Abstract
We describe a case of rachipagus parasitic twin with spinal cord malformations (lipomyelomeningocele and tethered cord) in a 7-month-old Ethiopian infant. The parasitic mass had a well-formed foot, ankle and lower leg and a small sinus that resembled an anus. Magnetic resonance imaging scans revealed spinal malformations including a distal syringohydromyelia. The mass was successfully resected and the dural attachment was closed. Histopathological examination confirmed the diagnosis. Postoperatively, the child had unchanged, intact neurological function in both lower limbs. Almost all rachipagus parasitic twins are associated with spinal malformations. They should, therefore, be operated on by surgeons experienced in myelomeningocele surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
“Parasitic twin”, also called ”foetus in foetu” (FIF), is a well-known, but rare condition that occurs at 3 weeks of gestation [1]. Grant and Pearn [2] indicated an incidence of 1 per 500,000 births. It was first described by Banks [3] in 1789, by Meckel [4] in 1815 and later by Jones and Larkin in 1889 [5], and it was defined further by Willis [6]. A PubMed search for the terms “foetus in foetu” or “parasitic twin” found at least 148 publications dating back to 1950. Several authors have also reviewed previous cases [7–14]. A majority of the published cases have appeared in relation to the peritoneum, most often retroperitoneally [11]. The term “parasitic twin” is used to describe a partial fetus that is joined to an otherwise relatively normal fetus at one of the same sites of union as in intact conjoined twins [15]. They usually consist of externally attached supernumerary limbs, not infrequently with some viscera, as in a case previously published by our group [16]. Humphreys et al. [17] published a case with an accessory arm originating in the neck midline and offered an interesting discussion about the possible causes and pathogenesis of such malformations.
Conjoined twins with an asymmetric growth result in variably developed viable fetus or body parts (parasite) completely dependent on the other, normal fetus (autosite).
Imaging now allows early antenatal diagnosis of conjoined twins, and depicts the anatomy of the involved organs and associated anomalies, which is vital for parent counselling, prenatal and postnatal management decisions, and for presurgical planning. Awareness of the types and possible associated anomalies of conjoint twins is important for both the managing physicians and the radiologist.
We report an additional case of rachipagus parasitic male twin. Most of the reported rachipagus twins are parasitic and the most common parasitic organ is a limb, usually the upper extremity in the cervical rachipagus and the lower extremity in the thoracic or lumbar rachipagus [29]. Other structures: lung, bladder, genital organs, cartilage, urinary bladder, kidney, breast, nipple and intestinal organs may also be found in the parasite. Cardiac and central nervous system tissues in parasites and also some nervous tissue from the autosite may dominate the parasite. Commonly associated malformations in the autosite are nervous system malformations: spina bifida, tethered cord, vertebral body abnormalities. Other malformations, such as cardiac, renal, rectovaginal fistula and foot deformities (pes equinovarus) may also be found.
Though neural tube defects are relatively rare in the developed world, it is not an uncommon problem in neurosurgical paediatric practice in developing countries. Although these are two separate entities, they have been found together in our patient as in other rachipagus parasitic twins.
Case story
The patient was a 7-month-old infant girl born to a 23-year-old para-2 mother from northern Ethiopia, who had an uneventful pregnancy and gave birth by spontaneous vaginal delivery at home. The child was born with a progressively growing mass over the lower back with an appendage hanging from it. There was no paresis of the lower limbs. The child was feeding well and showed no signs of delayed developmental milestones.
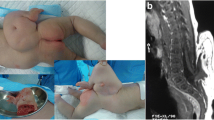
On examination at admission, there was a large midline mass over the lumbar region about 12 × 8 cm in size with a well-formed foot, ankle and lower third of the leg along with small 2 × 2-cm bud of what would presumably become an extremity or genitalia and a small sinus tract over the inferior portion of the mass that resembled the anal orifice (Figs. 1 and 2). The mass was completely covered with skin; it was soft in consistency with the attached appendage that showed no movement of its own. It was not tender, but was sensitive to touch, pain and pressure. The patient had no neurological deficit. Magnetic resonance imaging (MRI) was done and revealed a huge asymmetrical lumbosacral lipomatous mass containing complex structures, cystic and irregular T1 and T2 hypo-intense components converging to the dysraphic lumbosacral defect. These were in continuity with the bone in the supernumerary limb. MRI also revealed a tethered spinal cord containing a distal syringohydromyelia (Fig. 3).
