Abstract
Type 2 diabetes mellitus is a common comorbidity of COPD, but there are still many doubts about the relation among diabetes and COPD. We retrospectively collected data from patients afferent to our Respiratory Diseases outpatient clinic at the Tor Vergata University Hospital between 2010 and 2012. The study population was analyzed by clusters of age, gender, body mass index (BMI), smoking status, lung function, concomitant pharmacologic therapies and comorbidities. The values of the association between variables were expressed as odds ratio. Data were adjusted for gender, age and possible confounding variables by Mantel–Haenszel method. We identified 493 patients with COPD. Ninety-two (18.7 %) patients were affected by type 2 diabetes mellitus, with no significant gender differences. The prevalence distribution was similar among the different age clusters, but the association was stronger in patients younger than 65 years. The association was present only in obese subjects in whom it was significant only in patients with moderate-to-severe COPD, but not mild COPD. The presence of cardiovascular diseases was significantly associated with diabetes mellitus in patients with COPD. There was a slight association of inhaled corticosteroid (ICS) use with the presence of diabetes mellitus in COPD, but the combination of an ICS with a β2-agonist apparently reduced this association. The association with type 2 diabetes mellitus was greater in patients with COPD respect to general population, and correlated with the increase in BMI and the presence of other comorbidities, suggesting that both diseases may be targets of systemic inflammation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Type 2 diabetes mellitus is a common comorbidity of COPD. Epidemiological data suggest that diabetes mellitus is much more common in patients with COPD than in controls [1–3]. A population-based retrospective study using information obtained from the Health Search Database, owned by the Italian College of General Practitioners, which contains data on more than 900,000 subjects, documented that compared to the non-COPD people, in patients with COPD, there is a higher prevalence of diabetes mellitus (10.5 % in the general population vs. 18.7 % in patients with COPD) [4]. Moreover, a recent study conducted in Taiwan has shown that patients with COPD have a higher risk of type 2 diabetes compared with control subjects after adjusting for confounding factors such as sex, age, residential area, insurance premium, steroid use, hypertriglycemia, hypertension, coronary artery disease and cerebrovascular disease [5]. In contrast to these findings, Korean researchers did not find any association between COPD and higher prevalence of diabetes mellitus, which may be related to high percentage of underweight subjects in the studied population [6]. These differences in results may be due to differences in race and environmental and nutritional factors, and in any case, there may have been misclassification when general practitioners have used specific diagnostic categories, mainly COPD [5].
Since diabetes affects 2–37 % of people with COPD, depending on the patient subgroup studied [7], and in addition, even more important, there are many doubts about the relation among diabetes and COPD [8], we have investigated the association between type 2 diabetes mellitus and COPD, considering the role of further comorbidities, concomitant therapies and morphometric characteristics, by collecting the information recorded in the database of Respiratory Diseases outpatient clinic of a large Italian university hospital.
Materials and methods
Characteristics of the study population
We retrospectively collected data from 830 patients afferent to our Respiratory Diseases outpatient clinic at the Tor Vergata University Hospital between 2010 and 2012.
The data were entered into a spreadsheet consisting of a unique code for patient and aspects of medical history [age, gender, weight, height and body mass index (BMI)], diagnosis of obstructive airway disease (asthma, COPD) and diabetes mellitus, smoking habit and drug therapies prescribed for the respiratory system [β2 agonists, anticholinergic agents, inhaled corticosteroids (ICS), and theophylline] and diabetes mellitus (insulin and hypoglycemic agents) were recorded. Data for cardiovascular and metabolic comorbidities, together with the presence of gastroesophageal reflux disease, osteoporosis, psychiatric disorders and depression were also added as well as all the functional parameters of spirometric tests performed. A total of 785 records passed the quality tests to be used for the epidemiological study.
Statistical analysis
The study was carried out by a cross-sectional and observational field method. It permitted to describe the situation at the time of data collection, at the end of February 2013, and it allowed determining the prevalence of investigated outcomes.
