Abstract
Background
Balancing survival versus risk of inducing functional deficits is a challenge when resecting gliomas in or near eloquent areas. Our objectives were to assess deficits prior to and at 6 and 12 months after awake craniotomies with cortical and subcortical mapping in patients with suspected grade 2 gliomas in eloquent areas. We analyzed whether pre- and intraoperative factors were linked to an increased risk of postoperative deficits.
Method
Retrospective study of 92 consecutive patients operated between January 2010 and June 2014. All deficits reported by any healthcare professional and KPS-score preoperatively, immediately postoperatively (day 1–10), at 6 months and 12 months, were analyzed.
Results
A decrease in neurological and or cognitive function was common in the first days after surgery, with a significant improvement at 6 months after surgery and further improvement at 12 months. Immediately after surgery, 33% of the patients had severe deficits compared to 2% prior to surgery; this improved to 9% at 6 months and 3% at 12 months. However, at 12 months, 18% of the patients had new or worsened minor or moderate deficits and only 10% had no deficits compared to 39% prior to surgery. There were only minor changes in KPS. None of the recorded pre/intraoperative factors were found significantly to influence the risk of moderate/severe late postoperative deficits.
Conclusion
A significant amount of the patients in this study experienced new or worsened neurological and or cognitive deficits during follow-up. We found a higher frequency of deficits than normally reported. This is due to the inclusion of mild deficits, the use of patient-reported data, and our focus on cognitive deficits. Our study indicates that the impact of awake craniotomy with mapping on patient outcome is larger than expected. This in no way negates the use of the technique.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Maximal safe resection is the current gold standard as primary treatment of gliomas [2, 8, 11, 15, 28], based on evidence that more extensive resection prolongs overall survival. This evidence has accumulated particularly in the last decade, with some of the strongest evidence coming from a Norwegian research group [14, 16, 17, 21]. The use of awake craniotomy with mapping (ACWM) is by many considered the best operative technique in order to obtain maximal resection and at the same time protect neurological and cognitive function. Tumor growth often leads to neuroplasticity upsetting normal functional anatomical relations, particularly but not exclusively at the cortical level. This renders awake craniotomy with cortical and subcortical mapping with electrical stimulation and continuous testing of functions during resection an elegant technique to ascertain neuronal structures that needs to be spared in order to preserve function [24]. Postoperative neuroplasticity is much more likely to restore function related to cortical than to tract damage [9].
A meta-analysis comparing ACWM versus low- and high-grade glioma resection under general anesthesia (GA) found that with ACWM in average a greater percentage of tumor was resected (74.8 vs. 58.3%) with fever postoperative neurological deficits (3.4 vs. 8.6%) [6]. The number of neurological deficits following resection of tumors in eloquent areas is high immediately after surgery, but in many studies reported to decline to less than 10% 3 months after surgery, a time point often used as a divider between temporary and permanent deficits.
Hence, on one side, the literature indicates that the more extensive the resection of gliomas, the longer the expected survival will be; on the other hand, more extensive resections run a higher risk of inducing permanent neurological and cognitive deficits. This balance between maximal surgical treatment of the glioma and the preservation of function, i.e., the onco-functional balance, needs to be addressed by the team treating the patient typically together with their family. The choice of onco-functional balance can be standardized as in the concept of maximal safe surgery or individualized as we and others have suggested previously [4, 10]. Although there are numerous studies concerning glioma surgery with ACWM, there is relative sparse information regarding less severe neurological and even more sparse information regarding less severe cognitive deficits following surgery. In many studies, the information is dichotomized into severe or no deficits, with often limited information regarding the allocation of patients into these two groups.
In this study, we investigate not only severe neurological deficits but all deficits documented or reported by physicians, neuropsychologists and patients or relatives in a cohort treated according to the maximal safe surgery doctrine. Deficits are compared with the Karnofsky Performance Score (KPS) for each patient, and we assess whether certain pre- and intraoperative factors are linked to an increased risk of late moderate/severe deficits. Our main finding is a substantially higher total frequency of deficits than previously reported, although the frequency of severe deficits is similar to previous reports. This indicates that moderate and minor deficits have been neglected in previous reports. This is an important issue as both the treating neurosurgeon and the patient need to have an unbiased picture of the likely outcome of surgery.