Surgery
After being admitted to the hospital, the patient was operated on without neurophysiological monitoring and the entire mass was excised from its attachment to the lipoma. The dural defect (1.0 × 0.5 cm) was identified deep in the resection cavity. There were no neural structures identified and there was no lipoma identified extending into the dura, and the dural defect was closed. The lipoma was removed and the skin was closed over the midline. The specimen was sent for biopsy. The immediate postoperative period passed uneventfully, and the patient was discharged from the hospital without any complications on the 3rd postoperative day.
Follow-up
One year after the operation, the patient was seen at the follow-up clinic. The surgical scar was acceptable; she was neurologically intact and had normal development. The biopsy revealed normal looking neural tissue, skeletal muscle, smooth muscle, fat tissue and cyst lined with pseudo-stratified ciliated columnar cells with epidermal lining.
Discussion
The incidence of conjoined twinning is said to be 1 per 50,000–100,000 births (60 % are stillbirths) and 10 % of these again are parasitic. Heteropagus is the term used to describe the development of asymmetry in conjoined twinning when one of the twins (autosite) monopolises the placental blood at the expense of the other fetus (parasite) with consequent ischaemic atrophy. The parasite continues to grow attached to the autosite. According to Spencer, parasitic twins are aberrations of monozygotic twinning, appearing as foetus in foetu (FIF) or teratomas. It is just the degree of malformation and the timing of the embryological insult that differ [15].
The aetiology of conjoined twins, parasitic or not, is not yet clear. There are two theories to explain the phenomenon. The fission theory states that incomplete division of the blastocyst between the 13th and the 15th days of gestation results in conjoining and the fusion theory says that fusion of monozygotic twins results from a secondary union of two separate monovular embryonic discs; for an overview, see [18].
In their extensive review on imaging in conjoined twins, Kingston et al. [19] made some important points: “Planning of surgical separation is aided by accurate preoperative imaging. Such twins are classified according to the most prominent site of connection: the thorax (thoracopagus), abdomen (omphalopagus), sacrum (pygopagus), pelvis (ischiopagus), skull (craniopagus), face (cephalopagus), or back (rachipagus). The area of fusion largely determines the imaging modalities used”. This also applies to parasitic twins, and it must apply to surgery as well; the surgery has to be tailored according to the organs and tissue of the region of fusion.
The site of connection must consequently determine which surgical specialty should deal with the case. It has been demonstrated that there are spinal malformations underneath the supernumerary limb in most rachipagus parasitic twins [16, 20–29], ranging from spina bifida to tethered cord, myelomeningocele (MMC), diastematomyelia, and other spinal cord malformations. Removal of a supernumerary limb attached to the back is, therefore, not just a simple and straight forward limb amputation; there will often be neurosurgical challenges lurking in the depth. It is, therefore, our advice that a surgeon experienced in MMC surgery should be in charge when performing surgery in such cases. We believe this is the most important lesson that can be learned from this case report.
Conclusions
Most reported rachipagus parasitic twins are associated with dysraphic spinal column and cord anomalies. If not detected prenatally, the condition will be diagnosed after birth. We recommend MRI as the neuroimaging method of choice in these cases to map the anatomy of the anomaly as accurately as possible before surgery. As there are spinal malformations underneath the supernumerary limb in most rachipagus parasitic twins, removal of a supernumerary limb attached to the back is, therefore, not just a simple amputation. We, therefore, recommend that a surgeon experienced in MMC surgery should be in charge when performing such surgery.
