Abstract
Background
Mild cerebrospinal fluid (CSF) hypovolemia is a well-known clinical entity, but critical CSF hypovolemia that can cause transtentorial herniation is an unusual and rare clinical entity that occurs after craniotomy. We investigated CSF hypovolemia after microsurgical aneurysmal clipping for subarachnoid hemorrhage (SAH).
Method
This study included 144 consecutive patients with SAH. Lumbar drainage (LD) was inserted after general anesthesia or postoperatively as a standard perioperative protocol. CSF hypovolemia diagnosis was based on three criteria.
Results
Eleven patients (7.6 %) were diagnosed with CSF hypovolemia according to diagnostic criteria in a postoperative range of 0–8 days. In all patients, signs or symptoms of CSF hypovolemia improved within 24 hours by clamping LD and using the Trendelenburg position.
Conclusions
As a cause of acute clinical deterioration after aneurysmal clipping, CSF hypovolemia is likely under-recognized, and may actually be misdiagnosed as vasospasm or brain swelling. We should always take the etiology of CSF hypovolemia into consideration, and especially pay attention in patients with pneumocephalus and subdural fluid collection alongside brain sag on computed tomography. These patients are at higher risk developing of pressure gradients between their cranial and spinal compartments, and therefore, brain sagging after LD, than after ventricular drainage. We should be vigilant to strictly manage LD so as not to produce high pressure gradients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cerebrospinal fluid (CSF) pressure is commonly maintained in the range of 70–150 mmH2O in healthy human adults. However, if the production of CSF decreases, absorption is promoted, or it leaks into epidural space, however, the pressure may decline. Mild CSF hypovolemia is a well-known clinical entity that can occur spontaneously or after lumbar puncture, head injury, cerebral or spinal transdural surgery. Postural headache is the main symptom and the outcome is typically benign. In contrast, critical CSF hypovolemia is a rare clinical entity that occurs after craniotomy because of CSF overdrainage, which is termed as “brain sag” or “sinking brain syndrome” [1, 5, 6].
Lumbar drainage (LD) is a simple, safe and effective procedure for improvement of acute hydrocephalus, relaxing brain swelling during surgery, or prevention of vasospasm after subarachnoid hemorrhage (SAH), and previous studies have reported its effectiveness [4]. However, the main objective during perioperative management may be whether CSF flows satisfactorily, and we may not be aware of CSF hypovolemia. In cases of mental state decline after aneurysmal clipping, vasospasm or brain swelling may actually be considered at first because CSF hypovolemia is not well-known as a complication after aneurysmal clipping. Transtentorial herniation is the most feared complication of LD, although it is rare.
Material and methods
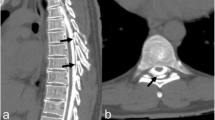
Between January 2007 and May 2011, 144 consecutive patients with SAH were included in this study, and were prospectively investigated as to whether they had complications of CSF hypovolemia after microsurgical aneurysmal clipping. LD was inserted after general anesthesia or postoperatively as a routine perioperative treatment protocol for improvement of acute hydrocephalus, relaxing brain swelling during surgery, or prevention of vasospasm in all patients. Lumbar catheter was placed at the L4-L5 level under sterile condition on the operation room or intensive care unit. Intraoperatively, CSF was drained intermittently, based on the surgeon’s discretion. Postoperatively, CSF was drained continuously with a target CSF drainage amount of 5 to 10 ml per hour within 14 days. CSF hypovolemia was diagnosed based on the following three criteria proposed by Komotar et al. [5, 6]. (1) Noncontrast axial computed tomography (CT) revealing effacement of the basal cisterns with an oblong brainstem (Fig. 1). (2) Signs or symptoms of transtentorial herniation (mental state decline or anisocoria). (3) Clinical improvement by clamping of the LD, additional drips, or using the Trendelenburg position.