Method
The study design is a retrospective consecutive cohort study, including patients operated with ACWM procedure for expected grade II gliomas at Copenhagen Neurosurgery department, Rigshospitalet, Denmark, from January 2010 to June 2014. Almost half of the patients (49%) had undergone prior surgery before 2010 (28 resection in GA, 11 ACWM, nine biopsies, six SEEG, and three other procedures).
Patients were identified by cross-checking the hospital operation booking system and the patient coding system for all mapping procedures. Data, entered by all healthcare professionals from the departments of neurosurgery, neuro-oncology, and neurology, as well as data from patients and relatives, were collected from the electronic hospital records. Data were obtained at the following time periods: Preoperative data collected maximal 2 months prior to surgery. Follow-up data collected at three time periods: immediate postoperative (day 1–10), 6 (5–7) months, and 12 (11–13) months, postoperatively.
Deficits were defined as follows: neurological (motor, sensory, visual, and auditory functions) and cognitive (executive functions, language, memory, attention, and mood). All patients had neuropsychological evaluation preoperatively, two thirds had follow-up neuropsychological evaluations. All deficits were graded in four categories: none (0), mild (1), moderate (2), and severe (3). Mild deficits were subtle and/or episodic deficits that did not affect the patient’s daily life. Moderate deficits had some effect on the patient’s quality of life and the ability to perform normal activities, and severe deficits incurred a significant reduction in quality of life and/or resulted in a need for assistance by others to perform normal daily activities. When more than one deficit was present, the collective deficit was assigned a grade, based on the influence on daily activities (Table 1).
Extraction and grading of deficits were carried out by two independent observers. If varying degrees of deficits were recorded within the same time period by the two observers, the most severe deficit description was used.
The KPS was calculated for the same four time periods as the neurological and cognitive deficits.
Tumor volume
Pre- and 3 months’ postoperative tumor volumes (MRI FLAIR sequence) were determined using the IPlan3.1 software (Brainlab ®, Münich Germany) segmentation tool.
Surgical procedure
Our surgical approach in this cohort was maximal safe resection. The time period from 2010 to 2014 is specifically chosen to represent a period prior to accepting a more individualized onco-functional balance agreed on with the patient where deficits may be chosen in order to increase resection [4]. If resection was terminated due to patient distress, tiredness, or emerging new deficits, we often performed a repeat procedure 3–6 months later when deficits had improved based on the hypothesis that neuronal reorganization/neuroplasticity will allow further tumor resection with acceptable low risk of inducing new permanent functional deficits [25]. In this series, 32 out of 92 (35%) patients had such repeated surgeries. In the analysis, we considered such staged operations as one surgical treatment. Hence, the preoperative status was recorded before the first operation (index procedure) and the postoperative data after the last surgical procedure.
Bipolar constant current biphasic 1 ms, 50 Hz stimulation, with a 5 mm distance between the poles, was used at the lowest stimulation intensity eliciting activation or inhibition at the cortex level. The same intensity was used for subcortical stimulation. Electrocorticography with a 4-point electrode strip was used after discharge monitoring in close proximity to the stimulation site. Activation or inhibition in 2/3 stimulations at the same site was regarded as demonstrating eloquence if there was no after discharge.
Statistical method
We employed dependency matrices and multiple regressions analysis to assess whether specific pre- and intraoperative factors were linked to an increased risk of new/worsened deficits 6 months after surgery. The factors analyzed were as follows: preoperative neurological and cognitive status, KPS, WHO grade (II, III), tumor location in one or more lobes, earlier cerebral procedures, new/worsened deficits at end of operation, adjuvant therapy during follow-up, time from diagnosis to operation, preoperative tumor size, volume of tumor resected, and Pignatti score [22].
Results
In the specified period from January 2010 until June 2014, 92 patients with suspected grade 2 glioma underwent a total of 115 ACWM; the cohort is described in Table 2. The aim was maximal safe resection of tumor, and the reasons for terminating resections are given in Table 3.