References
Husain AN, Muraskas J, Lambert G, Dado D, Lynch J (1989) Parasitic conjoined twins with omphalocele and tetralogy of Fallot. Pediatr Pathol 9:321–328
Grant P, Pearn JH (1969) Foetus-in-foetu. Med J Aust 1:1016–1019
Banks J (1789) An account of a monster of the human species, in two letters; one from Baron Reichel to Sir joseph Banks, Bart. and the other from Mr. Andersson to Baron Reichel. Communicated by Sir Joseph Bank, Bart PRS. Philos Trans R Soc London 79:157–160
Meckel JF (1815) De duplicitate monstrosa commentarius. Halle, Berlin
Jones R, Larkin FC (1889) Removal of accessory limb and meningocele from the back of a child, and its anatomy. Br Med J 2:310–311
Willis RA (1935) The structure of teratomata. J Pathol Bacteriol 40:1–36
Arlikar JD, Mane SB, Dhende NP, Sanghavi Y, Valand AG, Butale PR (2009) Fetus in fetu: two case reports and review of literature. Pediatr Surg Int 25:289–292
Chua JH, Chui CH, Sai Prasad TR, Jabcobsen AS, Meenakshi A, Hwang WS (2005) Fetus-in-fetu in the pelvis: report of a case and literature review. Ann Acad Med Singap 34:646–649
Gude D, Rayudu BR, Bansal D, Sashidhar C (2012) Revisiting fetus-in-fetu. Ann Saudi Med 32:427–429
Hager J, Sanal M, Trawoger R, Gassner I, Oswald E, Rudisch A, Schaefer G, Mikuz G, Sergi C (2007) Conjoined epigastric heteropagus twins: excision of a parasitic twin from the anterior abdominal wall of her sibling. Eur J Pediatr Surg 17:66–71
Hoeffel CC, Nguyen KQ, Phan HT, Truong NH, Nguyen TS, Tran TT, Fornes P (2000) Fetus in fetu: a case report and literature review. Pediatrics 105:1335–1344
Magnus KG, Millar AJ, Sinclair-Smith CC, Rode H (1999) Intrahepatic fetus-in-fetu: a case report and review of the literature. J Pediatr Surg 34:1861–1864
Moorthy K, Rao PP, Deshpande AA, Thakur RK, Supe AN (1997) Fetus in fetu or a retroperitoneal teratoma—a controversy revisited. A case report and review of literature. Indian J Cancer 34:179–181
Thakral CL, Maji DC, Sajwani MJ (1998) Fetus-in-fetu: a case report and review of the literature. J Pediatr Surg 33:1432–1434
Spencer R (2001) Parasitic conjoined twins: external, internal (fetuses in fetu and teratomas), and detached (acardiacs). Clin Anat 14:428–444
Lende G, Wendemu W, Mork S, Wester K (2007) A girl with spina bifida, an extra leg, and ectopic intestinal loops—a “foetus in foetu” or a whim of the neural crest? Acta Neurochir (Wien) 149:1071–1075
Humphreys RP, Manwaring KH, Carroll NC (1991) Accessory arm—dysraphism or disparity? Case report. J Neurosurg 74:297–300
Spencer R (2000) Theoretical and analytical embryology of conjoined twins: part II: adjustments to union. Clin Anat 13:97–120
Kingston CA, McHugh K, Kumaradevan J, Kiely EM, Spitz L (2001) Imaging in the preoperative assessment of conjoined twins. Radiographics 21:1187–1208
Albert G, Campos M, Menezes A, Vogel T, Weinstein S (2008) Rachipagus parasite associated with myelocystocele and diastematomyelia. Pediatr Neurosurg 44:418–421
Chadha R, Lal P, Singh D, Sharma A, Choudhury SR (2006) Lumbosacral parasitic rachipagus twin. J Pediatr Surg 41:e45–e48
Esenkaya S, Gurbuz B, Yalti S (2004) Asymmetric parasitic dicephalus conjoined twins. J Clin Ultrasound 32:102–105
Navaei AA, Habibi Z, Moradi E, Nejat F (2015) Parasitic rachipagus twins; report of two cases. Childs Nerv Syst 31:1001–1003
Ratan SK, Rattan KN, Magu S, Rohilla S, Purwar P, Mathur SK (2004) Thoracolumbar rachipagus parasite. Pediatr Surg Int 20:298–300
Ringo Y, Drake D, Sillo T, Lakhoo K (2012) Parasitic twin within spina bifida. Afr J Paediatr Surg 9:240–242
Sanoussi S, Rachid S, Sani CM, Mahamane B, Addo G (2010) Rachipagus: a report of two cases—thoracic and lumbar. J Surg Tech Case Rep 2:27–29
Snelling CM, Ellis PM, Smith RM, Rossiter JP (2008) Lipomatous lumbar mass with an attached digit and associated split cord malformation. Can J Neurol Sci 35:250–254
Solak A, Ergun S, Polat I, Sahin N, Genc B (2012) A rare form of heteropagus twinning: three-armed infant with spinal dysraphism. Case Rep Pediatr 2012:831649
Zhang J, Duan H, Zhang Y, Yi Z, Bao S (2011) Parasitic rachipagus conjoined twins with spina bifida, diplomyelia, scoliosis, tethered cord syndrome, and ventricular septal defect—case report. Neurol Med Chir (Tokyo) 51:736–739
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organisation or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Funding
This study received no financial support.
Patient consent
The guardian (father) has consented to the submission of this case report to the journal.
Rights and permissions
About this article
Cite this article
Sahlu, A., Mesfin, B., Tirsit, A. et al. Parasitic twin—a supernumerary limb associated with spinal malformations. A case report. Acta Neurochir 158, 611–614 (2016). https://doi.org/10.1007/s00701-016-2710-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-016-2710-y