Abstract
Background
Transsphenoidal endoscopic surgery has gained popularity in the last 2 decades and is becoming a standard technique for resection of pituitary adenomas. In contrast to their ENT colleagues, neurosurgical residents have practically no endoscopic experience when they reach the training stage for transsphenoidal procedures. We have developed an affordable method for repetitive training in endoscopic (and microscopic) work in a narrow channel, allowing training of the basic movements needed for resection of pituitary adenoma.
Methods
In collaboration with colleagues in the ENT Department, Cantonal Hospital St. Gall, and the Technical University of Zurich, a three-dimensional model of the nasal cavity was developed and patented. The Egghead model consists of a 3D synthetic reconstruction of the head nasal cavity and sphenoid sinus. A boiled egg represents the sella. For validation, 17 neurosurgical residents from the Department of Neurosurgery, University Hospital of Basel, and Department of Neurosurgery, Cantonal Hospital of St. Gall, St. Gall, Switzerland, and two experts performed a standardized procedure mimicking a transsphenoidal pituitary procedure by dissecting a corridor to the egg yolk and resecting it, respecting the surrounding egg white. This procedure was performed under both microscopic and video-endoscopic visualization. A score for the precision and speed of the surgical performance was developed and used.
Results
The model allows repetitive training of the resection of the egg yolk under sparing of the egg white after careful opening of the shell. The validation data showed a steeper learning curve using the endoscopic technique than performing the same task using the microscope. After three repetitions, the quality of resection was better with the endoscopic technique.
Conclusions
Our model, the Egghead, is affordable, offers tactile feedback and allows infinite repetitions in basic training for pituitary surgery. It can be used for training of advanced neurosurgical residents, who thus far have very few possibilities of acquiring endoscopic experience.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Simulation training models in neurosurgery are needed to improve the quality of care and decrease the financial burden [11, 10, 8, 2, 3, 9, 5, 13]. In the case of (endoscopic) transsphenoidal surgery for resection of pituitary adenomas, there are large differences in who performs this procedure and how. In many centers the operation is conducted solely by neurosurgeons. Others have teamed up with their ENT colleagues to improve their endoscopic experience, thus accelerating some of the operative steps as the rhinologist performs the transnasal approach rapidly and giving the team security in the manipulation of the endoscope itself during resection of the tumor [12]. In contrast to their ENT colleagues, most neurosurgical residents practically have neither endoscopic nor transsphenoidal experience when they reach the training stage for transsphenoidal procedures. In addition, the number of pituitary surgeries per center is relatively low compared to meningiomal surgery, for example. On the other hand, in North American teaching hospitals up to 20 % of cranial neurosurgery is performed through a transsphenoidal approach [19]. As manual skills should be trained as early and often as possible [23], a demand for transsphenoidal training models has been identified [19, 3]. We have developed an affordable physical simulation model, the Egghead, enabling repetitive training of transsphenoidal procedures through a narrow canal. Hereby we introduce the model and its first validation.
Methods and materials
Identification of required technical skills/performance metrics
Before developing and testing a cognitive task, analysis is needed to identify which steps and processes are necessary to perform the operation from the beginning to end. A basic list of technical requirements was published by Choudhury and colleagues for graduation in neurosurgical oncology [3]. Not all requirements apply to pituitary surgery as much as to other tumor resections. The skills that seemed most important to us to be possibly implemented in a simplified training model were positioning, opening, resecting, demonstrating capability with the use of surgical instruments including operating the microscope and endoscope, and identifying the interface between the tumor and normal tissue. Especially using an endoscope would be a new skill for our participants. Of course skills for controlling intraoperative bleeding and closure, as well as actual decision-making about the next action, are as important as those selected for the current validation study, but were left out of this model for developmental reasons.
Development of the model
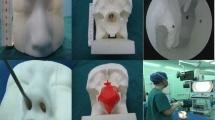
The first prototype for the Egghead model was made using cranial MRI images to carve the tunnel and pituitary space in Styrofoam, paying special attention to the dimensions of the canal and angle between the nostrils and sella, where a boiled egg was placed to simulate the pituitary gland and tumor. After that, in cooperation with Inspire® (Institute for Rapid Product Development, IRPD, ETH-Zurich), the actual Egghead model was developed using selective laser sintering (DTM Sinterstation 2500 plus) for the rigid components and PolyJet technology (3D printer, EOS P760) for the flexible components. The materials used were Duraform PA12 and Duraform Flex, respectively. Fixation of the egg was planned using 3D planning software. Two plug-ins were developed for chicken and quail eggs to vary the difficulty. The production cost of the model was around 2500 euros. Figure 1 shows the model and inlays.
