Abstract
Aims
To investigate whether the risk for post-partum cardiovascular diseases (CVD) is driven by gestational diabetes (GDM), by GDM-related risk factors and/or by pre-gestational (Pre-GD) or post-gestational diabetes (Post-GD).
Methods
Women delivering in Tuscany, Italy in years 2010–2012 (n = 74,720), were identified from certificates of care at delivery and further identified as affected with GDM, Pre-GD or Post-GD through regional administrative databases. Women with GDM, Pre-GD or Post-GD were retrospectively evaluated for risk of post-partum hospitalizations for CVD (myocardial infarction or stroke; n = 728) across years 2013–2021, comparing women with different forms of diabetes to those without diabetes. Risk of CVD was assessed as odds ratio (OR 95% CI), after logistic multivariate models, considering all recorded pre-gestational characteristics as covariates.
Results
The adjusted OR (aOR) for post-partum CVD hospitalizations was not significantly related to GDM itself (aOR: 0.85; 0.64–1.12; p = ns), but increased in women with Pre-GD (aOR: 2.02; 1.09–3.71; p = 0.024) and Post-GD, associated or not to prior GDM (aOR; 4.21; 2.45–7.23 and respectively aOR: 3.80; 2.38–6.05; p < 0.0001 for both). In presence of pre-pregnancy maternal obesity (BMI ≥ 30 kg/m2) the aOR of CVD approximatively doubled (aOR: 1.90; 1.51–2.40); p < 0.0001, independently of GDM and of Post-GD. The adjusted risk of CVD was lower among employed women (aOR: 0.83; 0.70–0.99); p = 0.04 and significantly higher in presence of poorer education levels (aOR: 1.32; 1.11–1.57); p < 0.0001.
Conclusion
In this population the risk of post-partum CVD was driven by Pre- and Post-GD, not by GDM alone. Pre-gestational obesity represented a major independent risk factor for post-partum CVD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gestational diabetes (GDM) is significantly associated with increased risk of type 2 diabetes and of cardiovascular diseases (CVD) after pregnancy [1,2,3,4,5]. Open, however, remains the question whether the augmented risk of CVD is driven directly by GDM itself, by GDM related risk factors or by incident post-gestational diabetes (Post-GD). As a matter of fact, the overall risk of Post-GD as well as of CVD after GDM appear to be influenced by several factors such as length of post-partum follow up, maternal history of CVD, pre-gestational obesity, parity, and ethnicity/race of mothers. [1]. A recent meta-analysis and a recent population cohort study based on a large Danish registry found a significant, albeit small, independent increase in risk (by about 10%) exerted by GDM alone, on the incidence of post-partum CVD, after eliminating the possible confounding effect of newly diagnosed Post-GD [4, 5]. The heterogeneity of prior studies, however, leaves open some questions especially about the eventual independent contribution on the incidence of post-partum CVD by pre-gestational risk factors for GDM.
Taking advantage of a regional database containing pregnancies occurred in Tuscany, Italy in years 2010–2012 and followed up over a long enough period (2013 to 2021) the aim of this study was to evaluate whether and to what extent the overall risk for incident CVD after a pregnancy with GDM was influenced by Post-GD and/or by the independent contribution of GDM-related risk factors. In addition, we also analyzed an aspect so far scarcely evaluated namely the possible contribution of pre-gestational diabetes (Pre-GD) on the risk of post-partum cardiovascular diseases.
Methods
Population under study
Live births that occurred in Tuscany, in years 2010–2012, from women present in the Regional Health System registry were identified in the regional database of certificates of care at delivery (CAP: Certificato di Assistenza al Parto (Delivery Assistance Certificates) [6]. If, during this three-year period, there were two pregnancies from the same woman, one of them was randomly identified as index pregnancy. CAP certificates include information about mothers and newborns such as age of mothers at delivery, pre-gestational BMI, parity (parous vs. nulliparous), mothers’ education degree stratified as low/none vs. higher degree or graduation, as well as employment status (employed vs. unemployed). Further information regards women’ countries of origin. whether from Italy/western countries or from high migration pressure countries (HMPC), mainly including Africa, Asia, Central-South America or Eastern Europe [7]. The completion of these certificates by midwives is mandatory for all deliveries taking place everywhere in Tuscany, thus covering almost the total number of pregnancies occurring in Tuscany.
