Abstract
Aim
6q24-related transient neonatal diabetes mellitus (6q24-TNDM) is a rare imprinting disorder characterized by uncontrolled hyperglycemia during the first 6 months of life. The molecular etiology of 6q24-TNDM is attributable to overexpression of the paternally inherited PLAGL1 and HYMAI genes located on the 6q24 locus. One of these major defects is maternal loss of methylation (LOM) at 6q24. In addition, approximately 50% of TNDM patients that present LOM at 6q24 can also display hypomethylation at additional imprinted loci (multilocus imprinting disturbances, MLID). Interestingly, the majority of these patients carry mutations in the ZFP57 gene, a transcription factor required for the adequate maintenance of methylation during early embryonic development.
Methods
Methylation analysis of 6q24 and additional imprinted loci was carried out by MS-MLPA in a Tunisian male patient with clinical diagnosis of TNMD. For the same patient, mutation analysis of the ZFP57 gene was conducted by direct Sanger sequencing.
Results
We report a novel nonsense mutation (c.373C > T; p.R125*; ENST00000376883.1) at the ZFP57 gene causing TNDM-MLID and describe detailed phenotype/epigenotype analysis of TNMD patients carrying ZFP57 mutations.
Conclusion
We provide additional support to the role of ZFP57 as a genetic determinant cause of MLID in patients with TNMD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neonatal diabetes mellitus can be subdivided into transient and permanent forms based on its clinical phenotype. It presents an incidence of 1 case in about 100,000 live births in European countries with the transient form accounting for about 50% (i.e., 1 in 200,000) [1]. Interestingly, different figures have been obtained in the Middle East with higher prevalence of the permanent form [PMDM, 1:30,000 to 1;48,000 in Abou Dhabi and Anatolia (Turkey), respectively] compared with the transient form (TNDM, 1:350.000 in Abou Dhabi and 1:77,400 in Anatolia) [2, 3].
Transient neonatal diabetes mellitus (TNDM; OMIM#601410) is defined as a type of diabetes that appears during the first 6 months of life in a term infant and usually reverts before 5 months of age in most cases [4]. The cardinal presenting features of TNDM are hyperglycemia (which requires treatment with exogenous insulin), intrauterine growth retardation (IUGR), and variable degrees of dehydration [5].
TNDM is most frequently related to defects causing overexpression of the paternally expressed genes PLAGL1 and HYMAI, located on human chromosome 6q24 (6q24-TNDM) [6, 7]. PLAGL1 is a zinc finger DNA-binding protein with tumor suppressor activity and HYMAI is a non-coding RNA gene, whose function is currently unknown. Up-to-date, three mayor disease-causing mechanisms have been described for this disorder: (1) paternal uniparental disomy of chromosome 6 [UPD(6)pat] (40%); (2) paternal duplications of 6q24 (32%); and (3) maternal loss of methylation (LOM) at the PLAGL1 differentially methylated region (PLAGL1:alt-TSS-DMR) (28%) [8]. In addition, patients with LOM at PLAGL1:alt-TSS-DMR may also present methylation defects at additional imprinted loci (multilocus imprinting disturbances, MLID); mostly affecting GRB10:alt-TSS-DMR (7p12.1), PEG3:TSS-DMR (19q13.4), and PPP1R13L (19q13.32), while MEST:alt-TSS-DMR (7q32.2), KCNQ1OT1:TSS-DMR (11p15.5), GNAS-AS1:TSS-DMR (20q13.3), NAP1L5:TSS-DMR (4q22.1), SNU13:alt-TSS-DMR (22q13.2), WRB:alt-TSS-DMR(21q22.2) and PPIEL:Ex1-DMR (1p35.3) are hypomethylated in some patients [9,10,11,12]. In a proportion of these MLID patients, recessive mutations in the ZFP57 gene have been identified. The ZFP57 gene, located at 6p22.3, is a transcription factor involved in the correct maintenance of methylation of imprinted loci [13, 14].
