Abstract
Aims
The impact of macrovascular and microvascular complications, the common vascular complications of type 2 diabetes, on long-term mortality has been well evaluated, but the impact of different complications of newly diagnosed type 2 diabetes (diagnosed within the past 2 years) on long-term mortality has not been reported. We aimed to investigate the relationship between all-cause mortality and vascular complications in U.S. adults (aged ≥ 20 years) with newly diagnosed type 2 diabetes.
Methods
We used data from the 1999–2018 National Health and Nutritional Examination Surveys (NHANES). Cox proportional hazard models was used to assess hazard ratios (HR) and 95% confidence intervals for all-cause mortality.
Results
A total of 928 participants were enrolled in this study. At a mean follow-up of 10.8 years, 181 individuals died. In the fully adjusted model, the hazard ratio (HR) (95% confidence interval [CI]) of all-cause mortality for individuals with any single complication compared with those with newly diagnosed type 2 diabetes without complications was 2.24 (1.37, 3.69), and for individuals with two or more complications was 5.34 (3.01, 9.46).Co-existing Chronic kidney disease (CKD) and diabetic retinopathy (DR) at baseline were associated with the highest risk of death (HR 6.07[2.92–12.62]), followed by CKD and cardiovascular disease (CVD) (HR 4.98[2.79–8.89]) and CVD and DR (HR 4.58 [1.98–10.57]).
Conclusion
The presence of single and combined diabetes complications exerts a long-term synergistic adverse impact on overall mortality in newly diagnosed U.S. adults with type 2 diabetes, underscoring the importance of comprehensive complication screening to enhance risk stratification and treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the past 30 years, global disease burden research has identified diabetes (all forms) as the ninth leading cause of shortened life expectancy [1]. Currently, approximately 1 in 11 adults worldwide have diabetes, with 90% having type 2 diabetes. Global health is threatened by diabetes and its complications [2]. Complications of diabetes mainly include microvascular (kidney disease, retinopathy, and neuropathy) and macrovascular (cardiovascular) complications [3]. In previous studies, vascular complications were linked to an increase in deaths among individuals with type 2 diabetes [4]. Compared to individuals without type 2 diabetes, individuals with type 2 diabetes with cardiovascular disease (CVD) have a two to fourfold higher mortality rate [5]. The presence of any level of diabetic retinopathy (DR) increases all-cause mortality by 234% (HR 3.34 [1.96–2.80]) compared to individuals without DR [6]. Likewise, as the severity of Chronic kidney disease (CKD)escalates, the likelihood of mortality rises. Moreover, the collective impact of these two microvascular complications on fatality. Moreover, the researchers also analyze the two kinds of microvascular complications of the combined effect of fatality rate. In comparison to a solitary complication, the existence of both DR and CKD escalates the likelihood of demise by 176% (HR 2.76 [2.05–3.72]) [7]. The investigators of another study found whentype 2 diabetes s accompanied by DR, CKD, and diabetic autonomic neuropathy, at the same time, the risk of death increases by 692% (HR 7.92 [2.93–21.37]) [8]. Hence, it is crucial to screen for complications related to diabetes to diagnose and treat the condition effectively. Research has indicated that regularly screening for vascular complications in individuals with type 2 diabetes, along with closely monitoring and managing these conditions, can somewhat decrease the risk of mortality from any cause among Asian populations [9].
However, in recent years, researchers have predominantly focused on singular microvascular complications when studying the prognosis of diabetic complications, with limited attention given to concurrent investigations of comprehensive prognosis of multiple vascular complications. Moreover, individuals with diabetes often have asymptomatic or mild symptoms at the onset of diabetes, and many guidelines recommend screening for complications at the initial diagnosis [10,11,12]. However, current research on the incidence and prognosis of multiple complications among newly diagnosed diabetic individuals is hampered by small sample sizes and short observation periods. The investigation of the prevalence of complications in newly diagnosed diabetic individuals and the mortality rate of different complications in newly diagnosed diabetic individuals can draw attention from clinical physicians and individuals. Strengthening the screening for complications can effectively delay the progression of the disease in individuals, thus reducing the socioeconomic burden.