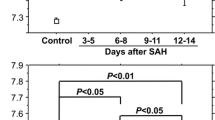
Axial noncontrast computed tomography (CT) at the level of midbrain. This demonstrates the oblong brainstem deformity and the effacement of the basal cisterns that are characteristics, which mean transtentorial herniation. Maximum anteroposterior distance (a) /maximum bipeduncular distance (B) is used to generate brainstem deformity. The sag ratio (a/b) during brain sag is significantly increased
Results
Eleven patients (7.6 %) were diagnosed with CSF hypovolemia according to diagnostic criteria mentioned above in the postoperative range of 0–8 days (Table 1). The serum sodium level of all patients was within normal limit. In all patients LD was inserted perioperatively. Nine patients of the 11 patients were female. The mean age of the patients was 67.5 (46–79) years old. Preoperative Hunt and Kosnik (H & K) grades of the patients were as follows: grade II/3 cases, grade III/4 cases, grade IV/3 cases, grade V/1 case. Fisher classifications on CT were as follows: group II/2 cases, group III/4 cases, group IV/5 cases. Locations of ruptured aneurysms were as follows: anterior communicating artery/4 cases, distal anterior cerebral artery/3 cases, middle cerebral artery/3 cases, and internal carotid artery/1 case. One case was diagnosed as progression of brain swelling because of early vasospasm, and external decompression was performed. However, anisocoria did not improve despite external decompression, and CSF hypovolemia was not turned out until that time (Fig. 2). In another case, papillary asymmetry was demonstrated in the middle of awaking from general anesthesia, and CSF hypovolemia was turned out because emergent CT revealed brain sag with sinking brain syndrome (Fig. 3). The cause of a fatal case was not CSF hypovolemia but pneumonia (case 4). In all patients, signs or symptoms of CSF hypovolemia improved within at least 24 hours by clamping LD and using the Trendelenburg position.
Case-1. a: Axial noncontrast computed tomography (CT) on admission. b: CT showing brain sag at postoperative day 1. c: CT after external decompression. The herniation signs and brain sag on CT were not improved despite external decompression. d: CT showing improving of brain sag (postoperative day 4)
Case-11 a-c: Axial noncontrast computed tomography (CT) on admission showing subarachnoid hemorrhage with sylvian hematoma in the left side. d-f: The papillary asymmetry was demonstrated during awaking from general anesthesia. Emergent CT showing brain sag with sinking brain syndrome immediately after aneurysmal clipping
Discussions
Intracranial hypotension that occurs spontaneously or after lumbar puncture, head injury, or operative procedures (craniotomy, spinal surgery, or shunt for hydrocephalus) is familiar as mild CSF hypovolemia, and the clinical outcome is typically benign. Mokri et al. reported that there is no linear correlation between CSF volume and pressure, and the common pathological physiological denominator in this syndrome is hypovolemia and not intracranial hypotension [8]. Postural headache is a typical symptom, and various symptoms such as vertigo/dizziness, nausea/vomiting, visual disturbance, and hearing disturbance were also seen in some cases. These symptoms are related to a downward traction on pain-sensitive intracranial and meningeal structures, distention of the chemotactic area, and direct pressure on the optic nerves and chiasm [5, 7]. In contrast, critical CSF hypovolemia that can cause transtentorial herniation is an unusual and rare clinical entity that occurs after craniotomy because of CSF overdrainage. Recently, Komotar et al. described critical CSF hypovolemia related to LD after microsurgical aneurismal clipping as “brain sag” [5, 6]. This clinical etiology is very important in postoperative management after microsurgical aneurismal clipping.
In microsurgical aneurysmal clipping, CSF diversion or dripping of osmotic diuretics for relaxing brain swelling is generally used. Generally, bloodstained CSF is aspirated and drained by ventricular drainage (VD) or LD during surgery. It is reported that early LD is effective for prevention of vasospasms [4]. In our institution, all SAH patients typically receive early LD to clear bloodstained CSF from the lumbar and basal cisterns. Although LD is a safe, simple and effective procedure, the main concern during perioperative management is whether CSF flows satisfactorily. In other words, surgeons may not be aware of the CSF hypovolemia itself.