In this study, we present the case of a TNMD patient with 6q24 LOM, MLID and a novel nonsense mutation in the ZFP57 gene. We also review data from the literature and discuss the clinical picture and molecular basis of our patient, highlighting the role of ZFP57 as an important genetic determinant for the diagnosis of TNDM-MLID.
Methods
Case report
The patient was the second child of a young consanguineous couple. The mother had a first pregnancy, poorly followed, giving birth to an anencephalic premature baby who died 24 h later. The patient was born by caesarean section at 37 weeks of gestation due to acute foetal distress after an uneventful pregnancy. He was small for gestational age, weighting 2380 g (between 3rd and 10th percentile), with a length of 47 cm (25th percentile) and a head circumference of 34 cm (50–75 percentile). He was left in maternity near his mother. His blood glucose level (BGL) was checked using Bedside reagent test-strip glucose. BGL was high (5 g/l) after 1 h of life, confirmed by laboratory analysis (27.8 mM of glucose). The neonate was then admitted in neonatology department. On examination, there were no particular physical findings, except a mild dysmorphism consisting in macrostomia, large protruding tongue, and nasal bridge. Unilateral cryptorchidism was also noticed. Thyroid function testing, performed because of the protruding tongue, showed elevated TSH level on the 5th day of life (9 mUI/l) alongside normal T4 levels (14 pmol/l). Thyroid function test showed normal values of TSH (3.4 mUI/l) 15 days later. The blood gasometry, blood cell count, and C reactive protein levels were normal on admission, 24 h and 48 h later, which ruled out a possible maternofoetal infection. The transfontanellar sonography and abdominal ultrasound test did not reveal any abnormalities. The echocardiography and karyotype analysis were normal. Islet cell antibodies were negative. Upon hospitalisation, adequate glycemic control was achieved using continuous intravenous infusion of standard insulin with an initial rate 0.06 U/kg/day via central venous catheter. Insulin doses were increased up to 0.1 U/kg/day. Blood ketones were negative at hyperglycemic periods with no episodes of acidosis. A progressive normalisation of glycemia was observed. Insulin need declined gradually and normoglycemia was obtained with insulin withdrawal at 2 months of age, while he was still hospitalised. Within the first 3 months, BGL values ranged between 0.8 and 1.5 g/l; then, at the forth month, they stabilised and never exceeded 1 g/l. The patient is currently 4 years of age; his growth and physical development are normal.
Genetic analyses
Genomic DNA was extracted from the peripheral blood of the patient and his parents using the FlexiGene DNA Kit (Qiagen, Hilden, Germany) after the informed written consent was signed. This study has been approved by the national Ethics Committee at Farhat HACHED University Hospital (Tunisia).
Methylation analysis
Methylation analysis was used to detect the methylation status at 6q24 using the SALSA MS-MLPA® ME032 kit (MRC-Holland, Amsterdam, The Netherlands) according to the manufacturer’s instructions. Polymorphic microsatellite analysis including D6S286, D6S262, D6S472, D6S976, D6S314, D6S311, D6S308, and D6S305 (http://genome.ucsc.edu/) was performed by fluorescent PCR.
Methylation analysis of additional DMRs was also performed using SALSAMS-MLPA® ME030, ME031, and ME028 kits (MRC-Holland, Amsterdam, The Netherlands). The studied loci included the 11p15.5 region, the GNAS locus (20q13.3), as well as the promoter regions associated with SNRPN (15q11.2). The products were analyzed with the ABI PRISM 3500 DNA Analyzer (Applied Biosystem). MS-MLPA results were then confirmed by methylation-sensitive single-nucleotide primer extension (MS-SNuPE) as previously reported [15].
ZFP57 gene sequencing
ZFP57 gene was analyzed by direct sequencing of exons 1–6 and flanking exon/intron boundaries in the patient and his parents (Transcript: ENST00000376883.1). The primers and conditions are available on request.
For phenotype–genotype correlations, the effect of previously described non-synonymous variants was calculated using in-silico softwares such as PolyPhen-2 and Mutation Taster.