This study aims to explore the link between vascular complications, considering both their combined effects and individual occurrences, and the overall risk of mortality for newly diagnosed adult individuals with type 2 diabetes in the United States. This research will provide insights into how various vascular complications might influence survival outcomes in this demographic. To achieve this goal, we analyzed the data from National Health and Nutrition Examination Survey (NHANES) from 1999 to 2018.
Materials & methods
The NHANES study is a research initiative aimed at evaluating the health and nutritional well-being of individuals, both adults and children, residing in the United States [13]. The data gathered from this survey conducting epidemiological and scientific research related to health. It helps in formulating effective public health policies, guiding the development and implementation of health programs and services, and advancing our understanding of various health aspects within the population. The National Center for Health Statistics (NCHS), a division of the Centers for Disease Control and Preventions (CDC), conducts NHANES with the approval of the NCHS Institutional Review Board. Before taking the survey, all participants must give written informed consent.
The research enrolled participants who were 20 years old or above and had type 2 diabetes. The definition of type 2 diabetes is being diagnosed as diabetes by a doctor, taking hypoglycemic drugs, having a fasting blood glucose concentration of ≥ 7.0 mmol/L (126 mg/dL), a 2-hour postprandial blood glucose concentration of ≥ 11.1 mmol/L (200 mg/dL), or a glycated hemoglobin (HbA1c) concentration of ≥ 6.5% (48 mmol/mol) [14]. A diagnosis of newly diagnosed diabetes is defined as one that occurred within the past two years [15]. We included 1262 participants with newly diagnosed type 2 diabetes. We excluded participants who had any of the following conditions: (1) having cancer at baseline (n = 139); (2) being pregnant at baseline (n = 170); (3) being younger than 20 years old (n = 69); (4) being deceased with missing information (n = 2); (5) lacking information on glomerular filtration rate (eGFR); (6) lacking information on albuminemia; (7) lacking information on diabetic retinopathy (DR) (n = 3). Ultimately, 928 participants were included in the analysis. A flowchart of the study participant selection process is shown in Supplementary Fig. 1.
Microvascular complications
By utilizing the Chronic Kidney Disease Epidemiology Collaboration formula to compute eGFR, We defined reduced eGFR as having an eGFR ,60 mL/min/1.73 m2. [16]. Using both the solid-phase fluorescent immunoassay and an enhanced Jaffe kinetic method, we assessed the proportion of albumin to creatinine in a solitary spot urine specimen. We defined albuminuria as an albumin-to-creatinine ratio ≥ 30 mg/g. Chronic kidney disease is defined as reduced eGFR, albuminuria, or both [17]. Diabetic retinopathy was based on self-reported physician-diagnosed history by the participants. Cardiovascular disease is characterized by the presence of congestive heart failure, stroke, or heart attack [15].
Covariates
Data on different demographic factors collected in the database, such as age, sex, race or ethnicity, education level, household income, smoking status, and alcohol consumption, were obtained using standardized interview questionnaires. Four categories were used to classify race and ethnicity: non-Hispanic white, non-Hispanic black, Mexican American or Hispanic, and others. Education level was divided into three categories: less than high school, high school, and college and above. The poverty-income ratio (PIR) was used to classify household income into three groups: less than 1.30, between 1.31 and 3.50, and greater than 3.50. A higher PIR value indicates a more favorable economic status. The eGFR was divided into three groups < 60 ml/min / 1.73 m2, 60–90 ml/min / 1.73 m2 and > 90 ml/min / 1.73 m2 [15]. The smoking status was divided into three categories: never, previous, or present. The classification of alcohol consumption was based on whether individuals were drinking or not. To calculate the body mass index (BMI), the body weight, measured in kilograms, was divided by the square of the height, measured in meters. The BMI was categorized into three groups: <25.0 kg/m2, 25.0–29.9 kg/m2, and ≥ 30.0 kg/m2 .Hypertension was determined by a systolic blood pressure of 140 mmHg or higher, a diastolic blood pressure of 90 mmHg or higher, or a self-reported hypertension history [18]. During the interviews, individuals were questioned about the duration of their diabetes and their utilization of hypoglycemic medications.