The study population was analyzed by clusters of age (45–54, 55–64, 65–74, 75–84, and older than 84 year), gender, BMI (underweight, normal weight, overweight, and obese), smoking status (current smokers, former smokers and never-smokers), lung function (GOLD criteria), concomitant pharmacologic therapies and comorbidities (single or multiple comorbidities). The primary objective of the present epidemiological study was to evaluate the prevalence of type 2 diabetes mellitus in patients affected by COPD and to compare the observed prevalence to expected prevalence in general population according to 2009 data of the Italian National Institute of Statistics (ISTAT) [8].
The values of the association between variables were expressed as odds ratio (OR) and 95 % confidence interval (95 % CI). Positive or negative OR means a co-relative positive or negative association between evaluated variables. Data were adjusted for gender, age and possible confounding variables by Mantel–Haenszel method, which allows a precision-based estimate of the OR. Furthermore, if the prevalence of variables was >10 %, and the value of the OR was greater or less than 2.5 or 0.05, correction of the OR was carried out [9, 10].
In order to calculate statistical and epidemiological values, computer software GraphPad Prism (CA, USA) and OpenEpi (Dean AG, Sullivan KM, Soe MM. Open Source Epidemiologic Statistics for Public Health) were used.
Results
Demographic characteristics
Four hundred ninety-three patients with COPD represented the study population. These patients had a mean age of 72.1 years (95 % CI 71.2–72.9), 336 (68.1 %) were males and 157 (31.8 %) females, and 30.2 % were current smokers and 59.7 % former smokers. Demographic characteristics and smoking habits are reported in Table 1.
Prevalence of diabetes mellitus in patients with COPD
Ninety-two (18.7 %) patients were affected by diabetes mellitus. There was no difference in the prevalence of diabetes mellitus between men and women (men 19.3 %, women 17.2 %), and the prevalence distribution was similar among the different age clusters (Table 2). The standardized prevalence ratio (SPR) between the observed (study population) and the expected (general population by ISTAT data) prevalence of diabetes mellitus was significantly increased in patients with COPD, in particular in the age clusters from 45 to 64 years (P < 0.001) (Table 2).
With regards to the therapy of diabetes mellitus, 27.5 % of patients were treated with insulin, 63.8 % were receiving oral hypoglycemic agents and 8.7 % were receiving both classes of these drugs. The therapy for type 2 diabetes mellitus, including oral hypoglycemic agents, was not correlated (P > 0.05) with the severity of COPD.
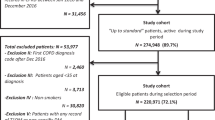
Analysis of the association between COPD and diabetes mellitus
The association between diabetes mellitus and COPD was not influenced (P > 0.05) by age, COPD severity (GOLD classification) and smoking habits, but it was significantly (P < 0.001) modulated by BMI (OR 2.3 and 95 % CI 1.6–3.4). The subset data analysis of BMI categories indicated that the association with diabetes mellitus was detected in obese (P < 0.01), but not in the overweight patients (P > 0.05), independently by the age cluster. In obese subjects, a significant association was detected from moderate-to-severe COPD (P < 0.01), but not in mild COPD (P > 0.05) (Fig. 1; Table 3).
Adjusted odds ratios and 95 % confidence limits of diabetes in patients with COPD through age, GOLD stages, smoking habits and BMI clusters and subset data analyses. ** and *** mean a positive association between diabetes and the relative cluster into the subset strata of COPD population. BMI body mass index
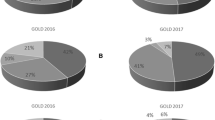
The presence of comorbidities was significantly (P < 0.001) associated with diabetes mellitus in patients with COPD. In particular, cardiovascular diseases, with the exception of cardiac arrhythmia and pulmonary embolism, had significant OR (P < 0.05) ranging from 1.7 to 2.9, and also, the variable dyslipidemia was significantly (P < 0.05) associated with the presence of diabetes mellitus in COPD subjects. The subset analysis of other comorbidities, such as gastroesophageal reflux, osteoporosis, psychiatric diseases and depression, did not indicate statistically significant (P > 0.05) association with diabetes mellitus (Fig. 2; Table 3).