Results
Methylation analysis
Initial methylation testing of PLAGL1:alt-TSS-DMR(6q24) using MS-MLPA revealed a complete loss of maternal methylation. Microsatellite analysis of the patient and his parents around 6q24 region showed biparental inheritance and confirms the diagnosis of TNDM due to 6q24 hypomethylation (supplementary Table 1). To extend these findings, DNA methylation was then analyzed at other imprinted loci across the genome. In addition to the PLAGL1:alt-TSS-DMRLOM, the patient had MLID: he presented total LOM at GRB10:alt-TSS-DMR and partial LOM at MEST:alt-TSS-DMR, GNAS-XL:Ex1-DMR, and GNAS A/B:TSS-DMR. No aberrant methylation was found at the remaining studied DMRs. Results were confirmed by the MS-SNuPE assay.
ZFP57 analysis
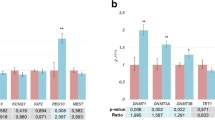
Sanger sequencing of ZFP57 showed a novel homozygous coding variant c.373C > T in exon 6 which generated a premature stop codon (p.Arg125*). The same mutation was found in heterozygosis in both parents. Structure and domains of ZFP57 protein are illustrated in Fig. 1. Up-to-date, 14 ZFP57 gene mutations (six missense, five frameshift, and three nonsense mutations) have been reported. Table 1 summarises previously reported mutations and their expected functional effects. In-silico predictions of missense mutations (p.H438D, p.R228H, p.H257N, p.R228C, p.L254F, and p.S252F) revealed them to be probably damaging on PolyPhen-2v.2.2.2.Online tool Mutation Taster also revealed these mutations to be ‘disease causing’.
Epigenotype–phenotype correlations
Comparison of the clinical and (epi)genetic features of our patient and all reported individuals with ZFP57-related TNDM-MLID are summarised in Table 2. All affected individuals were ascertained through presentation of IUGR 28/29 (96%), hyperglycemia 28/30 (93%), and macroglossia 17/29 (63%) as key clinical features. The high rate of IUGR seems to be related to the crucial role of insulin in foetal growth. Various combinations of congenital anomalies were observed in ZFP57-related TNDM-MLID patients, including facial dysmorphism in 9/30 (30%), cardiac anomalies in 7/29 (24%), umbilical hernia in 7/30 (23%), and developmental delay in 5/29 (17%). Epilepsy and structural brain abnormalities occurred occasionally in 2/28 (7%) and 2/30 (6%) of patients. Furthermore, patients with TNDM-MLID are less likely to develop ketoacidosis, reported in only one newborn.
Genetically, notable similar methylation anomalies were observed in the affected individuals with ZFP57 gene mutations. The epigenotype always included loss of methylation at the TNDM locus and variable combinations of hypomethylation at other maternally imprinted loci: the most affected DMRs are GRB10:alt-TSS-DMR (18/30; 60%) and PEG3:TSS-DMR (17/30; 57%). LOM at MEST:alt-TSS-DMR, KCNQ1OT1:TSS-DMR, and GNAS-AS1:TSS-DMR is less common.
So far, there have been 14 mutations described at ZFP57, including both missense and truncating variants. Most of them are located at the third and fourth zinc finger domains.
There seems to be no correlation between the mutation type or its location and the methylation profile (including affected DMRs and the level of the methylation defect). Regarding the phenotype, it is not related to the mutation, neither the number of affected DMRs nor the methylation levels.
Discussion
TNDM, as uncontrolled hyperglycemia during the first 6 months of life, is an extremely rare presentation of diabetes [1,2,3]. Even some genetic defects have been associated with the disease, it is mainly caused by epigenetic defects at 6q24 [7]. Despite their common epimutation, 6q24 LOM, 50% of TNDM patients have MLID and a portion of them are associated with mutations of the ZFP57 gene [9].