As causes of acute clinical deterioration after aneurysmal clipping, vasospasm, brain swelling, seizure, or hyponatremia are more common postoperative complications. CSF hypovolemia is likely an under-recognized cause, and may actually be misdiagnosed as vasospasm or brain swelling [5]. If misdiagnosed, additional and invasive interventions that are not effective for CSF hypovolemia may be performed, and thus it is very important to consider CSF hypovolemia when forming a differential diagnosis. In this study, we were not aware of CSF hypovolemia, and the cause of acute clinical deterioration after craniotomy was sometimes considered to be brain swelling because of early vasospasm, in spite of brain sag revealed by CT (Fig. 2). Early awareness of CSF hypovolemia as causes of acute clinical deterioration after microsurgical aneurysmal clipping is very important, and we should take this etiology into consideration in cases revealing “brain sag” on CT [5, 6, 10].
CSF volume may decrease beyond our expectations as a result of suction and CSF diversion during surgery. Although CSF hypovolemia is an attractive concept to explain brain sag, additional parameters may influence CSF circulation, such as fluid viscosity, anatomy of the arachnoid cisterns and Pacchionian granulations, bridging veins, and elasticity of the meningeal membranes [2, 11]. These parameters vary between individuals. Additionally, clots from SAH may be considered as acquired factors. Because there are several brain compartments such as cisterns, communication between the compartments is essential to avoid formation of steep pressure gradients in CSF circulation, potentially staving off the threat of herniation. In SAH patients, barriers caused by clots may block CSF circulation into the lumbar cistern partially because they are usually located in the basal cisterns. Thus, a partial hydrocephalus may be present. CSF diversion via LD, when it exceeds the capacity of CSF communication over the clots, may, therefore, produce pressure gradients [10]. Komotar et al. reported that risk factors include the presence of global cerebral edema on admission CT and prolonged operating times [6]. In short, patients are at higher risk of developing pressure gradients between the cranial and spinal compartments, and therefore, brain sag after LD, than after VD [2]. We must be careful to manage LD so as not to produce high pressure gradients.
It is reported that brain sag is typically seen about 1–4 days after craniotomy [5, 6]. However, in our study, we also experienced brain sag postoperatively on days 6 and 8. Therefore, we need to attentive to recognize the etiology of brain sag as long as LD is inserted. Moreover, if CSF is drained excessively during surgery, brain sag can develop even immediately after surgery [9]. Indeed, we experienced such a case (case 11). However, it is difficult to accurately measure CSF volume during surgery.
Radiographic findings of intracranial hypotension have been generally documented on magnetic resonance imaging (MRI) rather than CT because it is difficult to capture characteristic alterations. MRI signs include narrowing of ventricles or sulci, subdural fluid collections and thickening and enhancement of the dura, swelling of the pituitary stalk, and engorgement of venous structures after contrast administration. Hadizadeh et al. reported that signal changes of the thalamus, basal ganglia, cerebellum, and brainstem can be a prognostic factor for CSF hypovolemia [3]. On the other hand, the finding of brain sag is a diagnostic rather than a prognostic factor. Nevertheless, the finding of brain sag is important because CT is a common modality after aneurysmal clipping. We should especially pay attention in cases with pneumocephalus (Fig. 4), and subdural fluid collection (Fig. 5) besides effacement of the basal cisterns with an oblong brainstem (Fig. 6) on CT [5]. Recently, Alaraj et al. reported characteristic angiographic features of brain sag, which include descent of the basilar tip with respect to the posterior clinoid process, kinking of the midbasilar artery, and kinking of the intracranial vertebral arteries [1].