Deficits
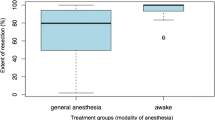
Two patients were censored at 6 months and eight patients at 12 months due to MRI-verified tumor progression. This was done as our objective was to investigate the effect of surgery, not that of tumor progression. A significant decline in neurological and cognitive function was observed immediately after surgery compared to just before surgery, with a significant improvement at 6 months and even further improvement at 12 months after surgery (Fig. 1).
All deficits (neurological and cognitive) present before, immediately after 6 and 12 months after surgery, graded according to severity (see Table 1): Severe (black), moderate (gray), minor (hatched), none (white)
Immediately after surgery, 33% of the patients had severe deficits compared to 2% prior to surgery; this improved to 9% at 6 months and 3% at 12 months. A similar pattern of increased frequency immediately after surgery and continuous improvement at 6 and 12 months was seen for moderate deficits (Fig. 1). The frequency of none and minor deficits was not surprisingly seen to decline immediately after surgery, as the patients shifted towards moderate and severe deficit, and then again increase later as the patients improved.
There was a differential pattern in the severity of neurological and cognitive deficits when comparing preoperative deficits with deficits at 6 and 12 months (Fig. 2). The pattern of neurological deficits demonstrated a small increment of patients with no neurological deficits and a small increase in patients with severe neurological deficits from 1 to 3%. The pattern of cognitive deficits showed a more substantial decline in minor and moderate deficits but with a similar increase in major deficits.
Neurological and cognitive deficits present before, immediately after 6 and 12 months after surgery, graded according to severity (see Table 1): Severe (black), moderate (gray), minor (hatched), none (white)
All new or worsened deficits, irrespective of neurological or cognitive in nature, are shown in Table 4 and grouped according to severity.
When KPS was dichotomized according to the best group (> 70) “Able to carry out normal activity and to work; no special care needed,” there was only minor statistically insignificant changes in KPS between preoperatively (88%), 6 (81%) and 12 months postoperatively (84%) (Table 5). The complete range of KPS is given in Table 6.
Epilepsy
Epilepsy was present at diagnosis in 74 patients (78%), and 23 patients (24%) had medically intractable epilepsy. This means that at least two antiepileptic drugs had been tried at relevant doses without obtaining seizure freedom. Twenty of these 23 patients (87%) were seizure-free at 1 month, and 18 (78%) were seizure-free at 3, 6, and 12 months after surgery.
Disposing factors
No statistically significant correlations were found between the pre- and intraoperative factors listed in Table 1 and the worsening of postoperative deficits at 6 months’ follow-up.
Discussion
Our objective was to assess the amount and severity of deficits related to tumor resection with cortical and subcortical mapping according to the maximal safe surgery doctrine. We found an increase in deficits and a slight decrease in KPS in the early period following surgery, with improvement at 6 and further improvement at 12 months postoperatively.
Our finding of 36% new or worsened deficits at 6 months compared to preoperatively is at odds with the much lower frequency of new deficits reported by others following ACWM, typically 3–10% at 3–6 months after the procedure [3, 6]. The main difference between our study and previous studies is that we specifically included not only severe deficits but also moderate and minor deficits and both neurological and cognitive deficits. Furthermore, we did not limit the search for deficits to neurosurgical records but investigated all patient records entered by all health care professionals as well as symptoms reported by patients or relatives. We therefore believe that our data more accurately reflects the patients’ true conditions than most previous studies. However, other factors of influence need to be considered.
Could the increased frequency of deficits be related to more aggressive resection?