Splitting the study population by respiratory therapy clusters (single-, double- and triple-therapy), we observed that the association between COPD and diabetes was regardless of the use of concomitant medications, although there was a slight association of ICS use with the presence of diabetes mellitus in COPD, but surprisingly, the combination of an ICS with a β2-agonist apparently reduced this association (Fig. 3; Table 3).
Discussion
In the present study, 18.7 % of patients with COPD were affected by type 2 diabetes mellitus, with no significant gender differences. The observed prevalence was higher than the expected prevalence in general Italian population, although the association between COPD and diabetes mellitus was stronger in patients younger than 65 years. This finding confirms what already reported by Feary et al. [3].
It is unknown why people with COPD are affected with type 2 diabetes mellitus more often than controls. Several mechanisms, such as increased obesity, reduced physical activity, increased cigarette smoke and corticosteroid exposure and disease-related inflammation, oxidative stress and hypoxia, may contribute to the increased prevalence of diabetes in COPD [11].
At the best of our knowledge, this is the first study that specifically investigated in patients with COPD the association between type 2 diabetes mellitus and comorbidities. Our data showed that the association of type 2 diabetes mellitus with COPD was present only in obese, but not in the overweight patients, and that in subjects with obesity, there was a significant association with moderate-to-severe.COPD, but not with mild COPD. Obesity has been identified as an important risk factor for diabetes mellitus, and a potential link between obesity and COPD is also increasingly recognized [12]. Recently, we have documented a significant effect size association between BMI and COPD regardless the smoking habit [13]. Adipose tissue is a potent producer of inflammatory mediators and may contribute to systemic inflammation in COPD, possibly via hypoxia [14], but mild-to-moderate COPD, per se, does not enhance adipose tissue inflammation or its contribution to systemic inflammation compared with in well-matched healthy control subjects [15].
Although this is a cross-sectional study, that in its nature cannot identify the real cause of the relationship between variables, systemic inflammation may explain why patients with COPD have an increased risk of developing diabetes mellitus [16]. This is an intriguing hypothesis considering that cigarette smoking can increase the risk of insulin resistance and diabetes by triggering systemic inflammation [17, 18] and oxidative stress [19], both of which are common in COPD [20]. Interestingly, compared to healthy subjects, non-hypoxemic patients with COPD have higher insulin levels, which are related to inflammatory markers such as CRP, IL-6 and soluble receptors for TNF-α [21]. The approach of our study did not allow us to confirm or deny this hypothesis. Nonetheless, it showed that cigarette smoking is not a link between diabetes mellitus and COPD. This is significant information because tobacco smokes exposure is central to the development of COPD [22] and an independent and modifiable determinant of diabetes mellitus [23]. Smoking generates oxidative stress that can activate local and systemic inflammation [24]. If cigarette smoking is not a link, it is possible that other mechanisms beyond systemic inflammation may explain the link between diabetes mellitus and COPD.
The Third National Health and Nutrition Examination Survey (NHANES III) [25] found that previously diagnosed diabetics have an FEV1 lower than that of non-diabetics. Impaired lung function was also greater in patients with poorly controlled diabetes, a finding that is not explained by either obesity or increasing age. The mechanisms involved in the reduction in pulmonary function in patients affected by diabetes are still unclear. Several studies have proposed different mechanisms, such as glycosylation of chest wall and bronchial tree [26], thickening of the pulmonary basal lamina [27] and increased susceptibility to respiratory infections [28]. It has also been demonstrated that increased serum osmolality, which the hyperglycemia contributes to an important part, is associated with a reduction in pulmonary function [29]. Recently, we demonstrated that high glucose concentrations could lead to an enhanced responsiveness of human airway smooth muscle [30]. In particular, results of this study suggested that the Rho/ROCK pathway, together with the mobilization of the intracellular calcium and the phosphorylation of MYPT-1, might play a crucial role in the reduced lung function observed in patients with diabetes [30].
