Abstract
Purpose
As a safe and reliable alternative to central venous catheters (CVCs), peripherally inserted central catheters (PICCs) are commonly used in clinical practice. However, the insertion of PICCs by nurse practitioners (NPs), especially in Japan, has not been reported extensively. Thus, we investigated the safety and efficiency of PICC insertions by NPs.
Methods
The participants were 1322 patients who underwent PICC insertion by NPs at Fujita Health University Hospital (FNPs). The basilic vein in the brachium was the preferred vein for insertion; the brachial vein was the alternative. Patients were monitored from the time of PICC insertion until its removal. Ultrasonography-guided puncture was used for all catheter insertions, and the catheter tip was replaced into the superior vena cava under fluoroscopic imaging with maximal sterile barrier precautions. The outcomes of the PICC insertions by the FNPs were evaluated retrospectively.
Results
Overall, 23 FNPs inserted a collective total of 1322 PICCs, which remained in place for a collective total of 23,619 catheter days. The rate of successful PICC insertion was 99% (1310 patients). The median time taken for PICC insertion was 12 min (interquartile range, 10–15 min). Intraoperative complications occurred in two patients (0.2%). The confirmed incidence of central line–associated bloodstream infection was 3.4% (45 patients), and these infections occurred on 1.9 per 1000 catheter days. The median duration of PICC placement was 15 days (range, 10–23 days).
Conclusion
PICC insertion by NPs is safe and a potential alternative to CVC insertion by surgeons.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastroenterological surgeons in Japan tend to work excessively and their risk of burnout is high. In April 2019, the “Act on the Arrangement of Related Acts to Promote Work Style Reform” was implemented to reduce long working hours for all workers, including medical professionals [1]. To promote work-style reform and to reduce the burden on surgeons, task shifting is necessary. Nurse practitioners (NPs) play an essential role in resolving this issue; however, the implementation of NPs has been limited in Japan, compared with other countries. Oita University of Nursing and Health Sciences founded the master class of NPs in 2008, with the first NPs graduating in 2010 [2]. Fujita Health University initiated a clinical master’s degree course for NP development in its graduate school in 2012 [3]. The Act on Public Health Nurses, Midwives, and Nurses was amended in 2015 to include the requirement for nurses performing specified medical interventions in accordance with procedure manuals (a type of instruction rendered by physicians) to receive training in specific interventions [4]. The establishment of this new system enabled trained nurses to perform specific medical interventions without always having to wait for a physician’s decision. Since then, both the demand for and the number of NPs have been increasing in Japan.
Central venous catheters (CVCs) are essential for parental nutrition, chemotherapy, perioperative management, and other procedures in patients with gastroenterological diseases. As a safe and reliable alternative to CVCs, peripherally inserted central catheters (PICCs) are used commonly by clinicians in daily practice [5,6,7,8]. PICCs are associated with fewer serious insertion-related complications, such as inadvertent arterial puncture and pneumothorax, and can be inserted faster and are more cost effective than CVCs [7,8,9,10]. Furthermore, with special training, nurses can insert PICCs safely. In fact, PICC insertion by nurses is common worldwide [8, 8,11,12,13,14]; yet, there are few reports of PICC insertion by NPs, especially in the field of gastroenterological surgery in Japan. We conducted this study to investigate the safety of PICC insertion by NPs.
Methods
Patients
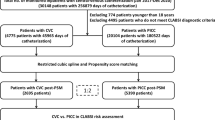
The eligible participants were 1554 consecutive patients who required central venous access, as CVC or PICC, at the Department of Surgery in Fujita Health University Hospital between January 2018 and December 2021. During the study period, PICCs and CVCs (including those in central venous ports) were inserted in 1424 and 130 patients, respectively. Of the 1424 patients with PICCs, 1322 were enrolled in this study, after the exclusion of 102 patients whose PICCs were placed by a physician. Informed consent for PICC insertion was obtained from all patients by the operators themselves under the supervision of physicians, based on the premise that they are responsible for all interventions that FNPs can perform. Informed consent for this study was obtained through an opt-out method.