The generally accepted relationship between extend of resection and overall survival is an incentive for the surgeon to aim for high-resection degrees which has to be balanced against the increased risk of inducing neurological and or cognitive deficits. Sometimes during ACWM, it is difficult to differentiate with absolutely certainty between a condition where the patient is getting tired in the process of the procedure and for the team to decide whether the patient is demonstrating fatigue as a sign of cognitive decline or due to exhaustion. As given in Table 3, we rarely terminated a procedure due to perceived fatigue but often because we perceived we had reached a functional border, but this may in fact have been an exhaustion causing a declined performance level of the patient during surgery. However, if we misjudged an emerging cognitive deficit as exhaustion, this might have led us to a more extensive resection than the planned maximal safe resection resulting in a higher frequency of postoperative deficits. A number of facts argues against this hypothesis. Firstly, we observed a late improvement in cognitive function and no significant change in KPS which would be expected if we had caused severe fatigue related to cognitive damage due to aggressive resection. Secondly, we obtained ≥ 90% resection in 55% of the patients and ≥ 80% resection in 75% of the patients which is comparable to other publications, e.g., a gross total resection in 75% reported in the meta-analysis by De Witt Hamer et al. [6]
Comparison of resection degrees is unfortunately still hampered by the lack of a common method of assessment. Most commonly tumor size and resection degree are based on simple measurements of tumor diameter in two or three orthogonal planes because this is easy in comparison, although unprecise compared with time-consuming volume segmentation recommended by the leading authorities [27]. Volume segmentation may soon be more common as post-processing techniques with automated tumor volume segmentation are being developed [20]. However, independent of the technique used evaluation of FLAIR images following surgical and or radiation treatment is not without problems as it can be difficult to differentiate between remnant tumor and gliosis caused by treatment. In conclusion, comparison of the percentage of resection obtained in this cohort with those reported in the literature does not indicate more aggressive surgery in our cohort as an explanation of more deficits.
Comparability of the population
By comparison with other mapping studies, we used fewer exclusion criteria. This is an unselected population with inclusion of all patients operated in a 53-month period for expected grade 2 glioma with ACWM technique, a fifth of the patients turned out to be grade III tumors. We included patients with previous surgeries, patients with repeat procedures during the study period, and patients with moderate and severe neurological or cognitive deficits prior to surgery. More than half of our patients had some deficit prior to their surgery/first surgery in the study period (63%).
All these factors may have caused our cohort to be more “fragile” due to an accumulated risk exposure by repetitive surgeries leading to potentially more extensive cerebral damage with less reserve capacity. We did investigate whether there were correlations between the listed pre- and intraoperative factors and worsened/new or increased deficits at 6 months. Despite smaller differences, no statistically significant correlation was found. It is important to highlight the small cohort size. In conclusion, the broader inclusion in this study, reflecting the practice in our department, may have resulted in a population of patients more susceptible to deficits. The statistical analysis did, however, not reveal this as a statically significant factor.
Comparability of follow-up methodology
In this study, all types of deficits were included regardless of the severity of the deficit or symptom. As an example, one male patient had completely normal neurological and neuropsychological evaluation at 6 months. However, he functioned as a soccer trainer for children in his free time and he reported that he had some difficulty maneuvering the football between obstacle cones, where he would sometimes stumble. This had never been a problem prior to the surgery, and hence, it was categorized as a minor neurological deficit.
The meta-analysis study by De Witt Hamer [6] is a logical reference as they analyzed the reported outcome from a large cohort of glioma patients (n = 8.091) from 90 published studies where tumor resection had been performed with or without ACWM technique. They reported a rate of late severe neurological deficits of 3.4% when ACWM technique was used, which is very similar to the frequency of late severe neurological and cognitive deficits we find, i.e., 7% at 6 months and 2% at 12 months. In most mapping studies, the definition of neurological deficits is often vague or non-existing, highlighting the need for a generally accepted common classification system [7, 8]. Currently, it is up to each research group to define and decide what to include. In some studies, only vague descriptions such as “no disabling permanent deficits” are used, while others report only on moderate to severe deficits, without thoroughly defining how these are defined or assessed. In the meta-analysis by De Witt Hamer et al., deficits were divided into severe (paresis grade 1–3, aphasia or severe dysphasia, hemianopia or vegetative state) and less severe [6]. We are not aware of other studies that have included minor neurological and cognitive deficits. This inclusion of minor deficits is the most likely reason for the high frequency of both preoperative and especially early and late postoperative deficits found in our study. The majority of our patients had a KPS over 80 (6 months 81%, 12 months 84%), indicating that the deficits did not prevent them from carrying out normal activities. So, although we report a higher frequency, it does not significantly interrupt the daily life abilities of most patients.
