Abstract
Aims
We aimed to explore the relationship between gestational weight gain (GWG) after Institute of Medicine (IOM) and pregnancy outcomes in women with type 1 and type 2 diabetes.
Methods
Retrospective cohort study at a tertiary medical center (1981–2011). Outcome variables: 2 maternal and 14 fetal. Main exposure variable: GWG according to IOM. We calculated crude and adjusted ORs as well as population attributable (PAF) and preventable fractions (PPF) for significant positive and negative associations, respectively.
Results
We evaluated 633 pregnant women with type 1 or type 2 diabetes. GWG was insufficient (iGWG) in 16.7% and excessive (eGWG) in 50.7%. In the adjusted analysis, GWG according to IOM was significantly associated with maternal outcomes (pregnancy-induced hypertension and cesarean delivery) and four fetal outcomes (large-for-gestational age, macrosomia, small-for-gestational age and neonatal respiratory distress). The association with large-for-gestational age newborns was negative for iGWG (0.48, CI 95% 0.25–0.94) and positive for eGWG (1.76, CI 95% 1.18–2.63). In addition, iGWG was associated with a higher risk of small-for-gestational age newborns and respiratory distress and eGWG with a higher risk of pregnancy-induced hypertension, caesarean delivery and macrosomia. PAF and PPF ranged from the 20.4% PPF of iGWG for large-for-gestational age to 56.5% PAF of eGWG for macrosomia.
Conclusion
In this cohort of women with type 1 or type 2 diabetes, inadequate GWG after IOM was associated with adverse pregnancy outcomes; associations were unfavorable for eGWG and mixed for iGWG. The attributable fractions were not moderate, pointing to the potential impact of modifying inadequate GWG.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pregnant women with diabetes mellitus (DM) have a higher risk of adverse outcomes, both for the mother and the child, in the short and long term, including pregnancy-induced hypertension (PIH), cesarean delivery, congenital malformations, perinatal mortality, preterm birth, large-for-gestational age (LGA) newborn and macrosomia [1,2,3,4,5,6,7]. Gestational weight gain (GWG) [8,9,10] and increased prepregnancy body mass index [11,12,13] are important risk factors of adverse pregnancy outcomes, with a profile of associated outcomes similar to that of DM complicating pregnancy. As GWG is a modifiable variable during pregnancy, in 2009 the Institute of Medicine (IOM) provided recommendations for GWG to optimize pregnancy outcomes [14] and classified it in three categories: insufficient, adequate or excessive. In women with pregestational diabetes, some studies have related GWG to pregnancy outcomes [15,16,17,18], but in some of the studies, the analysis was limited to absolute GWG or not adjusted by other potential predictors [15].
Therefore, the purpose of the current study was to address the associations between GWG according to IOM and pregnancy outcomes in women with type 1 or type 2 DM and calculate the corresponding population attributable (PAF) and preventable fractions (PPF) when appropriate. We hypothesized that eGWG would be associated with worse pregnancy outcomes.
Methods
Participants
We conducted a retrospective analysis of data prospectively collected during usual clinical practice and entered in the database of the Endocrinology and Pregnancy Clinic at Hospital de la Santa Creu i Sant Pau (Barcelona). The study was approved by the Ethics Committee of the Institut d’Investigació Biomèdica Sant Pau (IIB Sant Pau) (reference number IIBSP-IPE-2020-44) and has been performed in accordance with the Declaration of Helsinki as revised in 2008. The Ethics Committee waived the requirement for informed consent. The analysis was limited to women with pregestational diabetes attended between January 1985 and December 2011. Sample size calculation was not undertaken. Women with pregestational diabetes are provided with structured therapeutic education during pregnancy, and before it when prepregnancy care is sought. The advice includes a healthy normocaloric diet, physical activity according to guidelines, self-monitoring of glucose and treatment adjustment. Healthy diet and physical activity are stressed as relevant in themselves and in the impact of their timing on the glucose profile.