On the other hand, several prospective studies have demonstrated that reduced lung function is an independent predictor of type 2 diabetes [31–33]. In particular, a cross-sectional and prospective study of lung function in adults with type 2 diabetes has suggested the notion that abnormalities in lung function precede diabetes and then continues after the onset of diabetes [34]. Also in this case, our study did not allow us to confirm or deny this hypothesis because the information available to us did not include lung function data collected before the onset of diabetes. However, the prevalence distribution of diabetes mellitus was similar among the various age clusters and there was a significant increase in OR between observed and expected prevalence of diabetes mellitus in clusters of age comprised between 45 and 64. This feature might indicate that COPD and diabetes tend to develop simultaneously and indirectly support the hypothesis that COPD and diabetes mellitus could be two different expressions of a systemic inflammatory syndrome [35].
Another indirect evidence of the possible development of COPD and type 2 diabetes mellitus in the context of a “chronic systemic” inflammatory state lies, in our opinion, in the fact that our study documented that the presence of cardiovascular or metabolic diseases, which have been related to systemic inflammation [36], increased the association between COPD and diabetes mellitus. These results support the evidence that this study has been developed in the context of integrated systems medicine for the study of chronic non-communicable diseases (NCDs) such as type 2 diabetes, COPD and their related comorbidities. This strategy allowed collecting complex data from every patient, useful for a holistic approach to NCDs [37].
In susceptible individuals, hyperglycemia may occur after administration of corticosteroids. Among diabetic patients, ICS use has been reported to be associated with an increased serum glucose concentration in a dose–response manner [36]. Moreover, in a small, prospective, crossover study in patients with established type 2 diabetes mellitus, glycosylated hemoglobin levels rose significantly after 6 weeks of treatment with inhaled fluticasone [38]. However, a recent retrospective analysis that evaluated all double-blind, placebo-controlled trials in patients ≥4 years of age involving budesonide or budesonide/formoterol in COPD (eight trials; budesonide: n = 4,616; non-ICS: n = 3,643) documented that treatment with ICSs in patients with COPD was not associated with increased risk of new onset diabetes mellitus or hyperglycemia [39]. Our data showed a slight association of ICS use with the presence of diabetes mellitus in COPD, but surprisingly, the combination of an ICS with a β2-agonist, but not with an anticholinergic agent, was able to reduce this association. A pooled clinical trial analysis of tiotropium safety showed that there was no apparent increased risk of diabetes overall in patients receiving tiotropium compared with patients receiving placebo, but the relative risk of hyperglycemic events was 1.69 [40]. This finding fits well with our data, but we are unable to explain why the combination of an ICS with a β2-agonist could decrease the OR of diabetes in patients with COPD. In fact, β-adrenoceptors stimulation in the liver induces glycogenolysis and raises blood sugar level [41, 42].
In conclusion, in the present retrospective epidemiological study, we obtained data from a single clinical database, conferring to the study objective features of homogeneity. The association with type 2 diabetes mellitus was greater in patients with COPD respect to general population, and correlated with the increase in BMI and the presence of other comorbidities, suggesting that both diseases may be targets of systemic inflammation. In terms of prognostic implications, there is the need to better understand the link between COPD and type 2 diabetes mellitus, and in particular, whether the center of therapy should be shifted to the systemic inflammatory state. We should also understand whether treatment of COPD influences the course of diabetes mellitus or is altered by the presence of the concomitant comorbid disease. It is also important to know whether treatment of type 2 diabetes mellitus can alter the natural history of concomitant COPD.