Test setup
A chicken egg was placed in the model with the blunt end toward the nose. The opening was pre-stamped on the shell for standardization purposes. The participant was sitting in front of the head. The participants needed to adjust the microscope (Model OPMI MD, Leica Microsystems, Heerbrugg, Switzerland) or endoscope (Hopkins II Straight Forward Telescope 0°, pure HD CCU camera and image capture unit, Medical LCD flatscreen 19 inches, Karl Storz, Tuttlingen, Germany) by themselves. When operating with the endoscope the participant had the possibility to fix the endoscope into the holding system to enable bimanual manipulation. A standardized set of regular pituitary surgery instruments was pre-set.
Validation of the model
All residents of the Neurosurgical Departments of the Cantonal Hospital of St. Gall and University Hospital of Basel were asked to participate. None of them had performed endoscopic or transsphenoidal operations themselves, as both centers are low-volume centers for pituitary surgery. Each participant operated on seven eggs in two sessions. In the first session the first egg was the test egg operated on outside the model with the microscope and naked eye to develop an understanding of the expected task. The first egg in the model was operated on microscopically, the next endoscopically and so on. In the second session four eggs were operated on also alternating the microscopic and endoscopic techniques, always in the same order.
Performance metrics
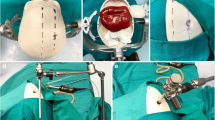
Three main simplified performance metrics were identified for the resection of pituitary adenomas: opening, resection and preservation of normal/healthy tissue. These were translated into opening the eggshell using a chisel, hammer and Cloward punches within standard margins (see Fig. 2a, b), resection of the egg yolk and preservation of the egg white, respectively. The surgical skills trained with the model are recognition of different tissues in depth and microsurgical preparation and manipulations in depth, in addition to using and getting used to switching from a 3D (microscope) to 2D view (endoscope).
a Pre-stamped rectangle on the egg showing the boundaries of the opening. b Opening with a Cloward punch, after the beginning had been performed with a chisel. c–d Endoscopic resection. e–g Microscopic resection. Notice the difference in width of the view between the endoscopic and microscopic techniques
Operation time was another performance metric: For logistical reasons the maximum operation time was set to 45 min per egg. Scoring was conducted by either author DE or AF as well as the trained study nurse. For additional post-hoc analysis, photos were taken of the split eggs.
As validated metrics for this neurosurgical procedure do not exist so far, the above-mentioned metrics were converted into a fictitious negative scoring system (see Table 1). Figure 2 shows representative resections of both endoscopic (c and d) and microscopic (e–g) experiments. Our concept of reliability and validity criteria for this model is listed in Table 2.
Statistics
A power analysis was not conducted because of the new metrics and number of residents available in these centers. The study that most closely resembles this study used 15 participants [7]. The Kruskal-Wallis test was used to compare subject-specific differences for time/scores between the two methods across three repetitions. P-values less than 0.05 were considered statistically significant. All analysis was performed in the R programming language [R Core Team, version 3.0.2 (2013)].
Results
In total, eight residents from St. Gall and nine from Basel completed both sessions of the test. Due to a change of residents more than the planned 15 could be included. An analysis between the St. Gall and Basel groups showed a significant difference in operation time, but not in the other metrics. Consequently, the data shown below are medians of all participants. Two experienced pituitary surgeons, one using the endoscopic technique and the other the microscope technique, were used as references.
Opening
The opening of the eggshell within the margins did not show a significant learning effect.
Resection
The resection of the egg yolk showed a decrease of 4 points between the first (median 13, range 1–16) and second test (median, 9, range 0–16) and a further statistically insignificant decrease of 1 point between the second and third (median 8, 0–16) test using the microscope (p = 0.02 and p = 0.2, respectively). Overall the egg yolk resection score was on average 5 lower with endoscopy (median 7, range 0–16) than with microscopy (median 12, range 0–16; p < 0.0001) (see Fig. 3a). This suggests that using the known microscopic technique fewer learning effects were observed and that even using the new endoscopic technique the residents benefited from the larger angle of view.
