Abstract
Diabetes mellitus (DM) is an important risk factor for accelerated atherosclerosis and increases cardiovascular disease. Several studies found a higher mortality rate in postoperative diabetic patients than in non-diabetic patients. However, other studies found conflicting evidence on bypass graft dysfunction in patients with diabetes mellitus. We therefore investigated the influence of diabetes mellitus on the long-term outcome after coronary artery bypass surgery (CABG). In this prospective study, 936 consecutive CABG patients were included. These patients were divided into three groups: patients without diabetes mellitus, patients with diabetes mellitus using oral drugs (non-insulin-treated DM) and patients with diabetes mellitus using insulin (insulin-treated DM). The three groups were compared for mortality and (angiographic) bypass graft dysfunction. Of the 936 included patients, 720 (76.8%) patients were non-diabetics, 138 (14.7%) were non-insulin-treated DM, and 78 (8.3%) patients were insulin-treated DM. Follow-up was achieved in all patients, at a mean of 33 months. Mortality was significantly higher in patients with insulin-treated DM, compared with non-insulin-treated DM or non-diabetic patients (P = 0.003). Fourteen (1.5%) patients suffered a myocardial infarction after CABG. A coronary angiography was performed in 77 (8.2%) patients during follow-up, proven bypass graft dysfunction was found in 41 (53.2%) patients. There was no significant difference in bypass graft dysfunction between the three groups. Diabetes mellitus has a significant impact on long-term follow-up after coronary surgery. Particularly insulin dependency is related to an increased mortality. However, diabetes has no influence on angiographically proven bypass graft dysfunction.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Diabetes mellitus is an important risk factor that contributes to accelerated atherosclerosis. Different theories about the pathophysiology exist. Probably the coronary artery endothelial cells become inflamed that accelerate the atherosclerotic process [1]. This continuous process is responsible for the development of coronary artery disease (CAD) and may be the pivotal mechanism in the development of the extensive multi-vessel atherosclerosis seen in diabetic patients, who subsequently need to have cardiac bypass surgery.
Accelerated atherosclerosis is not limited to the coronary arteries, other vessels are also affected. These vessels, such as the internal mammary artery and saphenous veins, are used in CABG to bypass the coronary stenoses. If accelerated atherosclerosis results in bypass graft dysfunction, it may influence long-term mortality.
Several studies found a higher mortality in patients with DM undergoing CABG [2–5]. Additionally, others also found a higher incidence of bypass graft dysfunction in diabetic patients [6, 8].
However, the results differed between non-insulin-dependent diabetes mellitus (non-insulin-treated DM) and insulin-dependent diabetes mellitus (insulin-treated DM). One study found more bypass graft dysfunction only in patients with insulin-treated DM [6, 7], while the other study found this both in non-insulin-treated DM and in insulin-treated DM [8].
Therefore, we aimed to investigate whether diabetes has a negative impact on bypass graft dysfunction and mortality in a series of consecutive patients undergoing coronary artery bypass graft surgery.
Methods
We prospectively included 936 consecutive patients who underwent an isolated CABG from December 2001 until November 2006. This group encompasses all patients, both stable outpatients as well as unstable clinical patients. All patients were referred from the Medical Centre Alkmaar to the department of thorax surgery at the VU Medical Centre.
The patients were divided into three groups: patients without diabetes mellitus, patients with non-insulin-treated DM using only oral hyperglycemic drugs, and patients with insulin-treated DM using insulin with or without oral hyperglycemia.
The primary endpoint of this study is the occurrence of death. The secondary endpoints were myocardial infarction, re-CABG, PCI, and angiographically proven bypass graft dysfunction. Repeat angiography was performed on clinical indications at the discretion of the treating physician. Angiographically proven bypass graft dysfunction is defined as the occurrence of a >50% stenosis in a bypass graft.
End-points were obtained from the hospital charts or by telephone contact with the family doctor.
Permission for this study has been given by the Medical Ethics Commission.
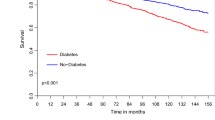
Statistical analysis was performed using SPSS version 14.0. For comparing the description of study population, Chi-square tests and ANOVA tests were used. A P-value of 0.05 is considered statistically significant. Cox-regression was used for multivariate analysis. The Kaplan–Meier curves were used to show mortality and bypass graft dysfunction in relation to time.
