Abstract
Background
The activation of matrix metalloproteinases (MMPs) is a critical event for disruption of the blood–brain barrier (BBB) during cerebral ischemia. Among the MMPs, MMP-2, and MMP-9 expression were reported to be significantly elevated after the onset of ischemia. The aim of this study was to investigate which one is more significant for BBB disruption in the photothrombotic cerebral ischemia.
Materials and methods
Male Sprague–Dawley rats weighing 250–300 g received focal cerebral ischemia by photothrombosis. MMP-2 and MMP-9 activities were assessed by gelatin zymography at various times from 2 h to 7 days. The BBB integrity was assessed using Evans blue dye with a spectrophotometric assay.
Findings
The Evans blue extravasation was increased within 2 h after cerebral ischemia, and was maximal at 12 and 24 h after the injury, and then gradually decreased. MMP-9 protein activity was detected as early as 2 h after the focal ischemic event; it rapidly increased at 6 h after ischemia, and reached a maximum level 48 h after the ischemic event. Thereafter, the MMP-9 level abruptly decreased and returned to the baseline at 72 h after the insult. By contrast, the MMP-2 protein activity was up-regulated at 6 h after the focal ischemic insult, and reached a maximum level at 72 h after the event. The elevated MMP-2 levels persisted for 7 days after the injury.
Conclusions
The early activation of MMP-9 was correlated with the increase in the permeability of the BBB. Our findings suggest that MMP-9 is the key factor involved in BBB disruption and subsequent brain injury after photothrombotic cerebral ischemia in rats.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The blood–brain barrier (BBB) is essential for maintenance of the homeostasis and normal functioning of the brain. The BBB consists of endothelial cell tight junctions, basal lamina, and integrin-mediated interactions of glial cells with the extracellular matrix (ECM) [8]. The cerebral microvessel integrity requires maintenance of the endothelial permeability barrier and the ECM-containing basal lamina [5, 8]. The cerebral microvessel ECM consists of type IV collagen, laminins, fibronectin, heparan sulfates, and other glycoproteins [9]. During cerebral ischemic events, endothelial basal lamina degradation begins as soon as 2 h after the onset of ischemia; this is rapidly followed by an increase in BBB permeability in mice [10]. The dysfunction of the BBB after ischemic events has been attributed to the activation of matrix metalloproteinases (MMPs) [10, 19].
MMPs are a family of zinc-binding proteolytic enzymes that degrade the ECM components of the basement membrane [13, 19]. MMPs have been implicated in numerous pathological conditions including atherosclerosis, inflammation, tumor growth, metastasis, and cerebral ischemia [19]. The activation of MMPs has been reported to be essential in ischemia-induced degradation of the ECM, BBB disruption, facilitation of leukocyte infiltration, and the inflammatory response [8, 12, 25]. Among the members of the MMP family, MMP-2 (72-kD gelatinase A) and MMP-9 (92-kD gelatinase B) have been shown to be significantly increased during a stroke in humans and in rat models of focal ischemia [1, 19, 21]. MMP-2 injections directly into the rat brain have been shown to disrupt the BBB and are associated with the increased expression of MMP-9 [20]. These findings imply that MMP-2 and MMP-9 play a critical role in brain injury after stroke. In the current study, we sought to clarify whether MMP-9 is a major participant in the pathophysiologic cascade of neuronal tissue damage after focal cerebral ischemia. For this purpose, focal cortical ischemia was induced by photothrombosis, and the activities of MMP-2 and MMP-9 and the BBB disruption were investigated.
Materials and methods
Animal model of focal cerebral ischemia
All surgical procedures and postoperative care were performed in accordance with the guidelines of the Chonnam National University Animal Care and Use Committee. A total of 46 male Sprague–Dawley rats weighing 250–300 g were used in the present study; two rats died after surgery. Focal cortical ischemia was induced by photothrombosis of the cortical microvessels according to a modified method described by Watson et al. [27]. Each rat was anesthetized with 5% isoflurane and maintained with 2% isoflurane in an oxygen/air mixture using a gas anesthesia mask in a stereotactic frame (Stoelting, Wood Dale, IL, USA). The rectal temperature was controlled at 37 ± 0.5°C with a homeothermic blanket (Harvard apparatus) during surgery. The skull was exposed via a midline incision of the skin. The periosteum over the skull was removed completely and a cold light source was placed as close as possible to the skull. For illumination, a fiber-optic bundle of the cold light source (Zeiss FL1500 LCD, Germany) with a 4.5-mm aperture was positioned onto the skull, 0.5 mm anterior to bregma and 3.7 mm lateral to the midline over the left sensorimotor cortex, as described in detail elsewhere [28, 29]. The photochemical dye, Rose Bengal (50 mg/kg, Sigma Chemical Co., St. Louis, MO, USA) in normal saline, was infused into the femoral vein via a microinjection pump within 1 min. Immediately afterwards, the brain was illuminated for 10 min through the exposed intact skull. The scalp was sutured and the rats were allowed to waken before being returned to their home cages. In the sham surgery, two animals received illumination after normal saline was applied instead of Rose Bengal.
