Abstract
Aims
The intricate connections between health and the environment are often overlooked globally, yet they play a pivotal role in shaping our well-being.
Results
Astonishingly, environmental risk factors contribute to nearly 24% of the global disease burden, underscoring the critical impact of our surroundings on health. At the crossroads of this issue lies Diabetes, a rapidly growing non-communicable disease that highlights the delicate balance between human health and environmental sustainability. This epidemic offers a unique lens through which to explore how environmental factors contribute to the prevalence of Diabetes, revealing the complex interplay at work. Despite growing awareness, healthcare systems worldwide face challenges integrating environmental threats into more effective diabetes care strategies
Conclusions
This perspective highlights the urgent need for collaborative efforts and innovative solutions that address the environmental dimensions of diabetes management. Doing so can build healthier communities and pave the way for a more sustainable future.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Health and the environment are closely intertwined. However, the significance of this bidirectional relationship could be better perceived globally. Notably, during the United Nations General Assembly 2018, only 13% of the countries participating in the debate made a joint reference to health and climate in their statements [1]. For this very reason, this document aims to emphasize the complex interactions linking human health and the environment by paying particular attention to the socio-economic impacts generated by environmental determinants in the pathogenesis of diabetes mellitus. We also wish to describe potential achievable interventions to mitigate environmental factors impact on the predisposition to pathological glucose tolerance.
Integrated view of health determinants and the role of environmental factors
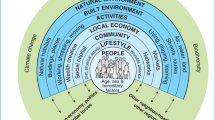
Health determinants are the diverse factors that shape the health outcomes of individuals and communities alike. These determinants encompass various influences, including biological, behavioral, socio-economic, and environmental elements. While access to and quality healthcare services are crucial, they account for only 20% of an individual’s overall health status. The remaining influence comes from a complex interplay of other determinants, particularly environmental factors. Contrary to what one might think, access to and quality of healthcare facilities impact only 20% of health. According to the World Health Organization (WHO) definition, environmental factors are all physical, chemical, biological, and social elements capable of positively or negatively influencing individuals’ health status [2]. Notably, the diseases most impacted by these environmental risks are those with the highest mortality rates, such as cardiovascular diseases, which claim around 2.6 million lives annually, followed by enteric and respiratory infections. This highlights the critical need to address environmental health risks to improve global health outcomes.
The socioeconomic burden of diabetes
The prevalence of type 2 diabetes is drastically increasing globally [3]. It is estimated that approximately 67 million people in Europe will be affected by this condition by 2045 [4]. In the Italian context, the prevalence of type 2 diabetes has doubled in the last decade (2002–2022), rising from 3.9 to 6.6% [5]. This increase is due to the aging population and the adoption of unhealthy lifestyles. Diabetes is tightly linked to other non-communicable diseases, such as obesity, cancer, and chronic obstructive pulmonary disease, all associated with a significantly increased risk of mortality. It is estimated that inadequate glycemic control reduces the patient’s life expectancy by approximately 7–8 years [6]. The escalating prevalence of Diabetes is placing an enormous financial strain on healthcare systems worldwide. The cost of managing this chronic condition in Italy exceeds €20 billion annually.
Of this staggering amount, €9 billion is allocated to direct medical expenses, equating to approximately €2800 per person. The remaining €11 billion accounts for indirect costs, highlighting the far-reaching economic impact of this growing epidemic. As the burden of Diabetes continues to rise, so does the urgency to address this challenge with practical strategies to alleviate both the human and financial costs.