Registration as a Fujita nurse practitioner (FNP)
To be eligible for enrolment in the Fujita NP (FNP) program, registered nurses must have ≥ 5 years of clinical experience and must obtain at least 55 academic credits and > 1410 h of clinical learnings in 2 years at Fujita Health University. In the first year, 39 credits and 690 h of lectures about physical assessment, pharmacology, and pathophysiology are required. In the second year, the requisites are 16 credits and 720 h of bedside learning. To achieve bedside learning, the FNPs must pass the objective structured clinical examination (OSCE) at the end of the first year. Graduates will have acquired the following seven competencies as NPs in Japan: (1) advanced physical and environment assessment, (2) advanced clinical management, (3) expert clinical practice, (4) administration, (5) collaboration with other professionals, (6) consultation, and (7) ethical decision making [2, 4]. To be registered as an FNP, the following three credentials are necessary: (1) certification by this NP graduate course, (2) certification by the Japanese Organization of Nurse Practitioner Faculties, and (3) expertise in 38 specified interventions [15] grouped into 21 categories [16] defined by the Ministry of Health, Labour, and Welfare in Japan. Initially, two FNPs were assigned to our department and another FNP was assigned in April 2021. The junior FNPs rotated in our department for 1–3 months, in turns.
Selection of PICCs
Two different types of PICC are used depending on the purpose. The Groshong® catheter (single lumen, 4 Fr, 60 cm, Becton, Dickinson, and Company; Franklin Lakes, NJ, the USA) is used mainly for parenteral nutrition and chemotherapy. This type of catheter is made of silicone to enhance biocompatibility and has a three-way valve to reduce blood reflux and clotting. Alternatively, the Power PICC® catheter (Becton, Dickinson, and Company) is used primarily for perioperative management and venous access, including as the injection root for contrast media. This catheter has three types: a single lumen [4 Fr/55 cm], a double lumen [5 Fr/55 cm], and a triple lumen [5 Fr/55 cm]). Moreover, it can allow the injection of contrast media for a contrast-enhanced CT scan at a maximum rate of 5 mL/s. Multiple lumen power PICC® catheters are selected for patients scheduled to undergo esophagectomy and hepatobiliary pancreatic surgery and for clinically ill patients requiring management such as transfusion, sedatives and catecholamines.
PICC insertion by FNPs
In the FNP program, the OSCE includes the skill test for PICC insertion using the PICC simulators (MW18, Kyoto Kagaku, Kyoto). To pass the OSCE, this procedure was practiced repeatedly by FNP students. Moreover, the instructor teaching PICC insertion should have the following credentials: (1) certification by the Committee of the CVC at Fujita Health University Hospital, (2) ≥ 3 years of clinical experience as an FNP, and (3) ≥ 30 cases of successful PICC insertion. The instructor should also be able to perform PICC insertion independently. FNP trainees can perform PICC insertion under the supervision of a physician or the PICC insertion instructor. If the operator fails twice to complete the insertion, the PICC insertion instructor or the physician performs the procedure. After four failed attempts, the PICC is withdrawn. The basilic vein in the brachium is the preferred vein for insertion and the brachial vein is the alternative.
Procedure for PICC insertion by FNPs
Patients were monitored from the time of PICC insertion until its removal. Maximal sterile barrier precautions, with the use of a large sterile drape, surgical hand antisepsis, and a mask, cap, sterile gloves, and gown, were mandatory during catheter insertions, according to the recommendations of the U.S. Centers for Disease Control and Prevention [17]. Ultrasonography-guided puncture using the Sonosite SII portable ultrasound machine (Fujifilm Co., Tokyo) with an HSL25x, 6–13-MHz linear transducer (Fujifilm Co.) was performed for all catheter insertions, as described in previous studies [18, 19] (Fig. 1). Briefly, after disinfection with 2% chlorhexidine and the administration of local anesthesia (1% lidocaine), the site was punctured with real-time ultrasonographic guidance by positioning the ultrasonic probe in the short-axis direction relative to the vein. After the needle was inserted into the vein, the guidewire was introduced. Subsequently, the opening was expanded using a dilator. After removing the dilator component of the peel-away sheath, the PICC was introduced via the sheath. Next, the catheter tip was advanced into the superior vena cava at the level of the bifurcation of the trachea under fluoroscopic guidance (Fig. 1). All catheters were flushed routinely with 10 mL of 0.9% sodium chloride every 3 days. No heparin products were used to flush or lock the PICC. Every 2 days, or earlier if clinically required, the nursing staff changed the dressing, cleaned the insertion site and catheter hub with an iodine solution, and changed the intravenous accessory tubing.