Determination of BBB disruption
Vascular permeability was quantitatively evaluated by fluorescent detection of extravasated Evans blue dye. Disruption of the BBB was assessed 2, 6, 12, 24, and 72 h after ischemia using Evans blue dye as reported previously (n = 4 per time point) [17]. Evan’s blue dye (2%, 4 mL/kg) was injected over 2 min into the left femoral vein; it was allowed to circulate for 60 min. The rats were deeply anesthetized and transcardially perfused with phosphate-buffered saline (PBS) until colorless perfusion fluid was obtained from the right atrium. After decapitation, the brain was removed and coronal sections were divided into the right and left hemispheres. Brains were weighted and homogenized in ten-fold volume of 50% trichloroacetic acid solution. The supernatant was obtained by centrifugation and diluted fourfold with ethanol. The fluorescence intensity was determined by a microplate fluorescent reader. Evans blue extravasation was quantified in the supernatants by spectrophotometry. The amount of extravasated Evans blue dye was quantified as microgram per gram of brain tissue.
Preparation of tissue extracts
The experimental animals were deeply anesthetized and transcardially perfused with ice-cold PBS (pH 7.4) at 2, 6, and 24 h and 2, 3, 7 days after the ischemic insult (n = 4 per time point). The brains were rapidly removed, and ischemic brain tissue was homogenized in lysis buffer including protease inhibitors. After centrifugation, the supernatant was collected. Total protein concentrations were determined using the Bradford assay (Bio-Rad Laboratories, Hercules, CA, USA). Ipsilateral cortical samples, from sham-operated animals, and the contralateral cortex, of all operated focal ischemic rats, were compared.
Gelatin zymography
Gelatin zymography was performed as described previously [11]. Briefly, equal amounts of protein samples (60 μg) were prepared. After mixing with equal volumes of sample buffer, each sample was separated by Tris–glycine SDS-PAGE with 0.1% gelatin at 4°C. After electrophoresis was completed, the gel was then incubated with developing buffer overnight at 37°C. After development, the gel was stained with 0.5% Coomassie Brilliant Blue R-250 for 30 min and then destained appropriately. Clear bands on the blue background indicated zones of digestion corresponding to the presence of activated MMPs on the basis of their molecular weights.
Statistical analysis
Statistical analysis was performed using the SPSS software program (version 14.0 for Windows; SPSS INC., Chicago, IL). Quantitative data are expressed as the mean ± SEM. Statistical analysis was performed using the Student’s t test and Pearson’s correlation coefficient. P values of less than 0.05 were considered significant.
Results
BBB permeability
We determined the sequential changes in BBB disruption of the injured cortex after a focal ischemic insult. No Evans blue was detected in the non-ischemic brain. Evans Blue extravasation was increased within 2 h after the ischemic event, reaching maximal levels at 12 and 24 h after the insult in the ischemic hemisphere, and then gradually decreased (Fig. 1).
MMP-2 and MMP-9 expression in the ischemic brain
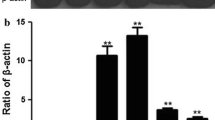
MMP-2 and MMP-9 activities were analyzed by gelatin zymography. The baseline levels of MMP-2 and MMP-9 were very low in the sham-operated brains. MMP-9 activity was detected as early as 2 h after the focal ischemic event and increased over time after ischemia was induced. It was rapidly increased at 6 h after the ischemic insult, and reached a maximum level 48 h after the ischemic insult. Thereafter, the MMP-9 activity abruptly decreased and returned to the baseline levels at 72 h after the ischemic insult (Fig. 2). By contrast, the MMP-2 activity was detected at 6 h after the ischemic insult, and reached a maximum level at 72 h after the insult. The elevated MMP-2 levels persisted for up to 7 days after the injury. Significant positive correlation was observed between BBB disruption and MMP-9 activities (correlation coefficient = 0.507, p value = 0.023). However, no significant correlation was observed between BBB disruption and MMP-2 activities.
