Abstract
Background
We hypothesized that shunt dysfunction in the ventricular catheter and the shunt valve is caused by different cellular responses. We also hypothesized that the cellular responses depend on different pathophysiological mechanisms.
Methods
Removed shunt material was collected. Macroscopic tissue in the catheters was paraffin-embedded and HE-stained. Valves were incubated with trypsin-EDTA in order to detach macroscopically invisible biomaterial, which was then cytospinned and HE-stained. Associated aetiological and surgical data were collected by reviewing patient files, and ventricular catheter position was examined using preoperative radiology (CT scans).
Results
We examined eleven ventricular catheters and ten shunt valves. Catheters: 6/11 catheters contained intraluminal tissue consisting of vascularised glial tissue and inflammatory cells (macrophages/giant cells and a few eosinophils). Catheter adherence correlated with the presence of intraluminal tissue, and all tissue containing catheters had some degree of ventricle wall contact. All obstructed catheters contained intraluminal tissue, except one catheter that was dysfunctional because of lost ventricular contact. Valves: Regardless of intraoperative confirmation of valve obstruction, all ten valves contained an almost uniform cellular response of glial cells (most likely ependymal cells), macrophages/giant cells, and lymphomonocytic cells. Some degree of ventricle wall catheter contact was present in all examined valves with available radiology (9/10).
Conclusions
The same cellular responses (i.e., glial cells and inflammatory cells) cause both catheter obstruction and valve obstruction. We propose two synergistic pathophysiological mechanisms. (1) Ventricle wall/parenchymal contact by the catheter causes mechanical irritation of the parenchyma including ependymal exfoliation. (2) The shunt material provokes an inflammatory reaction, either nonspecific or specific. In combination, these mechanisms cause obstructive tissue ingrowth (glial and inflammatory) in the catheter and clogging of the valve by exfoliated glial cells and reactive inflammatory cells.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Extrathecal shunting of CSF remains very important in the hydrocephalus treatment regimen, even though recurring shunt dysfunction often complicates the treatment. The risk of shunt dysfunction is approximately 40 % after one year and upwards to 53 % after two years [3, 14]. The two major complications are shunt obstruction and shunt infection, accounting for 72 % (108/150) and 19 % (28/150), respectively, in a study series of shunt dysfunction [14]. In another study, the risk of mechanical (noninfected) shunt dysfunction having occurred after ten years was approximately 70 %, while the risk of shunt infection after ten years was approximately 9 %. Mechanical shunt dysfunction was caused by obstruction in 56.1 % of the cases, and proximal obstruction comprised more than half of these [33]. Pediatric patients younger than two years constitute a particular high risk group. In general, shunt revision within six months of last shunt surgery predicts a higher probability of shunt failure [30].
Given the high rate of complications, it is no surprise that several previous studies have investigated the causes of shunt obstruction with a variety of analysis methods, including: light microscopy, [1, 4, 18, 24, 25, 34, 39–41] scanning (SEM) [9–11, 20, 21, 24, 27, 35, 38] and transmission (TEM) [20, 38, 39] electron microscopy, and assays for protein and other deposits [9, 26, 27, 35, 42]. Because proximal obstruction is the most prevalent cause of mechanical shunt dysfunction, [5, 33] the majority of these studies have focused on ventricular catheter obstruction [1, 4, 9–11, 18, 21, 24–27, 34, 36, 38, 39]. Less often the distal (most often peritoneal) catheter has been included as object of interest [9, 11, 20, 21, 25, 26, 34, 42]. To our knowledge, only three previous studies have specifically investigated causes of valve obstruction [8, 35, 41]. Only one of these studies investigated the cellular response [41]. No previous publications deal with comparing the cellular response in ventricular catheters and shunt valves. The biological material previously described in shunts include: choroid plexus, ependymal cells, granulation tissue/connective tissue, neural tissue, glial tissue, macrophages, multinucleated giant cells, erythrocytes, thrombocytes, leukocytes, plasma cells, mast cells, proteinacious debris and mineral deposits [1, 4, 8–11, 18, 20, 21, 24–27, 34–36, 38–42].
