Abstract
Background
The prevalence of ivy sign on fluid-attenuated inversion recovery (FLAIR) imaging in patients with asymptomatic moyamoya disease is unclear. The aim of this study was to clarify the incidence of ivy sign in these patients, as well as the correlation between MRI and 15O gas PET findings.
Methods
A retrospective analysis including 16 consecutive patients with asymptomatic moyamoya disease enrolled between 2001 and 2010 in a single center. FLAIR imaging at the initial visit was categorized as ivy sign present, negative, or equivocal. Hemodynamic and metabolic parameters were quantified in 11 of 16 patients by 15O-gas positron emission tomography, and the relationship between ivy sign and 15O-gas PET parameters was analyzed. Cerebrovascular events within the follow-up period (54 ± 28 months) were also examined.
Results
Five of 16 asymptomatic moyamoya patients (31.3 %) had positive ivy sign (6/30 hemispheres, 20 %). In 15O-gas PET examinations, 18 % of 22 hemispheres had elevated oxygen extraction fraction values that were significantly associated with positive ivy sign. Of these 16 asymptomatic moyamoya patients, six patients (37.5 %) underwent combined surgical revascularization. In this series, no patients experienced ischemic stroke, but one had intraventricular bleeding 1 year after surgery.
Conclusions
Ivy sign on FLAIR imaging is still not rare in patients with moyamoya disease, even when asymptomatic. Although optimal management is still under debate, ivy sign may be an indicator of misery perfusion, and patients with asymptomatic moyamoya disease and ivy sign on FLAIR imaging will benefit from more careful follow-up.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Moyamoya disease is characterized by a progressive occlusion of the terminal portions of both internal carotid arteries with formation of an abnormal collateral vascular network at the base of the brain [22]. Recent imaging research on moyamoya disease has focused on cerebral hemodynamics as predictors of cerebrovascular events and peri-operative complications in patients considering revascularization [19]. Thus, there is growing evidence that enables us to assess cerebral hemodynamic status, such as with fluid-attenuated inversion-recovery (FLAIR) MR imaging [15], 15O-gas positron emission tomography (PET), and perfusion imaging, as well as cerebrovascular reactivity measured by arterial spin labeling and blood oxygen level-dependent MRI [17]. Of these, the ivy sign was first reported as a unique characteristic of the pial network observed in moyamoya disease on post-contrast T1-weighted MRI [18], and was also known to be demonstrated on FLAIR images [15]. The ivy sign is useful as an indirect indicator of hemodynamic status of the leptomeningeal collateral pathways in moyamoya disease [9], but it is still unclear how frequently this sign is seen in asymptomatic moyamoya patients. A recent multicenter, nationwide survey in Japan revealed that asymptomatic moyamoya disease was not rare, in addition to being associated with severely impaired cerebral hemodynamics in 10 % of involved hemispheres [12]. The present study examines the incidence of ivy sign in patients with asymptomatic moyamoya disease. Our aim is to understand more thoroughly the incidence and importance of ivy sign in patients with asymptomatic moyamoya disease and to further study the correlation of this imaging change with a sophisticated isotopic assessment of cerebral blood flow and metabolism.
Patients and methods
Patients
This retrospective study included 22 (8.6 %) of 256 consecutive patients with moyamoya disease whom we treated between 1980 and 2011 at Hokkaido University Hospital. All of the 22 patients first visited us between 2001 and 2010, were Japanese adults, and met the criteria for asymptomatic moyamoya disease [12]. All were free from previous ischemic or hemorrhagic stroke episodes and without neurologic deficit. Of these 22 patients, FLAIR images at first visit were available for 16. Therefore, 16 patients of whom two had unilateral disease (total 30 hemispheres) were included in the analysis. Patient demographics and clinical data are shown in Table 1; four patients were male and 12 were female (mean age, 46.2 ± 9.4 years). Fourteen the of 16 were considered as having definitive moyamoya disease. The rest were considered as probable cases, but not as quasi-moyamoya disease, because no underlying diseases were present, such as atherosclerosis, autoimmune disease, post-irradiation or other. Clues to the diagnosis were as follows: other organ disease, history of tension-type headache, brain health check-up, screening due to family history, and minor head trauma. Because there is no set guideline for management of asymptomatic moyamoya disease, decisions for surgical or nonsurgical management were made for individual patients based on radiological results including hemodynamic findings and other considerations. All patients were followed up with regular, repeat MRI/MRA examinations. This study was approved by the institutional review board at Hokkaido University Hospital.