Results
Between December 2001 and November 2006, 936 consecutive patients were referred from our center to the VU medical center for isolated CABG. A majority of them were men (76%) with a mean age of 67 (SD ± 10) years. Previous CABG was reported in 5%, percutaneous coronary intervention (PCI) in 20 and 63% experienced a previous myocardial infarction. Multi-vessel coronary disease was found in 94%, while 7% had a poor left ventricle function.
Diabetes mellitus was found in 23% in this study population (Table 1). Of these diabetic patients, 138 (15%) used oral medication and 78 patients used insulin (8%). Nineteen percent of the diabetic patients had microvascular complications such as retinopathy, neuropathy, and amputations. Nine percent of diabetic patients had at least a 1.5 times increase in serum creatinine level.
Follow-up was achieved in all patients, at an average of 33 months (SD ± 20). Table 2 shows the outcome of the primary and secondary endpoints. The long-term mortality rate in these real-world consecutive bypass graft surgery patients is 7.5%. During this follow-up period, the incidence of the secondary endpoints were: 1% myocardial infarction, 0% re-CABG, and 4% PCI.
Mortality
The 30-day mortality was 0.9% (8 patients). All patients left the operating room alive. One patient died within 24 h postoperatively, five patients died before discharge, and two additional patients died within 30 days. Of these, four had a cardiac-related death of whom two suddenly died. Two patients died neurologically and one after femur fracture. The eighth patient died of an unknown cause.
The average 3-year (4 month–5 years) mortality was 7.5% (70 patients). Twenty-three patients had a cardiac course of death, 46 cases had a non-cardiac death, while in one case the course of death was unknown. Non-cardiac death was predominantly driven by oncology-related death (23%) and CVA (23%). Cardiac death was primarily driven by sudden death (40%) and heart failure (24%).
The 3-years mortality rates among the three patient subgroups is significantly higher in the insulin-treated diabetic patients than in non-insulin-treated diabetic and non-diabetic patients (17% vs. 9% vs. 6%; P = 0.003) (Fig. 1).
In multivariate analysis, age, poor left ventricle function, and diabetes were found predictors for late mortality after coronary artery bypass surgery (Table 3). Using these data, a power calculation indicates that 900 patients would be needed to ascertain that this difference in mortality between diabetic and non-diabetic patients reaches significance.
Myocardial infarction
Fourteen (1.5%) patients suffered a myocardial infarction postoperatively. Of these patients, two patients had insulin-treated DM, two patients had non-insulin-treated DM, and 10 patients had no DM. There is no significant difference between the three groups.
PCI
On long-term follow-up, 36 patients underwent a PCI postoperative. In 11 cases, the PCI was performed in the native coronary system. On angiography, 25 patients had bypass graft dysfunction, for which an intervention was deemed necessary; 24 patients received a PCI in the diseased bypass graft and 1 patient received a PCI in the native system. No significant difference was found between the three groups.
Angiographically proven bypass graft dysfunction
Seventy-seven patients underwent a coronary angiographic during follow-up; bypass graft dysfunction was found in 41 (53.2%) patients. One patient needed a re-CABG, 25 patients received a PCI and 15 patients were treated conservatively with medicines. There is no significant difference between the three groups.
Discussion
We investigated the relationship between diabetes and long-term outcome in consecutive real-world patients undergoing coronary bypass surgery. The mortality of patients with insulin-treated DM was significantly higher than that of patients with non-insulin-treated DM and patients without diabetes mellitus. Second, the incidence of bypass graft dysfunction was not significantly different between the three groups.
Diabetes mellitus, an increasing problem
Diabetes mellitus is an increasing health problem in the Netherlands [9] and one of the key risk factors for coronary artery disease. Therefore, the incidence of DM in patients with CAD will increase, particularly in bypass surgery patients. The prevalence of DM in the Netherlands is 39 in 1,000 people and still increasing [9]. In 2007, there were 740,000 people with diabetes and this figure is expected to increase to 1.3 million in 2025. At the same time, the age on which diabetes becomes apparent decreases, caused by overweight and other risk factors for diabetes [9]. With an increase in prevalence and a longer duration of the disease, we may anticipate a larger cohort of patients who may develop diabetic complications.
Cardiovascular complications are among the most obvious hallmarks of a long-lasting state of metabolic dysregulation during diabetes. Furthermore, it is well known that both complications and therapy-induced normalization of hyperglycemia are more difficult to manage or obtain when diabetes lasts longer. The process of accelerated arteriosclerosis in the coronary arteries will be augmented by the long-lasting hyperglycemia in these patients and cause extensive CAD [1]. Therefore, the real-world bypass surgery population will consist of high percentage diabetic patients [10–13].