We hypothesized that shunt dysfunction in the ventricular catheter and the shunt valve is caused by different cellular responses. We also hypothesized that the cellular responses depend on different pathophysiological mechanisms. In order to investigate this, we examined cytology and histology in removed shunt material and reviewed patient files, surgical descriptions and relevant radiology. To gain further knowledge of the cellular response in valve obstruction, we developed a novel method based on cytospinning for extracting and analysing shunt valve contents, while proven histological methods including paraffin-embedding and microtome sections were used to examine the material in ventricular catheters.
Methods and materials
During a period of one year from 2011 to 2012 material removed from shunts during shunt revisions was collected at the University Clinic of Neurosurgery at Copenhagen University Hospital, Rigshospitalet. The project was approved by The National Committee on Health Research Ethics (protocol no. H-2-2011-025), and informed (written and oral) consent was obtained from all the included patients.
The collected material consisted of ventricular catheters and/or shunt valves. External ventricular drainage systems and shunt material removed due to intracranial infection were not included. The shunt material was immediately fixed after removal in 4 % formaldehyde solution for later laboratory analysis. Ventricular catheters and shunt valves were analysed by two different methods at the Laboratory of Neuropathology at Copenhagen University Hospital, Rigshospitalet.
Ventricular catheters
The proximal part of the catheter, which contains the drainage holes, was thoroughly inspected for possible material clogging the holes, and the catheter was then split longitudinally in its entire length to reveal any macroscopic tissue hidden inside the lumen. If any tissue was found, this was embedded in paraffin for histological analysis. The material was finally hematoxylin and eosin (HE) stained.
Shunt valves
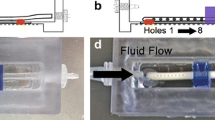
All removed shunt valves were examined, regardless of whether biomaterial was visible or not. In order to detach biomaterial for examination, the valves were filled with trypsin-EDTA solution (Sigma-Aldrich T3924) followed by five minutes of incubation time. The valves were then flushed with Dulbecco’s phosphate-buffered saline (Lonza DPBS) and the suspension was collected in a 2 mL Eppendorf tube. To ensure that only intraluminal biomaterial was collected during the flushing procedure, a surgical forceps was used to clamp the shunt valve where the 21G needle was introduced into the entrance hole of the valve. To concentrate the collected material, the contents were centrifuged with an Eppendorf MiniSpin Plus centrifuge at 3,500 RPM for five minutes. The volume of the supernatant was halved and the pellet was resuspended in the remaining fluid for cytospinning using a StatSpin Cytofuge 2 cytocentrifuge. Each examined shunt valve resulted in four microscopy slides. Two slides were HE stained for cellular morphology, and two slides were prepared for specific immunohistochemistry (IHC). Unfortunately, the cellular material did not prove to be robust enough for IHC even though cellular morphology was evident.
Slides with material from both catheters and valves were examined by light microscopy by the consultant neuropathologists (HB and HL).
In order to compare the laboratory analyses with clinical data, we thoroughly reviewed the patient files and surgical descriptions of our cases. This included aetiological (gender, age, hydrocephalus type, allergy, shunt type and implantation time) and surgical (type of dysfunction and catheter adherence) information. We defined six types of shunt dysfunction: catheter obstruction, valve obstruction, distal obstruction, disconnection, overdrainage and other. The category of “other” included cases of elective shunt removal.
Furthermore, the preoperative radiology (cerebral CT scans) of each case was reviewed to gain information about intraventricular catheter position and ventricular morphology. The type of catheter used has the drainage holes covering the distal 19 mm from the tip. We defined four possible degrees of ventricular position of the catheter tip (Table 1):
The position of the catheter tip in relation to the interventricular foramina was also noted: Anteriorly to the interventricular foramina, posteriorly to the interventricular foramina and inside the third ventricle. Furthermore, all radiology was systematically reviewed for presence and degree of slit ventricles.
For statistical description we used the Fisher’s exact test and the non-parametric Mann–Whitney U test.
Results
Table 2 summarizes the aetiological, surgical, radiological and neuropathological data. We collected 11 ventricular catheters and 10 shunt valves in total. Each separate ventricular catheter or shunt valve represents an individual patient case, except cases C10 and V10, which corresponds to the catheter and valve from the same patient, who had the shunt system removed in toto. Thus, we collected 21 samples from 20 patients.