Another considerable difference was the source of data extraction. The majority of mapping studies are based solely on data (pre- and postoperative) from surgeons involved in the treatment of the patients, making these studies fragile towards investigator bias. There is often no further description included on how deficits were assessed or how the examination of the patient was performed. In contrast, this study included deficits reported by all healthcare professionals including neurosurgeons, neurologists, oncologists, neuropsychologists, nurses, and therapists as well as the patients and their relatives. Patient-reported outcome (PRO) is seldom reported, perhaps because they are considered to be subjective in nature and therefore of low validity. However, PRO measures (PROM) may significantly increase the sensitivity of glioma follow-up programs and allow us knowledge of symptoms and functions judged important by the patients. This is supported by Drewes et al., who demonstrated that the frequency of deficits was considerably higher when patients were questioned in person, compared with data collected by medical records and that prospective studies tend to report a significantly higher proportion of deficits than retrospective studies [7]. Therefore, although we report a higher frequency of all types of deficits in the present study compared to most other studies, it is likely that our study underestimated the frequency of deficits as it is a retrospective study without systematic use of PROM.
In the present study, we also included data from neuropsychologists and cognitive deficits were included as a defined entity. It is difficult to assess how many of mapping studies include neuropsychological evaluations in assessment. The generally low number of cognitive deficits reported seems to indicate a lack of proper neuropsychological evaluation [7, 19]. Our analysis demonstrates a significant number of patients experiencing cognitive deficits, both prior to and after surgery. Including our neuropsychological evaluations and the definition of deficits, what we used has led to a more solid foundation for discovering cognitive deficits. In spite of an apparent improvement of mild cognitive deficits, after surgery, a significant part of the cohort continued to experience cognitive deficits (31% at 6 months follow-up, 20% at 12). This is in concordance with several studies, who found that the majority of patients experienced cognitive deficits both before and after surgery with the majority being stable or improving after surgery [18, 23]. Postoperative cognitive improvement compared to preoperative status is often thought to be related to reduced clinical or subclinical seizure activity following tumor resection [5] [26] [8, 18]. This is in line with our finding that 78% of the patients had epilepsy at diagnosis, and 18 out of 23 patients (78%) with medically intractable epilepsy became seizure-free after surgery. Cognitive deficits have been found to decrease the quality of life significantly, whereas motor function disability often had a less negative effect [1, 13]. Though these studies are small, they do support the importance of including cognitive deficits and their effect on the patients’ perception of postoperative quality of life.
In conclusion, many factors such as follow-up methodology, definition, and classification of deficits, whether cognitive deficits are included or not, onco-functional balance, PROM etc. all contribute to a significant heterogeneity as previously demonstrated [6, 12]. We are convinced that the inclusion of mild deficits, a greater focus on cognitive deficits, the use of data reported by patients/relatives, and neuropsychologists along with patient records from other departments has resulted in the discovering of significantly more mild and moderate deficits, and we believe that these results can be replicated within the majority of ACWM cohorts, if the same methodology is applied.
Massive heterogeneity of course makes comparisons between studies very difficult and necessitates a common protocol for reporting of neurological and cognitive function, as has been advocated also by others [7], as well as for determination of tumor size and degree of resection, in order to advance research into effect of surgical treatment of gliomas.
Weakness of the study
The major limitation of our study is its retrospective nature based on the standard practice of registration in patient records by a large group of health care professionals. As argued above it is likely that the study design leads to an underestimation of the true number of deficits. Some of the strengths of our study are that it includes all procedures in a given timeframe, thereby representing the institutional practice that it includes reports of deficits by all hospital-based healthcare professionals involved in the care of these patients and the systematic volume segmentation of the tumors before and after surgery.