Representative findings in the investigation of peripherally inserted central catheter (PICC) insertion by the Fujita nurse practitioners (FNPs). (A) The intraoperative finding of PICC insertion using ultrasound and fluorescent images. (B) Ultrasonographic image during venous puncture. The needle tip was identified by the short-axis method (black arrow). (C) Fluoroscopic image during catheter insertion. (D) The completion of PICC insertion
Measurements
To obtain data, we reviewed our department’s prospectively maintained database. The primary outcome of this single-center retrospective analysis was the rate of successful PICC insertion. Secondary endpoints were clinicopathological characteristics and procedural outcomes, including the duration of the insertion procedure (PICC placement time), the rate of insertion-related complications, the rate of central line–associated bloodstream infection (CLABSI), and the duration of PICC placement. The puncture time was defined as the time from disinfection of the operative field to guide-wire placement. The total PICC placement time was defined as the time from disinfection of the operative field to catheter fixation. CLABSI was defined as the presence of bacteremia or fungemia originating from the PICC, according to the definition established by the Centers for Disease Control and Prevention [17]. This includes a positive blood culture result from the catheter and/or the peripheral vein with clear evidence showing the catheter as the source, as well as clinical symptoms of infection [17].
Statistical analyses
We used IBM SPSS Statistics 26 (IBM Corporation, Armonk, NY, USA) to perform all statistical analyses. To perform between-group comparisons, we used the χ2 test for categorical variables and the Mann–Whitney U test for continuous variables. The χ2 test was used for univariable analysis; factors with a P value of < 0.05 were then subjected to multivariable logistic regression. The median value was used to define the cutoff values for each factor during the univariable and multivariable analyses. Data were calculated as medians with interquartile ranges or as odds ratios (ORs) with 95% confidence intervals (CI) unless otherwise noted. Two-tailed P values of < 0.05 were considered significant.
Results
Annual trends in the insertion of central lines
Figure 2 illustrates the annual trends in the insertion of central lines in our department. The number of PICC insertions by FNPs increased yearly, from 261 in 2018, to 309 in 2019, 326 in 2020, and 426 in 2021. The number of PICC insertions by physicians also increased gradually (16, 24, 28, and 34, respectively). In contrast, the total number of CVC insertions during this study period was 142 (71 directly in central veins and 71 through central venous ports) and this decreased gradually after 2019 (Fig. 2).
Outcomes of PICC insertion
PICC insertion was attempted by 23 FNPs: 4 FNP instructors and 19 FNP trainees, and was successful in 1310 (99%) of the 1322 patients. The rates of successful PICC insertion by instructors and trainees were 99% (in 1134 of 1141 patients) and 99% (in 143 of 144 patients), respectively. In contrast, the success rate when there was a need to switch from trainees to instructors was 89% (in 33 of 37 patients). There was no incidence of requirement to switch from an FNP to a physician. Only one puncture was required for 1107 (84%) patients, two punctures were required for 139 (10.5%), and three or more were required for 76 (6%). Table 1 summarizes the backgrounds of the 1310 patients with successful PICC insertion by an FNP. The median age of the patients was 71 years (61–78 years), 896 patients had no history of PICC insertion, and 414 patients had undergone prior PICC insertion. The patients’ pathological conditions were malignant in 68% and benign in 32%. The purpose of PICC insertion was for parenteral nutrition in 685 patients (52%), for venous administration of medication in 362 (28%), for chemotherapy in 103 (8%), and for perioperative management in 160 (12%). The median PICC insertion time was 5 min (5–10 min) and the median time taken to place the PICC was 12 min (10–15 min; Table 1). The PICCs were inserted in the basilic vein in the brachium in 957 (73%) patients, in the brachial vein in 346 (26%), in the saphenous vein in 5 (0.4%), and in the cephalic vein in the brachium in 2 (0.15%).