Statistical analyses
All statistical analyses were conducted, taking into consideration the complex sampling design of NHANES, which involved multiple stages, stratification, and clustering. To guarantee the inclusion of national estimates, this design incorporated the oversampling of particular subgroups. Incorporating sample weights, strata, and primary sampling units embedded in NHANES data was done to ensure an accurate representation of the population. The mean values (with standard deviation) were used to present the baseline characteristics for continuous variables, while number (with percentages) were used for categorical variables. Furthermore, Cox proportional hazard models were employed to ascertain the adjusted hazard ratios (HRs) and the corresponding 95% confidence intervals.
Models were fully adjusted for age, sex, race/ethnicity, education levels, ratio of family income to poverty smoking status, duration of diabetes, drinking status, HbA1c concentration, BMI, and use of antidiabetic drugs. All models assumed the proportional hazards assumption. We utilized the Mann-Whitney test to examine disparities among groups for continuous variables, while Fisher’s exact test was employed for categorical variables. Empowerstats 2.0 and STATA software version 17 were utilized for statistical analyses, with a significance level of 0.05 set at a two-sided α.
Results
The study population consisted of 928 participants with a mean follow-up time of 10.8 years. The demographic, clinical, and metabolic characteristics of the study participants at baseline are presented in (Table 1). In the study, 47.8% were men, and most participants reported the use of glucose-lowering medications (64.4%). Additionally, the majority of individuals had overweight or obese (BMI ≥ 25 kg/m2, 87.8%), and had high blood pressure (55.6%). At baseline, 505 (54.4%) individuals had no complications, 316 (34.1%) had one complication, and 107 (11.5%) had two or more complications. The prevalence of CKD was 29.8%, DR was 13.0%, and CVD was 15.6%.
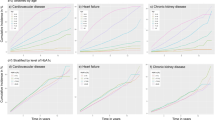
Long-term prognostic value of individual complications
At a mean follow-up time 10.8 years, 181 individuals had died. Fully adjusted hazard ratios for death for each complication, irrespective of other complications, are shown in Table 2.
The presence of CKD increased the risk of death by 195% (HR 2.95 [1.99–4.38]) in the unadjusted model, and by 135% (HR 2.35 [1.54–3.60]) in the fully adjusted model.
There were 460 individuals with eGFR between > 90 ml/min/1.73 m2, among whom 62 died; 359 individuals with eGFR between 60 and 90 ml/min/1.73 m2, among whom 71 died; and 109 individuals with eGFR < 60 ml/min/1.73 m2, among whom 48 died. Compared with individuals with eGFR > 90 ml/min/1.73 m2, those with eGFR between 60 and 90 ml/min/1.73 m2 had a 74% increase in the unadjusted risk of all-cause mortality (HR 1.74 [1.11–2.72]), and those with eGFR < 60 ml/min/1.73 m2 had a 444% increase in the unadjusted risk of all-cause mortality (HR 5.44 [3.29–8.99]). After full adjustment, compared with individuals with eGFR > 90 ml/min/1.73 m2, those with eGFR < 60 ml/min/1.73 m2 had a 105% increase in the risk of all-cause mortality (HR 2.05 [1.12–3.74]), while there was no difference in the risk of mortality among those with eGFR between 60 and 90 ml/min/1.73 m2. There were 204 individuals with albuminuria, among whom 72 died. In the unadjusted model, albuminuria was associated with a 139% increase in the risk of all-cause mortality (HR 2.39 [1.58–3.63]), and in the adjusted model, albuminuria was associated with a 147% increase in the risk of all-cause mortality (HR 2.47 [1.63–3.76]). There were 145 individuals with CVD, among whom 63 died. In the unadjusted model, CVD was associated with a 387% increase in the risk of all-cause mortality (HR 4.87 [3.26–7.27]) compared with individuals without CVD, while in the fully adjusted model, CVD was associated with a 172% increase in the risk of all-cause mortality (HR 2.72 [1.75–4.22]) compared with individuals without CVD. There were 121 individuals with DR, among whom 28 died. Compared with individuals without DR, the unadjusted risk of all-cause mortality was it was not statistically significantly higher in individuals with DR (HR 1.49 [0.89–2.49]). However, in the fully adjusted model, DR was associated with a 99% increase in the risk of all-cause mortality (HR 1.99 [1.17–3.39]).
Long-term prognostic value of different combinations of complications
Fully adjusted hazard ratios for death after various combinations of complications are shown in Table 3.