Study design
We addressed 2 maternal and 14 neonatal outcomes, defined as follows: PIH (blood pressure ≥ 140/90 mmHg, × 2 times separated ≥ 6 h, starting at a gestational age ≥ 20 weeks or worsening chronic hypertension), cesarean delivery (primary + iterative), fetal scalp blood pH < 7.25 [19], preterm birth (defined as a gestational age at birth less than 37 complete weeks), Apgar 5 min < 7 [20], cord arterial pH < 7.10 [21], significant obstetric trauma, LGA newborn (birth weight > 90% centile for the same gestational age and sex [22], macrosomia (defined as a birth weight ≥ 4000 g), small-for-gestational age (SGA) newborn (birth weight < 10% centile for the same gestational age and sex) [22], neonatal hypoglycemia (Cornblath criteria applied to capillary blood) [23], neonatal jaundice requiring treatment [24], neonatal respiratory distress requiring treatment [25], neonatal hypocalcemia [26], polycythemia [27] and perinatal mortality (intrauterine or until 28 days postpartum). As to perinatal mortality, different limits of fetal viability were considered according to the period (before 1991: ≥ 28 completed weeks; 1991–1994: ≥ 26 completed weeks; 1995–1999: ≥ 24 completed weeks; from 2000 onwards: ≥ 23 weeks). GWG was derived as the last maternal weight before delivery minus prepregnancy weight, linearly adjusted for a gestational age of 40 weeks. As additional potential independent variables for pregnancy outcomes we considered the following characteristics: maternal ethnicity, age at the beginning of pregnancy, maternal anthropometry (height and prepregnancy body mass index category), type of diabetes, prior pregnancy, multiple pregnancy, prepregnancy care, average HbA1c and insulin dose in each trimester, smoking habit during pregnancy (non-smoker at the beginning of pregnancy, quitter or active smoker during pregnancy), diabetic retinopathy, nephropathy or neuropathy in early pregnancy, fetal sex and concordant sex in multiple pregnancy. The variable of concordant fetal sex was used in the analysis of fetal outcomes; for maternal outcomes, the sex of the fetus with higher risk was used (i.e., female sex for maternal hypertension) [28]. The rate of women using treatment with an insulin pump and short or long-acting analogs is reported for descriptive purposes.
Statistical analysis
All statistical analyses were performed using the SPSS version 26.0 software package. Maternal characteristics were expressed as mean ± standard deviation (SD) or P50 (P25 and P75) for continuous data (the normality of the data was assessed using the Kolmogorov–Smirnov Test). Categorical data were expressed as percentages. Imputations were not used to deal with missing data.
To determine the association of pregnancy outcomes with IOM recommendations on GWG, we first tested outcome differences across the three IOM categories using a chi-square test. A bivariate logistic regression analysis was performed to determine the unadjusted ORs, and the same test was carried out for all potential predictor variables. All variables that displayed an association with perinatal results at p < 0.100, were used for the multivariate logistic regression analysis (forward method) to determine the adjusted ORs (aORs). Statistical significance was established at a two-sided p value < 0.05. The results will indicate if GWG according to IOM was included in the last step of the regression.
For outcomes where IOM displayed a significant association in the adjusted analysis, we calculated the population attributable fraction (PAF) for associations with an aOR > 1 and the population preventable fractions (PPF) for associations with an aOR < 1 [29] even when significance versus aGWG was not reached for individual GWG categories. PAF is defined as the excess number of cases resulting from an exposure divided by the total number of cases in a defined population, and is calculated as follows:
PPF is defined as the number of cases prevented in the population resulting from an exposure to a protective factor and is calculated as follows:
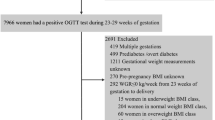
A total of 848 pregnant women with pregestational diabetes mellitus were attended during the study period. The flow-chart of patients included is depicted in Fig. 1. After exclusions due to delivery before 28 weeks, other types of diabetes and missing data for GWG according to IOM, 633 pregnancies were included for analysis (624 singleton pregnancies and 9 multiple pregnancies for a total of 644 babies). Table 1 presents the characteristics of these women; 535 women had type 1 diabetes, 98 type 2 diabetes, average diabetes duration was 11 years (5–17). Weight gain during pregnancy was 14.8 kg (11.5–17.9), and the distribution of corrected GWG according to IOM was 32.5% of women gained within the IOM guidelines, but 16.7% had iGWG and 50.7% had eGWG.