Mild CSF hypovolemia usually resolves spontaneously, but may require the patient to lie flat for a time with or without performing an epidural blood patch. Because there are no effective treatment options for critical CSF hypovolemia and it may in fact worsen the condition if misdiagnosed, it is important to be aware of brain sag early to avoid acute postoperative clinical deterioration after microsurgical aneurysmal clipping. We can expect improvement of symptoms by clamping of the LD, additional drips, or using the Trendelenburg position [5, 6]. Staykov et al. reported that lumboventricular pressure measurement may be a useful tool to avoid developing pressure gradients between the cranial and spinal compartments [10]. Ventricular drainage may also be effective to invert the pressure gradient [2]. In patients with severe SAH, strict LD management is particularly needed because there is a higher risk of brain sag [6]. In practice, small fixed-volume intermittent CSF drainage may be safer than continuous LD, but evaluation of this requires further research.
Conclusions
When patients manifest mental state decline after microsurgical aneurysmal clipping, etiology of CSF hypovolemia should be considered if CT reveals brain sag. Although LD is a safe, simple, and effective procedure for perioperative managing of SAH, strict CSF management is needed in severe SAH because of the higher risk factor of brain sag. If the etiology is diagnosed as CSF hypovolemia, we can expect improvement of symptoms by clamping of LD, additional drips, or using the Trendelenburg position.
References
Alaraj A, Munson T, Herrera SR, Aletich V, Charbel FT, Amin-Hanjani S (2011) Angiographic features of "brain sag". J Neurosurg 115:586–591
Bloch J, Regli L (2003) Brain stem and cerebellar dysfunction after lumbar spinal fluid drainage: Case report. J Neurol Neurosurg Psychiatry 74:992–994
Hadizadeh DR, Kovacs A, Tschampa H, Kristof R, Schramm J, Urbach H (2010) Postsurgical intracranial hypotension: Diagnostic and prognostic imaging findings. AJNR Am J Neuroradiol 31:100–105
Klimo P Jr, Kestle JR, MacDonald JD, Schmidt RH (2004) Marked reduction of cerebral vasospasm with lumbar drainage of cerebrospinal fluid after subarachnoid hemorrhage. J Neurosurg 100:215–224
Komotar RJ, Mocco J, Ransom ER, Mack WJ, Zacharia BE, Wilson DA, Naidech AM, McKhann GM 2nd, Mayer SA, Fitzsimmons BF, Connolly ES Jr (2005) Herniation secondary to critical postcraniotomy cerebrospinal fluid hypovolemia. Neurosurgery 57:286–292
Komotar RJ, Ransom ER, Mocco J, Zacharia BE, McKhann GM 2nd, Mayer SA, Connolly ES Jr (2006) Critical postcraniotomy cerebrospinal fluid hypovolemia: Risk factors and outcome analysis. Neurosurgery 59:284–290
Lay CM (2002) Low cerebrospinal fluid pressure headache. Curr Treat Options Neurol 4:357–363
Mokri B (1999) Spontaneous cerebrospinal fluid leaks: From intracranial hypotension to cerebrospinal fluid hypovolemia-evolution of a concept. Mayo Clin Proc 74:1113–1123
Samadani U, Huang JH, Baranov D, Zager EL, Grady MS (2003) Intracranial hypotension after intraoperative lumbar cerebrospinal fluid drainage. Neurosurgery 52:148–151
Staykov D, Speck V, Volbers B, Wagner I, Saake M, Doerfler A, Schwab S, Bardutzky J (2011) Early recognition of lumbar overdrainage by lumboventricular pressure gradient. Neurosurgery 68:1187–1191
Ursino M, Lodi CA (1997) A simple mathematical model of the interaction between intracranial pressure and cerebral hemodynamics. J Appl Physiol 82:1256–1269
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kawahara, I., Tsutsumi, K., Matsunaga, Y. et al. Early awareness of cerebrospinal fluid hypovolemia after craniotomy for microsurgical aneurysmal clipping. Acta Neurochir 155, 1543–1548 (2013). https://doi.org/10.1007/s00701-013-1755-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-013-1755-4