The age range of the included cases was 24 to 65 years (median 53.0 years) for the examined catheters and 8 to 80 years (median 51.5 years) for the examined valves.
In general, there were no differences in patient age, gender, type of hydrocephalus, kind of shunt dysfunction, shunt type, implantation time and allergy when comparing cases with catheter obstruction and cases with valve obstruction, and also when comparing obstructed and non-obstructed cases internally.
The cases represent a variety of both acquired and congenital hydrocephalus with different causality (Table 2). The collected shunt types were: ventriculoperitoneal (VP) shunt (16/20), ventriculoatrial (VA) shunt (2/20), and Sinushunt (2/20).
Seventeen out of the 18 cases with available radiology had the ventricular catheter placed via a frontal burr hole, and the catheter tip was situated either anteriorly to the interventricular foramina (10/17) or inside the third ventricle (7/17). The only exception was case V3, which was placed via an occipital burr hole and had the catheter tip situated posteriorly to the interventricular foramina.
Manifest slit ventricles were present in cases V8 and C10/V10, while cases C2, C6, V1 and V2 were borderline cases (Fig. 1bdf). The remainder had normal or dilated ventricles.
Representative CT scans of our cases. For case details see Table 2. a C3: contact with wall of third ventricle. b C6: catheter tip buried in the parenchyma and a narrowed ventricular system c C7: loss of ventricular contact with catheter almost tangentially to the ventricle d V2: catheter contacting multiple ventricle walls in a narrowed ventricular system e V5: catheter touching septum pellucidum f V8: slit ventricles (bilateral ventricular catheters)
Case C10/V10 had ethylene oxide (EO) allergy, and case V1 was under suspicion for EO allergy. Case V8 was allergic to latex.
Ventricular catheters
An intraluminal tissue plug was found in six out of 11 removed ventricular catheters. In four of these cases containing a tissue plug, the cause of shunt dysfunction was intraoperatively confirmed as catheter obstruction. In the remaining two cases the tissue was discovered following elective removal of the shunt system. These two catheters were therefore not tested for mechanical obstruction, but it is most likely that the flow capacity of the catheters would have been compromised due to the present intraluminal tissue.
The neuropathological examination of the tissue plugs revealed that in all cases the plugs consisted of vascularised glial tissue, locally organized in circular patterns corresponding to an ingrowth through the catheter’s drainage holes (Fig. 2a-c). Furthermore, macrophages and a few multinucleated giant cells were observed, and in one tissue plug (C3) a cellular response of slight lymphocytosis and eosinophilia was seen (Fig. 2b), in addition to fragments of a normal looking choroid plexus.
Representative light microscopy of our cases. For case details see Table 2. a C1: intraluminal tissue, circle = circular tissue ingrowth b C3: intraluminal tissue, arrows = eosinophils c C4: intraluminal tissue d V1: cluster of glial cells e V2: cluster of glial cells f V2: blood vessel g V4: multinucleated giant cell h V6: cluster of glial cells i V8: macrophage
Only one of the examined catheters without intraluminal tissue (C7) was intraoperatively found to be obstructed. In this case, the cause was a loss of ventricular contact (Fig. 1c).
The implantation time of the ventricular catheters ranged from 0.4 to 5.1 years for catheters with intraluminal tissue and from 0.3 to “minimum” 4.0 years for catheters without intraluminal tissue. The “minimum” designation describes the longest confirmable implantation time found in the patient file for case C9. Assuming that the actual implantation time for case C9 does not differ markedly from the minimum implantation time, there is no significant difference between the two groups (p > 0.92). Thus, implantation time does not seem to be a determining factor for tissue invasion. A longer actual implantation time for C9 would only support this view, since no tissue was present in this catheter.
Intracerebral catheter adherence seemed to be related to the presence of intraluminal tissue. Four out of the six tissue containing catheters were adherent compared to none of the empty catheters, though this did not reach statistical significance (p > 0.06).
Furthermore, the presence or absence of ventricle wall contact by the catheter seemed to influence whether glial tissue had invaded the catheter or not. Ventricle wall contact was present in eight out of ten examined catheters (no radiology available for case C5). All examined tissue-containing catheters (5/8) and three of the five empty catheters (3/8) had contact with the ventricle wall. Thus, the presence of ventricle wall contact is associated with obstructive tissue ingrowth in almost two-thirds of the cases. A completely free catheter was only observed in two cases, and notably these catheters did not contain tissue.