As to outcomes, PIH was present in 16.3%, cesarean delivery in 60.4%, preterm birth 21.7% and LGA 35.4%. Additional outcomes and their distribution according to IOM 2009 are presented in Table 2. Significant associations were observed between IOM and the two maternal outcomes (PIH, cesarean delivery) and six of all 14 fetal outcomes (cord arterial pH < 7.1, LGA, macrosomia, SGA, neonatal respiratory distress and perinatal mortality). Most of these associations were attributable to a higher risk in women with eGWG although higher risk was also present in women with iGWG for some of the outcomes (i.e., SGA, respiratory distress and perinatal mortality).The unadjusted and adjusted ORs resulting from the logistic regression are presented in Table 3. In the adjusted analysis, the GWG according to IOM was significantly associated with PIH, cesarean delivery, LGA, macrosomia, SGA and neonatal respiratory distress, essentially concordant with the unadjusted analysis. eGWG was associated with higher risk for PIH (aOR 2.41; 95% CI 1.38, 4.23), cesarean delivery (1.65; 1.11, 2.46) and macrosomia (3.20; 1.65, 6.23), while iGWG was associated with higher risk for SGA (4.06; 1.16, 14.23) and respiratory distress (4.44; 1.83, 10.74). Furthermore, eGWG and iGWG displayed associations of opposite direction with LGA; eGWG was associated with a higher risk (1.76; 1.183, 2.63), while iGWG was associated with a lower risk (0.48; 0.28, 0.94), respectively.
PAF and PPF for outcomes significantly associated with GWG are displayed in Table 4. For the categories with significant association, the range goes from 20.4% PPF of iGWG for LGA to 56.5% PAF of eGWG for macrosomia.
Discussion
In this cohort of pregnant women with type 1 or type 2 diabetes, we have examined the association of GWG according to IOM 2009 with adverse pregnancy outcomes.
In the adjusted analysis, inadequate GWG was associated with 6 of the outcomes analyzed: PIH, cesarean delivery, LGA, macrosomia, SGA and neonatal respiratory distress. Both iGWG and eGWG were linked to a higher risk of adverse pregnancy outcomes (iGWG with SGA and respiratory distress; eGWG with PIH, caesarean delivery, LGA and macrosomia). In addition, eGWG was also associated with a lower risk for LGA. The PAFs and PPFs indicate that the contribution of GWG to perinatal outcomes is moderate.
This study has several strengths. First, we have carried out a comprehensive analysis of inadequate GWG according to IOM 2009 in women with pregestational diabetes and its contribution to adverse pregnancy outcomes that was not limited to variables related to newborn weight. The second strength is its relatively large study population for pregestational diabetes. Some study limitations also deserve consideration. First, the study is a retrospective single-center study, so that generalization to other settings cannot be directly assumed. Second, only information on total GWG was available so that GWG in each trimester could not be addressed. Additional limitations would be that we have addressed PIH but not preeclampsia.
The distribution of GWG according to IOM in women with type 1 and type 2 diabetes indicates a high frequency of inadequate GWG, fundamentally at the expense of eGWG. The fact that the study period spanned could also be viewed as a limitation since treatment changes took place during this period. However, the impact of these changes should mainly be in glycemic control or weight gain itself and would not influence the current analysis.
As to the associations observed between inadequate GWG and adverse pregnancy outcomes, some differences were noticed between the bivariate analysis using chi-square test, the bivariate analysis using logistic regression and the multivariate logistic regression analysis. All observed associations are in line with information in the literature for the general obstetric population and when the information was available, for women with diabetes.
Thus, two outcome variables, arterial pH < 7.1 and perinatal mortality displayed an association with GWG in the analysis using chi-square test (at the expense of eGWG for arterial pH < 7.1 and of iGWG for perinatal mortality) but did not reach significance in the logistic regression analysis. For arterial pH < 7.1, the observation in the current study is in line with a higher risk of low cord pH in women with eGWG in the general obstetric population [30] and with a similar trend in non-adjusted analysis in women with gestational diabetes (GDM) [31]. Similarly, for perinatal mortality, the association at the expense of iGWG is in line with the increased risk described in the general obstetric population [32, 33]. The lack of significance in the adjusted analysis is probably attributable to insufficient statistical power.
