Abstract
Aim
The impact of cholesteryl ester transfer protein (CETP) on atherosclerotic development in humans remains unclear. Plasma cholesteryl ester transfer was shown to be associated with carotid intima-media thickness in type 2 diabetic (T2D) patients with adequate metabolic control. Since glycation of CETP may influence cholesteryl ester transfer processes, it is important to determine if plasma cholesteryl ester transfer is still a determinant of carotid intima-media thickness (IMT) in patients with poorly controlled diabetes. The aim of the present study was to determine whether CETP activity influences carotid IMT in T2D patients with poor metabolic control.
Methods
In 110 individuals with T2D, we measured CETP mass concentration with ELISA, CETP activity with a radioactivity method and carotid intima-media thickness with high-resolution real-time B-mode ultrasonography.
Results
The mean HbA1C was 8.8 ± 1.7%. Carotid IMT did not correlate with CETP activity in the total population. In T2D patients with HbA1C < 8% (n = 33), mean HbA1C was 6.9% and the correlation between carotid IMT and CETP activity was not significant (p = 0.09). In a multivariable analysis that included the total population, carotid intima-media thickness was positively associated with diabetes duration (p = 0.02) but not with CETP activity or HbA1C.
Conclusions
We observed no correlation between carotid intima-media thickness, a marker of early atherosclerosis, and CETP activity in T2D patients with poor metabolic control. Disease duration, which reflects accumulated metabolic abnormalities, may have blunted the potential effect of CETP on atherosclerosis. Metabolic control appears essential to determine the pro- or anti-atherogenic influence of CETP in patients with T2D.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cholesteryl ester transfer protein (CETP) is a transport protein that enables the exchange of cholesteryl esters and triglycerides between HDL and triglyceride-rich lipoproteins. Cohort studies and studies on human genetics have concluded that CETP gene polymorphisms associated with decreased CETP activity are accompanied by a significantly lower risk of atherosclerotic cardiovascular disease [1]. In addition, inhibition of CETP reduces low-density lipoprotein cholesterol (LDL-C) and increases high-density lipoprotein cholesterol (HDL-C), which is consistent with a reduced risk of atherosclerotic cardiovascular disease [2]. However, three different CETP inhibitors have failed to prove a reduced risk of atherosclerotic cardiovascular disease [1]. The impact of CETP on atherosclerotic development therefore remains unclear in humans.
Many studies have shown that plasma cholesteryl ester transfer increased in type 2 diabetes (T2D) [3,4,5]. Nevertheless, only one study has evaluated the association between cholesteryl ester transfer and intima-media thickness (IMT), a marker of early atherosclerosis, in patients with T2D. Plasma cholesteryl ester transfer was shown to be associated with IMT in T2D patients with adequate metabolic control as mean HbA1C was 6.7% [3]. It has been shown that plasma lipoproteins from patients with poor metabolic control and in vitro glycation of lipoproteins enhanced the transfer rate of cholesteryl ester from HDL to apoB-containing lipoproteins [6]. Since glycation of CETP and HDL-related apolipoproteins may influence the cholesteryl ester transfer process [6], it is probably important to determine if plasma cholesteryl ester transfer is still a determinant of IMT in patients whose diabetes is poorly controlled.
The aim of the present study was to determine whether CETP activity influences intima-media thickness in T2D patients with poor metabolic control.
Methods
Study design and patients
One hundred and ten patients were included at the endocrinology department of Dijon University Hospital between December 2008 and May 2010 in this prospective study. The inclusion criteria were: type 2 diabetes, age older than 18 years, no known acute or chronic disease based on history, physical examination and standard laboratory tests (blood counts and electrolyte concentrations). No participants were pregnant.
This prospective single-centered study was approved by our regional ethics committee. Written informed consent was obtained from all patients before inclusion.
Biochemical assay
All patients fasted for 12 h before blood collection. Plasma glucose, total HDL-C and triglycerides were measured on a Vista analyzer with dedicated reagents (Siemens Healthcare Diagnostics, Deerfield, IL). LDL-C was calculated with the Friedewald equation when triglycerides levels were < 3.87 mmol/l. When triglycerides levels were > 3.87 mmol/l, LDL-C was measured directly on the Vista analyzer with dedicated reagents (Siemens Healthcare, Diagnostics). HbA1c was measured with high-performance liquid chromatography on a Variant II device (Bio-Rad, Richmond, CA, USA) (normal range 4–6% [20–60 mmol/mol]).
Measurement of cholesteryl ester transfer activity using a radioactivity method
Cholesteryl ester transfer activity in individual plasma samples (25 μl per assay) was the measured transfer from [3H] cholesteryl ester-containing HDL (2.5 nmol per assay) toward endogenous apoB-containing lipoproteins. [3H] cholesteryl ester-containing HDL was obtained with HDL from one subject with no lipid or glucose metabolism abnormalities.