Comparison of scores within and between the microscopic (red) and endoscopic (blue) techniques. The expert value has been inserted as a line (microscopic red line, endoscopic blue line) in all graphs. a Resection of egg yolk (° ■ # are significant between the microscopic and endoscopic technique; * is significant within the microscopic technique). b Preservation of egg white (° is overall significant difference between the microscopic and endoscopic technique). c Operation time (no significant differences). d Total score of opening, resection and preservation (° is overall significant difference between the microscopic and endoscopic technique)
Preservation
The preservation of egg white, symbolizing preservation of normal surrounding tissue, did not show a statistically significant difference in microscopy among the first (median 2, range 0–6), second (median 2, range 0–8) and third test (median 2, range 0–6) (second test vs. first test: p = 0.8; third test vs. second test: p = 0.7). However, egg white preservation with endoscopy (median 3, range 0–8) was about 1 point higher on average than with microscopy (median 2, range 0–6, p = 0.003) (see Fig. 3b). This suggests that using the new endoscopic method interfered with available fine surgical motoric performance.
Operation time
Operation time showed a slight reduction using the microscope only between the first (median 45, range 29–45) and second test (median 42.5, range 22–45; p = 0.08) and increased again slightly in the third test (median 45, range 18–45; p = 0.7). With the endoscope, the new technique for all residents, time was slightly but not statistically significant longer by an average of 3 min (endoscope: median 42, range 22–45; microscope: median 42, range 18–45; p = 0.02; see Fig. 3c). This suggests that the cutoff of 45 min was not adequately chosen for this test.
Total score
The total score for opening, resecting the egg yolk and preserving the egg white showed a reduction in microscopy between the first (median 16, range 3–21) and second test (median 12, range 3–19; p = 0.003) and a further statistically insignificant reduction by 0.5 between the second and third test (median 11.5, 2–20; p = 0.09). The use of the endoscope (median 12, 2–21) was associated with a 2-point lower total score compared with the microscope (median 14, 4–21; p = 0.0005; see Fig. 3d). This suggests that the endoscopic technique has benefits due to the wider angle of view, even though this was the technique in which the participants had no previous experience.
Discussion
The presentation and validation of this basic physical simulation Egghead model for training in transsphenoidal pituitary surgery with both a microscope and endoscope show a significant learning curve in the resection rate. Thereby, this is the first model that could be validated for the basic performance metrics in transsphenoidal pituitary surgery. Last but not least the model is affordable.
In comparison to other published simulation models for pituitary surgery [19, 15], our model is a basic model for training in the first steps in pituitary surgery. The model of Okuda and colleagues is very similar but uses soft-boiled or raw eggs with a fluid egg yolk. They did not fixate the egg within the model. This is probably more suitable for advanced trainees [15]. The model is probably also affordable. Changes in our test, such as drilling the opening instead of chiseling, hammering and using Cloward punches and using raw eggs or smaller quail eggs, can make our model more challenging for the advanced trainee as well. A preliminary validation of the Okuda model was conducted with five trainees and showed that training on a model facilitates improvement of the surgical techniques needed for endoscopic endonasal transsphenoidal surgery [16].
The model of Rosseau and colleagues is a virtual reality (VR) simulation model, enabling training and testing of more performance metrics than in our basic model, such as (unexpected) bleeding and closure [19]. The model is assumably less self-explanatory, which makes the presence of a technical or teaching person mandatory. In contrast to other VR models, this model does have haptic feedback. Costs of development and production as well as software updates are probably much higher than for our physical model. A validation has not been published yet.
Other training alternatives are cadaveric workshops, which are relatively rare and expensive and do not allow the necessary repetitive training [4]. The advantage of such a course is the availability of the real and more detailed anatomy. However, training in complicated situations such as hemostasis or closing CSF fistulas is not possible.
Specific training in how to use an endoscope has been described in other studies, however not in transsphenoidal neurosurgery [22, 1].
Validation
All participants started with the microscopic technique, in which all had experience. This could be considered an impure method because the first microscopic is also a learning tool for the endoscopic test. However, as all participants performed the test the same way, this bias should have been minimized in the end. There was a standard explanation at the beginning of the test and a minimum of didactics during the test. For actual training of residents and not only validation of a model, the didactic component should play a major role, as mentioned before [10].
