Abstract
Purpose
Endoscopic submucosal dissection is recommended for early gastric cancer with a low risk of lymph node metastasis. When the pathological findings do not meet the curative criteria; then, an additional gastrectomy with lymph node dissection is recommended. However, most cases have neither lymph node metastasis nor a local residual tumor during an additional surgery.
Methods
This was a single-institutional retrospective cohort study, analyzing 200 patients who underwent an additional gastrectomy after non-curative endoscopic submucosal dissection from January 2005 to October 2015. We reviewed the patients’ clinicopathological data and evaluated the predictors for the presence of a residual tumor.
Results
Histopathology revealed lymph node metastasis in 15 patients (7.5 %) and a local residual tumor in 23 (11.5 %). A multivariable analysis revealed macroscopic findings (flat/elevated type) (p = 0.011, odds ratio = 4.63), lymphatic invasion (p < 0.0001, odds ratio = 14.2), and vascular invasion (p = 0.04, odds ratio = 4.00) to be predictors for lymph node metastasis. A positive vertical margin (p = 0.0027, odds ratio = 3.26) and horizontal margin (p = 0.0008, odds ratio = 5.74) were predictors for a local residual tumor. All cases with lymph node metastasis had lymphovascular invasion with at least one other non-curative factor.
Conclusions
The risk of a residual tumor can, therefore, be estimated based on the histopathology of endoscopic submucosal dissection samples. Lymphovascular invasion appears to be a pivotal predictor of lymph node metastasis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recent progress in diagnostic technology has increased the detection of early gastric cancer (EGC), especially in Japan and Korea, where nationwide screening systems have been established, and where EGC exceeds 50 % of all detected gastric cancer. EGC is defined as invasive cancer existing within the submucosa, regardless of the presence of lymph node (LN) metastasis. A large-scale analysis of surgical EGC revealed that the majority of EGC cases have no LN metastasis [1, 2]; therefore, endoscopic intervention, currently the performance of endoscopic submucosal dissection (ESD), has been recommended when patients are diagnosed with possible EGC with low risk of LN involvement.
According to the 2010 Japanese Gastric Cancer Association (JGCA) treatment guidelines [3], the absolute indications for endoscopic resection are the following tumor characteristics: differentiated-type in histology, T1a, ulceration (UL) (−), and ≤2 cm in diameter. The following are expanded indications: (a) differentiated-type, T1a, UL (−), but >2 cm; (b) differentiated-type, T1a, UL (+), and ≤3 cm; and (c) undifferentiated-type, T1a, UL (−), and ≤2 cm. The JGCA guidelines include the pathological criteria of curative resection after ESD, and patients not fulfilling the criteria are diagnosed as non-curative resection. For the non-curative resection patients, an additional gastrectomy with LN dissection is recommended because of the potential risk of LN metastasis or a local residual tumor. Although the JGCA guidelines recommend an additional surgery based on these criteria, many cases have neither LN metastasis nor a local residual tumor in surgical specimens obtained during an additional surgery. Therefore, avoiding unnecessary surgery is desirable regarding surgical invasiveness, medical costs, and expected effects on the patients’ quality of life. However, clinically, it can be difficult to decide whether to perform additional surgery when a patient is elderly or in the poor general condition, even if the pathological findings do not satisfy the criteria. In addition, the indications for ESD have recently been expanded; therefore, it is even more important to clarify the predictive factors for the presence of residual cancer.
This retrospective cohort study aimed to analyze the clinicopathological features of patients who underwent additional gastrectomy after ESD in our institution as well as to determine the predictive factors for LN metastasis or a local residual tumor and to identify the optimal strategy or management of non-curative resection after ESD.
Methods
Study design
This was a retrospective single-institutional cohort study using a clinical database. The medical records of patients who underwent additional gastrectomy after ESD from January 2005 to October 2015 at our institution were retrospectively reviewed. The incidence of pathologically proven LN metastasis or local residual tumor was investigated. In addition, using clinicopathological variables, the predictive factors for these outcomes were estimated by the univariable and multivariable analyses. This study was approved by the Institutional Review Board of the National Cancer Center, Japan (IRB file No.: 2015-050, approval date: May. 27, 2015).