There were 39 individuals with both CKD and DR, among whom 15 died. Compared with individuals without CKD and DR, the unadjusted risk of all-cause mortality in these individuals was HR 5.32 (2.77–10.23), while the fully adjusted risk of all-cause mortality was HR 6.07 (2.92–12.62). There were 23 individuals with both CVD and DR, among whom 7 died. The unadjusted risk of all-cause mortality in these individuals was increased by 446% (HR 5.46 [2.24–13.31]), while the fully adjusted risk of all-cause mortality was HR 4.58 (1.98–10.57). Finally, there were a total of 71 individuals with both CKD and CVD, among whom 41 died. The unadjusted risk of all-cause mortality in these individuals was HR 9.07 (5.33–15.43), while the fully adjusted risk of all-cause mortality was HR 4.98 (2.79–8.89).
Long-term prognostic value of multiple complications
Compared to individuals without any complications, there were 316 and 107 individuals with one or two or more complications, respectively, with 77 and 53 deaths in the former and latter groups, respectively. The unadjusted risk of all-cause mortality was higher in individuals with any single complication compared to those without any complication (HR 2.62 [1.64–4.19]), and increased by 747% in individuals with two or more complications (HR 8.47 [5.13–13.96]). After full adjustment, the risk of all-cause mortality was HR 2.24 (1.37–3.69) in individuals with any single complication and HR 5.34 (3.01–9.46) in individuals with two or more complications, compared to those without any complication. (Table 4)
To further investigate the connection between various individual complications and the mortality risk in newly diagnosed type 2 diabetes (Table 5). After comprehensive adjustment, compared with individuals without complications who have newly diagnosed type 2 diabetes, the HR (95%CI) for combined DR was 2.14 (0.99 to 4.63), for combined CVD was 3.07 (1.44 to 4.63), and for combined CKD was 2.36 (1.34 to 4.16).
To further examine the association between different combinations of complications and the death risk in newly diagnosed type 2 diabetes (Table 6). After full adjustment, compared with individuals with newly diagnosed type 2 diabetes without complications, the HR (95%CI) for combined DR and CKD was 4.88 (1.73–13.80), for combined DR and CVD was 3.56 (0.50–25.00), and for combined CVD and CKD was 5.11 (2.64–9.89). At the same time, when having DR, CVD, and chronic kidney disease (CKD) concurrently, it was 6.53 (1.75 24.35).
Discussion
Every year, the incidence of newly diagnosed type 2 diabetes has been increasing year on year [19]. The overall relative mortality of individuals with type 2 diabetes is approximately twice that of non-diabetic individuals [20, 21] (including all causes and cardiovascular death), and the loss in life expectancy can be as high as 30% of the conventional life expectancy without diabetes [22]. People with type 2 diabetes may have the disease for up to 12 years before clinical diagnosis, develop diabetes-related complications from the time of diagnosis [23], and in many parts of the world, disability due to diabetes is increasing at a faster rate than mortality from diabetes [19]. The Da Qing Diabetes Prevention Outcome Study shows that early intervention can prevent or at least delay the onset of diabetes complications [24]. However, there are no studies on the risk of related complications and death in individuals with newly diagnosed type 2 diabetes.
Our research shows that in the United States adult newly diagnosed type 2 diabetes a mean follow-up of 10.8 years of follow-up, single complications can shorten life expectancy, and with the increase of number of complications, and also increase the risk for all-cause mortality. Among single complications, fully adjusted data indicated that the risk of death was highest in individuals with CVD. In addition, we found that individuals with concurrent CVD and CKD had the highest risk of death after full adjustment compared to the other two combinations. Previous studies have shown a negative correlation between age at diabetes diagnosis and overall mortality rate as well as the risk of macrovascular and microvascular diseases [25]. Comprehensive screening for single or combined complications in newly diagnosed diabetes individuals has clinical value for better risk stratification and guidance of treatment decisions. As far as we know, our research is the initial examination of the influence of individual or combined complications on the lifespan of recently diagnosed individuals with type 2 diabetes.