Diagnosis of diabetes
From index pregnancies we identified mothers, classifying them into 5 categories according to their glucose tolerance before, during or after index pregnancy: 1. with GDM, 2. with Post-GD after prior gestational diabetes [Post-GD (prior GDM)], 3. with Post-GD without prior gestational diabetes: Post-GD (no GDM), 4. with Pre-GD or 5. with no diabetes after pregnancy. GDM was currently diagnosed in our region by IADSPG criteria [8], and for the purpose of this study, it was identified by an algorithm including at least one of the following conditions: a) women without previous anti-diabetic therapy who, during the pregnancy, were prescribed insulin—the only glucose-lowering drug recommended by Italian guidelines in case of GDM—and stopped after delivery, b) women who received at least one specialistic visit by a diabetologist during pregnancy or were included into an educational program for patients with diabetes before the delivery, c) those who received an OGTT within six months after delivery. This algorithm has been previously validated in our population, pairing data obtained with this algorithm to those obtained after administering a 75g-OGTT and evaluated by IADSPG criteria [8], giving acceptable parameters for sensitivity (0.91) as well as for specificity (0.81) [9]. Pre-GD was identified from the regional registry of people with diabetes including prescription claims for glucose lowering drugs, diabetes-related consumables, clinical chemistry examinations, prescriptions for specialists’ consultations, legal certifications concerning diabetic status and previous hospitalization records containing a diagnosis of diabetes (ICD-9 code: 250.xx). This regional registry has been demonstrated to cover about the 80% of the regional population with diabetes [10]. Finally, Post-GD has been identified from this same registry, by retrieval of newly registered cases of diabetes across years 2013–2021 and identified as whether Post-GD (prior GDM) or Post-GD (no GDM).
Cardiovascular diseases
Women with at least one hospitalization for CVD after index pregnancy were identified by ICD-9 codes 410.xx, 36.01, 36.02, 36.05, 36.06, 36.1 for myocardial infarction, or by ICD-9 codes 430.xx, 431.xx, 432.xx, 434.xx or 436.xx for acute stroke. In the light of the expected low rate of events, myocardial infarction and/or stroke were incorporated into a unique composite cardiovascular outcome.
Statistics
Descriptive analysis of data used Chi-square method for categorical and ANOVA for continuous variables. The contribution given by each considered maternal characteristic (pre-gestational obesity, parity, ethnicity from HMPC countries, education, occupation) on each considered glucose tolerance stratum, expressed as relative risks, was assessed using Chi-square analysis. The effects of GDM as well as of other types of diabetes were expressed as odds ratios: (OR; 95% Confidence Intervals) for hospitalizations for CVD, across the entire period 2013–2021 by utilizing logistic regression analysis models. In these models post-partum CVD was the dependent variable, and GDM or other types of diabetes, age, parity (nulliparous vs. multiparous), pre-gestational obesity (BMI ≥ 30 Kg/m2), country of origin whether or not from HMPC countries, employment status and education (low-none vs. higher degrees or graduation) were considered as independent variables. We preferred to evaluate the OR of hospitalizations for CVD after stratifying cases by diabetes, utilizing a case-control methodologic approach rather than a time-course analysis, in order to better highlight the role by each form of glucose intolerance associated with pregnancy on the final prevalence of post-partum CVD. In a sensitivity analysis, additionally, we included in the model only the group of women present at the end of the study (December 31st, 2021).
Each certificate record contains a unique regional identifier number which represents the access key to all regional databases and does not allow disclosing the identity of women as well as of any other sensitive information. For this reason, no informed consent or any approval by the Ethics Committee was required according to current regional and national laws.
All statistical analyses were performed using SAS ver. 9.3, SAS Institute Inc., Cary, NC, USA. and of STATA 14th Rel., College Station, TX, USA. A p level < 0.05 was considered as significant.
Results
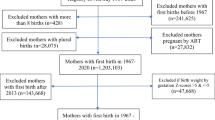
The flowchart concerning the population under study is shown in Fig. 1. The total number of live births across years 2010 to 2012 was 77,304 from 74,720 women with at least one pregnancy. Of them 48,568 (65%) were present in the database of the Regional Health service on December 31st, 2021. Women affected with GDM were 6637 (8.88%), 752 (1.01%) had developed Post-GD, of whom 290 (0.39%) with Post-GD (prior GDM) and 462 (0.62%) with Post-GD (no GDM), 495 (0.66%) had Pre-GD and 66,836 (89.45%) had no diabetes across the entire follow up period 2013–2021.