Introduced by Wild, the concept of exposome refers to the environmental factors and pathogens everyone is exposed to throughout their life, starting from conception [7]. Inspired by the concept of the genome, the term "exposome" has evolved over the years to capture a holistic view of our environment’s influence on health. The exposome encompasses all environmental exposures throughout a person’s life and their cumulative impact on well-being. By integrating these diverse factors, the exposome offers a robust framework for understanding how our surroundings shape our health over time. Exposome can be classified into three different domains: the general external exposome, which includes factors such as climate and urbanization, measurable at the population level; the specific external exposome, which contains information about individual exposures such as lifestyles, measurable, for example, through questionnaires; the internal exposome, which encompasses the multiple biological responses to external factors, such as hormonal and inflammatory processes, detected through molecular and "omics" analyses. If we consider the general external exposome domain, approximately half of the avoidable deaths in Europe from non-communicable diseases (~ 700,000) are due to air pollution, precisely the particulate matter with a diameter of 10 microns (PM10) or smaller (PM2·5) [8].
Air pollution is a significant yet often overlooked factor in the intricate web of diabetes pathogenesis. Exposure to fine particulate matter disrupts glucose metabolism by triggering endothelial dysfunction, promoting inflammation within adipose tissue, and contributing to insulin resistance. These harmful effects collectively pave the way for the onset of diabetes, highlighting the profound impact of our environment on metabolic health. The risk of developing Diabetes increases by 10–27% for each increment of exposure to 10 μg/m3 of PM2·5, while the risk of mortality increases by about 1% [9]. Urban design can also profoundly affect human health by inducing acoustic and light pollution. Increased exposure to residential noise and artificial light and an increased risk of type 2 diabetes [10, 11]. By disrupting sleep quality and duration: circadian rhythm alterations lead to altered insulin secretion and worsening insulin sensitivity. High temperatures are also linked to altered glucose metabolism: a 1 °C rise in outdoor temperature may be associated with over 100,000 new diabetes cases per year. Therefore, there is convincing evidence of how Urbanization plays a fundamental role in the spread of Diabetes, influencing the built and natural environment [12].
Access to healthy food is another environmental factor closely tied to the risk of Diabetes. Food insecurity and limited availability of nutritious options significantly increase the likelihood of developing this chronic condition. Ensuring equitable access to healthy foods is essential in combating the rising tide of Diabetes and promoting overall well-being [13]. The availability of healthy dietary options can reduce the risk of obesity and Diabetes, while lack of access to such foods can increase this risk [14]. Socio-economic factors are powerful determinants in the risk of developing Diabetes. Low income, occupational status, and education levels can limit access to essential resources and opportunities, profoundly impacting lifestyle choices and overall health. Addressing these disparities is crucial in reducing the prevalence of Diabetes and fostering healthier communities [15].
Stressful events, both physical and psychological, can enhance the risk not only of Diabetes but also of cardiovascular disease [16]. Experiencing hardships during childhood and adolescence—such as poverty and loneliness—significantly heightens the risk of developing Diabetes in adulthood. This underscores the importance of starting health promotion as early as pregnancy, with targeted interventions to reduce stress and improve socio-economic conditions.
These insights reinforce the understanding that Diabetes is a multifaceted disease shaped by environmental, socioeconomic, and psychological factors. Addressing these diverse influences from the earliest stages of life is crucial to effectively preventing and managing diabetes.
Interactions between health, climate change, and the environment
As emphasized at the beginning of this document, recognizing the complex interactions between the environment, climate change, and health is crucial for developing a comprehensive and integrated approach. Such an approach enables practical actions that can effectively address these interconnected issues. Although the level of attention to this relationship varies among countries, significant progress has been made on an international scale. Organizations like the World Health Organization (WHO) and the European Union (EU) have been at the forefront of these efforts. With its long-standing commitment to environmental issues, the EU has notably advanced this cause. A prime example of this dedication is the establishment of the EU Climate and Health Observatory. This initiative represents a joint effort to produce vital information and data, supporting policies safeguarding the environment and public health. In Italy, the Minister of Health has emphasized the commitment to promote a One Health vision integrated into the National Recovery and Resilience Plan. This project, called "Health, Environment, Biodiversity, and Climate," aims to improve the National Health Service’s prevention and response to diseases related to environmental and climatic risks, with an investment of 500 million euros. As Italy takes the helm of the G7, there is a solid commitment to ensuring that health issues remain a top priority within the broader strategy to combat climate change. By prioritizing health in its climate strategy, Italy aspires to lead a global response that tackles environmental challenges and protects public health. This integrated approach—aligning and coordinating health and environmental policies—has the potential to unlock significant co-benefits. By addressing climate change and health together, resources can be optimized, ecological quality enhanced, and the well-being of populations improved worldwide.