Our study focused on the risk of death in individuals with multiple complications at initial diagnosis, and if a individuals had both DR and CKD, their fully adjusted risk of death was 6.07 (2.92–12.62). According to previous studies, the presence of CKD and DR In individuals with type 2 diabetes was most significantly associated with reduced mean overall survival (3.90 years or -21.9%), with a 195% increased risk of all-cause mortality after full adjustment (HR 2.95[1.63–5.32]). In microvascular complications, diabetes-induced endothelial dysfunction can lead to the expression of the Intercellular cell adhesion molecule-1(ICAM-1) adhesion molecule [26]. The presence of ICAM-1 facilitates the attraction and migration of white blood cells, enabling their infiltration into the tissues associated with diabetic complications [27]. According to previous research, the lack of ICAM-1 in individuals with diabetic nephropathy has the potential to halt the progression of renal disease [28]. In diabetic retinopathy, the protective impact of blocking ICAM-1 can be seen in the same way, as it prevents blood-retinal barrier disruption, capillary occlusion, and injury to endothelial cells [29, 30]. Both mechanisms have a certain synergistic effect in the development of these diseases, resulting in poor prognosis in individuals with type 2 diabetes with both DR and CKD compared to those with a single complication.
When a individual has both a macrovascular complication and a microvascular complication, their risk of death is increased. The risk of death from CVD and DR is 4.58 (1.98–10.57), and the risk of death from CKD and CVD is 4.98 (2.79–8.89). Prior studies have suggested that in people with both CVD and CKD who have type 2 diabetes, the fundamental pathological process is linked to compromised inflammation resolution. The presence of this disability leads to increased amounts of pro-inflammatory cytokines like Tumour necrosis factor-α (TNF-α), interleukin- 6(IL-6), and other similar substances. Consequently, this inflammatory milieu further facilitates the development and advancement of both complications, ultimately resulting in a poorer prognosis [31]. The development of type 2 diabetes with CVD and DR involves multiple metabolic and hemodynamic disorders, with the formation and action of advanced glycation end products (AGEs) being the key factors [32, 33]. AGEs formed on the extracellular matrix lead to decreased vascular elasticity and inhibition of nitric oxide (NO), mediating endothelial-dependent vasodilator dysfunction in individuals with type 2 diabetes [34]. The gathering of these items will speed up vascular harm, additionally, hasten the advancement of illness, and eventually result in a noteworthy rise in the rate of mortality.
According to our study, the likelihood of mortality is 5.43 (3.09–9.53) in cases where type 2 diabete is present along with two or more complications. According to prior research, individuals with type 2 diabetes who have two or three microvascular abnormalities face mortality risks of 1.98 (0.75–5.21) and 7.02 (2.44–20.20) correspondingly, after accounting for all factors in the model. Moreover, type 2 diabete individuals experiencing all three complications exhibit the greatest likelihood of death [35]. As diabetes advances, high glucose, high blood pressure, and abnormal blood lipid concentration cause activation of endothelial cells and inflammation through various pathways, including oxidative stress, activation of NF-κB, dysfunction of nitric oxide synthase (NOS), and formation of AGEs [36]. Vascular abnormalities arise as a consequence of persistent high blood sugar concentration, causing heightened oxidative stress and inflammatory reactions. Vascular anomalies arise due to proteins undergoing irreversible non-enzymatic glycation, alterations in cellular redox potential, heightened oxidative stress and inflammation, the emergence of endothelial dysfunction, and a prothrombotic condition [37]. Diabetic individuals experiencing both microvascular and macrovascular complications exhibit elevated concentration of various biomarkers associated with endothelial dysfunction, inflammation, and blood clotting, including Von Willebrand Factor (VWF), IL-6, TNF-α, D-dimer, and Plasminogen Activator Inhibitor 1 (PAI-1). This intricate interaction between inflammation, impaired endothelial function, and a tendency for blood clotting contributes to the hastened deterioration of blood vessels and the advancement of the disease [31]. Therefore, individuals with two or more concurrent complications have a compounded degree of vascular damage and the poorest prognosis. This highlights the importance of screening early for diabetic complications in this population.