References
Mannino DM, Thorn D, Swensen A, Holguin F (2008) Prevalence and outcomes of diabetes, hypertension and cardiovascular disease in COPD. Eur Respir J 32(4):962–969
Barr RG, Celli BR, Mannino DM, Petty T, Rennard SI, Sciurba FC, Stoller JK, Thomashow BM, Turino GM (2009) Comorbidities, patient knowledge, and disease management in a national sample of patients with COPD. Am J Med 122(4):348–355. doi:10.1016/j.amjmed.2008.09.042
Feary JR, Rodrigues LC, Smith CJ, Hubbard RB, Gibson JE (2010) Prevalence of major comorbidities in subjects with COPD and incidence of myocardial infarction and stroke: a comprehensive analysis using data from primary care. Thorax 65(11):956–962
Cazzola M, Bettoncelli G, Sessa E, Cricelli C, Biscione G (2010) Prevalence of comorbidities in patients with chronic obstructive pulmonary disease. Respiration 80(2):112–119. doi:10.1159/000281880
Lee CT, Mao IC, Lin CH, Lin SH, Hsieh MC (2013) Chronic obstructive pulmonary disease: a risk factor for type 2 diabetes: a nationwide population-based study. Eur J Clin Invest 43(11):1113–1119. doi:10.1111/eci.12147
Joo H, Park J, Lee SD, Oh YM (2012) Comorbidities of chronic obstructive pulmonary disease in Koreans: a population-based study. J Korean Med Sci 27(8):901–906. doi:10.3346/jkms.2012.27.8.901
Cavailles A, Brinchault-Rabin G, Dixmier A, Goupil F, Gut-Gobert C, Marchand-Adam S, Meurice JC, Morel H, Person-Tacnet C, Leroyer C, Diot P (2013) Comorbidities of COPD. Eur Respir Rev 22(130):454–475. doi:10.1183/09059180.00008612
ISTAT Annuario statistico italiano 2009. Capitolo 3: Sanità e Salute. http://www3.istat.it/dati/catalogo/20091120_00/PDF/cap3.pdf
Schmidt CO, Kohlmann T (2008) When to use the odds ratio or the relative risk? Int J Public Health 53(3):165–167
Zhang J, Yu KF (1998) What’s the relative risk? a method of correcting the odds ratio in cohort studies of common outcomes. J Am Med Assoc 280(19):1690–1691
Wells CE, Baker EH (2013) Metabolic syndrome and European Respiratory Monograph 59: COPD and Comorbidity 117–134
Franssen FM, O’Donnell DE, Goossens GH, Blaak EE, Schols AM (2008) Obesity and the lung: 5.Obesity and COPD. Thorax 63(12):1110–1117. doi:10.1136/thx.2007.086827
Cazzola M, Calzetta L, Lauro D, Bettoncelli G, Cricelli C, Di Daniele N, Rogliani P (2013) Asthma and COPD in an Italian adult population: role of BMI considering the smoking habit. Respir Med 107(9):1417–1422. doi:10.1016/j.rmed.2013.04.021
Mancuso P (2010) Obesity and lung inflammation. J Appl Physiol 108(3):722–728. doi:10.1152/japplphysiol.00781.2009
van den Borst B, Gosker HR, Wesseling G, de Jager W, Hellwig VA, Snepvangers FJ, Schols AM (2011) Low-grade adipose tissue inflammation in patients with mild-to-moderate chronic obstructive pulmonary disease. Am J Clin Nutr 94(6):1504–1512. doi:10.3945/ajcn.111.023911
Rana JS, Mittleman MA, Sheikh J, Hu FB, Manson JE, Colditz GA, Speizer FE, Barr RG, Camargo CA Jr (2004) Chronic obstructive pulmonary disease, asthma, and risk of type 2 diabetes in women. Diabetes Care 27(10):2478–2484
Walter RE, Beiser A, Givelber RJ, O’Connor GT, Gottlieb DJ (2003) Association between glycemic state and lung function: the Framingham Heart Study. Am J Respir Crit Care Med 167(6):911–916. doi:10.1164/rccm.2203022167/6/911