The main characteristics of women are reported in Table 1. Women with Post-GD (prior GDM) and those with Pre-GD were older than those with other types of diabetes in pregnancy, with women without diabetes representing the youngest group (p < 0.05 after Duncan’s test, in one-way ANOVA). All considered maternal characteristics as well as the prevalence rate of women with post-gestational hospitalizations for CVD (n = 728) were unevenly distributed across different types of diabetes, being post-partum CVD prevalence several times higher among women with Pre- or Post-GD.
The univariate contribution by each maternal characteristic (pre-gestational obesity, parity, country of origin, education, and employment status) on the relative risk for each single type of diabetes is reported in Table 2. Compared to women without diabetes, pre-gestational obesity was related with a marked increase in risk of GDM as well as of Pre- or Post-GD. Nulliparous women had a lower risk for Post-GD, being however associated with a higher risk for Pre-GD, while those coming from HMPC countries had a greater risk for GDM as well as for Post-GD. A poorer education as well as mothers’ unemployment status were related with a greater risk for Post-GD (Table 2).
After a multivariate logistic analysis, adjusted for GDM, age, obesity, parity, country of origin, mothers’ education, employment status and with further pregnancies. the OR for Post-GD was significantly higher among women with GDM, pre-gestational obesity and originating from HMPC countries (Table 3).
Post-gestational cardiovascular events
The risk of incident hospitalizations for CVD after pregnancy (a composite outcome including acute myocardial infarction or stroke) associated with each form of diabetes, was evaluated by univariate and multivariate logistic models, including as covariates GDM, Pre-GD, Post-GD (prior GDM), Post-GD (no GDM), age, obesity, parity, country of origin, education, employment status and having had further pregnancies. After the univariate analysis, comparing women with or without diabetes, GDM had no significant correlation with the risk of post-partum CVD, while women with Post-GD (prior GDM) or Post-GD (no GDM), were up to five times more likely of being affected with post-partum CVD. In addition, women with Pre-GD had a about three-fold higher risk for post-partum CVD (Table 4, a). After a multivariate logistic analysis, GDM was not associated with a significant risk of CVD which was instead about four-fold higher among women with Post-GD and about two-fold higher in those with Pre-GD (Table 4, b). Among covariates pre-gestational obesity was significantly and independently related to the risk of post-partum CVD hospitalizations OR: 1.90; 1.51–2.40; p < 0.0001 (Table 4, b). In addition, there was a 5% increase in the risk for CVD for each BMI unit: OR: 1.05; 1.050 1.03–1.07; p < 0.0001 (data not shown). GDM was associated with an about five-fold increase in risk for Post-GD, and obesity with an about six-fold increase (Table 3). Pre-gestational obesity, however, had no independent additive effect when associated with GDM on the overall risk of Post-GD as evidenced by introducing into the model the interaction term Post-gestational obesity x GDM (p = 0.183). Having further pregnancies after the index ones. (n = 1936) was associated with a significant increase in the risk of Post-GD: OR: 1.54; 1.07–2.22; p = 0.0201. Further covariates associated with a higher risk of post-gestational CVD were low degrees of education and unemployment status. Finally, a sensitivity analysis including only women who were present in the regional database on December 31st, 2021, led to not dissimilar results (data not shown).