As to the association of GWG with preterm birth, it had borderline significance in the chi-square analysis, iGWG displayed a higher risk in unadjusted logistic regression analysis (OR 1.83), and the association turned again to non-significant in the adjusted analysis. The higher risk of preterm birth in women with iGWG is in line with the well-described association in women in the general obstetric population [34] and in women with GDM [31, 35]. Again, the lack of significance in the adjusted analysis can be attributed to insufficient statistical power.
In the adjusted analysis, GWG according to IOM was associated with PIH, with a higher risk in women with eGWG (aOR 2.41). This observation is in agreement with data in the general population, where Fortner et al. reported that women with eGWG were at three-fold higher risk of hypertension and four-fold risk of preeclampsia compared with women with aGWG [36]. However, in the literature, no significant association of GWG with PIH/preeclampsia has been described in women with pregestational diabetes, probably due to insufficient statistical power of the published series. In turn, the insufficient statistical power in articles studying women with pregestational diabetes is attributable both to the study size and to the fact that the risk or PIH/preeclampsia associated to eGWG seems to be lower in women with diabetes than in the general obstetric population [16, 17, 37, 38].
We have also observed an association of GWG with cesarean delivery at the expense of eGWG (aOR 1.65). The association is consistent with the reports in the general obstetric population [34] and in women with GDM [31, 35]. As to women with pregestational diabetes, an association of eGWG with a higher frequency of cesarean delivery has been documented in a large series of women with type 2 diabetes [18], but the association does not reach significance in other reports in women with type 1 or pregestational diabetes [16, 37,38,39]. The magnitude of the association observed in the current study (aOR 1.65) is similar to the range described in women with diabetes [18, 31, 36].
In this study, inadequate GWG was also associated with LGA, eGWG with a higher likelihood of LGA (aOR 1.76) and iGWG with a lower likelihood of the outcome (aOR 0.48). The results are concordant with the information in the literature. Thus, for eGWG, a higher risk of LGA is present in the general population (OR 1.85) [34], in women with GDM (RR 2.08 [35], aOR 2.00 [31]), in women with type 2 diabetes (aOR of 2.00) [18] and in women with type 1 diabetes where in different reports the risk ranges from aOR 1.64 (non-significant) [16] to OR 4.53 [39]. Similarly, as to the negative association of iGWG with LGA, our results are in agreement with reports in the general population (OR 0.59) [34] and in women with GDM (RR 0.71 [35], aOR 0.57 [31]). In women with pregestational diabetes, published reports provide similar but not significant OR (aOR 0.78 [16], OR 0.79 [15], aOR 0.85 [18]), while other studies do not specifically address iGWG [17, 38].
The higher risk macrosomia (aOR 3.2) in women with eGWG is consistent with observations in the general obstetric population (OR 1.95) [34] and in women with GDM (RR 1.87) [35], type 1 (aOR 2.78) [16] and type 2 diabetes (aOR 2.59) [18].
The higher risk of SGA newborns in women with iGWG (aOR 4.06) is in agreement with data in the general obstetric population (OR 1.53) [34] but the association appears to be stronger. In women with diabetes, the trend is also to a higher risk, but does not reach significance either in women with GDM [31, 35], type 1 [16] or type 2 diabetes [18].
The observation that iGWG is associated with a higher risk of neonatal respiratory distress is in agreement with the data in women with twin gestation (OR 1.63) [40] and with recently reported data in the general population where infants born to not obese mothers with small GWG displayed higher requirements of assisted ventilation and surfactant therapy [41]. However, in women with type 1 and type 2 diabetes, no differences have been described in the prevalence of respiratory distress according to GWG [16, 17, 37, 39], again probably attributable to insufficient statistical power.
Last but not least, the PAFs and PPFs of inadequate GWG categories were of moderate magnitude. While some articles have addressed PAF and PPF in women in the general population [42] or with GDM [8, 43,44,45], we are not aware of similar analyses in women with pregestational diabetes. Current results indicate that despite the needed emphasis on glycemic control during pregnancy, GWG can also have a relevant impact in women with pregestational diabetes and should probably deserve more attention.