Ventricle wall contact versus intraluminal tissue was however not statistical significant when plotted in a 2 × 2 contingency table (p > 0.44), (Table 3).
Shunt valves
In five (V1-V5) out of the ten valve cases, the cause of shunt dysfunction was intraoperatively found to be valve obstruction. The shunt valves were either OSVII valves (V2-V9) or Hakim valves (V1 and V10).
The neuropathological examination of the flushed-out trypsinated valve contents revealed no difference in cellular composition or quantifiable severity of valve clog-up between confirmed obstructed valves and valves removed on other indication, and neither did the valve type affect these observations. We were able to classify the majority of observed cells based on their morphology. In all cases, the general result was a sparse cellular content of either glial cells or macrophages/giant cells, or a combination of both, with a varying degree of lymphomonocytic cells (Fig. 2d-i). In the majority of cases the glial cells were most likely to be clusters of ependymal cells. In two cases (V2 and V10) a single thin-walled blood vessel was observed (Fig. 2f). The examined contents were often mixed with erythrocytes, but as the microscopy did not resemble old blood clot formation, the blood was assessed to have contaminated the valve at the time of removal.
Cellular autolysis, possibly caused by the cells being aggregated in the valve over time and intravalvular protection against the formaldehyde fixing, made a usable classification of the cells based on IHC staining impossible.
The implantation time of the shunt valve did not vary significantly (p > 0.14) between confirmed obstructed valves (range 1.7–11.3 years) and valves removed on other indication (range 0.2–7.0 years).
Preoperative radiology was available in nine out of ten valve cases. In all nine cases there was some degree of intraventricular wall contact by the catheter (Fig. 1d–f). Glial/ependyma-like cells were present in eight out of nine of these valves.
Discussion
Our findings of cellular contents in both ventricular catheters and shunt valves are consistent with previous descriptions, and in combination with our complementary aetiological, surgical and radiological data, a further insight in the pathophysiological mechanisms of shunt dysfunction is offered.
Ventricular catheters
The intraluminal tissue of the catheters consisted predominantly of vital, vascularised glial tissue. Since the histological architecture represented circular patterns, the tissue had most likely invaded the lumen through the catheter’s drainage holes in a reactive process against the foreign material. This supports the endoscopic observations of a previous study that described ependymal catheter ingrowth and neovascularization of the invading tissue [36]. Several animal studies have analyzed the cellular response to ventricular catheter implantation, and the described response is consistent with our findings [7, 13, 17]. The general experimental response consists of ependymal attenuation and denudation in vicinity of the catheter, combined with glial outgrowths corresponding to the location of the drainage holes. The mechanism of tissue ingrowth is proposed to be a combination of both mechanical factors, e.g. an intraluminal versus parenchymal pressure difference, and inflammatory factors mediated by the catheter material causing active cellular proliferation and migration.
In our observations, ventricle wall/parenchymal catheter contact seems to be more of a determining factor for catheter obstruction than implantation time. Physical contact was present in all cases of catheter obstruction, and importantly, cases with a completely free catheter did not contain any obstructive tissue. We therefore propose that physical contact between the ventricle wall/parenchyma and the catheter is the most important causal factor in regards to the pathophysiology of catheter obstruction. Possible reasons for the catheter to gain contact with the ventricle wall/parenchyma are: surgical misplacement of the catheter in the first place, a secondary collapse of the ventricle walls onto the catheter, or extracranial migration of the shunt. We therefore emphasize that the first line of prophylaxis against catheter obstruction should be correct intraventricular catheter placement, since it is the easiest and most obvious of the three to do something about. The criteria of success in regards to catheter placement should therefore not “just” be a functioning catheter, but a functioning catheter placed completely intraventricularly and free of the ventricle walls. This could be achieved with the aid of, e.g., stereotactic neuronavigation or intraoperative ultrasound. One study showed an accurate placement rate when using freehand technique of only 55 % versus 88 % and 89 % when using neuronavigation and ultrasound [44]. Further emphasizing the need for improved techniques for ventricular catheter placement, another study showed that almost 27 % of catheters placed with freehand technique were positioned suboptimally [43]. The ventricular size often decreases as a consequence of ventricular decompression by the shunting procedure. If ventricular reduction is marked, this results in contact between the catheter and the ventricle wall/parenchyma [10, 18]. In more pronounced cases of ventricle wall collapse, the catheter would simply become impacted, or as we observed in one case, lose contact to the ventricular system. Undiagnosed overdrainage could also eventually result in a narrowed ventricular system [6, 33]. These mechanisms are more difficult to control surgically. We therefore propose that ventricle wall/parenchymal contact, and following catheter obstruction, is an almost inevitable side effect of the intended therapeutic measure. The magnitude of ventricular size reduction primarily depends on the hydrodynamic characteristics of the valve, and in case of unintended ventricular narrowing only a correctly placed catheter can oppose the effects of the reduced ventricular size. The high prevalence of slit or borderline slit ventricles among all our cases emphasizes that decreased ventricular size is a complicating factor to be taken seriously. Since the reviewed radiology predominantly was performed on indication of shunt dysfunction, and the ventricles therefore might have become enlarged, shunt-induced narrowing of the ventricles might actually be more prevalent than we observed among our cases.