Radiological examinations
Of 16 patients, 12 underwent cerebral angiogram for the diagnosis of moyamoya disease. The rest were diagnosed using MRI and MRA. Four patients chose not to have angiography. MRI and MRA were performed using a Siemens Magnetome Symphony 1.5-T scanner (Siemens). FLAIR images were obtained with a fast inversion recovery sequence with a repetition time of 9,000 ms, an effective echo time of 114 ms, and an inversion time of 2,500 ms. Image thickness, gap, and matrix were 5.0 mm, 1.5 mm, and 256 × 192, respectively. Three-dimensional time of flight MRA was obtained with a repetition time of 26 ms, echo time of 7.15 ms, and flip angle 20°. Slice thickness, field of view, number of slices, and acquisition matrix were 0.7 mm, 210 mm, 180 images (without any spacing), and 512 × 187, respectively. No contrast agents were used. 15O-gas PET was performed in 11 (69 %) patients at initial diagnosis, and cerebral blood flow (CBF), cerebral blood volume (CBV), cerebral metabolic rate of oxygen (CMRO2), and oxygen extraction fraction (OEF) were determined as previously described [6, 14].
Image analysis and clinical follow-up
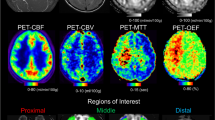
The ivy sign on FLAIR imaging is defined by areas of increased signal intensity in the leptomeninges and perivascular spaces [15], but it has been termed and classified variably in various reports [1, 5, 9, 11, 16, 23]. In the present study, three investigators (SV, MI and KK) reviewed FLAIR images and ivy sign was defined in accordance with recent reports [9] as any area of continuous linear or punctate, high signal intensity along the cortical sulci and subarachnoid space. Investigators rated the ivy sign in each hemisphere by consensus as positive, negative, or equivocal (Figs. 1, 2 and 3). Equivocal ivy sign was defined as more subtly elevated signal intensity along the cortical sulci [9]. The disease stage was also evaluated by MRA staging [8]. Ten-millimeter-diameter circular regions of interest (ROIs) were drawn on ipsilateral regions where ivy sign was observed, except for in infarct areas, on 15O-gas PET images from each of the 11 patients (22 hemispheres). Control PET values were obtained from normal volunteers: CBF, 44 ± 4 mL/100 g/min; CBV, 3.4 ± 0.5 mL/100 g; CMRO2, 3.3 ± 0.3 mL/100 g/min and OEF, 0.40 ± 0.05 (mean ± SD) [6]. Any values less than mean −2SD were considered decreased and those more than mean + 2SD were considered increased, as previously described [6].
A 47-year-old female with asymptomatic moyamoya disease and positive ivy sign. FLAIR images at initial diagnosis showed obvious linear or punctate high signal intensity along the cortical sulci and subarachnoid space within the bilateral ACA and MCA regions (a, arrows). 15O-gas PET showed decreased CBF, increased CBV, and elevated OEF in the bilateral frontal lobes (b). CMRO2 was similar to controls (b). Scale bar = 50 mm
A 42-year-old female with asymptomatic moyamoya disease and equivocal ivy sign. FLAIR images at diagnosis showed more subtle punctate high signal intensity in the subarachnoid space within bilateral MCA regions (a, arrows). 15O-gas PET showed increased CBV in bilateral frontal lobes (b). Scale bar = 50 mm
Finally, all ischemic and hemorrhagic stroke events within the mean follow-up period of 54.3 months were recorded and precisely analyzed. In addition, we reviewed FLAIR images and determined the presence of ivy sign at the latest follow-up in each hemisphere.