ZFP57 gene is localized on chromosome 6p22.1. It is comprised of 6 exons and encodes a protein of 516 amino acids (ENST00000376883.1). The ZFP57 protein contains a Kruppel associated box (KRAB) domain encoded by exons 4 and 5 and seven zinc fingers (ZFs) domains encoded by exon 6 (Fig. 1) [9, 13]. The previous studies have demonstrated the critical role of ZFP57 in the maintenance of DNA methylation at multiple germline DMRs [13, 14]. Mouse and human ZFP57 proteins bind the methylated hexanucleotide TGCmetCGC [16]. It has been suggested that, in mouse, the protein recognises the methylated TGCmetCGC target sequence using the first and the second ZFs, while specific recognition of the same methylated sequence in human is made through the third and the fourth ZFs [17, 18].
To date, 14 ZFP57 variants have been identified in relation to TNDM-MLID, including the novel mutation described here (Table 2) [4, 9, 13, 19,20,21,22]. Eight of these ZFP57 mutations [p.E86Vfs*28, p.A105*, p.A123*, p.R125*, p.L133Hfs*49, p.C241*, p.T280* (previously named p.279fs*1], and p.Y442Ifs*16 [previously named p.G441Gfs*17)] generate truncated forms of the protein unable to bind the methylated hexanucleotide TGCmetCGC, while six are missense mutations (p.R228C, p.R228H, p.S252F, p.L254F, p.H257N, and p.H438D). Functional studies conducted by Baglivo et al. described the effect of some of the reported ZFP57 mutations on protein structure [18]. In the majority of the cases, truncated and missense mutations affect ZF3 and ZF4 regions, though genetic variants have been also detected at the different domains in patients with 6q24-TNDM. Sequence analysis of hypomethylated regions in ZPF57mut/mut individuals revealed enrichment in TGCmetCGC motif of five maternally imprinted regions: PLAGL1:alt-TSS-DMR, GRB10:alt-TSS-DMR, PEG3:TSS-DMR, GNAS-AS1:TSS-DMR, and NAP1L5:TSS-DMR [8], the most affected DMRs in TNDM-MLID. At a phenotypic level, TNDM-MLID individuals carrying ZFP57 mutations show no clear genotype–phenotype correlation, which explains the variable clinical presentation of this disease [13]. It is, therefore, difficult to predict the phenotype in individuals with MLID, even if compared with patients with hypomethylation confined to 6q24 they present a higher frequency of congenital abnormalities [17]. Table 1 summarises the percentages of occurrence of clinical and (epi)genetic features of the reported TNDM-MLID patients with ZFP57 mutations. Most patients are diagnosed with hyperglycemia (and associated IUGR); commonly reported congenital abnormalities are macroglossia, facial dysmorphism, cardiac anomalies and umbilical hernia [4, 9, 13, 19,20,21,22].
Epigenotype–phenotype correlation, that may explain the clinical variability observed in some TNDM-MLID, was discussed by Boonen et al. [13]. Two possible mechanisms were proposed: the affected loci and the divergent levels of hypomethylation at each of them However, no obvious relationship between both mechanisms and the phenotype was found in their studies [10]. Our data were broadly in line with these results: genetically, notably similar methylation anomalies were observed in our TNDM-MLID patient with total LOM at PLAGL1:alt-TSS-DMR and GRB10:alt-TSS-DMR and partial LOM at MEST:alt-TSS-DMR, and GNAS-AS1:TSS-DMR. However, apart from TNDM-DMR LOM associated with hyperglycemia and IUGR, no consistent abnormalities attributed to changes at GRB10:alt-TSS-DMR, MEST:alt-TSS-DMRand GNAS-AS1:TSS-DMR were found. Regarding the divergent levels of hypomethylation, we found no obvious correlation between methylation levels of affected loci and neither the phenotype. Extending the hypothesised mechanisms, we did not find correlation between the phenotype and the mutation type and its location (affected zinc finger regions).
Besides the implication of epigenetic defects at 6q24 as major finding, TNDM can be associated with some additional genetic defects [7]. Activating heterozygous mutations in the genes encoding either of the subunits of the ATP-sensitive K channel (KATP channel; KCNJ11 or ABCC8) of the pancreatic beta-cell are the second most common cause [22], followed by recessive activating mutations at INS [23] and some very rare cases with genetic alterations at SLC2A2 [24] or HNF1B [25].
