoue, and Mustaqim Prasetya. Supervision: Takanori Fukushima. All authors approved the final version of the submitted manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments.
Consent for publication
Not applicable.
Conflict of interest
The authors declare that the research was conducted without any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 89154 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Inoue, T., Goto, Y., Satoh, S. et al. Anatomical considerations and surgical manipulation of the rhomboid lip in microvascular decompression for hemifacial spasm. Acta Neurochir 166, 255 (2024). https://doi.org/10.1007/s00701-024-06155-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00701-024-06155-2