The cholesteryl ester transfer rate was calculated from the known specific radioactivity of the HDL donors and the accumulation of radiolabeled cholesteryl esters in the LDL acceptors after the deduction of blank values from control mixtures that were incubated at 37 °C without a plasma sample [7, 8]. Total CETP activity was expressed as pmol of 3H-CE transferred per hour.
CETP mass concentration was measured with a specific ELISA with TP1 anti-CETP antibodies as previously described [9]. Intrinsic CETP activity values were calculated from the ratio of the plasma cholesteryl ester transfer rate to the plasma CETP mass concentration and were expressed as nmol of 3H-CE transferred per mg of CETP per hour.
Carotid intima-media thickness measurement
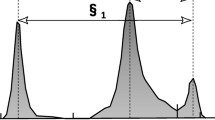
Carotid IMT was measured in all subjects using high-resolution real-time B-mode ultrasonography with a 7.5-MHz linear transducer (Philips HD 11). Each subject was examined in the supine position. The carotid arteries were investigated bilaterally in longitudinal projections. The examination included sections of approximately 2–3 cm of common carotid artery just below the carotid bulb. IMT was defined as the distance between the leading edge of the first echogenic line (lumen–intima interface) and the second echogenic line (media–adventitia interface) of the far wall. IMT was measured at a plaque-free location with a specially designed computer program (Philips Qlab 6.0). Three measurements from both sites were averaged to give the mean IMT.
Statistics
Data are shown as mean ± SD or percentages as indicated. Univariate analyses were done using a linear regression model, with a robust variance estimator. Multivariable analyses were done using a linear regression model. Linearity was checked using multivariable fractional polynomials. Multicollinearity was investigated via the correlation matrix and VIF (variance inflation factor). The adequacy of the model was checked by analysis of residuals. The interaction between CETP activity and HbA1C was tested in the multivariable analyses.
The statistical analyses were done using STATA software version 12.0 (StataCorp, College Station, TX, USA).
Statistical significance was set at a p value of < 0.05.
Results
Table 1 presents the characteristics of the 110 T2D patients. Mean age was 60.5 ± 9.2 years, mean BMI was 35 ± 7.4 kg/m2, and mean HbA1C was 8.8 ± 1.7%. Carotid IMT was 0.72 ± 0.11 mm. The mean plasma triglyceride level was 1.9 ± 0.9 mmol/l, 51% of patients were taking statin therapy, and 17.3% of patients were smokers.
In univariate analysis, carotid IMT correlated with age (β = 0.003, p = 0.02), male gender (β = 0.05, p = 0.02), duration of diabetes (β = 0.002, p = 0.027), systolic blood pressure (β = 0.001, p = 0.01) and CETP mass (β = − 0.03, p = 0.03). Carotid IMT did not correlate with total CETP activity (β = − 0.13, p = 0.790), with intrinsic CETP activity (β = 0.07, p = 0.254) or with lipid parameters (Table 2). All these correlations remained stable after adjustments for statin therapy and smoking.
Intrinsic CETP activity correlated positively with triglycerides (β = 0.08, p < 0.0001), LDL (β = 0.04, p = 0.02) and negatively with HDL (β = − 0.27, p < 0.0001) in all T2D patients. All these correlations were persistent after adjustment for statin therapy.
In TD2 patients with HbA1C < 8% (n = 33), mean HbA1C was 6.9% and the correlation between carotid IMT and intrinsic CETP activity was not significant (p = 0.09). In T2D patients with HbA1C ≥ 8%, mean HbA1C was 9.6% and there was no correlation between carotid IMT and CETP activity (p = 0.706). The results were similar to total CETP activity. In multivariable analyses that included the total population (including CETP activity, HbA1C and duration of diabetes), carotid IMT was independently associated with duration of diabetes (β = 0.002, p = 0.02) but not with CETP activity (β = 0.06, p = 0.335) or HbA1C (β = 0.007, p = 0.237). The interaction between CETP activity and HbA1C has been included in the multivariable analyses, and it was not significantly associated with carotid IMT. In this model, carotid IMT was still independently associated with duration of diabetes (β = 0.002, p = 0.02), but not with other variables. The results of multivariable analysis were similar to total CETP activity.
Discussion
In the current study, we found no correlation between carotid IMT and CETP activity in type 2 diabetic patients with poor metabolic control. This suggests that metabolic control may influence the possible link between plasma cholesteryl ester transfer and premature atherosclerosis in patients with type 2 diabetes.