Conclusion
In this study, we demonstrate that the frequency of deficits after awake craniotomy with cortical and subcortical mapping has likely been underestimated in most studies, for two major reasons. First, most studies have limited their data collection to deficits noted by neurosurgeons. Secondly, most studies have only included severe or moderate deficits. We find that it is important to have detailed knowledge concerning any and all types of deficits in order to evaluate and if pertinent adjust the technique. But it is equally important as a solid foundation for the informed consent obtained from the patients. A detailed information regarding risks of deficits is an intricate part of the discussion regarding the onco-functional balance between surgeon and patient. We believe that the mapping techniques as used in this study are an important tool when treating glioma patients but there is no “one size fits all.” The planned onco-functional balance has to be personalized to the individual patient and their wishes for the future in the context of the individual tumor [4]. This retrospective study covers a period before we changed our doctrine from maximal safe surgery to this more flexible and individual approach to the onco-functional balance in the surgical planning.
References
Aaronson NK, Taphoorn MJ, Heimans JJ, Postma TJ, Gundy CM, Beute GN, Slotman BJ, Klein M (2011) Compromised health-related quality of life in patients with low-grade glioma. J Clin Oncol 29(33):4430–4443
Aghi MK, Nahed BV, Sloan AE, Ryken TC, Kalkanis SN, Olson JJ (2015) The role of surgery in the management of patients with diffuse low grade glioma: a systematic review and evidence-based clinical practice guideline. J Neuro-Oncol 125(3):503–530
Bello L, Gallucci M, Fava M, Carrabba G, Giussani C, Acerbi F, Baratta P, Songa V, Conte V, Branca V, Stocchetti N, Papagno C, Gaini SM (2007) Intraoperative subcortical language tract mapping guides surgical removal of gliomas involving speech areas. Neurosurgery 60(1):67–80 discussion 80
Brennum J, Maier CM, Almdal K, Engelmann CM, Gjerris M (2015) Primo non nocere or maximum survival in grade 2 gliomas? A medical ethical question. Acta Neurochir 157(2):155–164
Chang EF, Potts MB, Keles GE, Lamborn KR, Chang SM, Barbaro NM, Berger MS (2008) Seizure characteristics and control following resection in 332 patients with low-grade gliomas. J Neurosurg 108(2):227–235
De Witt Hamer PC, Gil Robles S, Zwinderman AH, Duffau H, Berger MS (2012) Impact of intraoperative stimulation brain mapping on glioma surgery outcome: a meta-analysis. J Clin Oncol 30:2559–2565
Drewes C, Sagberg LM, Jakola AS, Gulati S, Solheim O (2015) Morbidity after intracranial tumor surgery: sensitivity and specificity of retrospective review of medical records compared with patient-reported outcomes at 30 days. J Neurosurg 123(4):972–977
Duffau H (2014) Towards an “active” cognitive assessment in patients with diffuse low-grade glioma. World Neurosurg 82(1–2):e129–e131
Duffau H (2017) Mapping the connectome in awake surgery for gliomas: an update. J Neurosurg Sci 61(6):612–630
Duffau H, Mandonnet E (2013) The “onco-functional balance” in surgery for diffuse low-grade glioma: integrating the extent of resection with quality of life. Acta Neurochir 155(6):951–957
Duffau H, Taillandier L (2015) New concepts in the management of diffuse low-grade glioma: proposal of a multistage and individualized therapeutic approach. Neuro-Oncology 17(3):332–342
Fountain DM, Allen D, Joannides AJ, Nandi D, Santarius T, Chari A (2016) Reporting of patient-reported health-related quality of life in adults with diffuse low-grade glioma: a systematic review. Neuro-Oncology 18(11):1475–1486
Gustafsson M, Edvardsson T, Ahlström G (2006) The relationship between function, quality of life and coping in patients with low-grade gliomas. Support Care Cancer 14(12):1205–1212