ESD procedure
All ESD procedures were performed by endoscopic instructors or skillful endoscopists using a single-channel upper gastrointestinal endoscope (GIF-Q260J; Olympus Medical Systems, Tokyo, Japan) with a water-jet system (OFP; Olympus), and a high-frequency generator (ICC200 or VIO300D; Erbe Elektromedizin Ltd, Tuebingen, Germany). The transparent attachment (disposable distal attachment; Olympus) was fitted onto the tip of the endoscope.
The mucosa around the lesion was cut circumferentially with an insulation-tipped diathermic knife 2 (IT knife 2; Olympus) after injection into the submucosal layer of 0.4 % sodium hyaluronate (MucoUp®; Johnson & Johnson, Tokyo, Japan) diluted with normal saline solution to create a submucosal cushion. The swollen submucosal layer was subsequently dissected with the same devices after additional injections into the submucosal layer. All patients underwent ESD using carbon dioxide (CO2) insufflation.
The patients were placed in the left lateral decubitus position and put under sedation with an intravenous injection of 2–3-mg midazolam and 35-mg pethidine hydrochloride. Sedative drugs were added as required to keep the patients calm, and the patients were monitored with pulse oximeters and administrated oxygen via a cannula when their saturation became low.
Criteria for non-curative resection of ESD
Pathological diagnoses were provided by two authorized pathologists. The pathological findings were evaluated according to the JGCA classification, the third English Edition [4]. In this study, non-curative resection of ESD was diagnosed when the pathological findings did not fulfill the criteria for curative resection as defined by the JGCA guidelines [3]. The JGCA guidelines have been amended several times during the study period. Until 2010, we followed the second edition algorithm and the third edition algorithm until 2014. Since 2014, we have followed the fourth edition algorithm. Following the latest guidelines, in this study, patients were diagnosed as non-curative resection when they satisfied at least one of the following conditions (Table 1): (1) undifferentiated dominant type, and (1-a) submucosal invasion, (1-b) ulceration (+), and (1-c) >2 cm; (2) differentiated dominant type, and (2-a) the existence of an undifferentiated component in the submucosal (sm) layer, (2-b) within mucosa but ulceration (+) and >3 cm, (2-c) sm1 invasion (<500 μm) and >3 cm, and (2-d) sm2 invasion (≥500 μm); (3) lymphatic invasion (+); (4) vascular invasion (+); (5) vertical margin (VM) (+) or could not be assessed; (6) horizontal margin (HM) (+) or could not be assessed; and (7) without en-bloc resection. Tubular adenocarcinoma and papillary adenocarcinoma were defined as differentiated. Poorly differentiated adenocarcinoma, signet-ring cell adenocarcinoma, and mucinous adenocarcinoma were defined as undifferentiated. The histological type was determined according to each quantitatively predominant component.
Additional gastrectomy
The type of gastrectomy was determined based on the location of the ESD scar [3]. Regarding the extent of LN dissection, in principle, D1 + dissection was performed, but D2 was also done when an undifferentiated tumor massively invaded the submucosa in an ESD specimen. The surgical approach has changed over time with open surgery performed until 2009 and laparoscopic surgery the predominant choice since 2010. Robot-assisted surgery was introduced in 2014 as a clinical investigation. The grading of postoperative complications was done according to the Clavien-Dindo classification system [5].
Statistical analysis
All analyses were conducted by the Chi-square test using the JMP software version 12.0 for windows (SAS Inc., Cary, NC, USA). Univariable and multivariable analyses were performed using a logistic regression analysis. p < 0.05 was considered statistically significant. Odds ratios (OR) and 95 % confidence intervals (CI) were also calculated for the multivariable analyses.