Shunt valves
All but one of the examined shunt valves contained glial cells that most likely were ependymal cells. All valves with available radiology drained from a ventricular catheter with ventricle wall/parenchymal contact. We therefore propose that valve obstruction, similarly to catheter obstruction, is an unavoidable side effect of ventricle wall/parenchymal contact by the catheter, causing the catheter tip to exfoliate ependymal and subependymal cells, which by means of cerebrospinal fluid (CSF) transportation eventually aggregates in the valve and cause obstruction. The shunt valve is the narrowest part of the shunt system and could therefore easily function as a filter for passing CSF. We propose that it is the exact same underlying mechanisms as mentioned in regards to catheter obstruction that cause physical contact between the catheter and the ventricle wall/parenchyma. In support of the proposed catheter-induced ependymal and subependymal irritation, ependymal hyperemia and growth of large new vessels in vicinity of the catheter tip have been endoscopically observed in respectively 37 % and 28 % of a study population [36]. This is also consistent with our observations of blood vessels in two examined shunts valves.
It is possible that valve obstruction can develop even without ventricle wall/parenchymal contact as a consequence of a general cell aggregation, but our results suggest that the process of accumulation is accelerated by physical contact between the catheter and the ventricle wall/parenchyma. This implies that even if a ventricular catheter is functioning at the time of valve revision, it should be considered whether the ventricular catheter should be replaced as well, since a ventricular catheter with ventricle wall/parenchymal contact could be a predisposing factor for repeated valve obstruction.
A previous study, investigating catheter obstruction, found that ependymal cells more often obstructed anteriorly placed catheters while choroid plexus obstructed those placed posteriorly [10]. The presence of ependymal cells in our study is consistent with the observed location of the catheter tip. The tip of every catheter, except one, was located either anteriorly to the interventricular foramina or inside the third ventricle.
Regardless of being obstructed or not, the examined shunt valves contained a uniform cellular composition. Our study did not offer the possibility of quantifying the actual amount of cells or cellular debris aggregated in the valve, but we hypothesize that the amount of biomaterial would be higher in the cases of confirmed valve obstruction. All obstructed valves had been implanted for a minimum duration of 1.7 years, thus it could be suggested that true valve obstruction takes a certain amount of time to aggregate.
Inflammatory response
In addition to the described glial response in both catheters and valves, we also observed inflammatory cells that to a lesser degree contributed to shunt obstruction. In general, an unspecific foreign body reaction, consisting of inflammatory cells, directed towards an implanted material is inevitable [16]. Even though the silicone material, that most shunt systems are made of, is generally considered to be biological inert, the adsorption of endogenic proteins to the surface elicits an unspecific inflammatory response of macrophages, giant cells and reactive tissue growth [12, 16, 22, 28, 45]. Our observations of macrophages and a few multinucleated giant cells, in both ventricular catheters and shunt valves, support previous studies suggesting a degree of inflammatory response being involved in the pathophysiological mechanism of shunt dysfunction [4, 20, 24, 25]. Furthermore, our results confirm that this also applies to valve obstruction [41].