This study has some limitations, mainly related to the retrospective design. First and most importantly, because our sample was derived from a U.S. population, we cannot generalize our results to other ethnic groups with different pathological backgrounds and cardiovascular disease profiles, especially East Asians, which warrants further investigation. Second, we relied on self-reported questionnaires for CVD and DR, which largely limited the accuracy of our results. Third, we were unable to assess the time course of complications, which may have affected the findings. Therefore, the potential influence of unexplained factors on temporal correlation and temporal variation between different complications should be evaluated from a prognostic perspective in future studies [35]. Fourth, some potential confounders of diabetes were not fully adjusted for when adjusting variables. For example, a mixed diet. In addition, it should be noted that diabetic peripheral neuropathy is an important complication that was not addressed in this study and could be explored in future studies. We did not analyze the data due to incomplete monitoring in NHANES.
The advantage of this study is that, for the first time, the impact of the number of complications on outcomes in individuals newly diagnosed with type 2 diabete in the United States has been examined. Second, the selected database represents the entire population of the United States and is relatively comprehensive and reproducible.
Conclusions
According to our study, the presence of one or more complications adversely affects overall mortality in individuals with newly diagnosed type 2 diabetes in the US population. Individuals with newly diagnosed type 2 diabetes have a considerable burden of complications, making thorough initial screening necessary to detect all complications associated with an increased risk of death. This approach could greatly benefit from targeted interventions aimed at improving survival and quality of life.
References
Fang M, Selvin E (2021) Thirty-year trends in complications in U.S. adults with newly diagnosed type 2 diabetes. Diabetes Care 44(3):699–706. https://doi.org/10.2337/dc20-2304
Zheng Y, Ley SH, Hu FB (2018) Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol 14(2):88–98. https://doi.org/10.1038/nrendo.2017.151
Harding JL, Pavkov ME, Magliano DJ, Shaw JE, Gregg EW (2019) Global trends in diabetes complications: a review of current evidence. Diabetologia 62(1):3–16. https://doi.org/10.1007/s00125-018-4711-2
Ling W, Huang Y, Huang YM, Fan RR, Sui Y, Zhao HL (2020) Global trend of diabetes mortality attributed to vascular complications, 2000–2016. Cardiovasc Diabetol. 19(1):182. Published 2020 Oct 20. https://doi.org/10.1186/s12933-020-01159-5
Taylor KS, Heneghan CJ, Farmer AJ et al (2013) All-cause and cardiovascular mortality in middle-aged people with type 2 diabetes compared with people without diabetes in a large U.K. primary care database. Diabetes Care 36(8):2366–2371. https://doi.org/10.2337/dc12-1513
Taneja GS, Kumar R, Merwah R, Thakur S (2018) Frequency of Macro Vascular complications in individuals of newly diagnosed type 2 Diabets Mellitus and its correlation with Major Cardiovascular Risk factors; a Hospital based study. J Assoc Physicians India 66(8):26–29
Sabanayagam C, Chee ML, Banu R et al (2019) Association of Diabetic Retinopathy and Diabetic Kidney Disease With All-Cause and Cardiovascular Mortality in a Multiethnic Asian Population. JAMA Netw Open. 2(3):e191540. Published 2019 Mar 1. https://doi.org/10.1001/jamanetworkopen.2019.1540
Sacchetta L, Chiriacò M, Nesti L et al (2022) Synergistic effect of chronic kidney disease, neuropathy, and retinopathy on all-cause mortality in type 1 and type 2 diabetes: a 21-year longitudinal study. Cardiovasc Diabetol 21(1):233. https://doi.org/10.1186/s12933-022-01675-6. Published 2022 Nov 5
Schellhase KG, Koepsell TD, Weiss NS, Wagner EH, Reiber GE (2003) Glucose screening and the risk of complications in type 2 diabetes mellitus. J Clin Epidemiol 56(1):75–80. https://doi.org/10.1016/s0895-4356(02)00533-4