Intraoperative complications occurred in two patients (0.15%; Table 1): one patient experienced upper limb numbness while the dilator was being used, which resolved immediately after the removal of the dilator. In another patient, the catheter migrated into the azygos vein, but after removal of the PICC, no further event occurred. Among the 12 patients in whom initial PICC insertion failed, instructors attempted subsequent insertion in 8 and trainees, in 4. The causes of failure were venous dilation as a result of obesity in one patient, thrombotic occlusion (the guide wire could not be passed) in three patients, stenosis in the central vein (failure to perform cannulation despite the successful passage of the guide wire) in four patients, and venous collapse as a result of hypovolemia in four patients (Table 2). In the four patients with hypovolemia, PICC insertions were successful several days later, after the hypovolemia was corrected. In the other eight patients, CVCs were inserted by physicians.
Outcomes after PICC insertion
The median duration of PICC placement was 15 days (10–23 days). The collective total number of catheter days was 23,619 (Table 3). The treatment via PICC was completed in 69% of patients, with a median duration of PICC placement of 16 days (10–23 days). PICCs were replaced in 10% of the 1310 patients, among whom the median duration of PICC placement was 19 days (8–29 days). PICCs were removed accidentally in 276 patients (21%), but the most frequent reason for removal was fever, in 206 patients (15.7%; Table 3). Catheter-related thrombosis was confirmed in five patients (0.4%). CLABSI was confirmed in 45 patients (3.4%) and occurred on 1.9 per 1000 catheter days (Table 4). The duration of PICC placement was 15 (10–23) days for patients with CLABSI. Table 4 lists the causative microorganisms in the 45 CLABSI cases. Staphylococcus species, including methicillin-resistant Staphylococcus epidermidis, methicillin-resistant Staphylococcus aureus, and methicillin-sensitive S. aureus, were the most prevalent (45%). Fungi, including Candida albicans and Candida parapsilosis, were the second most prevalent (33%).
Risk factors for removal because of fever
To identify the risk factors for removal because of fever, we performed a univariable analysis of factors related to patients’ backgrounds and surgical procedures (Table 5). The univariable and multivariable analyses revealed that a history of prior PICC insertion (OR, 1.517; 95% CI, 1.111–2.070; p = 0.009), the use of anticoagulants (OR, 1.588; 95% CI, 1.079–2.336; p = 0.019), and the use of multi-lumen catheters were significant risk factors (OR, 1.541; 95% CI, 1.089–2.179; p = 0.015; Table 5). On the other hand, to identify the surgical risk factors for CLABSI, we performed univariable and multivariable analyses of factors related to the patients’ backgrounds and surgical procedures (Supplementary Table). The univariable and multivariable analyses revealed that the use of multi-lumen catheters was the only significant risk factor for CLABSI (OR, 2.183; 95% CI, 1.170–4.082; p = 0.023; Supplementary Table).
Discussion
This single-center retrospective study examined 1322 patients who underwent PICC insertion, which failed in only 12 (1%) during the observation period. The rate of successful PICC insertion by 23 FNPs was very high (99%) during the 4-year study period, and the rate of intraoperative complications was only 0.2%. The success rate was similar to those of previous reports (ranging from 92 to 99%) [8, 11]. Therefore, our results suggest that PICC insertion by specially trained NPs is a safe, highly reproducible, and reliable procedure in Japan. Although PICCs were removed unexpectedly in 21% of the patients, the rate of treatment completion with PICC was 69%, and the median duration of PICC placement was 16 days. These outcomes suggest that the PICC fulfills its purpose. To the best of our knowledge, this is the first report of a large-scale study demonstrating the clinical efficacy of PICC insertion by NPs in the field of gastroenterological surgery in Japan.