Representative gelatin zymogram showing elevation of MMP activities in ischemic tissue extracts from rat brain. a Tissue extracts were analyzed for MMP activities over a time course of 6 h to 7 days. b, c Bar graph of measurement of optical densities for MMP-9 and MMP-2 in ischemic cortex tissue extracts as detected by zymography. A significant increase in the protein expression of MMP-9 is evident at 6 h after the insult, and reached its maximum level 48 h after the ischemic insult. A significant increase of the protein expression of MMP-2 is evident at 48 h after the insult. Measurements for all animals studied were made, including all sham samples and every time point indicated. Columns represent mean ± SEM (n = 4 per time point; *p < 0.05; **p < 0.01 compared with control; Student’s unpaired t test)
Discussion
Cerebral ischemia produces disruption of the BBB, followed by edema of the brain and secondary brain damage. The postischemic edema reaches a maximum at about 2 days after the ischemic insult [7, 18]. The dysfunction of the BBB after an ischemic stroke has been attributed to the activation of MMPs. The up-regulation of MMP-2 and MMP-9 after the onset of cerebral ischemia have been documented [2, 10, 11, 16, 19, 21, 22]. In rodent models of cerebral ischemia, MMP-2 is constitutively expressed in the brain and may play a role in ischemia [10]. However, MMP-9 is not normally expressed, but is induced after an ischemic insult and appears to potentiate the injury [2]. Several reports have suggested that MMP-9 may play a key role in the pathophysiology of ischemia [15, 21, 22]. The protein and mRNA levels of MMP-9 have been reported to be up-regulated in the mouse brain after focal cerebral ischemia. In MMP-9 knockout mice, BBB disruption and the volume of the ischemic lesions were significantly reduced compared with the wild-type mice [2, 26], whereas MMP-2 gene knockout mice were not protected against ischemia [3]. Nonetheless, MMP-2 was found during the later reparative phases when the blood vessels began to regrow [1, 7]. Clark et al. [7] reported that human brain tissue, after a stroke, demonstrates MMP-2 after several months, whereas MMP-9 is elevated within days after the infarct. Therefore, the later increase of MMP-2 activity would correlate better with the poststroke time course of capillary remodeling than with that of cerebral edema. The result of the present study demonstrated that increased MMP-9 and MMP-2 activities were increased by brain ischemia. However, MMP-9 up-regulation was detected much earlier after the ischemic insult than was MMP-2. MMP-9 protein activity was detected as early as 2 h after the ischemic insult, when the alteration of the BBB permeability was detected in the ischemic brain. By contrast, a significant elevation of MMP-2 expression was not significantly increased until 48 h after the ischemic insult. These findings suggest that MMP-9 plays a significant role in the disruption of the BBB and the development of brain injury caused by the photothrombotic insult, in the rat model. In particular, the expression of MMP-9 within the first 24 h after the ischemic event indicates that MMP-9 might be involved in the initial tissue destruction and contributes to the rapid development of brain injury after an ischemic insult. Therefore, MMP-9 inhibition could reduce the alteration and destruction of the BBB and brain injury after an ischemic insult.
Although the intraluminal suture model for the middle cerebral artery occlusion (MCAO) has been widely used, the procedure requires sophisticated microsurgical skills, and the lesions obtained by the MCAO tend to be variable in size [4, 24]. Furthermore, the mortality may be high because of the large size of the infarction and the severe neurologic deficit [14]. In this study, focal ischemia was induced noninvasively by photothrombotic occlusion of the cerebral microvessels [23, 27]. The photosensitive dye, Rose Bengal, was absorbed into the blood flow and focal illumination of the skull activated the local dye. The formation of free radicals leads to peroxidative damage of the endothelial membrane. Consequently, disturbance of the endothelium activates platelet aggregation and the coagulation cascade leading to thrombotic occlusion of small vessels [6, 24]. The features associated with the photothrombotic stroke model include acute severe endothelial cell damage, BBB damage and edema formation [29]. There has been no prior report of MMP-2 and MMP-9 activity with the photothrombotic stroke model. In the present study, we investigated the activities of MMP-2 and MMP-9 and the BBB disruption in the photothrombosis-induced brain injury. Collectively, the results demonstrated the up-regulation of MMP-2 and MMP-9 activities after an ischemic insult, which are consistent with a previous report. Therefore, the photothrombotic stroke model could be a suitable model for study of MMPs in association with a breakdown of the BBB.