Results
Patients’ characteristics
A total of 1884 patients underwent ESD between January 2005 and October 2015 at our institution. Among these, 1349 (71.6 %) satisfied the criteria of curative resection. In 535 patients, (28.4 %) diagnosed as non-curative resection, 310 (16.5 %) were observed without further treatment, because the patients either declined treatment or had a poor general condition related to comorbidities, five (0.27 %) underwent repeat ESD, and the remaining 200 (10.6 %) underwent additional gastrectomy (Fig. 1). The clinicopathological features of these 200 patients are summarized in Table 2. Among them, 95 patients (47.5 %) underwent ESD as absolute indications of the JGCA guidelines, 98 patients (49 %) as expanded indications and 7 patients (3.5 %) beyond these indications, but with a diagnostic intent due to the patients’ request or conditions. Regarding the macroscopic appearance of the primary tumor, a depressed type was the most common (72 %). Histologically, the undifferentiated dominant type was recorded in 15.0 % of patient specimens. The pathological statuses defining non-curative resection in these 200 patients are shown in Table 1. The most frequent factor for non-curative resection was sm2 invasion in the differentiated dominant type (58.5 %), and the second was lymphatic invasion (36.5 %). VM (+), and HM (+) were recognized in 17.5 and 17.0 % of the specimens, respectively.
Flowchart after ESD for clinically early gastric cancer. Among 1884 patients who underwent ESD, 1349 fulfilled the criteria of curative resection. In 535 patients diagnosed as non-curative resection, 310 were observed without treatment, five underwent repeat ESD, and the remaining 200 underwent additional gastrectomy. ESD endoscopic submucosal dissection
Additional surgery
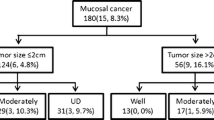
The most common procedure was distal gastrectomy (65.5 %). Proximal gastrectomy, a type of function-preserving surgery, was also commonly performed (21.0 %) (Table 3). Approximately half of the patients underwent laparoscopic surgery (46.5 %), no deaths were observed related to the surgery. Ten patients (5.0 %) developed grade III postoperative complications, including pancreatic fistula or anastomotic leakage. A pathological examination of the surgical specimens revealed LN metastasis in 15 patients (7.5 %) and local residual tumor in 23 patients (11.5 %). When these incidences were analyzed for each of the indication criteria of ESD, the incidence of LN metastasis was 4.2 % in absolute indications, 10.2 % in expanded indications, and 14.0 % beyond these indications. Likewise, the incidence of a local residual tumor was 9.5 % in absolute indications, 13.2 % in expanded indications, and 14 % beyond these indications. The median number of metastatic LNs was 1 (range 1–7). All patients exhibited LN metastasis within D1 + level LN stations for each type of gastrectomy; two patients at station 1, eight at station 3, one at station 4d, two at station 6, two at station 7, two at station 8a, and one at station 11p.
Relationship between the clinicopathological parameters and LN metastasis/a local residual tumor
Table 4 shows the association between the clinicopathological parameters and LN metastasis/local residual tumor. A univariable analysis verified that LN metastasis was associated with the macroscopic appearance (flat/elevated type) (p = 0.004), lymphatic invasion (p < 0.0001), and vascular invasion (p = 0.007). Likewise, a local residual tumor was associated with VM (+) (p = 0.0005) and HM (+) (p < 0.0001). A multivariable analysis also revealed the macroscopic appearance (flat/elevated type) (OR = 4.63, 95 % CI 1.41–16.8), lymphatic invasion (OR = 14.2, 95 % CI 3.55–97.4), and vascular invasion (OR = 4.00, 95 % CI 1.04–18.0) to be independent predictive factors for LN metastasis, and that VM (+) (OR = 3.26, 95 % CI 1.15–8.94) and HM (+) (OR = 5.74, 95 % CI 2.10–15.8) were independent predictive factors for local residual tumor (Table 5). We further examined the patients’ characteristics of a flat/elevated appearance type. As one of the possible associated factors; histologically, a papillary type was also considered. A papillary type was more frequently found in patients with a flat/elevated type (11/56; 19.6 %) compared with those with a depressed type (10/144; 6.9 %), and the difference was statistically significant (p = 0.0012). However, a papillary type was not identified as an independent predictor for LN metastasis.
The clinicopathological characteristics of 15 patients with LN metastasis were further examined, and all 15 patients were diagnosed histopathologically as either lymphatic or vascular invasion positive. In addition, at least one other non-curative factor was present in each patient. Regarding this finding, a 2 × 2 contingency table was created (Table 6) which shows that the sensitivity of this qualification was 100 % (95 % CI 80.5–100 %), specificity was 63.8 % (95 % CI 62.2–63.8 %), positive predictive value was 18.3 % (95 % CI 14.7–18.3 %), and negative predictive value (NPV) as 100 % (95 % CI 97.5–100 %).