The proposed shift from a "Health in All Policies" strategy to a more holistic "Health for All Policies" approach is designed to address every element of health organically. This multidisciplinary framework acts on the underlying determinants of health, effectively tackling the root causes and impacts of physical and mental illnesses.
The "Health for All Policies" approach creates opportunities for significant co-benefits by promoting strategies like sustainable mobility and investment in renewable energy. Sustainable management of natural resources enhances the resilience of food and agricultural systems, bolstering food security—an essential pillar of human health. Engaging directly with sectors responsible for environmental impacts is crucial to achieving lasting sustainability, ensuring they are part of the solution.
The healthcare sector significantly contributes to air pollution, accounting for 4.4% of global greenhouse gas emissions [17]. Hospitals are among the most significant contributors to emissions, operating around the clock to power heating, ventilation, lighting, and essential equipment. These facilities consume three times more energy than residential and civil sectors under similar climatic conditions. In the United Kingdom, the National Health Service (NHS) alone is responsible for approximately 4% of the nation’s total emissions, mainly driven by medicines, medical devices, and infrastructure [18].
The 2030 Agenda offers a valuable framework to assess the environmental impact of healthcare systems and set targeted sustainability goals. For instance, 3.5% of UK road traffic—equating to 9.5 billion miles annually—is linked to the movement of NHS patients, visitors, staff, suppliers, and vehicles. This accounts for around 14% of the NHS’s total emissions, underscoring the urgent need for greener solutions in healthcare [18]. Hospitals are also significant water consumers, which has potential implications for Goal 6 of the 2030 Agenda related to clean water and hygiene [19]. Waste management in healthcare systems is challenging, with 30% of global healthcare facilities not equipped to handle their waste correctly.
Healthcare systems that actively combat pollution and socio-environmental impacts can drive significant economic sustainability. A brilliant example is the English NHS, which reduced its environmental impact by 62% between 1990 and 2020. This achievement contributed to a healthier planet and saved millions of pounds through energy efficiency and recycling initiatives, proving that green practices are both environmentally and economically beneficial. In Italy, the National Recovery and Resilience Plan allocates funds for sustainable hospital construction, but many hospital buildings still need to be updated and more efficient [18].
In conclusion, implementing policies to enhance energy efficiency, promote recycling, and improve waste management can increase economic and environmental sustainability in the healthcare sector.
Innovation and sustainability in diabetes
The Green Diabetes Summit of 2021 marked a significant milestone in addressing sustainability and innovation challenges in diabetes healthcare management. Organized by the Diabetes Technology Society, this groundbreaking event united stakeholders from diverse sectors to explore environmentally sustainable practices in diabetes care. By adopting the five Rs—reduce, reuse, recycle, redesign, and re-educate—to the field of diabetology, the summit set the stage for a greener, more responsible approach to managing diabetes.
Diabetes poses a significant challenge not only to public health but also to the environment, driven by its global prevalence and rising incidence. The management of this chronic condition generates a substantial amount of healthcare waste, particularly from single-use devices. Unlike other medical waste, diabetes-related waste is largely composed of packaging materials, with plastics being a major contributor. This dual impact underscores the need for innovative solutions addressing health outcomes and environmental sustainability [20] (Fig. 1). Challenges arise from the complex materials, hindering recycling and reuse efforts. Cultivating environmental awareness among healthcare professionals and patients and implementing regulatory reforms to encourage product redesign for reduced environmental impact is essential.