In this study, we found a prevalence of diabetes mellitus of 23% in a 4-year inclusion period. With an increasing incidence of diabetics in the whole population [9], we may expect that at least 50% of our future CABG population will have DM in the next 20 years.
Short-term mortality and diabetes mellitus
Our study population was an unselected population of consecutive surgery patients with similar baseline characteristics as in earlier studies. We also observed that lower age, more women, lower ejection fraction, and previous CABG were related to diabetes [4–6, 8, 14, 15]. Our 30-day mortality was beyond one percent and comparable with other studies with the same design. This low peri-operative and in-hospital mortality rate provide evidence that diabetes mellitus has no negative impact on short-term clinical outcome [16].
However, metabolic dysregulation is of importance in the immediate postoperative period and related to complications [17], particularly sternal wound infections. Another explanation could be the severity of the diabetes. The influence of such a high peri-operative glucose-level has been described earlier [18, 19]. These studies acknowledge the importance of peri-operative regulation of glucose-levels as this improved the prognosis.
The 30-day mortality is particularly driven by cardiac causes due to a reduced LV function and therapy-resistant heart failure or sudden death. No patients died due to immediate graft failure.
Long-term mortality and diabetes mellitus
Long-term (3 years) mortality, in contrast to short-term mortality, was related to the presence of diabetes. Patients with insulin-treated DM had a significantly higher mortality than others, and non-insulin-treated DM was not related to an adverse mortality rate. This observation is in line with that of Mehran et al. [8], but in conflict with others who found a higher mortality ratio in all diabetic patients [2, 4, 5].
One explanation for the difference between these outcomes could be the duration of diabetes. Most patients who use insulin have diabetes for a longer time than patients using only oral medication. Consequently, accelerated atherosclerosis by diabetes exists for a longer time. Also the influence of co-morbidity in diabetic patients might be higher in these patients. We are limited however in our knowledge regarding the influence of comorbidity in our patients.
Another explanation could be the severity of the diabetes. Patients using insulin might have had episodes of higher glucose-levels, particularly in the direct postoperative period. These patients therefore may represent a more extensive metabolic dysregulation burden indicated by a higher area under the hyperglycemia-to-time curve. Further studies on the relationship between DM severity and outcomes may unravel this issue.
Diabetes and bypass graft dysfunction
In this study, bypass graft dysfunction was defined as angiographically confirmed bypass graft dysfunction. We found no higher incidence of angiographically proven bypass graft dysfunction in patients with diabetes compared with non-diabetic patients.
Bypass graft dysfunction is difficult to compare between different studies, as the definition varies [6–8]. Probably a few studies overvalue bypass graft dysfunction, as they use both hard and soft endpoints. They used angiography or CT-scanning but also included angina as a marker of graft dysfunction. As we only used a hard endpoint, we may undervalue bypass graft dysfunction by refraining from angiography in all the patients.
Limitations
We acknowledge the fact that this study describes a single center experience; however, the findings are comparable with those of others. The provided multivariate analysis shows the importance of diabetes on late mortality. However, its interpretation should be cautioned given its modest predictive value.
Conclusion
Diabetes mellitus has a significant impact on long-term follow-up after coronary surgery whereby insulin dependency, in our study possibly reflecting the duration of diabetes mellitus, is related to an increased mortality. However, it had no influence on angiographically proven bypass graft dysfunction.