Discussion
This study reaffirms that GDM highly increases the risk of diabetes in the post-partum, in agreement with what observed by most prior studies [1,2,3]. The overall risk of post-partum cardiovascular diseases, however, does not seem to be associated with GDM itself, but rather mediated by Pre- or Post-GD. In this regard, however, conflicting results emerge from previously published studies. A former Swedish case-control study based on 2639 women with prior GDM compared to 13,310 controls suggested that GDM had an independent role in predicting a higher risk of post-partum CVD, even after adjusting for incident diabetes [11]. Interestingly, from this study further variables significantly associated with an increased risk of post-partum CVD were pre-gestational obesity, as well as a lower education level, in agreement with what found by the present study. Similarly, in a large cohort study of 1,515,079 Canadian women, those with GDM, regardless of the development of Post-GD, had an increased risk of CVD after pregnancy, being, however, such a risk doubled in presence of post-gestational diabetes [12]. A previous retrospective large cohort study of 1,070,667 women who had delivered infants in hospitals within Quebec, Canada and were followed up for a maximum of 25.2 years, showed that GDM was a significant predictor for CVD after pregnancy, even if no details were given whether associated or not with Post-GD [13]. A French study concerning 1,518,990 deliveries, methodologically like to ours since based on administrative data sources, evidenced that history of GDM was a risk factor for post-partum CVD, especially for coronary vascular diseases, within 7 years after index pregnancy [14]. From a retrospective analysis involving a large cohort of 1,002,486 women who gave birth in Denmark during the period 1978–2016 the overall risk of incident CVD events after GDM was equal to 40% with a Hazard Ratio (HR) of 1.40; 1.35–1.45; p < 0.0001. Interestingly, however, after excluding the effect of Post-GD, this value dropped to 1.07; 1.05–1.10 [5]. That the exclusion of Post-GD largely reduces the independent effect of GDM on the risk of post-partum CVD is moreover, reiterated by a recent metanalysis [4], according to which the risk associated with GDM alone is reduced to less than 10% with HR: 1.09; 1.06–1.13; p < 0.05. According to other studies, however, prior GDM was not an independent risk factor for CVD. According to an observational cohort study of 89,479 US nurses, followed for more than 20 years, prior GDM was associated with a subsequent rise in risk for post-partum CVD (HR: 1.43; 1.12–1.81; p = 0.004), but this excess risk completely disappeared after excluding progressors to diabetes [15]. Comparable results emerged from a recent large Korean population-based retrospective cohort study concerning 1,500,168 parous women followed for more than 10 years [16]. From this study GDM alone was not associated with a significant risk of post-partum CVD (HR: 1.06; 1.00–1.12), becoming the risk significant after progression to diabetes: (HR: 1.74; 1.40–2.15; p < 0.05). In conclusion, from published literature the effect of GDM alone on post-partum risk of CVD, when present is modest, while Post-GD significantly magnifies such a risk. The neutral effect of GDM on post-partum CVD risk, as shown by our study: OR: 0.97; 0.75–1.27, may be due to some peculiar aspects of our study. First, we considered the follow up after only one index pregnancy with GDM, excluding the possible incremental effect on CVD risk by further pregnancies with GDM, a point not taken into consideration by most previously published studies. In our case having further pregnancies at follow up increased by about the 50% the risk of Post-GD, without any effect, however, on the risk of post-partum CVD. In this regard, even whether multiparity is able to progressively increase the insulin resistance eventually leading to GDM remains controversial [17, 18]. There is to remember that, according to a recent Italian study, GDM shows a high recurrence rate (83.2%) [19]. Multiple pregnancies with recurrent GDM are expected to further magnify the risk of diabetes after pregnancy, while open remains the question whether they similarly increase the risk of post-partum CVD, as priorly suggested [20]. In our study, moreover, we observed a higher number of Post-GD in women without prior GDM (n = 462) compared to those with GDM (n = 290). According to the Korean study [16], type 2 diabetes after pregnancy either with or without prior GDM had a similar increasing effect on post-partum CVD risk. Contrarily, Ratnakaran et al. [12] found that Post-GD (prior GDM), compared to Post-GD (no GDM) had a greater impact on post-partum CVD risk, suggesting that GDM could anticipate the onset of Post-GD consequently anticipating the risk of post-partum cardiovascular diseases. A further aspect to consider is that the different length of follow up among studies, may expectedly modify the impact of GDM on the risk for post-partum diabetes [21] and, accordingly on the incidence of post-partum CVD. The key finding of our study, however, is that pre-gestational obesity, besides being strongly associated with all types of Post-GD, independently doubles the risk of CVD. It has been demonstrated that obesity increases the incidence of CVD at an earlier age in both genders [22,23,24], and the link between pre-gestational obesity and the risk of early CVD has also been highlighted by a previous retrospective epidemiological study from the Swedish Medical Birth Registry [25]. In addition, according to the study about the Danish national patient registry maternal obesity was associated with an even higher risk of CVD than the only history of prior GDM: HR: 1.49; 95% CI 1.44–1.54 versus 1.43; 95% CI:1.38–1.49 [5].
Limitations and strengths of the study
This study has several limitations. First, data is retrieved by administrative datasets and are therefore lacking in many important details such as for instance the glucometabolic status in women with GDM or diabetes, impossible, moreover, to be identified as type 1 or type 2. Further, some clinical characteristics of women during the pregnancy as well as at follow up are not recorded or considered in the analysis. In addition, due to the low number of CVD cases it was necessary to build a unique group of events including both myocardial infarctions and strokes. Moreover, these findings, originating in a peculiar geographic condition cannot automatically be extended to other populations. The population-based design with a large regional cohort of women was the major strength of this study.