Rimm EB, Manson JE, Stampfer MJ, Colditz GA, Willett WC, Rosner B, Hennekens CH, Speizer FE (1993) Cigarette smoking and the risk of diabetes in women. Am J Public Health 83(2):211–214
Rosen P, Nawroth PP, King G, Moller W, Tritschler HJ, Packer L (2001) The role of oxidative stress in the onset and progression of diabetes and its complications: a summary of a Congress Series sponsored by UNESCO-MCBN, the American Diabetes Association and the German Diabetes Society. Diabetes Metab Res Rev 17(3):189–212
Laghi F, Adiguzel N, Tobin MJ (2009) Endocrinological derangements in COPD. Eur Respir J 34(4):975–996. doi:10.1183/09031936.00103708
Bolton CE, Evans M, Ionescu AA, Edwards SM, Morris RH, Dunseath G, Luzio SD, Owens DR, Shale DJ (2007) Insulin resistance and inflammation: a further systemic complication of COPD. COPD 4(2):121–126. doi:10.1080/15412550701341053
Buist AS, McBurnie MA, Vollmer WM, Gillespie S, Burney P, Mannino DM, Menezes AM, Sullivan SD, Lee TA, Weiss KB, Jensen RL, Marks GB, Gulsvik A, Nizankowska-Mogilnicka E, Group BCR (2007) International variation in the prevalence of COPD (the BOLD Study): a population-based prevalence study. Lancet 370(9589):741–750. doi:10.1016/S0140-6736(07)61377-4
Manson JE, Ajani UA, Liu S, Nathan DM, Hennekens CH (2000) A prospective study of cigarette smoking and the incidence of diabetes mellitus among US male physicians. Am J Med 109(7):538–542
Chung KF, Adcock IM (2008) Multifaceted mechanisms in COPD: inflammation, immunity, and tissue repair and destruction. Eur Respir J 31(6):1334–1356. doi:10.1183/09031936.00018908
McKeever TM, Weston PJ, Hubbard R, Fogarty A (2005) Lung function and glucose metabolism: an analysis of data from the Third National Health and Nutrition Examination Survey. Am J Epidemiol 161(6):546–556. doi:10.1093/aje/kwi076
Sandler M (1990) Is the lung a ‘target organ’ in diabetes mellitus? Arch Intern Med 150(7):1385–1388
Weynand B, Jonckheere A, Frans A, Rahier J (1999) Diabetes mellitus induces a thickening of the pulmonary basal lamina. Respiration 66(1):14–19
Fine MJ, Smith MA, Carson CA, Mutha SS, Sankey SS, Weissfeld LA, Kapoor WN (1996) Prognosis and outcomes of patients with community-acquired pneumonia: a meta-analysis. J Am Med Assoc 275(2):134–141
Pogson ZE, McKeever TM, Fogarty A (2008) The association between serum osmolality and lung function among adults. Eur Respir J 32(1):98–104. doi:10.1183/09031936.00144207
Cazzola M, Calzetta L, Rogliani P, Lauro D, Novelli L, Page CP, Kanabar V, Matera MG (2012) High glucose enhances responsiveness of human airways smooth muscle via the Rho/ROCK pathway. Am J Respir Cell Mol Biol 47(4):509–516. doi:10.1165/rcmb.2011-0449OC
Lazarus R, Sparrow D, Weiss ST (1998) Baseline ventilatory function predicts the development of higher levels of fasting insulin and fasting insulin resistance index: the Normative Aging Study. Eur Respir J 12(3):641–645
Engstrom G, Janzon L (2002) Risk of developing diabetes is inversely related to lung function: a population-based cohort study. Diabet Med 19(2):167–170
Yeh HC, Punjabi NM, Wang NY, Pankow JS, Duncan BB, Brancati FL (2005) Vital capacity as a predictor of incident type 2 diabetes: the Atherosclerosis Risk in Communities study. Diabetes Care 28(6):1472–1479