The identification of the molecular underlying mechanism is very important as, for example, even 6q24-TNDM is a disorder diagnosed in infancy, a long-term follow-up is important during adolescence and early adulthood as about 50% of patient with 6q24-related TNDM may have a relapse to a permanent form of diabetes mellitus during these periods due to increased insulin demand [4]; the genetic counseling varies if they present only epigenetic changes (with no recurrence) or alterations at ZFP57 (with a recurrent risk on 25% if both parents are carriers); those patients with alterations at KATP channel are susceptible of treatment with sulfonylureas [26], patients carrying alterations at HNF1B are susceptible to present renal cysts among other disorders [27] or Fanconi–Bickel Syndrome if associated with SLC2A2 [28].
To conclude, ZFP57 is an important determinant for the diagnosis of TNDM as well as a crucial factor for understanding the genetic drivers of MLID. Therefore, ZFP57 analysis is advised for accurate genetic counseling. Gathering clinical and (epi)genetic data on TNDM-MLID patients carrying ZFP57 mutations, ZFP57 sequencing should be considered in any TNDM case when at least three DMRs are affected, mainly PLAGL1:alt-TSS-DMR, GRB10:alt-TSS-DMR, and PEG3:TSS-DMR (19q13.4).
References
Iafusco D, Massa O, Pasquino B et al (2012) Minimal incidence of neonatal/infancy onset diabetes in Italy is 1:90,000 live births. Acta Diabetol 49:405–408
Deeb A, Habeb A, Kaplan W et al (2016) Genetic characteristics, clinical spectrum, and incidence of neonatal diabetes in the emirate of Abu Dhabi, United Arab Emirates. Am J Med Genet Part A 170A:602–609
Demirbilek H, Arya VB, Ozbek MN et al (2015) Clinical characteristics and molecular genetic analysis of 22 patients with neonatal diabetes from the South-Eastern region of Turkey: predominance of non-KATP channel mutations. Eur J Endocrinol 172:697–705
Docherty LE, Kabwama S, Lehmann A et al (2013) Clinical presentation of 6q24 transient neonatal diabetes mellitus (6q24 TNDM) and genotype-phenotype correlation in an international cohort of patients. Diabetologia 56:758–762
Temple IK, Gardner RJ, Mackay DJG et al (2000) Transient neonatal diabetes: widening the understanding of the etiopathogenesis of diabetes. Diabetes 49:1359–1366
Mackay DJG, Boonen SE, Clayton-Smith J et al (2006) A maternal hypomethylation syndrome presenting as transient neonatal diabetes mellitus. Hum Genet 120:262–269
Lemelman MB, Letourneau L, Greeley SAW (2018) Neonatal diabetes mellitus: an update on diagnosis and management. Clin Perinatol 45:41–59
Mackay DJG, Temple IK (2010) Transient neonatal diabetes mellitus type 1. Am J Med Genet C Semin Med Genet 154C:335–342
Mackay DJG, Callaway JLA, Marks SM et al (2008) Hypomethylation of multiple imprinted loci in individuals with transient neonatal diabetes is associated with mutations in ZFP57. Nat Genet 40:949–951
Boonen SE, Pörksen S, Mackay DJG et al (2008) Clinical characterisation of the multiple maternal hypomethylation syndrome in siblings. Eur J Hum Genet 16:453–461
Bak M, Boonen SE, Dahl C et al (2016) Genome-wide DNA methylation analysis of transient neonatal diabetes type1 patients with mutations in ZFP57. BMC Med Genet 14:17–29
Docherty LE, Rezwan FI, Poole RL et al (2014) Genome-wide DNA methylation analysis of patients with imprinting disorders identifies differentially methylated regions associated with novel candidate imprinted genes. J Med Genet 51:229–238
Boonen SE, Mackay DJ, Hahnemann JM et al (2013) Transient neonatal diabetes, ZFP57, and hypomethylation of multiple imprinted loci. Diabetes Care 36:505–512