Some pharmaceutical companies have implemented recycling and reuse programs, repurposing single-use pen needles into various products, and developing collection programs for used devices. Efforts to redesign products have resulted in the creation of smaller glucose test strips, significantly reducing waste [21]. While some healthcare providers have started incorporating environmental objectives into their regulations, environmental impacts still need to be considered in economic assessments of healthcare technologies. Integrating environmental outcomes into health technology assessment models presents challenges but is essential for recognizing broader impacts on society and the environment. Tackling diabetes care’s environmental sustainability demands a united effort, combining collaborative initiatives, regulatory reforms, and innovative solutions. We can enhance patient outcomes by prioritizing environmental considerations, clinical efficacy, and economic sustainability while safeguarding our planet. Together, these efforts will lead to a healthier future for individuals and the environment.
Conclusions
Challenges related to health and the environment have been central topics in scientific discourse and political agendas for some time. There is ample evidence of their interconnections. However, these two realms often proceed on separate tracks despite increased political and regulatory connections at national and international levels. For example, during discussions at the United Nations General Assembly, only one out of ten countries mentioned health and the environment together in recent years. Our bustling environment has a hidden cost—environmental factors silently contribute to a global health crisis. These factors, responsible for a staggering 24% of the global disease burden and over 13 million deaths annually, are not merely bystanders in our well-being but active players in shaping our health.
While we often focus on the well-known culprits like air pollution, the spotlight must shift to lesser-known but equally powerful threats. Noise and light pollution, often overlooked, contribute to stress, disrupted sleep, and a cascade of health problems. These environmental factors are intertwined with our choices and the social, economic, and environmental conditions we navigate.
Diabetes, a stark example of this intricate relationship, presents a major challenge for our healthcare systems. It thrives in environments shaped by social inequalities, inadequate housing, limited mobility, and unhealthy work conditions. By prioritizing policies that promote sustainable housing, accessible mobility, social inclusion, and healthy workplaces, we can forge a path toward healthier urban landscapes. This shift will not only reduce the burden of diabetes but empower individuals and communities to thrive in a healthier environment. It’s time to recognize that our health is intricately woven with the environment we inhabit.
The fight against diabetes extends beyond medication and doctor’s visits. It reaches into the very fabric of our planet, demanding a mindful approach to sustainability. We must rethink the entire patient pathway, from producing medications and devices to their distribution and disposal. Implementing shared environmental and health policies and integrating environmental impact into HTA evaluations is crucial. Models like the HTA Core Model, which indirectly considers ecological impacts, provide a starting point. However, we must move beyond indirect measures and explicitly incorporate the environmental dimension into our decision-making processes. This requires a collaborative effort between healthcare providers, policymakers, and the medical technology industry.
References
Watts N, Amann M, Arnell N et al (2019) The 2019 report of The Lancet Countdown on health and climate change: ensuring that the health of a child born today is not defined by a changing climate. Lancet 394(10211):1836–1878
World Health Organization. Determinants of health. 2017 Feb 3; [cited 2024 Apr 7]. Available from: https://www.who.int/news-room/questions-and-answers/item/determinants-of-health
Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019). Seattle, United States: Institute for Health Metrics and Evaluation (IHME), 2020; [cited 2024 Apr 6]. Available from: https://ghdx.healthdata.org/gbd-2019
Cho NH, Shaw JE, Karuranga S et al (2018) IDF diabetes atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract 138:271–281