Conclusions
After reaffirming the significant link between GDM and Post-GD, this observational retrospective study suggests that the risk of post-partum CVD (acute myocardial infarction or stroke) was not related to previous GDM diagnosis, but rather mediated by Pre- or Post-GD. Furthermore, pre-gestational obesity was highly associated with a significant increase in the risk of post-partum CVD, independently of diabetes. The present study, therefore, highlights that pre-gestational obesity represents an important direct and independent risk factor not only for GDM or Post-GD but also for post-partum cardiovascular diseases, further reinforcing the recommendation for early prevention initiatives against obesity in young women.
Data availability
On motivated request, the access to data can be obtained by the Epidemiology Unit, Regional Health Agency of Tuscany, Florence, Italy.
References
Vounzoulaki E, Khunti K, Abner SC et al (2020) Progression to type 2 diabetes in women with a known history of gestational diabetes: systematic review and meta-analysis. BMJ 369:1361. https://doi.org/10.1136/bmj.m1361
Juan J, Sun Y, Wei Y et al (2022) Progression to type 2 diabetes mellitus after gestational diabetes mellitus diagnosed by IADPSG criteria: systematic review and meta-analysis. Front Endocrinol (Lausanne) 13:1012244. https://doi.org/10.3389/fendo.2022.1012244
Retnakaran R (2009) Glucose tolerance status in pregnancy: a window to the future risk of diabetes and cardiovascular disease in young women. Curr Diabetes Rev 5(4):239–244. https://doi.org/10.2174/157339909789804378
Xie W, Wang Y, Xiao S et al (2022) Association of gestational diabetes mellitus with overall and type specific cardiovascular and cerebrovascular diseases: systematic review and meta-analysis. BMJ 378:e070244. https://doi.org/10.1136/bmj-2022-070244
Yu Y, Soohoo M, Sørensen HT, Li J, Arah OA (2022) Gestational diabetes mellitus and the risks of overall and type-specific cardiovascular diseases: a population- and sibling-matched cohort study. Diabetes Care 45(1):151–159. https://doi.org/10.2337/dc21-1018
https://www.salute.gov.it/imgs/C_17_pubblicazioni_2585_allegato.pdf (last accessed January 10, 2024)
Buja A, Gini R, Visca M, Damiani G, Federico B, Francesconi P et al (2013) Valore Project Prevalence of chronic diseases by immigrant status and disparities in chronic disease management in immigrants: a population-based cohort study Valore Project. BMC Public Health 13:504. https://doi.org/10.1186/1471-2458-13-504
International Association of Diabetes and Pregnancy Study Groups Consensus Panel, Metzger BE, Gabbe SG, Persson B, Buchanan TA, Catalano PA et al (2010) International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care 33(3):676–682. https://doi.org/10.2337/dc09-1848
Di Cianni G, Gualdani E, Berni C et al (2017) Screening for gestational diabetes in Tuscany, Italy. A population study. Diabetes Res Clin Pract 132:149–156. https://doi.org/10.1016/j.diabres.2017.08.003
Gini R, Francesconi P, Mazzaglia G et al (2013) Chronic disease prevalence from Italian administrative databases in the VALORE project: a validation through comparison of population estimates with general practice databases and national survey. BMC Public Health 13:15. https://doi.org/10.1186/1471-2458-13-15
Fadl H, Magnuson A, Östlund I, Montgomery S, Hanson U, Schwarcz E (2014) Gestational diabetes mellitus and later cardiovascular disease: a Swedish population based case-control study. BJOG 121(12):1530–1536. https://doi.org/10.1111/1471-0528.12754
Retnakaran R, Shah BR (2017) Role of type 2 diabetes in determining retinal, renal, and cardiovascular outcomes in women with previous gestational diabetes mellitus. Diabetes Care 40:101–108. https://doi.org/10.2337/dc16-1400
McKenzie-Sampson S, Paradis G, Healy-Profitós J, St-Pierre F, Auger N (2018) Gestational diabetes and risk of cardiovascular disease up to 25 years after pregnancy: a retrospective cohort study. Acta Diabetol 55:315–322. https://doi.org/10.1007/s00592-017-1099-2
Goueslard K, Cottenet J, Mariet AS et al (2016) Early cardiovascular events in women with a history of gestational diabetes mellitus. Cardiovasc Diabetol 15:15. https://doi.org/10.1186/s12933-016-0338-0