In one catheter with intraluminal tissue, we observed a slight degree of localized eosinophilia, which points towards a more specific hypersensitivity reaction against the shunt material. Mainly two possible allergens have been proposed in relation to sterile shunt dysfunction: the silicone material alone or conjugated with adsorbed serum proteins, and the medical gas sterilant ethylene oxide (EO), which is used by several manufacturers to sterilize the shunt hardware [12, 15, 19, 20, 22, 25, 32, 37, 40, 42]. Hypersensitivity towards ethylene oxide has been reported in several spina bifida patients, and the frequency and duration of surgery-related allergen exposure is believed to be the major causing factor [2, 29, 31]. Both antibody-mediated type I hypersensitivity (allergy) and cell-mediated type IV hypersensitivity (delayed type hypersensitivity) have been proposed in relation to shunt dysfunction. Although manifest allergy did not correlate with the cellular response in our study, it is important to keep the possibility of a hypersensitivity reaction as underlying cause of recurrent shunt dysfunction in mind [15]. The presence of one confirmed EO allergic and another one suspected in our small study series demonstrates the relevance of this. Indeed, a study on CSF eosinophilia suggests that the presence of eosinophil cationic protein (ECP) released by activated eosinophils is associated with a higher risk of shunt dysfunction [23].
Conclusion
We have shown that it is the same cellular responses that are responsible for both catheter obstruction and valve obstruction: glial cells and inflammatory cells. We propose that it is also the same general pathophysiological mechanisms that are responsible for these cellular findings in shunt dysfunction. (1) Physical contact between catheter and ventricle wall/parenchyma causes mechanical irritation of the parenchyma including ependymal exfoliation, and occasionally the catheter simply becomes impacted or loses contact with the ventricle. (2) A chemically induced inflammatory reaction towards the shunt material (both catheter and valve material), or proteins adsorbed to the surface, causes an unspecific foreign body reaction or sometimes a specific hypersensitivity response.
Both pathophysiological mechanisms work together in synergy, eventually provoking obstructive tissue ingrowth (glial and inflammatory) in the ventricular catheter, and clogging of the shunt valve by exfoliated ependymal cells and reactive macrophages/giant cells.
Since our study stays at a descriptive level it does not give much clue to why some shunts remain functioning for years, even when the ventricles are very narrow. This is a difficult puzzle to solve, but should nevertheless be the focus of future research.
References
Aoki N, Sakai T (1990) Avulsion of choroid plexus during revision of ventricular shunting: Its high incidence and predictive value on computed tomography scan. Surg Neurol 33:256–260
Bache S, Petersen JT, Garvey LH (2011) Anaphylaxis to ethylene oxide—a rare and overlooked phenomenon? Acta Anaesthesiol Scand 55:1279–1282
Bierbrauer KS, Storrs BB, McLone DG, Tomita T, Dauser R (1990) A prospective, randomized study of shunt function and infections as a function of shunt placement. Pediatr Neurosurg 16:287–291
Bigner SH, Elmore PD, Dee AL, Johnston WW (1985) The cytopathology of reactions to ventricular shunts. Acta Cytol 29:391–396
Borgbjerg BM, Gjerris F, Albeck MJ, Hauerberg J, Borgesen SE (1995) Frequency and causes of shunt revisions in different cerebrospinal fluid shunt types. Acta Neurochir (Wien) 136:189–194
Browd SR, Gottfried ON, Ragel BT, Kestle JRW (2006) Failure of cerebrospinal fluid shunts. Part II: Overdrainage, loculation, and abdominal complications. Pediatr Neurol 34:171–176