Osservatorio ARNO Diabete. Il Profilo assistenziale della popolazione con diabete. Maggioli S.p.A. 2019; [cited 2024 Apr 6]. Available from: https://www.siditalia.it/clinica/linee-guida-societari/send/80-linee-guida-documenti-societari/5025-rapporto-arno-diabete-2019
Heald AH, Stedman M, Davies M et al (2020) Estimating life years lost to diabetes: outcomes from analysis of national diabetes audit and office of national statistics data. Cardiovasc Endocrinol Metab 9(4):183–185
Wild CP (2012) The exposome: from concept to utility. Int J Epidemiol 41(1):24–32
World Health Organization. Clean air + green planet = good health for all [Internet]. 2023 [cited 2024 Apr 7]. Available from: https://www.who.int/europe/news/item/05-07-2023-clean-air---green-planet---good-health-for-all
Eze IC, Hemkens LG, Bucher HC et al (2015) Association between ambient air pollution and diabetes mellitus in Europe and North America: systematic review and meta-analysis. Environ Health Perspect 123(5):381–389
den Braver NR, Lakerveld J, Rutters F, Schoonmade LJ, Brug J, Beulens JWJ (2018) Built environmental characteristics and diabetes: a systematic review and meta-analysis. BMC Med 16(1):12
Obayashi K, Saeki K, Iwamoto J, Ikada Y, Kurumatani N (2014) Independent associations of exposure to evening light and nocturnal urinary melatonin excretion with diabetes in the elderly. Chronobiol Int 31(3):394–400
Gassasse Z, Smith D, Finer S, Gallo V (2017) Association between urbanisation and type 2 diabetes: an ecological study. BMJ Glob Health 2(4):e000473
Te Vazquez J, Feng SN, Orr CJ, Berkowitz SA (2021) Food insecurity and cardiometabolic conditions: a review of recent research. Curr Nutr Rep 10(4):243–254
Beulens JWJ, Pinho MGM, Abreu TC et al (2022) Environmental risk factors of type 2 diabetes-an exposome approach. Diabetologia 65(2):263–274
Hill-Briggs F, Fitzpatrick SL (2023) Overview of social determinants of health in the development of diabetes. Diabetes Care 46(9):1590–1598
Falvey JR, Hajduk AM, Keys CR, Chaudhry SI (2022) Association of financial strain with mortality among older US adults recovering from an acute myocardial infarction. JAMA Intern Med 182(4):445–448
Health Care Without Harm and Arup. Health Care’s Climate Footprint Report. How the Health Sector Contributes to the Global Climate Crisis and Opportunities for Action. 2019; [cited 2024 Apr 7]. Available from: https://noharm-global.org/sites/default/files/documents-files/5961/HealthCaresClimateFootprint_092319.pdf
NHS England (2020). Delivering a Net Zero National Health Service. 2020; [cited 2024 Apr 7]. Available from: https://www.england.nhs.uk/greenernhs/wp-content/uploads/sites/51/2020/10/delivering-a-net-zero-national-health-service.pdf
D’Alessandro D, Tedesco P, Rebecchi A, Capolongo S (2016) Water use and water saving in Italian hospitals. A preliminary investigation. Ann Ist Super Sanita 52(1):56–62
Heinemann L, Krisiunas E (2019) Diabetes technology and waste: a complex problem piling up! J Diabetes Sci Technol 13(5):815–816
The European House - Ambrosetti. Position paper; Innovazione, salute e sostenibilità. 2023; [cited 2024 Apr 6]. Available from: https://healthcare.ambrosetti.eu/it/incontri/view/12954#lg=1&slide=0
Acknowledgements
The authors thank Francesco Saverio Mennini, PhD (Ministry of Health; Faculty of Economics, Università degli Studi di Roma Tor Vergata, Rome, Italy) and Roberta Toffanin (Consultant for the Ministry of Environment and Energy Security, Rome, Italy) for their insights. This research received no formal backing from any commercial or nonprofit entity.
Funding
None.
Author information
Authors and Affiliations
Contributions
Angelo Avogaro had full access to the study’s data and is responsible for its integrity and accuracy. Acquisition, analysis, or interpretation of data: All authors. Drafting of the manuscript: All authors. Critical review of the manuscript for important intellectual content: All authors. Administrative, technical, or material support: Daniela Bianco, Giovanni Brusaporco and Irene Gianotto. Supervision: Angelo Avogaro and Daniela Bianco.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Not available.
Informed consent
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Avogaro, A., Rigato, M., di Brino, E. et al. The socio-environmental determinants of diabetes and their consequences. Acta Diabetol (2024). https://doi.org/10.1007/s00592-024-02373-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00592-024-02373-3