Recurrence
The median follow-up period in the additional surgery group was 25.3 months (range 1–126 months). One patient experienced recurrence. This patient had a 0-IIc lesion (45 mm, tub2, cT1a) on the posterior wall of the prepyloric region. Primary ESD was employed as an expanded indication, but the pathological findings of the ESD specimen were sm1 (420 μm), tub2 > por/sig, ly2, v0, pHMX, and pVM0. As additional surgery, laparoscopic distal gastrectomy was performed. In the resected specimen, a residual tumor (poorly differentiated component) was recognized in the subserosal layer apart from the ESD scar. There were seven pathological metastatic LNs (LN stations of No.6, 7, and 8a); therefore, the patient was diagnosed as pT3Na3M0 StageIIIB. Adjuvant chemotherapy was done, but peritoneal recurrence was seen 10 months after the additional surgery.
Discussion
To the best of our knowledge, the present study had the largest number of cases compared with similar published studies. In our 200 cases of additional surgery, the rate of LN metastasis was 7.5 % and the rate of a local residual tumor was 11.5 %, which were similar to the outcomes in previous reports with smaller numbers of cases [6–10].
Regarding local residual tumor at the ESD scar, as expected, positive VM and positive HM were independent predictors in our study, as reported in previous studies [6, 8, 9, 11]. On the other hand, some authors reported only HM as risk factors for local residual tumor because of lower thermal injury caused by electrocoagulation devices [8, 12]. In the present study, actually 32.4 % of patients with positive HM had a local residual tumor. However, we believe that positive VM may suggest deep submucosal invasion of the primary tumor; therefore, careful clinical decision-making is necessary. In our series, 8.6 % of patients with positive VM had LN metastasis and 11.5 % had local residual tumor. The management of positive HM is debated, and there is no persuasive consensus. Several researchers have stated that LN metastasis is very low when positive HM is the only non-curative factor [13]. Numata et al. [14] reported that all local recurrences during follow-up in the positive HM cases that were intramucosal lesions and could be treated by repeat ESD. They concluded that for the positive HM cases, strict surveillance should be considered first; and repeat ESD can be employed when the recurrent lesion is a differentiated intramucosal lesion. Clinically, the decision should be specific for each patient. If there is an additional non-curative factor combined with the positive HM, then additional surgery should be considered.
In terms of ESD for remnant gastric cancer, some researchers have already reported its efficacy and favorable long-term outcomes [15–17], though for lesions involving an anastomotic ring or suture line, this procedure is technically demanding. In our center, ESD for remnant gastric cancer is basically applied with the same indications as that for usual cases. However, given the difficulty of surgical resection, it is likely to be employed as for diagnostic purposes. The current study included four cases (2 %) of ESD for remnant gastric cancer, and these patients received remnant gastrectomy as additional surgery. Among them one local residual tumor was recognized, and actually this patient received ESD for diagnostic purposes in spite of a suspicion of cT1b.
Regarding the predictive factors for LN metastasis, previous reports identified several parameters, including submucosal invasion, tumor size (larger than 2–3 cm), lymphovascular invasion, or undifferentiated-type [6, 7, 11]. Among these factors, several authors emphasized lymphovascular invasion as a crucial prognostic factor [6, 7, 18]. Kim et al. [19] and Lee et al. [20] stated that there was no LN metastasis in patients with the differentiated-type without lymphovascular invasion in their series. Lymphovascular invasion is also a reported prognostic factor in such patients without additional surgery [21, 22]. The present study also revealed that lymphovascular invasion and flat/elevated type are independent risk factors, and we, therefore, made an index to more precisely estimate the risk of LN metastasis using these factors. Interestingly, the condition “lymphovascular invasion plus at least one other non-curative factor” was an indicated factor for estimating LN metastasis, with an NPV of 100 %. High NPV means that this qualification is useful to define a low-risk subpopulation. In other words, patients not meeting this qualification are unlikely to have LN metastasis. This qualification may be helpful when treating elderly patients or patients with severe comorbidities. However, it should be noted that this qualification is not useful for making definitive diagnoses because of its low positive predictive value of 18.3 %. It is unclear why the flat/elevated type was associated with LN metastasis, although Jung et al. [8] also reported similar results. They presumed that the estimation of the invasion depth during diagnostic endoscopy might have been difficult with the elevated type tumor. Sekiguchi et al. [23] reported that the EGC cases with a papillary adenocarcinoma (pap) component were at higher risk for lymphatic invasion and also showed a higher percentage of positive LN metastasis. Actually, in our study, a pap component was found more frequently in 11 (19.6 %) of 56 cases with a flat/elevated type than in 10 (6.9 %) of 144 cases with a depressed type (p = 0.012).