In summary, in this cohort of women with type 1 or type 2 diabetes, inadequate GWG according to IOM was associated with adverse pregnancy outcomes, both in the mother and the offspring, also considering other potential predictors. eGWG was associated with unfavorable outcomes (PIH, cesarean delivery, LGA and macrosomia), while iGWG displayed mixed results (favorable for LGA and unfavorable for SGA and neonatal respiratory distress). The attributable fractions were moderate, pointing to the potential impact of modifying inadequate GWG according to IOM.
Data availability
Data available on request due to privacy/ethical restrictions.
References
Alexopoulos AS, Blair R, Peters AL (2019) Management of preexisting diabetes in pregnancy: a review. JAMA J Am Med Assoc 321:1811–1819. https://doi.org/10.1001/jama.2019.4981
Kitzmiller JL, Block JM, Brown FM et al (2008) Managing preexisting diabetes for pregnancy: summary of evidence and consensus recommendations for care. Diabetes Care 31:1060–1079. https://doi.org/10.2337/dc08-9020
Evers IM, De Valk HW, Visser GHA (2004) Risk of complications of pregnancy in women with type 1 diabetes: nationwide prospective study in the Netherlands. Br Med J 328:915–918. https://doi.org/10.1136/bmj.38043.583160.ee
Domanski G, Lange AE, Ittermann T et al (2018) Evaluation of neonatal and maternal morbidity in mothers with gestational diabetes: a population-based study. BMC Pregnancy Childbirth 18:367. https://doi.org/10.1186/s12884-018-2005-9
Balsells M, García-Patterson A, Gich I, Corcoy R (2009) Maternal and fetal outcome in women with type 2 versus type 1 diabetes mellitus: a systematic review and metaanalysis. J Clin Endocrinol Metab 94:4284–4291. https://doi.org/10.1210/jc.2009-1231
Maayan-Metzger A, Lubin D, Kuint J (2009) Hypoglycemia rates in the first days of life among term infants born to diabetic mothers. Neonatology 96:80–85. https://doi.org/10.1159/000203337
Bellamy L, Casas J-P, Hingorani AD, Williams D (2009) Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet 373:1773–1779. https://doi.org/10.1016/S0140-6736(09)60731-5
Black MH, Sacks DA, Xiang AH, Lawrence JM (2013) The relative contribution of prepregnancy overweight and obesity, gestational weight gain, and IADPSG-defined gestational diabetes mellitus to fetal overgrowth. Diabetes Care 36:56–62. https://doi.org/10.2337/dc12-0741
Catalano PM, McIntyre HD, Cruickshank JK et al (2012) The hyperglycemia and adverse pregnancy outcome study: associations of GDM and obesity with pregnancy outcomes. Diabetes Care 35:780–786. https://doi.org/10.2337/dc11-1790
Alberico S, Montico M, Barresi V et al (2014) The role of gestational diabetes, pre-pregnancy body mass index and gestational weight gain on the risk of newborn macrosomia : results from a prospective multicentre study. BMC pregnancy and childbirth 14(23):1–8
Farah N, Maher N, Barry S et al (2009) Maternal morbid obesity and obstetric outcomes. Obes Facts 2:352–354. https://doi.org/10.1159/000261951
Abenhaim HA, Kinch RA, Morin L et al (2007) Effect of prepregnancy body mass index categories on obstetrical and neonatal outcomes. Arch Gynecol Obstet 275:39–43. https://doi.org/10.1007/s00404-006-0219-y
Callaghan WM, Chu SY, Kim YS et al (2007) Maternal obesity and risk of gestational diabetes mellitus. Diabetes Care 30:2070–2076. https://doi.org/10.2337/dc06-2559a.The
Rasmussen KM, Yaktine AL (2009) Institute of Medicine (US) and National Research Council (US) Committee to reexamine IOM pregnancy weight guidelines. Weight gain during pregnancy: reexamining the guidelines. Washington (DC)
Secher AL, Parellada CB, Ringholm L et al (2014) Higher gestational weight gain is associated with increasing offspring birth weight independent of maternal glycemic control in women with type 1 diabetes. Diabetes Care 37:2677–2684. https://doi.org/10.2337/dc14-0896