Based on a report from the CVC committee of our institution (unpublished data), the complications were comparable between PICCs and CVCs (1.4% [52/3661] vs. 1.6% [47/2878], p = 0.484) during the same study period (from 2018 to 2022, Supplementary Table 2). According to a previous RCT by Parienti et al., the incidences of mechanical complications were 2.1% (18/843), 1.4% (12/845), and 0.7% (6/844) in patients with a CVC inserted in the subclavian, jugular, and femoral veins, respectively [20]. Furthermore, the incidences of pneumothorax were 1.5%, 0.5%, and 0% in patients with a CVC inserted in the subclavian, jugular, and femoral veins, respectively [20]. In a recent prospective study by Adrian et al., the incidence of mechanical complications of CVC was 7.7% (978/12,677), of which 0.4% were major complications including hemorrhage, cardiac arrythmia, arterial catheterization, pneumothorax, and persistent nerve injury [21]. Based on these findings, PICC insertion is comparable to the placement of a central venous line, or even safer, as it prevents major complications including pneumothorax. A recent study conducted by another team in our institution revealed that the success rate of PICC insertion was comparable between FNPs and physicians (97% [1460/1505] vs. 96.1% [697/725], respectively; p = 0.72). Moreover, the complication rate of FNP-led PICC insertion was significantly lower than that of physician-led PICC insertion (1.5% vs. 5.1%, p < 0.001) [19]. Therefore, FNP-led PICC insertion can become an alternative to CVC insertion or physician-led PICC insertion in clinical settings.
Interestingly, the CLABSI rate in this study was 3.4%, occurring on 1.9 per 1000 catheter days. This finding is comparable to that in a previous study of all outcomes after PICC insertion by NPs in our hospital (including those in the department of medicine, the department of surgery, and the intensive care unit: a total of 23,088 PICCs), in which the CLABSI rate was 6.1% and CLABSI occurred on 2.99 per 1000 catheter-days [22]. In previous prospective studies, the incidence of CLABSI after PICC insertion ranged from 1.3% to 2.1% [23, 24], and CLABSI occurred on 0.95 to 2.5 per 1000 catheter days [24,25,26]. In another study, however, CLABSI occurred at 0.47 to 6.6 per 1000 PICC days [27]. Therefore, the incidence of CLABSI in this study is comparable to those of previous reports.
In this study, the operator, PICC insertion time, and PICC placement periods were not identified as risk factors for removal because of either fever or CLABSI, although the use of anticoagulants, the use of multi-lumen catheters, and a history of prior PICC insertion were identified as risk factors for removal because of fever, and only the use of multi-lumen catheters was identified as a risk factor for CLABSI. Baxi et al. also documented that triple-lumen catheters were associated with an increased incidence of CLABSI [28]. These findings suggest that procedure-related factors do not necessarily increase the risk of CLABSI.
Although the use of PICCs entails a low risk for CLABSI, a previous meta-analysis showed that the overall incidence of PICC-related symptomatic venous thromboembolism was 3.7% and that the risk was higher with PICCs than with CVCs [29]. However, the incidence of thrombosis in our study was very low, at 0.4%, which is superior to those in previous reports. We attribute this low rate to the relatively short duration of PICC placement (approximately 2 weeks in most patients), although we cannot deny the possibility of a thrombus that was not detected during routine follow-up or by appropriate modalities. Thus, we demonstrated that PICC insertion not only can be safely performed by NPs but also has a low risk for complications even after placement.