Statistical analysis
Continuous variables were expressed as mean ± SD. Statistical analysis was performed using Chi-square or Fisher’s exact test for independent variables and one-way ANOVA followed by Bonferroni’s test for multiple comparisons as appropriate. Statistical significance was set at P < 0.05 for Chi-square or Fisher’s exact test and P < 0.01 for Bonferroni’s test. Statistical analysis was completed with Ekuseru-Toukei 2012® (Social Survey Research Information Co., Ltd., Tokyo, Japan).
Results
Ivy sign in asymptomatic moyamoya disease
Examiners reported positive ivy sign on FLAIR images in five (31.3 %) of 16 asymptomatic patients (6/30 involved hemispheres [20 %]), equivocal ivy sign in 11 of 30 hemispheres (36.7 %), and negative ivy sign in five (31.3 %) patients (13/30 involved hemispheres [43.3 %]) (Table 1). Positive or equivocal ivy signs were present in three anterior cerebral artery (ACA) regions, 17 middle cerebral artery (MCA) regions, and three posterior cerebral artery (PCA) regions. MRI detected cerebral infarct in five (16.7 %) of 30 involved hemispheres. There was no gross intracerebral hemorrhage, only cerebral microbleeds on T2*-weighted images. There were two of 30 hemispheres (6.7 %) with MRA grade 1 disease, 11 (36.7 %) with grade 2, nine (30 %) with grade 3, and eight (26.7 %) with grade 4. There were no significant correlations between ivy sign and cerebral infarct (3 × 2 contingency table, P = 0.577), nor the MRA staging (3 × 4 contingency table, P = 0.351).
Ivy sign and 15O-gas PET parameters
The 15O-gas PET parameters, including CBF, CBV, CMRO2, and OEF were quantitatively determined for a total of 88 ROIs in 22 involved hemispheres. As most ivy signs on FLAIR images in this study were observed in the ACA and MCA regions, most of the assigned ROIs in this study were located within these areas. As shown in Table 2, when analyzed in relation to ivy sign in each hemisphere, OEF was significantly elevated in 4/5 hemispheres with positive ivy sign. On the other hand, OEF was similar to control values in one hemisphere with positive ivy sign, and in 17 hemispheres with equivocal or negative ivy sign. Thus, we estimated a rate of misery perfusion of 18 % among the hemispheres examined. There was significant correlation between the presence of ivy sign and OEF elevation in cases included in this study (3 × 2 contingency table, P < 0.001). Furthermore, CBV was significantly increased in 4/5 ivy sign-positive hemispheres and 8/9 equivocal hemispheres, while it remained close to controls in 7/8 ivy sign-negative hemispheres. Thus, there was also significant correlation between the presence of ivy sign and CBV increase (P = 0.004). Moreover, as shown in Fig. 4, OEF was significantly elevated in hemispheres with positive ivy sign compared to those without (P = 0.0099, 0.50 ± 0.09 for positive, 0.40 ± 0.07 for equivocal and 0.38 ± 0.07 for negative ivy sign; respectively). Consistently, CBF was significantly decreased in the hemispheres with positive ivy sign (P = 0.0064, 34 ± 5 for positive, 40 ± 7 for equivocal and 47 ± 9 for negative ivy sign; respectively). CMRO2 in the positive ivy sign group was comparable to other groups and controls, suggesting that misery perfusion [2] or stage II ischemia [20] was more frequent in hemispheres with obviously positive ivy signs.