Kawakita T, Bowers K, McWhorter K et al (2016) Characterizing gestational weight gain according to Institute of Medicine guidelines in women with type 1 diabetes mellitus: association with maternal and perinatal outcome. Am J Perinatol 33:1266–1272. https://doi.org/10.1055/s-0036-1585420
Parellada CB, Ásbjörnsdóttir B, Ringholm L et al (2014) Fetal growth in relation to gestational weight gain in women with type 2 diabetes: an observational study. Diabet Med 31:1681–1689. https://doi.org/10.1111/dme.12558
Yee LM, Cheng YW, Inturrisi M, Caughey AB (2011) Effect of gestational weight gain on perinatal outcomes in women with type 2 diabetes mellitus using the 2009 Institute of Medicine guidelines. Am J Obstet Gynecol 205:257.e1-257.e6. https://doi.org/10.1016/j.ajog.2011.06.028
National Institute for Health and Care Excellence, NICE (2014) Intrapartum care: care of healthy women and their babies during childbirth guidance and guidelines. Available at www.nice.org.uk/guidance/cg190
American College of Obstetricians and Gynecologists, ACOG (2015) Committee opinion no. 644: the Apgar score. Obstet Gynecol 126:e52-5. https://doi.org/10.1097/AOG.0000000000001108
Yeh P, Emary K, Impey L (2012) The relationship between umbilical cord arterial pH and serious adverse neonatal outcome: analysis of 51 519 consecutive validated samples. BJOG 119:824–831. https://doi.org/10.1111/j.1471-0528.2012.03335.x
Santamaria Lozano R, Verdú Martín L, Martín Caballero C, García López G (1998) Tablas españolas de pesos neonatales según edad gestacional. Barcelona Lab Menarini
Cornblath M, Schwartz R (1993) Hypoglycemia in the neonate. J Pediatr Endocrinol 6:113–129
Maisels MJ (1972) Bilirubin; on understanding and influencing its metabolism in the newborn infant. Pediatr Clin N Am 19:447–501
Edwards MO, Kotecha SJ, Kotecha S (2013) Respiratory distress of the term newborn infant. Paediatr Respir Rev 14:29–37. https://doi.org/10.1016/j.prrv.2012.02.002
Loughead JL, Mimouni F, Tsang RC (1988) Serum ionized calcium concentrations in normal neonates. Am J Dis Child 142:516–518. https://doi.org/10.1001/archpedi.1988.02150050054030
Kates EH, Kates JS (2007) Anemia and polycythemia in the newborn. Pediatr Rev 28:33–34. https://doi.org/10.1542/pir.28-1-33
Shiozaki A, Matsuda Y, Satoh S, Saito S (2011) Impact of fetal sex in pregnancy-induced hypertension and preeclampsia in Japan. J Reprod Immunol 89:133–139. https://doi.org/10.1016/j.jri.2010.12.011
Miettinen OS (1974) Proportion of disease caused or prevented by a given exposure, trait or intervention. Am J Epidemiol 99:325–332. https://doi.org/10.1093/oxfordjournals.aje.a121617
Murata T, Kyozuka H, Yamaguchi A et al (2020) Gestational weight gain and foetal acidosis in vaginal and caesarean deliveries: the Japan environment and children’s study. Sci Rep 10:1–11. https://doi.org/10.1038/s41598-020-77429-9
Xie X, Liu J, Pujol I et al (2020) Inadequate weight gain according to the Institute of Medicine 2009 guidelines in women with gestational diabetes: frequency, clinical predictors, and the association with pregnancy outcomes. J Clin Med 9:E3343. https://doi.org/10.3390/jcm9103343
Yao R, Park BY, Foster SE, Caughey AB (2017) The association between gestational weight gain and risk of stillbirth: a population-based cohort study. Ann Epidemiol 27:638-644.e1. https://doi.org/10.1016/j.annepidem.2017.09.006
Vivian Ukah U, Bayrampour H, Sabr Y et al (2019) Association between gestational weight gain and severe adverse birth outcomes in Washington State, US: a population-based retrospective cohort study, 2004–2013. PLoS Med 16:2004–2013. https://doi.org/10.1371/journal.pmed.1003009
Goldstein RF, Abell SK, Ranasinha S et al (2017) Association of gestational weight gain with maternal and infant outcomes: a systematic review and meta-analysis. JAMA J Am Med Assoc 317:2207–2225. https://doi.org/10.1001/jama.2017.3635