The insertion time of 12 min was comparable to the 11 min reported in a previous study from our hospital [22]. Scimò et al. demonstrated that a well-trained nurse was able to insert a PICC within 10 min, with 73% of insertions by nurses completed in < 10 min [11]. Therefore, the time required for PICC insertion appears to be approximately 10 min. Prior to performing the procedure, the FNPs obtained informed consent from the patients, ordered the examinations associated with PICC insertion, prepared for the ultrasonographic examination, and gave instructions to nurses after PICC insertion. Even after the PICC insertion, FNPs also perform daily rounds to check the insertion site for any abnormalities after PICC placement and to remove that PICC if necessary. Our findings reinforce that PICC insertion by NPs can contribute greatly to reducing PICC-related physical and psychological burden among surgeons. Moreover, NPs skilled in inserting PICCs could educate inexperienced trainees, residents, fellows, and other NPs, thereby also reducing the educational burden. Therefore, we believe that the active participation of FNPs in clinical practice will enable sufficient task shifting among medical professionals.
This study had several limitations. First, it had a retrospective, single-center, single-arm design and we did not directly compare the clinical efficacy of PICC insertion by FNPs with that of CVC insertion or PICC insertion by physicians. Although our results, based on extensive data (> 1000 patients), are reliable to an extent, various patient biases cannot be ignored. Further studies, including large-scale, multicenter prospective investigations, are warranted to clarify the efficacy of PICC insertion by NPs. Second, our study period excluded the time before the first FNP assigned to our department achieved sufficient experience with PICC insertion. Therefore, the learning curve of inserting PICCs safely and quickly was not clarified. Third, with regard to task shifting, we did not investigate the time-saving effects or effects on alleviating the surgeon’s psychological burden. It is important to continue establishing solid evidence that PICC insertion by NPs could become key in alleviating burnout among overworked surgeons. Fourth, although PICCs were removed from 206 patients (15.7%) because of fever, CLABSI was eventually diagnosed in only 45 (3.4%) patients, and we did not investigate the causes of fever in these patients. The causes of fever, including febrile neutropenia after chemotherapy, postoperative intra-abdominal infectious complications, pneumonia, and urinary tract infections, were obvious in most patients; however, some patients may have been harboring microorganisms that were not detected in the blood and catheter, despite strong suspicion of CLABSI. Therefore, the true incidence of CLABSI may be higher than that documented in this study. Fifth, the cost-effectiveness of PICC insertion by NPs was not evaluated in this study. In Japan, the medical reimbursements for PICCs and CVCs covered by the Japanese national medical insurance are 7000 and 14,000 JPY, respectively. In contrast, the costs of CVCs and PICCs are as follows: CVC-single, 1790 JPY; CVC-double/triple, 7210 JPY; PICC-single, 13,400 JPY; and PICC-double/triple, 20,900 JPY. Therefore, hospitals incur higher costs for PICCs. However, Chen et al. and Pernar et al. have shown that PICCs are cost-effective as they can prevent bloodstream infection and thrombotic complications [30, 31]. Further investigation should be conducted to validate the cost-effective benefit of PICCs.
In conclusion, PICCs can be inserted safely by NPs, and this practice could become an alternative to the insertion of CVCs by surgeons. In the future, we hope to reduce the burden of gastroenterological surgeons by expanding the roles of NPs in the Japanese healthcare system.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Ministry of Health, Labour and Welfare [internet]. Act on the arrangement of related acts to promote work style reform updated Jul 2018. AVAILABLE from: https://www.mhlw.go.jp/content/000332869.pdf. Accessed 27 Jan 2023.
Fukuda H, Miyauchi S, Tonai M, Ono M, Magilvy JK, Murashima S. The first nurse practitioner graduate programme in Japan. Int Nurs Rev. 2014;61:487–90.
Fujita Health University [internet]. Department of Fujita Nurse Practitioner updated. 2020. Available from. https://www.department-of-fnp.com/. Accessed 27 Jan 2023.
Japanese Nursing Association [internet]. Nursing in Japan updated 2023. Available from. https://www.nurse.or.jp/english/assets/nursung/nursing-in-japan-en.pdf. Accessed 27 Jan 2023.
Taxbro K, Hammarskjöld F, Thelin B, Lewin F, Hagman H, Hanberger H, et al. Clinical impact of peripherally inserted central catheters vs implanted port catheters in patients with cancer: an open-label, randomised, two-centre trial. Br J Anaesth. 2019;122:734–41.