Average mean carotid IMT ranged from 0.72 to 0.97 mm in a multivariate analysis in 3902 T2D patients [10]. Age [11, 12], sex [11] and blood pressure [12] are well-established determinants of carotid IMT in T2D patients. These associations, which were also reported in a study by de Vries et al. [3], are consistent with our results.
De Vries et al. showed an association between carotid IMT and plasma cholesteryl ester transfer in T2D patients (n = 87) with adequate metabolic control (mean HbA1C = 6.7%) and in control subjects (n = 82) [3]. Nevertheless, it has been shown that plasma lipoproteins from patients (n = 10) with poorly controlled diabetes (Hb1AC > 140 g/l) increased transfer rates of cholesteryl ester from HDL to LDL or VLDL compared with normal controls [6]. Since glycation of CETP and HDL-related apolipoproteins may influence the cholesteryl ester transfer process [6], we hypothesized and demonstrated that the association between carotid IMT and CETP activity is lost in T2D patients with poor metabolic control. On top of that, in patients with HbA1C < 8% (n = 33), we observed a tendency (p = 0.09) between carotid IMT and intrinsic CETP activity in univariate analyses which is in line with de Vries’s observations [3]. The low number of patients in this group may explain the lack of significant correlation between carotid IMT and CETP activity. Duration of diabetes was an independent factor of carotid IMT in a multivariate analysis including CETP activity and HbA1C. Duration of diabetes, which is the reflection of accumulated metabolic abnormalities including chronic hyperglycemia, is an important factor in atherosclerosis development, which may have blunted a potential effect of CETP on atherosclerosis, particularly in T2D patients with poor metabolic control.
As in de Vries’s study, we found that CETP was positively correlated with triglycerides and LDL and negatively with HDL.
Even if the differences in CETP activity were not significant in T2D patients with good and poor metabolic control, CETP activity was higher in T2D patients with poor metabolic control, which echos the observations of Passarelli et al. [6].
Triglycerides were higher in patients with poor metabolic control than in patients with adequate metabolic control (2.1 vs. 1.6 mmol/l, p < 0.05). In patients with poor metabolic control, CETP activity correlated strongly with triglyceride levels (p < 0.0001), while CETP activity was not correlated with triglyceride levels (p = 0.1) in patients with adequate metabolic control. These results confirm that triglycerides are a major modulator of CETP activity [3, 13].
We observed a negative correlation between CETP mass and carotid IMT in the total population and in patients with HbA1C > 8%. Alssema et al. [14] showed no correlation between carotid IMT and CETP concentration in a subgroup of 104 T2D patients. Nevertheless, the metabolic control of these patients is not defined. We observed in our study no correlation between carotid IMT and CETP concentration in patients with HbA1C < 8%, while a negative correlation is observed in patients with HbA1C > 8%. As for the correlation between carotid IMT and CETP activity, we cannot exclude that metabolic control plays a role in the relation between carotid IMT and CETP concentration. In a Mendelian randomization analysis [15], a genetic propensity toward higher CETP concentration was not associated with cIMT in 5655 subjects. In this study, 14% of participants had diabetes. Higher CETP concentrations were associated with lower cIMT in men with diabetes, while higher CETP concentrations were associated with higher cIMT in women with diabetes. Even if we observed no correlation between cIMT and CETP concentration according to gender distribution in our study, our findings in 110 TD2 patients with poor metabolic control are in line with the results observed in men with diabetes in this Mendelian randomization analysis. While observational studies have suggested that lower concentration of CETP is associated with reduced cardiovascular risk, our findings highlight the importance to consider the metabolic background to assess the link between CETP concentration and carotid IMT.
The anti- and pro-atherogenic properties of CETP have been widely discussed for many years [16]. In humans, it is likely that CETP exerts both pro- and anti-atherogenic effects seeing as these properties are defined by a precise metabolic background at a given moment [16, 17]. What we observed in T2D patients with poor metabolic control conflicts with the results from patients with adequate metabolic control, demonstrating that metabolic conditions must be considered when studying CETP and cardiovascular risk.
In conclusion, we observed no correlation between carotid IMT and CETP activity in T2D patients with poor metabolic control, contrary to what has been shown in T2D patients with good metabolic control. We showed that disease duration, which reflects accumulated metabolic abnormalities, influences the development of atherosclerotic disease, potentially blunting the potential effect of CETP on atherosclerosis, particularly in T2D patients with poor metabolic control. Metabolic control has to be taken into account before positive or negative effect of cholesteryl ester transfer on cardiovascular risk can be measured. The mechanisms underlying the lack of association between CETP activity and carotid IMT in T2D patients with poor metabolic control remain unknown.