Regarding the optimal extent of LN dissection in the additional surgery, there is also no consensus or ideal recommendation. Performing D1 + dissection appears reasonable, because in principle, ESD-treated lesions are EGC. In the present study, extragastric LN metastasis was detected in four of 15 patients, but all were within D1 + level LN stations. Son et al. [7] also reported the status of LN metastasis after additional surgery, and stated that all except one patient exhibited metastases within level D1+; however, the invasion depth of this exceptional case was T3. If LN metastasis is strongly suspected, for example, several predictive factors coexist, D2 dissection may be selected, because in the JGCA guidelines [4], D2 LN dissection is recommended for patients preoperatively diagnosed with LN involvement. When there is a probability of invasion to the muscle layer (T2) based on the pathological findings, D2 dissection should thus be applied.
There are several limitations associated with our study, including the retrospective design and single-institution setting, which may include some selection bias. To more precisely identify risk factors, studies using larger, multi-institutional databases are required. A prospective study comparing additional surgery and observation, evaluating recurrence rate as an endpoint, should be conducted in the low-risk subpopulation with residual cancer. It also remains necessary to determine the optimal surveillance strategy for patients without additional surgery.
In conclusion, positive HM and VM were found to be independent predictive factors for a local residual tumor, and lymphovascular invasion and a macroscopic flat/elevated type were identified to be predictors for LN metastasis in patients who underwent additional surgery after ESD. Patients without lymphovascular invasion appear to be a low-risk subpopulation for LN metastasis. To determine the indications for additional surgery, both surgeons and gastroenterologists should consider the balance of risk for LN metastasis and a local residual tumor on and individual basis, including the presence of comorbidities or the patient’s life expectancy.
References
Gotoda T, Yanagisawa A, Sasako M, Ono H, Nakanishi Y, Shimoda T, et al. Incidence of lymph node metastasis from early gastric cancer: estimation with a large number of cases at two large centers. Gastric Cancer. 2000;3:219–25.
Hirasawa T, Gotoda T, Miyata S, Kato Y, Shimoda T, Taniguchi H, et al. Incidence of lymphnode metastasis and the feasibility of endoscopic resection for undifferentiated-typeearly gastric cancer. Gastric Cancer. 2009;12:148–52.
Association Japanese Gastric Cancer. Japanese gastric cancer treatment guidelines 2010 (ver. 3). Gastric Cancer. 2011;14:113–23.
Association Japanese Gastric Cancer. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011;14:101–12.
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187–96.
Toyokawa T, Ohira M, Tanaka H, Minamino H, Sakurai K, Nagami Y, et al. Optimal management for patients not meeting the inclusion criteria after endoscopic submucosal dissection for gastric cancer. Surg Endosc. 2015. doi:10.1007/s00464-015-4491-4.
Son SY, Park JY, Ryu KW, Eom BW, Yoon HM, Cho SJ, et al. The risk factors for lymph node metastasis in early gastric cancer patients who underwent endoscopic resection: is the minimal lymph node dissection applicable? A retrospective study. Surg Endosc. 2013;27:3247–53.
Jung H, Bae JM, Choi MG, Noh JH, Sohn TS, Kim S. Surgical outcome after incomplete endoscopic submucosal dissection of gastric cancer. Br J Surg. 2011;98:73–8.