Scatter plots showing the relationship between ivy sign on FLAIR images and cerebral blood flow and oxygen metabolism parameters determined by 15O-gas PET in 22 involved hemispheres with asymptomatic moyamoya disease. OEF were significantly higher in hemispheres with positive ivy signs than other groups (P = 0.0099). CBV was significantly higher in hemispheres with equivocal ivy sign (P = 0.0036) than in those with negative ivy sign. CBF were significantly lower in hemispheres with positive ivy sign (P = 0.0064). There were no significant differences in CMRO2 among the three groups
Cerebrovascular events
A total of 16 patients were managed and followed up with repeated and regular MRI/MRA examinations for a mean of 54.3 months. During this time, six patients with eight involved hemispheres underwent combined direct and indirect revascularization (STA-MCA and EDAMS or EDMAPS) [7, 13]. As mentioned above, there were no guidelines to recommend surgical revascularization for patients with asymptomatic moyamoya disease. Therefore, we presented a choice of surgical revascularization to the patients with ivy sign and/or signs of hemodynamic impairment. As a result, six patients with ivy sign or signs of hemodynamic impairment underwent combined revascularization for moyamoya disease. Of these, one patient (case 11) with unilateral disease and a positive ivy sign within the ipsilateral MCA territory in the involved hemisphere had intraventricular bleeding on the ipsilateral side during the postoperative follow-up. This patient did not undergo 15O-gas PET study but underwent single photon emission tomography (SPECT) to determine the regional CBF and cerebral vascular reactivity to acetazolamide preoperatively. One year after revascularization surgery, she delivered a baby and then presented with intraventricular hemorrhage during labor and delivery. FLAIR imaging at this time demonstrated equivocal ivy sign in the ipsilateral MCA territory. In addition, an MR angiogram revealed that STA-MCA bypass was clear, whereas development of surgical collaterals through indirect bypass was unknown. The patient was managed medically except for ventricular drainage and discharged independently within 1 month. No patients experienced ischemic stroke during the follow-up period in this series. As shown in Table 3, positive ivy signs were still present in four (67 %) of six hemispheres at the latest point of follow-up, whereas positive ivy sign in the remaining two hemispheres were assessed as negative after revascularization surgery. In one patient (Case 11) who was mentioned above, disease progression was observed in the right hemisphere. Negative ivy sign in the right hemisphere in case 11 was assessed to be positive at the latest follow-up period.
Discussion
The principal finding of this study was the observation of an ivy sign on FLAIR images in 31.3 % of patients with asymptomatic moyamoya disease. Ivy sign was noted in 20 % of all involved hemispheres. To our knowledge, this is the first published case series to analyze the presence of ivy sign in patients with asymptomatic moyamoya disease. Recently, the increasing availability of advanced noninvasive cerebral imaging techniques has indicated that the prevalence of asymptomatic moyamoya disease is much higher than would have been suspected previously [12], although there are not yet any prospective cohort or randomized studies regarding epidemiology, clinical features, radiological findings, and natural history of asymptomatic moyamoya disease. In a historical prospective cohort study of radiological findings, clinical course, and outcomes in Japanese individuals with indicators of asymptomatic moyamoya disease, Kuroda et al. [12] uncovered silent cerebral infarct in almost 20 % of 77 involved hemispheres and cerebral blood flow measurements suggested that 10 % of 70 hemispheres had markedly reduced cerebral perfusion pressures. Microbleeds on T2*-weighted images and ivy sign on FLAIR images were not assessed in that study. Since ivy sign was first reported on FLAIR images in 1999, studies have suggested the presence of ivy sign on FLAIR images in 41–66 % of involved hemispheres, in patients with moyamoya disease, particularly with ischemic symptoms [5, 9–11, 23]. Therefore, our study is the first to specifically detail the incidence of ivy sign in asymptomatic adults with moyamoya disease, although Sanossian et al. have reported that ivy sign is not seen on FLAIR imaging in uninvolved hemispheres contralateral to cerebral ischemia [21]. We believe that the rate of occurrence of ivy sign in FLAIR images is high in moyamoya patients regardless of ischemic symptoms, and that the sign can still be used as an indirect indicator of moyamoya disease as previously reported [9, 18].