McDiarmid S, Scrivens N, Carrier M, Sabri E, Toye B, Huebsch L, et al. Outcomes in a nurse-led peripherally inserted central catheter program: a retrospective cohort study. CMAJ Open. 2017;5:E535–9.
Moureau N. Vascular safety: it’s all about PICCs. Nurs Manage. 2006;37(22):7.
Park JY, Kim HL. A comprehensive review of clinical nurse specialist-led peripherally inserted central catheter placement in Korea: 4101 cases in a tertiary hospital. J Infus Nurs. 2015;38:122–8.
Maki DG, Kluger DM, Crnich CJ. The risk of bloodstream infection in adults with different intravascular devices: a systematic review of 200 published prospective studies. Mayo Clin Proc. 2006;81:1159–71.
Ng PK, Ault MJ, Ellrodt AG, Maldonado L. Peripherally inserted central catheters in general medicine. Mayo Clin Proc. 1997;72:225–33.
Scimò M, Vallecorsa I, Cini A, Cabelguenne D, Piriou V. Vascular access unit: six-years experience report in France. J Vasc Access. 2022. https://doi.org/10.1177/11297298221080228.
Jie C, Chunxue P, Jiawei X, Hongmei L, Huohong Q. Multidisciplinary cooperative mode led by infusion nurse specialists used to ensure the nursing quality of peripherally inserted central catheters in China: a 5-year retrospective study. J Vasc Access. 2021. https://doi.org/10.1177/11297298211033507.
Bedford E, Waterhouse D. Service development of a nurse-led community-based PICC insertion service. Br J Nurs. 2017;26:S22–7.
Oakley C, Wright E, Ream E. The experiences of patients and nurses with a nurse-led peripherally inserted central venous catheter line service. Eur J Oncol Nurs. 2000;4:207–18.
Ministry of Health, Labour and Welfare [internet] cited 27 Jan 2023. Available from: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000050325.html. 38 specified interventions.
Ministry of Health, Labour and Welfare [internet] cited 27 Jan 2023. Available from: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/0000077098.html. 21 categories.
O’Grady NP, Alexander M, Burns LA, Dellinger EP, Garland J, Heard SO, et al. Guidelines for the prevention of intravascular catheter-related infections. Clin Infect Dis. 2011;52:e162–93.
Parkinson R, Gandhi M, Harper J, Archibald C. Establishing an ultrasound guided peripherally inserted central catheter (PICC) insertion service. Clin Radiol. 1998;53:33–6.
Sakai H, Hirosue M, Iwata M, Terasawa T. The effect of introducing a nurse-practitioner-led peripherally inserted central venous catheter placement program on the utilization of central venous access device: A retrospective study in Japan. J Vasc Access. 2023. https://doi.org/10.1177/11297298231173160.
Parienti JJ, Mongardon N, Megarbane B, Mira JP, Kalfon P, Gros A, et al. Intravascular complications of central venous catheterization by insertion site. N Engl J Med. 2015;373:1220–9.
Adrian M, Borgquist O, Kroger T, Linne E, Bentzer P, Spangfors M, et al. Mechanical complications after central venous catheterization in the ultrasound-guided era: a prospective multicentre cohort study. Br J Anaesth. 2022;129:843–50.
Sakai H, Iwata M, Terasawa T. External validation of the Michigan PICC catheter-associated bloodstream infections score (MPC score) for predicting the risk of peripherally inserted central catheter-associated bloodstream infections: a single-center study in Japan. Infect Control Hosp Epidemiol. 2021;44:1–4.
Kang J, Chen W, Sun W, Ge R, Li H, Ma E, et al. Peripherally inserted central catheter-related complications in cancer patients: a prospective study of over 50,000 catheter days. J Vasc Access. 2017;18:153–7.
Bertoglio S, Faccini B, Lalli L, Cafiero F, Bruzzi P. Peripherally inserted central catheters (PICCs) in cancer patients under chemotherapy: A prospective study on the incidence of complications and overall failures. J Surg Oncol. 2016;113:708–14.