Lee JH, Kim JH, Kim DH, Jeon TY, Kim DH, Kim GH, et al. Is surgical treatment necessary after non-curative endoscopic resection for early gastric cancer? J Gastric Cancer. 2010;10:182–7.
Song KY, Hyung WJ, Kim HH, Han SU, Cho GS, Ryu SW, et al. Is gastrectomy mandatory for all residual or recurrent gastric cancer following endoscopic resection? A large-scale Korean multi-center study. J Surg Oncol. 2008;98:6–10.
Ito H, Inoue H, Ikeda H, Odaka N, Yoshida A, Satodate H, et al. Surgical outcomes and clinicopathological characteristics of patients who underwent potentially noncurative endoscopic resection for gastric cancer: a report of a single-center experience. Gastroenterology Research and Practice. 2013. doi:10.1155/2013/427405.
Yoon H, Kim SG, Choi J, Im JP, Kim JS, Kim WH, et al. Risk factors of residual or recurrent tumor in patients with a tumor-positive resection margin after endoscopic resection of early gastric cancer. Surg Endosc. 2013;27:1561–8.
Kim TK, Kim GH, Park do Y, Lee BE, Jeon TY, Kim DH, et al. Risk factors for local recurrence in patients with positive lateral resection margins after endoscopic submucosal dissection for early gastric cancer. Surg Endosc. 2015;29:2891–8.
Numata N, Oka S, Tanaka S, Kagemoto K, Sanomura Y, Yoshida S, et al. Risk factors and management of positive horizontal margin in early gastric cancer resected by en bloc endoscopic submucosal dissection. Gastric Cancer. 2015;18:332–8.
Nonoka S, Oda I, Makazu M, Haruyama S, Abe S, Suzuki H, et al. Endoscopic submucosal dissection for early gastric cancer in the remnant stomach after gastrectomy. Gasstroint Endosc. 2013;78:63–72.
Ojima T, Takifuji K, Nakamura M, Nakamori M, Katsuda M, Iida T, et al. Endoscopic submucosal dissection for gastric tumors in various types of remnant stomach. Endoscopy. 2014;46:645–9.
Ojima T, Takifuji K, Nakamura M, Nakamori M, Yamaue H. Long-term survival of patients with endoscopic submucosal dissection for remnant gastric cancers. Surg Laparosc Endo Percutaneous Techn. 2016;26:78–81.
Kim JY, Kim YY, Kim SJ, Park JC, Kwon YH, Jung MK, et al. Predictive factors for lymph node metastasis in signet ring cell gastric cancer and the feasibility of endoscopic submucosal dissection. J Gastric Cancer. 2013;13:93–7.
Kim DJ, Kim W. A case of single lymph node metastasis near the common hepatic artery following a curative endoscopic resection for gastric mucosal cancer. Gastric Cancer. 2014;17:387–91.
Lee IS, Yook JH, Park YS, Kim KC, Oh ST, Kim BS. Suitability of endoscopic submucosal dissection for treatment of submucosal gastric cancers. Br J Surg. 2013;100:668–73.
Kusano C, Iwasaki M, Kaltenbach T, Conlin A, Oda I, Gotoda T. Should elderly patients undergo additional surgery after non-curative endoscopic resection for early gastric cancer? Long-term comparative outcomes. Am J Gastroenterol. 2011;106:1064–9.
Ahn JY, Jung HY, Choi JY, Kim MY, Lee JH, Choi KS, et al. Natural course of noncurative endoscopic resection of differentiated early gastric cancer. Endoscopy. 2012;44:1114–20.
Sekiguchi M, Kushima R, Oda I, Suzuki H, Taniguchi H, Sekine S, et al. Clinical significance of a papillary adenocarcinoma component in early gastric cancer: a single-center retrospective analysis of 628 surgically resected early gastric cancers. J Gastroenterol. 2015;50:424–34.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Rights and permissions
About this article
Cite this article
Sunagawa, H., Kinoshita, T., Kaito, A. et al. Additional surgery for non-curative resection after endoscopic submucosal dissection for gastric cancer: a retrospective analysis of 200 cases. Surg Today 47, 202–209 (2017). https://doi.org/10.1007/s00595-016-1353-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-016-1353-1