Another important finding of this study was the indication of misery perfusion in 18 % of the hemispheres (n = 22) examined by 15O-gas PET. There was significant correlation (P < 0.001) between ivy sign and OEF elevation (Table 2). Moreover, OEF was significantly elevated in hemispheres with ivy sign compared to those without (P = 0.0099, Fig 4). These results indicate that misery perfusion or stage II ischemia is more frequently observed in hemispheres with obviously positive ivy sign. This is the first report that demonstrates significant correlation between ivy sign and misery perfusion. Moreover, this significant correlation is consistent with previous studies that demonstrated the relationship between the presence of ivy sign and impaired hemodynamic status measured by SPECT [9–11, 16]. Misery perfusion or stage II ischemia determined by elevated OEF in PET examinations is regarded as an indicator of critical reductions of cerebral perfusion pressure [2, 20]. Disease stage of moyamoya disease was known to have no correlation with cerebral hemodynamic status but to indicate the compensatory nature of moyamoya disease [4]. Therefore, positive ivy sign on FLAIR images may indicate a reduction of arterial blood flow velocity in leptomeningeal brain vessels. Past studies have discussed three main mechanisms of the ivy sign on FLAIR images [5, 9–11, 15, 16, 23], including slow retrograde flow of engorged pial arteries via leptomeningeal anastomosis [5, 15], maximally dilated pial vasculature compensating for decreased perfusion pressure [9–11, 16], and congestive thickening of the leptomeninges [15]. Ideguchi et al. [9] compared ivy sign findings on FLAIR with perfusion SPECT images before and after bypass surgery and demonstrated that cerebrovascular reactivity was significantly decreased in the area with the ivy sign compared to the area without it, while the ivy sign disappeared or decreased after bypass surgery in areas with improved blood flows. Mori [16] and Kawashima et al. [10, 11] also investigated the relationship between degree, asymmetry, and presence of ivy sign on FLAIR images and the severity of ischemic symptoms or hemodynamic status on SPECT and have shown that ivy sign was associated with impaired hemodynamic status. They speculated that the ivy sign on FLAIR images largely reflected the maximally dilated pial vasculature compensating for impaired cerebrovascular reactivity. Our findings on 15O-gas PET were consistent with these previous FLAIR and SPECT studies and also supported the theory that ivy sign on FLAIR indicates maximal dilatation of pial vasculature in response to reduced cerebral blood flow.
In this series, no patients experienced ischemic stroke, although there were three patients both with positive ivy sign and with elevated OEF. Of these three patients, one patient (case 8) underwent combined revascularization surgery. At the latest follow-up point, we confirmed both the disappearance of ivy sign and the recovery of OEF. The other two patients (cases 10 and 14) did not undergo revascularization surgery. This might not be consistent with previous studies that have proven elevated OEF to be an independent risk factor for subsequent ischemic stroke in patients with occlusive carotid artery disease [2, 14, 20]. As Derdeyn et al. have pointed out, the presence of normal CBV in patients with increased OEF may reflect preserved autoregulatory capacity [3]. Thus, one of our patients (case 14) with elevated OEF and normal CBV might have had a preserved autoregulatory capacity. The other patient (case 10) with positive ivy sign, elevated OEF and CBV increase has been treated nonsurgically and remains stroke-free for 2 years. This result suggests that further prospective studies may be necessary to identify an optimal management strategy for asymptomatic patients with moyamoya disease, as already noted [12].