ElSayed NA, Aleppo G, Aroda VR et al (2023) 12. Retinopathy, Neuropathy, and Foot Care: standards of Care in Diabetes-2023. Diabetes Care 46(Suppl 1):S203–S215. https://doi.org/10.2337/dc23-S012
ElSayed NA, Aleppo G, Aroda VR et al (2023) 11. Chronic kidney Disease and Risk Management: standards of Care in Diabetes-2023. Diabetes Care 46(Suppl 1):S191–S202. https://doi.org/10.2337/dc23-S011
ElSayed NA, Aleppo G, Aroda VR et al (2023) 10. Cardiovascular Disease and Risk Management: standards of Care in Diabetes-2023 [published correction appears in Diabetes Care. 2023]. Diabetes Care 46(Suppl 1):S158–S190. https://doi.org/10.2337/dc23-S010
Wong TY, Cheung CM, Larsen M, Sharma S, Simó R (2016) Diabetic retinopathy. Nat Rev Dis Primers 2:16012 Published 2016 Mar 17. https://doi.org/10.1038/nrdp.2016.12
Qiu Z, Chen X, Geng T et al (2022) Associations of serum carotenoids with risk of Cardiovascular Mortality among individuals with type 2 diabetes: results from NHANES. Diabetes Care 45(6):1453–1461. https://doi.org/10.2337/dc21-2371
Niu T, Fang J, Shi X et al (2021) Pathogenesis study based on high-throughput single-cell sequencing analysis reveals Novel Transcriptional Landscape and Heterogeneity of Retinal cells in type 2 Diabetic mice. Diabetes 70(5):1185–1197. https://doi.org/10.2337/db20-0839
King GL, Kunisaki M, Nishio Y, Inoguchi T, Shiba T, Xia P (1996) Biochemical and molecular mechanisms in the development of diabetic vascular complications. Diabetes 45(Suppl 3):S105–S108. https://doi.org/10.2337/diab.45.3.s105
Eckardt KU, Berns JS, Rocco MV, Kasiske BL (2009) Definition and classification of CKD: the debate should be about patient prognosis–a position statement from KDOQI and KDIGO. Am J Kidney Dis 53(6):915–920. https://doi.org/10.1053/j.ajkd.2009.04.001
Pavkov ME, Harding JL, Chou CF, Saaddine JB (2019) Prevalence of Diabetic Retinopathy and Associated Mortality among Diabetic adults with and without chronic kidney disease. Am J Ophthalmol 198:200–208. https://doi.org/10.1016/j.ajo.2018.10.019
GBD 2021 Diabetes Collaborators (2023) Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: a systematic analysis for the global burden of Disease Study 2021 [published correction appears in Lancet. 2023;402(10408):1132. Doi: 10.1016/S0140-6736(23)02044-5]. Lancet 402(10397):203–234. https://doi.org/10.1016/S0140-6736(23)01301-6
Mulnier HE, Seaman HE, Raleigh VS, Soedamah-Muthu SS, Colhoun HM, Lawrenson RA (2006) Mortality in people with type 2 diabetes in the UK. Diabet Med 23(5):516–521. https://doi.org/10.1111/j.1464-5491.2006.01838.x
Gulliford MC, Charlton J (2009) Is relative mortality of type 2 diabetes mellitus decreasing? Am J Epidemiol 169(4):455–461. https://doi.org/10.1093/aje/kwn342
Standl E, Khunti K, Hansen TB, Schnell O (2019) The global epidemics of diabetes in the 21st century: current situation and perspectives. Eur J Prev Cardiol 26(2suppl):7–14. https://doi.org/10.1177/2047487319881021
Harris MI, Klein R, Welborn TA, Knuiman MW (1992) Onset of NIDDM occurs at least 4–7 year before clinical diagnosis. Diabetes Care 15(7):815–819. https://doi.org/10.2337/diacare.15.7.815
Gong Q, Zhang P, Wang J et al (2019) Morbidity and mortality after lifestyle intervention for people with impaired glucose tolerance: 30-year results of the Da Qing diabetes Prevention Outcome Study. Lancet Diabetes Endocrinol 7(6):452–461. https://doi.org/10.1016/S2213-8587(19)30093-2
Nanayakkara N, Curtis AJ, Heritier S et al (2021) Impact of age at type 2 diabetes mellitus diagnosis on mortality and vascular complications: systematic review and meta-analyses. Diabetologia 64(2):275–287. https://doi.org/10.1007/s00125-020-05319-w
Shi Y, Vanhoutte PM (2017) Macro- and microvascular endothelial dysfunction in diabetes. J Diabetes 9(5):434–449. https://doi.org/10.1111/1753-0407.12521