Yeh HC, Punjabi NM, Wang NY, Pankow JS, Duncan BB, Cox CE, Selvin E, Brancati FL (2008) Cross-sectional and prospective study of lung function in adults with type 2 diabetes: the Atherosclerosis Risk in Communities (ARIC) study. Diabetes Care 31(4):741–746. doi:10.2337/dc07-1464
Fabbri LM, Rabe KF (2007) From COPD to chronic systemic inflammatory syndrome? Lancet 370(9589):797–799
Barnes PJ (2010) Chronic obstructive pulmonary disease: effects beyond the lungs. PLoS Med 7(3):e1000220. doi:10.1371/journal.pmed.1000220
Bousquet J, Anto JM, Sterk PJ, Adcock IM, Chung KF, Roca J, Agusti A, Brightling C, Cambon-Thomsen A, Cesario A, Abdelhak S, Antonarakis SE, Avignon A, Ballabio A, Baraldi E, Baranov A, Bieber T, Bockaert J, Brahmachari S, Brambilla C, Bringer J, Dauzat M, Ernberg I, Fabbri L, Froguel P, Galas D, Gojobori T, Hunter P, Jorgensen C, Kauffmann F, Kourilsky P, Kowalski ML, Lancet D, Pen CL, Mallet J, Mayosi B, Mercier J, Metspalu A, Nadeau JH, Ninot G, Noble D, Ozturk M, Palkonen S, Prefaut C, Rabe K, Renard E, Roberts RG, Samolinski B, Schunemann HJ, Simon HU, Soares MB, Superti-Furga G, Tegner J, Verjovski-Almeida S, Wellstead P, Wolkenhauer O, Wouters E, Balling R, Brookes AJ, Charron D, Pison C, Chen Z, Hood L, Auffray C (2011) Systems medicine and integrated care to combat chronic noncommunicable diseases. Genome Med 3(7):43
Slatore CG, Bryson CL, Au DH (2009) The association of inhaled corticosteroid use with serum glucose concentration in a large cohort. Am J Med 122(5):472–478. doi:10.1016/j.amjmed.2008.09.048
Faul JL, Wilson SR, Chu JW, Canfield J, Kuschner WG (2009) The effect of an inhaled corticosteroid on glucose control in type 2 diabetes. Clin Med Res 7(1–2):14–20. doi:10.3121/cmr.2009.824
O’Byrne PM, Rennard S, Gerstein H, Radner F, Peterson S, Lindberg B, Carlsson LG, Sin DD (2012) Risk of new onset diabetes mellitus in patients with asthma or COPD taking inhaled corticosteroids. Respir Med 106(11):1487–1493. doi:10.1016/j.rmed.2012.07.011
Kesten S, Jara M, Wentworth C, Lanes S (2006) Pooled clinical trial analysis of tiotropium safety. Chest 130(6):1695–1703. doi:10.1378/chest.130.6.1695
Philipson LH (2002) beta-Agonists and metabolism. J Allergy Clin Immunol 110(6 Suppl):S313–S317
Conflict of interest
The authors declare that they have no conflict of interest.
Human and Animal Rights disclosure
In this retrospective epidemiological study no experiments have been carried out on human subjects. All procedures were in accordance with the local Independent Ethics Committee standards and collected data can be used for scientific studies without any further authorization from an Ethics Committee.
Informed consent disclosure
Epidemiological data have been recorded in the database of Respiratory Diseases outpatient clinic at the Tor Vergata University Hospital (Rome, Italy) with the written consent of the patients, lawfully stored, managed according to privacy rules and all identifying details have been omitted.
Author information
Authors and Affiliations
Corresponding author
Additional information
Managed by Massimo Federici.
Rights and permissions
About this article
Cite this article
Rogliani, P., Calzetta, L., Segreti, A. et al. Diabetes mellitus among outpatients with COPD attending a university hospital. Acta Diabetol 51, 933–940 (2014). https://doi.org/10.1007/s00592-014-0584-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-014-0584-0