The present data contains precise information regarding FLAIR ivy sign, its chronological change, cerebral infarct and disease stage on MRI, as well as cerebral blood flow and metabolism measured by 15O gas-PET and clinical course. Therefore, it may slightly be confusing to interpret at first why, in this study, certain patients underwent surgery and others did not. However, there were no guidelines and evidence to recommend revascularization surgery to patients with asymptomatic moyamoya disease, although we believe patients with ivy sign and elevated OEF should be presented a choice of revascularization to prevent ischemic stroke. Therefore, there were no contradictions in our clinical results in which certain patients with asymptomatic moyamoya disease underwent surgery and others did not. We believe that some important data are revealed here, which will provoke further study and clinical correlation by researchers in this field. The study may only have made a valiant start at studying these imaging phenomena.
The present study was limited by the very small number of patients, short follow-up period, and retrospective nature. Moreover, ivy sign on FLAIR images was determined qualitatively. The qualitative nature of FLAIR ivy sign might not be able to simply replace positive ivy sign by OEF findings. The present study only suggests that ivy sign may indicate misery perfusion, and may be useful as an indirect indicator of the hemodynamic status of leptomeningeal collateral pathways in moyamoya disease. Therefore, a prospective cohort or randomized controlled study is warranted in a larger population of asymptomatic patients to confirm the present findings and their clinical implications and to establish the optimal management of asymptomatic or incidental moyamoya disease.
In conclusion, it appears that ivy sign is not rare on FLAIR images in patients with moyamoya disease, even when asymptomatic. Ivy sign may indicate misery perfusion, and may be useful as an indirect indicator of the hemodynamic status of leptomeningeal collateral pathways in moyamoya disease. Although the natural history and optimal direction of management of asymptomatic moyamoya disease remains undecided, it is possible that these patients will benefit from more careful follow-up when ivy sign is detected at initial diagnosis.
References
Azizyan A, Sanossian N, Mogensen MA, Liebeskind DS (2011) Fluid-attenuated inversion recovery vascular hyperintensities: an important imaging marker for cerebrovascular disease. AJNR Am J Neuroradiol 32:1771–1775
Baron JC, Bousser MG, Rey A, Guillard A, Comar D, Castaigne P (1981) Reversal of focal “misery-perfusion syndrome” by extra-intracranial arterial bypass in hemodynamic cerebral ischemia. A case study with 15O positron emission tomography. Stroke 12:454–459
Derdeyn CP, Videen TO, Yundt KD, Fritsch SM, Carpenter DA, Grubb RL, Powers WJ (2002) Variability of cerebral blood volume and oxygen extraction: stages of cerebral haemodynamic impairment revisited. Brain 125:595–607
Fujimura M, Tominaga T (2012) Lessons learned from moyamoya disease: outcome of direct/indirect revascularization surgery for 150 affected hemispheres. Neurol Med Chir (Tokyo) 52:327–332
Fujiwara H, Momoshima S, Kuribayashi S (2005) Leptomeningeal high signal intensity (ivy sign) on fluid-attenuated inversion-recovery (FLAIR) MR images in moyamoya disease. Eur J Radiol 55:224–230
Hokari M, Kuroda S, Shiga T, Nakayama N, Tamaki N, Iwasaki Y (2008) Combination of a mean transit time measurement with an acetazolamide test increases predictive power to identify elevated oxygen extraction fraction in occlusive carotid artery diseases. J Nucl Med 49:1922–1927