Téllez Gil L, Roselló AM, Collado Torres A, Moreno RL, Antonio Ferrón Orihuela J (2001) Modulation of soluble phases of endothelial/leukocyte adhesion molecule 1, intercellular adhesion molecule 1, and vascular cell adhesion molecule 1 with interleukin-1beta after experimental endotoxic challenge. Crit Care Med 29(4):776–781. https://doi.org/10.1097/00003246-200104000-00018
Chow FY, Nikolic-Paterson DJ, Ozols E, Atkins RC, Tesch GH (2005) Intercellular adhesion molecule-1 deficiency is protective against nephropathy in type 2 diabetic db/db mice. J Am Soc Nephrol 16(6):1711–1722. https://doi.org/10.1681/ASN.2004070612
Hirano Y, Sakurai E, Matsubara A, Ogura Y (2010) Suppression of ICAM-1 in retinal and choroidal endothelial cells by plasmid small-interfering RNAs in vivo. Invest Ophthalmol Vis Sci 51(1):508–515. https://doi.org/10.1167/iovs.09-3457
Miyamoto K, Khosrof S, Bursell SE et al (1999) Prevention of leukostasis and vascular leakage in streptozotocin-induced diabetic retinopathy via intercellular adhesion molecule-1 inhibition. Proc Natl Acad Sci U S A 96(19):10836–10841. https://doi.org/10.1073/pnas.96.19.10836
Domingueti CP, Dusse LM, de Carvalho Md LP, Gomes KB, Fernandes AP (2016) Diabetes mellitus: the linkage between oxidative stress, inflammation, hypercoagulability and vascular complications. J Diabetes Complications 30(4):738–745. https://doi.org/10.1016/j.jdiacomp.2015.12.018
Brownlee M (2001) Biochemistry and molecular cell biology of diabetic complications. Nature 414(6865):813–820. https://doi.org/10.1038/414813a
Yamagishi S, Nakamura K, Imaizumi T (2005) Advanced glycation end products (AGEs) and diabetic vascular complications. Curr Diabetes Rev 1(1):93–106. https://doi.org/10.2174/1573399052952631
Bucala R, Tracey KJ, Cerami A (1991) Advanced glycosylation products quench nitric oxide and mediate defective endothelium-dependent vasodilatation in experimental diabetes. J Clin Invest 87(2):432–438. https://doi.org/10.1172/JCI115014
Garofolo M, Gualdani E, Giannarelli R et al (2019) Microvascular complications burden (nephropathy, retinopathy and peripheral polyneuropathy) affects risk of major vascular events and all-cause mortality in type 1 diabetes: a 10-year follow-up study. Cardiovasc Diabetol 18(1):159 Published 2019 Nov 16. https://doi.org/10.1186/s12933-019-0961-7
Forbes JM, Cooper ME (2013) Mechanisms of diabetic complications. Physiol Rev 93(1):137–188. https://doi.org/10.1152/physrev.00045.2011
Goldberg RB (2009) Cytokine and cytokine-like inflammation markers, endothelial dysfunction, and imbalanced coagulation in development of diabetes and its complications. J Clin Endocrinol Metab 94(9):3171–3182. https://doi.org/10.1210/jc.2008-2534
Acknowledgements
Not applicable.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Approval of the research protocol
The study was approved by the local Human Ethics Committee and conducted in accordance with the principles expressed in the Declaration of Helsinki. All subjects provided written informed consent prior to enrollment. Approval date of Registry and the Registration No. of the study/trial: NHANES 1999–2004, Protocol #98 − 12. NHANES 2005–2006, Protocol #2005-06. NHANES 2007–2008, Continuation of Protocol #2005-06. NHANES 2009–2010, Continuation of Protocol #2005-06. NHANES 2011–2012, Protocol #2011-17. NHANES 2013–2014, Continuation of Protocol #2011-17. NHANES 2015–2016, Continuation of Protocol #2011-17. NHANES 2017–2018, Continuation of Protocol #2011-17 (Effective through October 26, 2017). Protocol #2018-01 (Effective beginning October 26, 2017)
Informed consent
All subjects provided written informed consent prior to enrollment.
Competing interests
The authors declare no conflict of interest.
Additional information
Managed by Salvatore Corrao
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, TY., Wang, XN., Kuang, HY. et al. Association between all-cause mortality and vascular complications in U.S. adults with newly diagnosed type 2 diabetes (NHANES 1999–2018). Acta Diabetol (2024). https://doi.org/10.1007/s00592-024-02342-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00592-024-02342-w