References
Mazzone T, Chait A, Pultzky J (2008) Cardiovascular disease risk in type 2 diabetes mellitus: insights from mechanistic studies. Lancet 371:1800–1809
Leavitt BJ (2007) The effects of diabetes mellitus on coronary artery bypass graft surgery. Curr Diab Rep 7:20–24
Leavitt BJ, Sheppard L, Maloney C, Clough RA, Braxton JH, Charlesworth DC, Weintraub RM, Hernandez F, Olmstead EM, Nugent WC, O’Connor GT, Ross CS (2004) Effect of diabetes and associated conditions on long-term survival after coronary artery bypass graft surgery. Circulation 110(suppl II):II-41–44
Filsoufi F, Rahmanian PB, Castillo JG, Mechanick JI, Sharma SK, Adams DH (2007) Diabetes is not a risk factor for hospital mortality following contemporary coronary artery bypass grafting. Interact Cardiovasc Thorac Surg 6:753–758
Rajakaruna C, Rogers CA, Suranimala C, Angelini GD, Ascione R (2006) The effect of diabetes mellitus on patients undergoing coronary surgery: a risk-adjusted analysis. J Thorac Cardiovasc Surg 132:802–810
Gitman MR, Okrainee K, Nguyen H, Duerr R, Del Cor M, Fourchy D, Huynh T, Lader E, Rogers FJ, Chaudry MR, Pilote L, Eisenberg MJ (2005) Impact of diabetes on 12 month outcomes following coronary artery bypass graft surgery: results from the ROSETTA-CABG registry. Can J Cardiol 21(13):1169–1174
Mohammadi S, Dagenais F, Mathieu P, Kingma JG, Doyle D, Lopez S, Baillot R, Perron J, Charbonneau E, Dumont E, Metras J, Desaulniers D, Voisine P (2007) Long-term impact of diabetes and its comorbidities in patients undergoing isolated primary coronary artery bypass graft surgery. Circulation 116(11 suppl I):1-220–1-225
Mehran R, Dangas GD, Kobayashi Y, Lansky AJ, Mintz GS, Aymong ED, Fahy M, Moses JW, Stone GW, Leon MB (2004) Short- and long-term results after multivessel stenting in diabetic patients. J Am Coll Cardiol 43:1348–1354
Baan CA, Schoemaker CG, Jacobs-van der Bruggen MAM, Hamberg-van Reenen HH, Verkleij H, Heus S, Melse JM (2009) Diabetes tot 2025. Preventie en zorg in samenhang. RIVM rapport 260322004. http://www.rivm.nl/bibliotheek/rapporten/260322004.html
Calafiore AM, Di Mauro M, Di Giammarco G, Contini M, Vitolla G, lacò AL, Canosa C, D’Alessandro S (2003) Effect of diabetes on early and late survival after isolated first coronary bypass surgery in multivessel disease. J Thorac Cardiovasc Surg 125:144–154
Niles NW, McGrath PD, Malenka D, Quinton H, Wennberg D, Shubrooks SJ, Tryzelaar JF, Clough R, Hearne MJ, Hernandez F Jr, Watkins MW, Gerald T (2001) O’Connor for the Northern New England cardiovascular disease study group. Survival of patients with diabetes and multivessel coronary artery disease after surgical or percutaneous coronary revascularization: results of a large regional prospective study. J Am Coll Cardiol 37:1008–1015
The BARI 2d study Group (2009) A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med 360:2503–2515
Marcheix B, Eynden FV, Demers P, Bouchard D, Cartier R (2008) Influence of diabetes mellitus on long-term survival in systematic off-pump coronary artery bypass surgery. Ann Thorac Surg Assoc 86:1181–1188
Cole JH, Jones EL, Craver JM, Craver JM, Guyton RA, Morris DC, Douglas JS Jr, Ghazzal Z, Weintraub WS (2002) Outcomes of repeat revascularization in diabetic patients with prior coronary surgery. J Am Coll Cardiol 40:1968–1975
Antunes PE, de Oliveira JF, Antunes MJ (2008) Coronary surgery in patients with diabetes mellitus: a risk-adjusted study on early outcome. Eur J Cardiothorac Surg 34(2):370–375
Carson JL, Scholz PM, Chen AY, Peterson ED, Gold J, Schnieder SH (2002) Diabetes mellitus increases short-term mortality and morbidity in patients undergoing coronary artery bypass graft surgery. J Am Coll Cardiol 40:418–423
Furnary AP, Gao G, Grunkemeier GL, Wu YX, Zerr KJ, Bookin SO, Floten HS, Starr A (2003) Continuous insulin infusion reduces mortality in patients with diabetes undergoing coronary artery bypass grafting. J Thorac Cardiovasc Surg 125:1007–1021
Ascione R, Rogers CA, Rajakaruna C, Angelini GD (2008) Inadequate blood glucose control is associated with in-hospital mortality and morbidity in diabetic and nondiabetic patients undergoing cardiac surgery. Circulation 118:113–123
Furnary AP, Wu YX (2006) Clinical effects of hyperglycemia in the cardiac surgery population: the Portland diabetic project. Endocr Pract 12(Suppl 3):22–26
Acknowledgments
The authors would like to acknowledge Sophie Umans for helping in data entry.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wit, M.A.M., de Mulder, M., Jansen, E.K. et al. Diabetes mellitus and its impact on long-term outcomes after coronary artery bypass graft surgery. Acta Diabetol 50, 123–128 (2013). https://doi.org/10.1007/s00592-010-0223-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-010-0223-3