Houkin K, Ishikawa T, Yoshimoto T, Abe H (1997) Direct and indirect revascularization for moyamoya disease surgical techniques and peri-operative complications. Clin Neurol Neurosurg 99(Suppl 2):S142–S145
Houkin K, Nakayama N, Kuroda S, Nonaka T, Shonai T, Yoshimoto T (2005) Novel magnetic resonance angiography stage grading for moyamoya disease. Cerebrovasc Dis 20:347–354
Ideguchi R, Morikawa M, Enokizono M, Ogawa Y, Nagata I, Uetani M (2011) Ivy signs on FLAIR images before and after STA-MCA anastomosis in patients with Moyamoya disease. Acta Radiol 52:291–296
Kawashima M, Noguchi T, Takase Y, Nakahara Y, Matsushima T (2010) Decrease in leptomeningeal ivy sign on fluid-attenuated inversion recovery images after cerebral revascularization in patients with Moyamoya disease. AJNR Am J Neuroradiol 31:1713–1718
Kawashima M, Noguchi T, Takase Y, Ootsuka T, Kido N, Matsushima T (2009) Unilateral hemispheric proliferation of ivy sign on fluid-attenuated inversion recovery images in moyamoya disease correlates highly with ipsilateral hemispheric decrease of cerebrovascular reserve. AJNR Am J Neuroradiol 30:1709–1716
Kuroda S, Hashimoto N, Yoshimoto T, Iwasaki Y (2007) Radiological findings, clinical course, and outcome in asymptomatic moyamoya disease: results of multicenter survey in Japan. Stroke 38:1430–1435
Kuroda S, Houkin K, Ishikawa T, Nakayama N, Iwasaki Y (2010) Novel bypass surgery for moyamoya disease using pericranial flap: its impacts on cerebral hemodynamics and long-term outcome. Neurosurgery 66:1093–1101, discussion 1101
Kuroda S, Shiga T, Houkin K, Ishikawa T, Katoh C, Tamaki N, Iwasaki Y (2006) Cerebral oxygen metabolism and neuronal integrity in patients with impaired vasoreactivity attributable to occlusive carotid artery disease. Stroke 37:393–398
Maeda M, Tsuchida C (1999) “Ivy sign” on fluid-attenuated inversion-recovery images in childhood moyamoya disease. AJNR Am J Neuroradiol 20:1836–1838
Mori N, Mugikura S, Higano S, Kaneta T, Fujimura M, Umetsu A, Murata T, Takahashi S (2009) The leptomeningeal “ivy sign” on fluid-attenuated inversion recovery MR imaging in Moyamoya disease: a sign of decreased cerebral vascular reserve? AJNR Am J Neuroradiol 30:930–935
Noguchi T, Kawashima M, Irie H, Ootsuka T, Nishihara M, Matsushima T, Kudo S (2011) Arterial spin-labeling MR imaging in moyamoya disease compared with SPECT imaging. Eur J Radiol 80:e557–e562
Ohta T, Tanaka H, Kuroiwa T (1995) Diffuse leptomeningeal enhancement, “ivy sign,” in magnetic resonance images of moyamoya disease in childhood: case report. Neurosurgery 37:1009–1012
Pandey P, Steinberg GK (2011) Neurosurgical advances in the treatment of moyamoya disease. Stroke 42:3304–3310
Powers WJ, Grubb RL Jr, Raichle ME (1984) Physiological responses to focal cerebral ischemia in humans. Ann Neurol 16:546–552
Sanossian N, Saver JL, Alger JR, Kim D, Duckwiler GR, Jahan R, Vinuela F, Ovbiagele B, Liebeskind DS (2009) Angiography reveals that fluid-attenuated inversion recovery vascular hyperintensities are due to slow flow, not thrombus. AJNR Am J Neuroradiol 30:564–568
Suzuki J, Takaku A (1969) Cerebrovascular “moyamoya” disease. Disease showing abnormal net-like vessels in base of brain. Arch Neurol 20:288–299
Yoon HK, Shin HJ, Chang YW (2002) “Ivy sign” in childhood moyamoya disease: depiction on FLAIR and contrast-enhanced T1-weighted MR images. Radiology 223:384–389
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Sandra V and Masaki I contributed equally to the present manuscript.
Rights and permissions
About this article
Cite this article
Vuignier, S., Ito, M., Kurisu, K. et al. Ivy sign, misery perfusion, and asymptomatic moyamoya disease: FLAIR imaging and 15O-gas positron emission tomography. Acta Neurochir 155, 2097–2104 (2013). https://doi.org/10.1007/s00701-013-1860-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-013-1860-4