Bruni JE, Del Bigio MR (1986) Reaction of periventricular tissue in the rat fourth ventricle to chronically placed shunt tubing implants. Neurosurgery 19:337–345
Brydon HL, Bayston R, Hayward R, Harkness W (1996) Removed shunt valves: Reasons for failure and implications for valve design. Br J Neurosurg 10:245–251
Brydon HL, Keir G, Thompson EJ, Bayston R, Hayward R, Harkness W (1998) Protein adsorption to hydrocephalus shunt catheters: CSF protein adsorption. J Neurol Neurosurg Psychiatry 64:643–647
Collins P, Hockley AD, Woollam DH (1978) Surface ultrastructure of tissues occluding ventricular catheters. J Neurosurg 48:609–613
Czernicki Z, Strzałkowski R, Walasek N, Gajkowska B (2010) What can be found inside shunt catheters. Acta Neurochir Suppl 106:81–85
Del Bigio MR (1998) Biological reactions to cerebrospinal fluid shunt devices: a review of the cellular pathology. Neurosurgery 42:319–325, discussion 325–316
Del Bigio MR, Bruni JE (1986) Reaction of rabbit lateral periventricular tissue to shunt tubing implants. J Neurosurg 64:932–940
Drake JM, Kestle JR, Milner R, Cinalli G, Boop F, Piatt J, Haines S, Schiff SJ, Cochrane DD, Steinbok P, MacNeil N (1998) Randomized trial of cerebrospinal fluid shunt valve design in pediatric hydrocephalus. Neurosurgery 43:294–303, discussion 303–295
Ellis MJ, Kazina CJ, Del Bigio MR, McDonald PJ (2008) Treatment of recurrent ventriculoperitoneal shunt failure associated with persistent cerebrospinal fluid eosinophilia and latex allergy by use of an “extracted” shunt. J Neurosurg Pediatr 1:237–239
Franz S, Rammelt S, Scharnweber D, Simon JC (2011) Immune responses to implants—a review of the implications for the design of immunomodulatory biomaterials. Biomaterials 32:6692–6709
Gedikoglu Y, Colak A, Benli K, Erbengi T (1993) Reaction of rabbit lateral periventricular tissue to non-infected and infected (Staphylococcus epidermidis) shunt tubing implants. A light and transmission electron microscope study. Acta Neurochir (Wien) 122:266–270
Go KG, Ebels EJ, van Woerden H (1981) Experiences with recurring ventricular catheter obstructions. Clin Neurol Neurosurg 83:47–56
Goldblum RM, Pelley RP, O’Donell AA, Pyron D, Heggers JP (1992) Antibodies to silicone elastomers and reactions to ventriculoperitoneal shunts. Lancet 340:510–513
Gower DJ, Lewis JC, Kelly DL Jr (1984) Sterile shunt malfunction. A scanning electron microscopic perspective. J Neurosurg 61:1079–1084
Guevara JA, La Torre J, Denoya C, Zúccaro G (1981) Microscopic studies in shunts for hydrocephalus. Childs Brain 8:284–293
Harris CA, McAllister JP 2nd (2012) What we should know about the cellular and tissue response causing catheter obstruction in the treatment of hydrocephalus. Neurosurgery 70:1589–1601, discussion 1601–1582
Heidemann SM, Fiore M, Sood S, Ham S (2010) Eosinophil activation in the cerebrospinal fluid of children with shunt obstruction. Pediatr Neurosurg 46:255–258
Koga H, Mukawa J, Nakata M, Sakuta O, Higa Y (1992) Analysis of retained ventricular shunt catheters. Neurol Med Chir (Tokyo) 32:824–828
Kossovsky N, Snow RB (1989) Clinical-pathological analysis of failed central nervous system fluid shunts. J Biomed Mater Res 23:73–86
Lundberg F, Li DQ, Falkenback D, Lea T, Siesjö P, Söderström S, Kudryk BJ, Tegenfeldt JO, Nomura S, Ljungh A (1999) Presence of vitronectin and activated complement factor C9 on ventriculoperitoneal shunts and temporary ventricular drainage catheters. J Neurosurg 90:101–108
Lundberg F, Tegenfeldt JO, Montelius L, Ransjö U, Appelgren P, Siesjö P, Ljungh A (1997) Protein depositions on one hydrocephalus shunt and on fifteen temporary ventricular catheters. Acta Neurochir (Wien) 139:734–742
Luttikhuizen DT, Harmsen MC, Van Luyn MJA (2006) Cellular and molecular dynamics in the foreign body reaction. Tissue Eng 12:1955–1970