References
Anthony DC, Ferguson B, Matyzak MK, Miller KM, Esiri MM, Perry VH (1997) Differential matrix metalloproteinase expression in cases of multiple sclerosis and stroke. Neuropathol Appl Neurobiol 23:406–415. doi:10.1111/j.1365-2990.1997.tb01315.x
Asahi M, Asahi K, Jung JC, del Zoppo GJ, Fini ME, Lo EH (2000) Role for matrix metalloproteinase 9 after focal cerebral ischemia: effects of gene knockout and enzyme inhibition with BB-94. J Cereb Blood Flow Metab 20:1681–1689. doi:10.1097/00004647-200012000-00007
Asahi M, Sumii T, Fini ME, Itohara S, Lo EH (2001) Matrix metalloproteinase 2 gene knockout has no effect on acute brain injury after focal ischemia. Neuroreport 12:3003–3007. doi:10.1097/00001756-200109170-00050
Aspey BS, Taylor FL, Terruli M, Harrison MJ (2000) Temporary middle cerebral artery occlusion in the rat: consistent protocol for a model of stroke and reperfusion. Neuropathol Appl Neurobiol 26:232–242. doi:10.1046/j.1365-2990.2000.00221.x
Aumailley M (1995) Structure and supramolecular organization of basement membranes. Kidney Int Suppl 49:S4–S7
Boquillon M, Boquillon JP, Bralet J (1992) Photochemically induced, graded cerebral infarction in the mouse by laser irradiation evolution of brain edema. J Pharmacol Toxicol Methods 27:1–6. doi:10.1016/1056-8719(92)90013-Q
Clark AW, Krekoski CA, Bou SS, Chapman KR, Edwards DR (1997) Increased gelatinase A (MMP-2) and gelatinase B (MMP-9) activities in human brain after focal ischemia. Neurosci Lett 238:53–56. doi:10.1016/S0304-3940(97)00859-8
del Zoppo GJ, Mabuchi T (2003) Cerebral microvessel responses to focal ischemia. J Cereb Blood Flow Metab 23:879–894. doi:10.1097/01.WCB.0000078322.96027.78
Fukuda S, Fini CA, Mabuchi T, Koziol JA, Eggleston LL Jr, del Zoppo GJ (2004) Focal cerebral ischemia induces active proteases that degrade microvascular matrix. Stroke 35:998–1004. doi:10.1161/01.STR.0000119383.76447.05
Gasche Y, Fujimura M, Morita-Fujimura Y, Copin JC, Kawase M, Massengale J, Chan PH (1999) Early appearance of activated matrix metalloproteinase-9 after focal cerebral ischemia in mice: a possible role in blood-brain barrier dysfunction. J Cereb Blood Flow Metab 19:1020–1028. doi:10.1097/00004647-199909000-00010
Heo JH, Lucero J, Abumiya T, Koziol JA, Copeland BR, del Zoppo GJ (1999) Matrix metalloproteinases increase very early during experimental focal cerebral ischemia. J Cereb Blood Flow Metab 19:624–633. doi:10.1097/00004647-199906000-00005
Jian Liu K, Rosenberg GA (2005) Matrix metalloproteinases and free radicals in cerebral ischemia. Free Radic Biol Med 39:71–80. doi:10.1016/j.freeradbiomed.2005.03.033
Lee JE, Yoon YJ, Moseley ME, Yenari MA (2005) Reduction in levels of matrix metalloproteinases and increased expression of tissue inhibitor of metalloproteinase-2 in response to mild hypothermia therapy in experimental stroke. J Neurosurg 103:289–297
Lee JK, Park MS, Kim YS, Moon KS, Joo SP, Kim TS, Kim JH, Kim SH (2007) Photochemically induced cerebral ischemia in a mouse model. Surg Neurol 67:620–625. doi:10.1016/j.surneu.2006.08.077 discussion 625
Lee SR, Tsuji K, Lee SR, Lo EH (2004) Role of matrix metalloproteinases in delayed neuronal damage after transient global cerebral ischemia. J Neurosci 24:671–678. doi:10.1523/JNEUROSCI.4243-03.2004
Mun-Bryce S, Rosenberg GA (1998) Matrix metalloproteinases in cerebrovascular disease. J Cereb Blood Flow Metab 18:1163–1172. doi:10.1097/00004647-199811000-00001