References
Barter PJ, Nicholls SJ, Kastelein JJP, Rye K-A (2015) Is cholesteryl ester transfer protein inhibition an effective strategy to reduce cardiovascular Risk? CETP inhibition as a strategy to reduce cardiovascular risk: the pro case. Circulation 132(5):423–432
Clark RW, Sutfin TA, Ruggeri RB et al (2004) Raising high-density lipoprotein in humans through inhibition of cholesteryl ester transfer protein: an initial multidose study of torcetrapib. Arterioscler Thromb Vasc Biol 24(3):490–497
de Vries R, Perton FG, Dallinga-Thie GM et al (2005) Plasma cholesteryl ester transfer is a determinant of intima-media thickness in type 2 diabetic and nondiabetic subjects: role of CETP and triglycerides. Diabetes 54(12):3554–3559
Kahri J, Syvänne M, Taskinen MR (1994) Plasma cholesteryl ester transfer protein activity in non-insulin-dependent diabetic patients with and without coronary artery disease. Metabolism 43(12):1498–1502
Riemens SC, van Tol A, Sluiter WJ, Dullaart RP (1999) Plasma phospholipid transfer protein activity is lowered by 24-h insulin and acipimox administration: blunted response to insulin in type 2 diabetic patients. Diabetes 48(8):1631–1637
Passarelli M, Catanozi S, Nakandakare ER et al (1997) Plasma lipoproteins from patients with poorly controlled diabetes mellitus and « in vitro » glycation of lipoproteins enhance the transfer rate of cholesteryl ester from HDL to apo-B-containing lipoproteins. Diabetologia 40(9):1085–1093
Gautier T, Masson D, de Barros JP et al (2000) Human apolipoprotein C-I accounts for the ability of plasma high density lipoproteins to inhibit the cholesteryl ester transfer protein activity. J Biol Chem 275(48):37504–37509
Zeller M, Masson D, Farnier M et al (2007) High serum cholesteryl ester transfer rates and small high-density lipoproteins are associated with young age in patients with acute myocardial infarction. J Am Coll Cardiol 50(20):1948–1955
Guyard-Dangremont V, Lagrost L, Gambert P, Lallemant C (1994) Competitive enzyme-linked immunosorbent assay of the human cholesteryl ester transfer protein (CETP). Clin Chim Acta Int J Clin Chem 231(2):147–160
Lorenz MW, Price JF, Robertson C et al (2015) Carotid intima-media thickness progression and risk of vascular events in people with diabetes: results from the PROG-IMT collaboration. Diabetes Care 38(10):1921–1929
Yamasaki Y, Kodama M, Nishizawa H et al (2000) Carotid intima-media thickness in Japanese type 2 diabetic subjects: predictors of progression and relationship with incident coronary heart disease. Diabetes Care 23(9):1310–1315
Yamasaki Y, Kawamori R, Matsushima H et al (1994) Atherosclerosis in carotid artery of young IDDM patients monitored by ultrasound high-resolution B-mode imaging. Diabetes 43(5):634–639
Barter PJ, Brewer HB, Chapman MJ, Hennekens CH, Rader DJ, Tall AR (2003) Cholesteryl ester transfer protein: a novel target for raising HDL and inhibiting atherosclerosis. Arterioscler Thromb Vasc 23(2):160–167
Alssema M, Dekker JM, Kuivenhoven JA et al (2007) Elevated cholesteryl ester transfer protein concentration is associated with an increased risk for cardiovascular disease in women, but not in men, with Type 2 diabetes: the Hoorn Study. Diabet Med 24(2):117–123
Christen T, Trompet S, Noordam R et al (2018) Mendelian randomization analysis of cholesteryl ester transfer protein and subclinical atherosclerosis: A population-based study. J Clin Lipidol 12(1):137–144.e1
Lagrost L (1999) relationship of cholesteryl ester transfer protein to atherosclerosis. In: Plasma Lipids and Their Role in Disease p. 217‑31. (Advances Vascular Biology; vol. 5)
Chapman MJ, Le Goff W, Guerin M, Kontush A (2010) Cholesteryl ester transfer protein: at the heart of the action of lipid-modulating therapy with statins, fibrates, niacin, and cholesteryl ester transfer protein inhibitors. Eur Heart J 31(2):149–164
Acknowledgements
This work was supported by the Centre Hospitalier Universitaire de Dijon (AOI 2011), and proofreading services were provided by Suzanne Rankin (DRCI). We thank Dr. Serge Aho for his help in complementary statistical analyses.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare they have no conflict of interest
Ethical approval
All procedures performed in the study were in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Written informed consent was obtained from all patients before inclusion.
Additional information
Managed by Antonio Secchi.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bouillet, B., Gautier, T., Terriat, B. et al. CETP activity is not associated with carotid intima-media thickness in patients with poorly controlled type 2 diabetes. Acta Diabetol 56, 749–754 (2019). https://doi.org/10.1007/s00592-019-01340-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-019-01340-7