Tobias DK, Stuart JJ, Li S et al (2017) Association of history of gestational diabetes with long-term cardiovascular disease risk in a large prospective cohort of US women. JAMA Intern Med 177(12):1735–1742. https://doi.org/10.1001/jamainternmed.2017.2790
Sun J, Kim GR, Lee SJ, Kim HC (2021) Gestational diabetes mellitus and the role of intercurrent type 2 diabetes on long-term risk of cardiovascular events. Sci Rep 11(1):21140. https://doi.org/10.1038/s41598-021-99993-4
Motevalizadeh E, Díaz-López A, Martín F, Basora J, Arija V (2023) Association of parity with insulin resistance early in pregnant women ECLIPSES study. J Clin Endocrinol Metab. https://doi.org/10.1210/clinem/dgad594
Seghieri G, De Bellis A, Anichini R, Alviggi L, Franconi F, Breschi MC (2005) Does parity increase insulin resistance during pregnancy? Diabet Med 22(11):1574–1580. https://doi.org/10.1111/j.1464-5491.2005.01693.x
Giuliani C, Sciacca L, Biase ND et al (2022) Gestational diabetes mellitus pregnancy by pregnancy: early, late and nonrecurrent GDM. Diabetes Res Clin Pract 188:109911. https://doi.org/10.1016/j.diabres.2022.109911
Parikh NI, Cnattingius S, Dickman PW et al (2010) Parity and risk of later-life maternal cardiovascular disease. Am Heart J 159(2):215-221.e6. https://doi.org/10.1016/j.ahj.2009.11.017
Dennison RA, Chen ES, Green ME et al (2021) The absolute and relative risk of type 2 diabetes after gestational diabetes: a systematic review and meta-analysis of 129 studies. Diabetes Res Clin Pract 171:108625. https://doi.org/10.1016/j.diabres.2020.108625
Khan SS, Ning H, Wilkins JT et al (2018) Association of body mass index with lifetime risk of cardiovascular disease and compression of morbidity. JAMA Cardiol 3:280–287. https://doi.org/10.1001/jamacardio.2018.0022
Choi S, Kim K, Kim SM et al (2018) Association of obesity or weight change with coronary heart disease among young adults in South Korea. JAMA Intern Med 178:1060–1068. https://doi.org/10.1001/jamainternmed.2018.2310
van Dis I, Kromhout D, Geleijnse JM, Boer JM, Verschuren WM (2009) Body mass index and waist circumference predict both 10-year nonfatal and fatal cardiovascular disease risk: study conducted in 20,000 Dutch men and women aged 20–65 years. Eur J Cardiovasc Prev Rehabil 16(6):729–734. https://doi.org/10.1097/HJR.0b013e328331dfc0
Dikaiou P, Björck L, Adiels M et al (2021) Obesity, overweight and risk for cardiovascular disease and mortality in young women. Eur J Prev Cardiol 28(12):1351–1359. https://doi.org/10.1177/2047487320908983
Acknowledgements
None
Funding
None.
Author information
Authors and Affiliations
Contributions
GS wrote the final draft of manuscript with input from all co-authors. EG and GS checked the accuracy of data and led the statistical analysis. FF, IC, PF, GS and GDC participated in the conception and design of the study. GS, PF and GDC participated in the interpretation of data. All Authors approved the definitive version. GS had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Guarantor
Giuseppe Seghieri.
Guarantor’s statement
As the guarantor of this work, Giuseppe Seghieri had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Ethical Standard Statement
All Authors declare that this study has been conducted in accordance with the Declaration of Helsinki and in accordance with the ethical standards of the responsable committe on human experimentation (institutional and national). Due to the study design and the anonymous by design database, based on Italian regulations, the signature of informed consent was not required.
Informed consent
Each patient was assigned a unique identifier that was the same for all administrative databases. This identifier does not allow the disclosure of the patient’s identity and other sensitive data. Therefore, no informed consent was required from all patients for being included in the study.
Additional information
Managed by Massimo Federici .
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Seghieri, G., Gualdani, E., Campesi, I. et al. Risk of cardiovascular events after gestational diabetes: a retrospective population study. Acta Diabetol 61, 1143–1150 (2024). https://doi.org/10.1007/s00592-024-02297-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-024-02297-y