Park S, Yamaguchi M, Zhou C, Calvert JW, Tang J, Zhang JH (2004) Neurovascular protection reduces early brain injury after subarachnoid hemorrhage. Stroke 35:2412–2417. doi:10.1161/01.STR.0000141162.29864.e9
Romanic AM, Madri JA (1994) Extracellular matrix-degrading proteinases in the nervous system. Brain Pathol 4:145–156. doi:10.1111/j.1750-3639.1994.tb00825.x
Romanic AM, White RF, Arleth AJ, Ohlstein EH, Barone FC (1998) Matrix metalloproteinase expression increases after cerebral focal ischemia in rats: inhibition of matrix metalloproteinase-9 reduces infarct size. Stroke 29:1020–1030
Rosenberg GA, Dencoff JE, McGuire PG, Liotta LA, Stetler-Stevenson WG (1994) Injury-induced 92-kilodalton gelatinase and urokinase expression in rat brain. Lab Invest 71:417–422
Rosenberg GA, Estrada EY, Dencoff JE (1998) Matrix metalloproteinases and TIMPs are associated with blood-brain barrier opening after reperfusion in rat brain. Stroke 29:2189–2195
Rosenberg GA, Navratil M, Barone F, Feuerstein G (1996) Proteolytic cascade enzymes increase in focal cerebral ischemia in rat. J Cereb Blood Flow Metab 16:360–366. doi:10.1097/00004647-199605000-00002
Schroeter M, Jander S, Huitinga I, Stoll G (2001) CD8+ phagocytes in focal ischemia of the rat brain: predominant origin from hematogenous macrophages and targeting to areas of pannecrosis. Acta Neuropathol 101:440–448
Schroeter M, Jander S, Stoll G (2002) Non-invasive induction of focal cerebral ischemia in mice by photothrombosis of cortical microvessels: characterization of inflammatory responses. J Neurosci Methods 117:43–49. doi:10.1016/S0165-0270(02)00072-9
Shigemori Y, Katayama Y, Mori T, Maeda T, Kawamata T (2006) Matrix metalloproteinase-9 is associated with blood-brain barrier opening and brain edema formation after cortical contusion in rats. Acta Neurochir Suppl (Wien) 96:130–133. doi:10.1007/3-211-30714-1_29
Wang X, Jung J, Asahi M, Chwang W, Russo L, Moskowitz MA, Dixon CE, Fini ME, Lo EH (2000) Effects of matrix metalloproteinase-9 gene knock-out on morphological and motor outcomes after traumatic brain injury. J Neurosci 20:7037–7042
Watson BD, Dietrich WD, Busto R, Wachtel MS, Ginsberg MD (1985) Induction of reproducible brain infarction by photochemically initiated thrombosis. Ann Neurol 17:497–504. doi:10.1002/ana.410170513
Wiessner C, Bareyre FM, Allegrini PR, Mir AK, Frentzel S, Zurini M, Schnell L, Oertle T, Schwab ME (2003) Anti-Nogo-A antibody infusion 24 hours after experimental stroke improved behavioral outcome and corticospinal plasticity in normotensive and spontaneously hypertensive rats. J Cereb Blood Flow Metab 23:154–165. doi:10.1097/00004647-200302000-00003
Zhao CS, Puurunen K, Schallert T, Sivenius J, Jolkkonen J (2005) Behavioral and histological effects of chronic antipsychotic and antidepressant drug treatment in aged rats with focal ischemic brain injury. Behav Brain Res 158:211–220. doi:10.1016/j.bbr.2004.09.001
Acknowledgment
This study was supported by a grant of the Korea Health 21 R&D Project, Ministry of Health & Welfare, Republic of Korea (CNUH RICM-U-2006-031).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Piao, MS., Lee, JK., Park, CS. et al. Early activation of matrix metalloproteinase-9 is associated with blood–brain barrier disruption after photothrombotic cerebral ischemia in rats. Acta Neurochir 151, 1649–1653 (2009). https://doi.org/10.1007/s00701-009-0431-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-009-0431-1