Our validation results show that there is a difference between the familiar microscopic and the new endoscopic technique. A trend toward faster learning is shown by a steeper egg yolk in the endoscopic graph. However, the resection rate was immediately better with the endoscope. This was probably due to the better range of vision with an endoscope. Preservation of the ‘normal tissue’ was worse in the endoscopic tests, showing that three repetitions is not enough to be as good at fine tasks with a microscope. In our opinion, this underlines the necessity of repeated training.
The opening of the eggshell did not show a learning curve. Possible reasons for this are the technique of using a chisel, hammer and Cloward punches. Using the chisel and hammer was a technique most residents had never used before, but fine-tuning of the opening was done with Cloward punches, which are often used in spinal procedures. The egg shell breaks relatively easily into larger fragments compared to human bone, making the need for positioning of the Cloward punches much more important than in spinal cases. Training in opening with a diamond drill might be a better approach for future training modifications.
Operation time differed significantly between the two groups of residents. There is no clear explanation for this. All participants were told they had a maximum of 45 min for each egg. Possibly the motivation for prestige differed between both groups.
Some residents outperformed the experts (shown in Fig. 3). This is best explained by evidence from laparoscopic studies. Ou et al. (2013) showed that video game experience improves laparoscopic skills [17]. This was especially true for games with high video spatial elements, which improve laparoscopic skills in terms of completion time, efficiency and fewer errors [21]. Some authors even found that past and present video game experience was a superior predictor of laparoscopic skills compared to the level of training [20]. The influence of video game experience has also been demonstrated for open surgery [14]. As the trainees in our experiment belong to a younger generation, several of them might have regular experience in video games, which could at least partially explain their better performance.
Limitations
As the two groups were rated by two different raters, recording every test on video instead of taking photos of the egg cut in half at the end of the test would have enabled better inter-rater variability checks. In addition, learning from watching your own videos is advantageous [6].
From a statistical point of view, a power calculation was necessary. The design of the study was planned as closely as possible to known criteria for such validation studies [18, 7]. A true power calculation was not possible as new metrics were used, and a limited number of participants was available.
As described earlier, the inability to detect and handle unexpected complications makes this model less close to reality.
Suggested future research
More research toward disassembling neurosurgical procedures steps and forming them into measurable and objective metrics is necessary in order to improve both the quality and efficacy of neurosurgical training. Also, measuring performance during the transition between model training and actual cases in comparison to the traditional way of learning should be tested.
Conclusion
The Egghead model shows that it is possible to train the neurosurgical skills needed for transsphenoidal endoscopic and microscopic pituitary surgery in an affordable and repetitive way.
References
Bakker NH, Fokkens WJ, Grimbergen CA (2005) Investigation of training needs for functional endoscopic sinus surgery (FESS). Rhinology 43(2):104–108
Burchiel K (2013) Commentary: simulation training in neurological surgery. Neurosurgery 73(4):6–7
Choudhury N, Gélinas-Phaneuf N, Delorme S, Del Maestro R (2013) Fundamentals of neurosurgery: virtual reality tasks for training and evaluation of technical skills. World Neurosurg 80(5):e9–e19
Csókay A, Papp A, Imreh D, Czabajszky M, Valálik I, Antalfi B (2013) Modelling pathology from autolog fresh cadaver organs as a novel concept in neurosurgical training. Acta Neurochir (Wien) 155(10):1993–1995
Dagi TF (2013) Commentary: the roles and future of simulation in neurosurgery. Neurosurgery 73(Suppl 1 (4)):S4–S5
Dahmen U, Sänger C, Wurst C, Arlt J, Wei W, Dondorf F, Richter B, Settmacher U, Dirsch O (2013) Video-based self-control in surgical teaching. A new tool in a new concept. Chirurg 84(10):851–858
Francis HW, Masood H, Laeeq K, Bhatti NI (2010) Defining milestones toward competency in mastoidectomy using a skills assessment paradigm. Laryngoscope 120(7):1417–1421
Gasco J, Holbrook TJ, Patel A et al (2013) Neurosurgery simulation in residency training: feasibility, cost, and educational benefit. Neurosurgery 73(Suppl 1(4)):S39–S45