Nolan ME, Yadav H, Cawcutt KA, Cartin-Ceba R. Complication rates among peripherally inserted central venous catheters and centrally inserted central catheters in the medical intensive care unit. J Crit Care. 2016;31:238–42.
Mollee P, Jones M, Stackelroth J, KuilenburgJoubert RvW, Faoagali J, et al. Catheter-associated bloodstream infection incidence and risk factors in adults with cancer: a prospective cohort study. J Hosp Infect. 2011;78(26):30.
Morano SG, Latagliata R, Girmenia C, Massaro F, Berneschi P, Guerriero A, et al. Catheter-associated bloodstream infections and thrombotic risk in hematologic patients with Peripherally Inserted Central Catheters (PICC). Support Care Cancer. 2015;23:3289–95.
Baxi SM, Shuman EK, Scipione CA, Chen B, Sharma A, Rasanathan JJK, et al. Impact of postplacement adjustment of peripherally inserted central catheters on the risk of bloodstream infection and venous thrombus formation. Infect Control Hosp Epidemiol. 2013;34:785–92.
Puri A, Dai H, Giri M, Wu C, Huang H, Zhao Q. The incidence and risk of venous thromboembolism associated with peripherally inserted central venous catheters in hospitalized patients: a systematic review and meta-analysis. Front Cardiovasc Med. 2022;9: 917572.
Chen N, Yang Q, Feng Y, Guo Q, Huang DY, Peng JL. Cost-utility analysis of different venous access devices in breast cancer patients: A decision-based analysis model. BMC Health Serv Res. 2023;23:497.
Pernar LI, Wolf LL, Seshadri A, Patel V. Impact of a surgeon-led peripherally inserted central venous catheter team on peripherally inserted central venous catheter-related complications and costs. Surg Infect. 2016;17:352–6.
Acknowledgements
The authors thank Maruzen-Yushodo Co., Ltd. (https://kw.maruzen.co.jp/kousei-honyaku/) for English language editing.
Funding
This study was approved by the Institutional Review Board of Fujita Health University (HM22-483).
Author information
Authors and Affiliations
Contributions
All authors have fully satisfied the ICMJE authorship criteria as follows: study design: Yuriko Takematsu, Susumu Shibasaki, and Koichi Suda; data collection: Yuriko Takematsu, Tsuyoshi Tanaka, Junichiro Hiro, Takeshi Takahara, and Hiroshi Matsuoka; statistical analysis and interpretation of results: Susumu Shibasaki, Junichiro Hiro, Takeshi Takahara, and Koichi Suda; drafting of the manuscript: Yuriko Takematsu, Susumu Shibasaki, and Koichi Suda; and critical revision of the manuscript for important intellectual content: Susumu Shibasaki, Ichiro Uyama, and Koichi Suda. All authors have read and approved the final manuscript and are accountable for all aspects of the work, particularly in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
Yuriko Takematsu, Susumu Shibasaki, Tsuyoshi Tanaka, Junichiro Hiro, Takeshi Takahara, Hiroshi Matsuoka, Ichiro Uyama, and Koichi Suda have no commercial association or financial involvement that might be construed as a conflict of interest in connection with the submitted article. Ichiro Uyama has received lecture fees from Intuitive Surgical, Inc., outside the submitted work. Tsuyoshi Tanaka and Ichiro Uyama have been funded by Medicaroid, Inc., in relation to the Collaborative Laboratory for Research and Development in Advanced Surgical Technology, Fujita Health Inc. Koichi Suda has been funded by Medicaroid, Inc., in relation to the Collaborative Laboratory for Research and Development in Advanced Surgical Intelligence, Fujita Health University, and has also received advisory fees from Medicaroid, Inc., outside the submitted work.
Informed consent
Informed consent for this study was obtained through an opt-out method.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Takematsu, Y., Shibasaki, S., Tanaka, T. et al. The safe implementation of peripherally inserted central catheters by nurse practitioners for patients with gastroenterological diseases in Japan: a single-center retrospective study. Surg Today 54, 487–495 (2024). https://doi.org/10.1007/s00595-023-02748-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-023-02748-z