Viecceli C, Remonti LR, Hirakata VN et al (2017) Weight gain adequacy and pregnancy outcomes in gestational diabetes: a meta-analysis. Obes Rev 18:567–580. https://doi.org/10.1111/obr.12521
Fortner RT, Pekow P, Solomon CG et al (2009) Prepregnancy body mass index, gestational weight gain, and risk of hypertensive pregnancy among Latina women. Am J Obstet Gynecol 200:167.e1-167.e7. https://doi.org/10.1016/j.ajog.2008.08.021
Scifres CM, Feghali MN, Althouse AD et al (2014) Effect of excess gestational weight gain on pregnancy outcomes in women with type 1 diabetes. Obstet Gynecol 123:1295–1302. https://doi.org/10.1097/AOG.0000000000000271
Egan AM, Dennedy MC, Al-Ramli W et al (2014) ATLANTIC-DIP: excessive gestational weight gain and pregnancy outcomes in women with gestational or pregestational diabetes mellitus. J Clin Endocrinol Metab 99:212–219. https://doi.org/10.1210/jc.2013-2684
Bashir M, Naem E, Taha F et al (2019) Outcomes of type 1 diabetes mellitus in pregnancy; effect of excessive gestational weight gain and hyperglycaemia on fetal growth. Diabetes Metab Syndr Clin Res Rev 13:84–88. https://doi.org/10.1016/j.dsx.2018.08.030
Pécheux O, Garabedian C, Drumez E et al (2019) Maternal and neonatal outcomes according to gestational weight gain in twin pregnancies: are the Institute of Medicine guidelines associated with better outcomes? Eur J Obstet Gynecol Reprod Biol 234:190–194. https://doi.org/10.1016/j.ejogrb.2019.01.010
Wang L, Zhang X, Chen T et al (2021) Association of gestational weight gain with infant morbidity and mortality in the United States. JAMA Netw Open 4:e2141498. https://doi.org/10.1001/jamanetworkopen.2021.41498
Rm BM, Berger H, Melamed N et al (2019) Weight gain during pregnancy: does the antenatal care provider make a difference? A retrospective cohort study. Can Med Assoc Open Access J 7:283–293. https://doi.org/10.9778/cmajo.20180116
Kim SY, Sharma AJ, Sappenfield W et al (2014) Association of maternal body mass index, excessive weight gain, and gestational diabetes mellitus with large-for-gestational-age births. Obstet Gynecol 123:737–744. https://doi.org/10.1097/AOG.0000000000000177
Barquiel B, Herranz L, Hillman N et al (2016) HbA1c and gestational weight gain are factors that influence neonatal outcome in mothers with gestational diabetes. J Women’s Health 25:579–585. https://doi.org/10.1089/jwh.2015.5432
Barquiel B, Herranz L, Grande C et al (2014) Body weight, weight gain and hyperglycaemia are associated with hypertensive disorders of pregnancy in women with gestational diabetes. Diabetes Metab 40:204–210. https://doi.org/10.1016/j.diabet.2013.12.011
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors. The authors do not report any potential conflict of interest.
Author information
Authors and Affiliations
Contributions
XX, JL and RC contributed to formal analysis; XX, JL, AG, AC, MMS, JA, JMA and RC contributed to investigation; XX, JL, AG, AC, MMS, JA, JMA and RC contributed to data curation; writing—original draft preparation by XX, JL and RC; XX, JL, AG, AC, MMS, JA, JMA and RC contributed to writing—review and editing; RC contributed to supervision. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest.
Ethical approval
The study protocol was approved by the Ethics Committee of the Institut d’Investigació Biomèdica Sant Pau (IIB Sant Pau) (reference number IIBSP-IPE-2020-44).
Informed consent
The Ethics Committee waived the requirement for informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article belongs to the topical collection Pregnancy and Diabetes, managed by Antonio Secchi and Marina Scavini
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xie, X., Liu, J., García-Patterson, A. et al. Gestational weight gain and pregnancy outcomes in women with type 1 and type 2 diabetes mellitus. Acta Diabetol 60, 621–629 (2023). https://doi.org/10.1007/s00592-023-02031-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-023-02031-0