Moneret-Vautrin DA, Laxenaire MC, Bavoux F (1990) Allergic shock to latex and ethylene oxide during surgery for spinal bifida. Anesthesiology 73:556–558
Piatt JH, Carlson CV (1993) A search for determinants of cerebrospinal fluid shunt survival: retrospective analysis of a 14-year institutional experience. Pediatr Neurosurg 19:233–241, discussion 242
Pittman T, Kiburz J, Steinhardt G, Krock J, Gabriel K (1995) Ethylene oxide allergy in children with spina bifida. J Allergy Clin Immunol 96:486–488
Pittman T, Williams D, Rathore M, Knutsen AP, Mueller KR (1994) The role of ethylene oxide allergy in sterile shunt malfunctions. Br J Neurosurg 8:41–45
Sainte-Rose C, Piatt JH, Renier D, Pierre-Kahn A, Hirsch JF, Hoffman HJ, Humphreys RP, Hendrick EB (1991) Mechanical complications in shunts. Pediatr Neurosurg 17:2–9
Sekhar LN, Moossy J, Guthkelch AN (1982) Malfunctioning ventriculoperitoneal shunts. Clinical and pathological features. J Neurosurg 56:411–416
Sgouros S, Dipple SJ (2004) An investigation of structural degradation of cerebrospinal fluid shunt valves performed using scanning electron microscopy and energy-dispersive x-ray microanalysis. J Neurosurg 100:534–540
Singh D, Saxena A, Jagetia A, Singh H, Tandon MS, Ganjoo P (2012) Endoscopic observations of blocked ventriculoperitoneal (VP) shunt: a step toward better understanding of shunt obstruction and its removal. Br J Neurosurg
Snow RB, Kossovsky N (1989) Hypersensitivity reaction associated with sterile ventriculoperitoneal shunt malfunction. Surg Neurol 31:209–214
Takahashi Y, Ohkura A, Hirohata M, Tokutomi T, Shigemori M (1998) Ultrastructure of obstructive tissue in malfunctioning ventricular catheters without infection. Neurol Med Chir (Tokyo) 38:399–404, discussion 403–394
Thomale UW, Hosch H, Koch A, Schulz M, Stoltenburg G, Haberl E-J, Sprung C (2010) Perforation holes in ventricular catheters—is less more? Childs Nerv Syst 26:781–789
Traynelis VC, Powell RG, Koss W, Schochet SS, Kaufman HH (1988) Cerebrospinal fluid eosinophilia and sterile shunt malfunction. Neurosurgery 23:645–649
Traynelis VC, Willison CD, Follett KA, Chambers J, Schochet SS Jr, Kaufman HH (1991) Millipore analysis of valvular fluid in sterile valve malfunctions. Neurosurgery 28:848–852
VandeVord PJ, Gupta N, Wilson RB, Vinuya RZ, Schaefer CJ, Canady AI, Wooley PH (2004) Immune reactions associated with silicone-based ventriculo-peritoneal shunt malfunctions in children. Biomaterials 25:3853–3860
Wan KR, Toy JA, Wolfe R, Danks A (2011) Factors affecting the accuracy of ventricular catheter placement. J Clin Neurosci 18:485–488
Wilson TJ, Stetler WR Jr, Al-Holou WN, Sullivan SE (2013) Comparison of the accuracy of ventricular catheter placement using freehand placement, ultrasonic guidance, and stereotactic neuronavigation. J Neurosurg. doi:10.3171/2012.11.JNS111384
Zhong Y, Bellamkonda RV (2008) Biomaterials for the central nervous system. J R Soc Interface 5:957–975
Acknowledgements
Lundbeckfonden; Aase og Ejnar Danielsens Fond; the staff at Laboratory of Neuropathology, Rigshospitalet (Ann Meisler, Jan Lauritzen & Diem Pham).
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Presentation at a conference
Oral presentations at:
International Society for Pediatric Neurosurgery (ISPN) 2012 in Sydney
International Society for Hydrocephalus and Cerebrospinal Fluid Disorders (ISHCSF) 2012 in Kyoto
Clinical Trial Registration number if required
The project was approved by The National Committee on Health Research Ethics (protocol no. H-2-2011-025).
Rights and permissions
About this article
Cite this article
Blegvad, C., Skjolding, A.D., Broholm, H. et al. Pathophysiology of shunt dysfunction in shunt treated hydrocephalus. Acta Neurochir 155, 1763–1772 (2013). https://doi.org/10.1007/s00701-013-1729-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-013-1729-6