Hervey-Jumper SL, Berger MS (2016) Maximizing safe resection of low- and high-grade glioma. J Neuro-Oncol 130(2):269–282
Ius T, Isola M, Budai R, Pauletto G, Tomasino B, Fadiga L, Skrap M (2012) Low-grade glioma surgery in eloquent areas: volumetric analysis of extent of resection and its impact on overall survival. A single-institution experience in 190 patients. J Neurosurg 117(6):1039–1052
Jakola AS, Myrmel KS, Kloster R, Torp SH, Lindal S, Unsgard G, Solheim O (2012) Comparison of a strategy favoring early surgical resection vs a strategy favoring watchful waiting in low-grade gliomas. JAMA 308(18):1881–1888
Jakola AS, Skjulsvik AJ, Myrmel KS, Sjåvik K, Unsgård G, Torp SH, Aaberg K, Berg T, Dai HY, Johnsen K, Kloster R, Solheim O (2017) Surgical resection versus watchful waiting in low-grade gliomas. Ann Oncol 28(8):1942–1948
Jakola AS, Unsgard G, Myrmel KS, Kloster R, Torp SH, Lindal S, Solheim O (2012) Low grade gliomas in eloquent locations - implications for surgical strategy, survival and long term quality of life. PLoS One 7(12):e51450. https://doi.org/10.1371/journal.pone.0051450
Klein M, Duffau H, De Witt Hamer PC (2012) Cognition and resective surgery for diffuse infiltrative glioma: an overview. J Neuro-Oncol 108(2):309–318
Li Z, Wang Y, Yu J, Shi Z, Guo Y, Chen L, Mao Y (2017) Low-grade glioma segmentation based on CNN with fully connected CRF. J Healthc Eng 2017:9283480
Pessina F, Navarria P, Cozzi L, Ascolese AM, Simonelli M, Santoro A, Tomatis S, Riva M, Fava E, Scorsetti M, Bello L (2016) Value of surgical resection in patients with newly diagnosed grade III glioma treated in a multimodal approach: surgery, chemotherapy and radiotherapy. Ann Surg Oncol 23(9):3040–3046
Pignatti F, van den Bent M, Curran D, Debruyne C, Sylvester R, Therasse P, Afra D, Cornu P, Bolla M, Vecht C, Karim AB, European OFRATOCBTCG, European OFRATOCRCG (2002) Prognostic factors for survival in adult patients with cerebral low-grade glioma. J Clin Oncol 20(8):2076–2084
Racine CA, Li J, Molinaro AM, Butowski N, Berger MS (2015) Neurocognitive function in newly diagnosed low-grade glioma patients undergoing surgical resection with awake mapping techniques. Neurosurgery 77(3):371–379
Southwell DG, Birk HS, Han SJ, Li J, Sall JW, Berger MS (2017) Resection of gliomas deemed inoperable by neurosurgeons based on preoperative imaging studies. J Neurosurg 10:1–9. https://doi.org/10.3171/2017.5.JNS17166
Southwell DG, Hervey-Jumper SL, Perry DW, Berger MS (2016) Intraoperative mapping during repeat awake craniotomy reveals the functional plasticity of adult cortex. J Neurosurg 124(5):1460–1469
Talacchi A, d’Avella D, Denaro L, Santini B, Meneghelli P, Savazzi S, Gerosa M (2012) Cognitive outcome as part and parcel of clinical outcome in brain tumor surgery. J Neuro-Oncol 108(2):327–332
van den Bent MJ, Wefel JS, Schiff D, Taphoorn MJ, Jaeckle K, Junck L, Armstrong T, Choucair A, Waldman AD, Gorlia T, Chamberlain M, Baumert BG, Vogelbaum MA, Macdonald DR, Reardon DA, Wen PY, Chang SM, Jacobs AH (2011) Response assessment in neuro-oncology (a report of the RANO group): assessment of outcome in trials of diffuse low-grade gliomas. Lancet Oncol 12(6):583–593
Zadeh G, Khan OH, Vogelbaum M, Schiff D (2015) Much debated controversies of diffuse low-grade gliomas. Neuro-Oncology 17(3):323–326
Acknowledgements
Thank you to the following people who have helped in gathering and analyzing the data presented in this article: Almdal K, Grøndal O, Johannsen M, and Azam A.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Brennum, J., Engelmann, C.M., Thomsen, J.A. et al. Glioma surgery with intraoperative mapping—balancing the onco-functional choice. Acta Neurochir 160, 1043–1050 (2018). https://doi.org/10.1007/s00701-018-3521-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-018-3521-0