Li X, Ito M, Zhou F et al (2008) A maternal zygotic effect gene, Zfp57, maintains both maternal and paternal imprints. Dev Cell 15:547–557
Begemann M, Leisten I, Soellner L et al (2012) Use of multilocus methylation-specific single nucleotide primer extension (MS-SNuPE) technology in diagnostic testing for human imprinted loci. Epigenetics 7:473–481
Quenneville S, Verde G, Corsinotti A et al (2011) In embryonic stem cells, ZFP57/KAP1 recognize a methylated hexanucleotide to affect chromatin and DNA methylation of imprinting control regions. Mol Cell 44:361–372
Liu Y, Toh H, Sasaki H et al (2012) An atomic model of Zfp57 recognition of CpG methylation within a specific DNA sequence. Genes Dev 26:2374–2379
Baglivo I, Esposito S, De Cesare L et al (2013) Genetic and epigenetic mutations affect the DNA binding capability of human ZFP57 in transient neonatal diabetes type 1. FEBS Lett 587:1474–1481
Court F, Martin-Trujillo A, Romanelli V et al (2013) Genome-wide allelic methylation analysis reveals disease-specific susceptibility to multiple methylation defects in imprinting syndromes. Hum Mutat 34:595–602
Boyraz M, Ulucan K, Taşkın N et al (2013) Transient neonatal diabetes mellitus in a turkish patient with three novel homozygous variants in the ZFP57 gene. J Clin Res Pediatr Endocrinol 5:125–128
Iyigun F, Ozcan B, Kulali F et al (2017) A newborn with transient diabetes mellitus accompanied by ketoacidosis attributable to a ZFP57 mutation. J Trop Pediatr 63:399–401
De Franco E, Flanagan SE, Houghton JA et al (2015) The effect of early, comprehensive genomic testing on clinical care in neonatal diabetes: an international cohort study. Lancet 386:957–963
Garin I, Edghill EL, Akerman I et al (2010) Recessive mutations in the INS gene result in neonatal diabetes through reduced insulin biosynthesis. Proc Natl Acad 107:3105–3110
Sansbury FH, Flanagan SE, Houghton JA et al (2012) SLC2A2 mutations can cause neonatal diabetes, suggesting GLUT2 may have a role in human insulin secretion. Diabetologia 55:2381–2385
Yorifuji T, Kurokawa K, Mamada M et al (2004) Neonatal diabetes mellitus and neonatal polycystic, dysplastic kidneys: phenotypically discordant recurrence of a mutation in the hepatocyte nuclear factor-1beta gene due to germline mosaicism. J Clin Endocrinol Metab 89:2905–2905
Bowman P, Sulen Å, Barbetti F et al (2018) Neonatal Diabetes International Collaborative Group. Effectiveness and safety of long-term treatment with sulfonylureas in patients with neonatal diabetes due to KCNJ11 mutations: an international cohort study. Lancet Diabetes Endocrinol 6:637–646
Clissold RL, Hamilton AJ, Hattersley AT (2015) HNF1B-associated renal and extra-renal disease-an expanding clinical spectrum. Nat Rev Nephrol 11:102–112
Setoodeh A, Rabbani A (2012) Transient neonatal diabetes as a presentation of Fanconi–Bickel Syndrome. Acta Med Iran 50:836–838
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interest.
Ethical approval
Ethical procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national, local ethics committee: Comitato Etico Centrale IRCCS Lazion, Sezione IFO/Fondazione Bietti, Rome, Italy) and with the Helsinki Declaration of 1975, as revised in 2008.
Informed consent
Informed consent was obtained from the patient included in the study.
Additional information
Managed by Massimo Porta.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Touati, A., Errea-Dorronsoro, J., Nouri, S. et al. Transient neonatal diabetes mellitus and hypomethylation at additional imprinted loci: novel ZFP57 mutation and review on the literature. Acta Diabetol 56, 301–307 (2019). https://doi.org/10.1007/s00592-018-1239-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-018-1239-3