Gélinas-Phaneuf N, Del Maestro RF (2013) Surgical expertise in neurosurgery: integrating theory into practice. Neurosurgery 73(Suppl 1(4)):S30–S38
Harrop J (2013) Introduction to neurosurgical simulation. Neurosurgery 73(Suppl 1(4)):S8
Harrop J, Lobel DA, Bendok B, Sharan A, Rezai AR (2013) Developing a neurosurgical simulation-based educational curriculum: an overview. Neurosurgery 73(Suppl 1(4)):S25–S29
Jagannathan J, Laws E, Jane J (2012) Advantage of the endoscope and transitioning from the microscope to the endoscope for endonasal approaches. In: Kassam AB, Gardner PA (eds) Endosc. Approaches to skull base. Karger, Basel, pp pp 7–pp 20
Limbrick DD, Dacey RG (2013) Simulation in neurosurgery: possibilities and practicalities: foreword. Neurosurgery 73(Suppl 1(4)):S1–S3
Lynch J, Aughwane P, Hammond TM (2010) Video games and surgical ability: a literature review. J Surg Educ 67:184–189
Okuda T, Kataoka K, Kato A (2010) Training in endoscopic endonasal transsphenoidal surgery using a skull model and eggs. Acta Neurochir (Wien) 152(10):1801–1804
Okuda T, Yamashita J, Fujita M, Yoshioka H, Tasaki T, Kato A (2014) The chicken egg and skull model of endoscopic endonasal transsphenoidal surgery improves trainee drilling skills. Acta Neurochir (Wien) 156(7):1403–1407
Ou Y, McGlone ER, Camm CF, Khan OA (2013) Does playing video games improve laparoscopic skills? Int J Surg 11(5):365–369
Reznick R, Regehr G, MacRae H, Martin J, McCulloch W (1997) Testing technical skill via an innovative “bench station” examination. Am J Surg 173(3):226–230
Rosseau G, Bailes J, Del Maestro R et al (2013) The development of a virtual simulator for training neurosurgeons to perform and perfect endoscopic endonasal transsphenoidal surgery. Neurosurgery 73(Suppl 1):S85–S93
Rosser JC, Lynch PJ, Cuddihy L, Gentile DA, Klonsky J, Merrell R (2007) The impact of video games on training surgeons in the 21st century. Arch Surg 142(2):181–186, discusssion 186
Schlickum MK, Hedman L, Enochsson L, Kjellin A, Felländer-Tsai L (2009) Systematic video game training in surgical novices improves performance in virtual reality endoscopic surgical simulators: a prospective randomized study. World J Surg 33(11):2360–2367
Tasman A, Wallner F, Kolling G, Stammberger H (1998) Is monocular perception of depth through the rigid endoscope a disadvantage compared to binocular vision through the operating microscope in paranasal sinus. Am J Rhinol 12:87–91
Voelcker-Rehage C (2008) Motor-skill learning in older adults—a review of studies on age-related differences. Eur Rev Aging Phys Act 5(1):5–16
Acknowledgments
This project was funded by the Clinical Trials Unit Commission of the Canton of St. Gall, Switzerland. The authors thank Karl Storz® for providing the endoscopic setup. The authors also thank Prof. Rachel Rosenthal, Department of Surgery, Basel University, for input on training models in surgery and Karin Inauen, BSc, for assistance during the experiments.
Conflict of interest
The authors declare that they have no conflict of interest. The services of Inspire AG (Schindel and Schmidt) for cooperation with development and production were reimbursed at regular rates.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comment
This is an interesting article describing an affordable training model for endoscopic transsphenoidal surgery—this could easily be incorporated into any neurosurgical training program. It seems a very good introduction to endoscopic neurosurgery in general. The methodology of the study is sound. It will be interesting in the future to gain more insight into the value of the type of practical technical skill training in neurosurgery and whether such training tools can be used to judge the aptitude of the individual trainee for certain types of procedures. It is indeed interesting that some of the trainees outperformed the experts, even though they had no previous hands-on experience with the surgical technique. It might well be that this is because the generation of upcoming neurosurgeons has spent more time playing video games, as suggested by the authors. Therefore, we need to consider the indications of such results. Should there be a change of guard where the older "non-video game" generation steps aside and lets the best man or woman do the job—or should we spend a bit more time playing video games? As funny as this might seem, it is always worth considering how we can assure that operations are always performed by the best possible technician in the unit.
Jannick Brennum
Copenhagen,Denmark
Rights and permissions
About this article
Cite this article
Engel, D.C., Ferrari, A., Tasman, AJ. et al. A basic model for training of microscopic and endoscopic transsphenoidal pituitary surgery: the Egghead. Acta Neurochir 157, 1771–1777 (2015). https://doi.org/10.1007/s00701-015-2544-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-015-2544-z