Abstract
Purpose
Periprosthetic joint infection is a complication of total joint arthroplasty with treatment costs over $1.6 billion dollars per year in the US with high failure rates. Therefore, generation of coatings that can prevent infection is paramount. Diamond-like carbon (DLC) is an ideal coating for implants as they are wear-resistant, corrosion-resistant, inert, and have a low friction coefficient. The purpose of this study was to test the efficacy of DLC surface treatment in prevention of biofilm on titanium discs infected with Staphylococcus aureus in vitro.
Methods
Titanium alloy discs (n = 4 non-coated and n = 4 DLC-coated) were infected with 5 × 105 colony-forming units (CFU) of S. aureus for 2 weeks then analysed via crystal violet and scanning electron microscopy (SEM).
Results
Crystal violet analysis yielded differences in the appearance of biofilm on implant surface where DLC-coated had a clumpier appearance but no difference in biofilm quantification. Interestingly, this clumpy appearance did lead to differences in SEM biofilm coverage where significantly less biofilm coverage was found on DLC-coated discs (81.78% vs. 54.17%, p < 0.003).
Conclusion
DLC-coated titanium alloy implants may have preventative properties in S. aureus infection. Observing differences in biofilm coverage does warrant additional testing including CFU titration and biofilm kinetics with eventual use in an animal model of periprosthetic joint infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Periprosthetic joint infection (PJI) is a complication of total joint arthroplasty (TJA) with high treatment cost, high failure rates, and reduced quality of life. PJI risk is highest during the early postoperative period but is a persistent risk throughout the lifetime of the joint ranging from 0.5 to 2.0% at 15 years [1]. With overall increases in the number of knee and hip replacements, the number of infections is expected to increase and cost over $1.85 billion annually by 2030 [2]. With current treatments including debridement, systemic antibiotics, local antibiotics, and staged revisions where implants are removed and replaced, failure rates are still quite high leading to over a 26% mortality rate at 5 years [1, 3].
The major culprit of failed treatment surgery is bacterial biofilm. This biofilm is produced by multiple bacterial species that are involved in PJI including gram-positive bacteria (82%)—Staphylococcus aureus (S. aureus) and S. epidermidis, coagulase-negative Staphylococci species, and gram-negative bacteria (11%)—Enterobacterales and Pseudomonas aeruginosa [1, 4]. Indeed, this biofilm growth on the implant surface makes bacteria over 1000 × less susceptible to antibiotics; therefore, staged revisions are the most successful treatment option for PJI [1, 5].
While overall infection rates have decreased with implementation of prophylactic strategies to limit infection, periprosthetic infections have not been eradicated. Therefore, alternative methods that can limit infection need to be developed that can provide long-acting protection outside the immediate surgical window, like antibacterial implant coatings.
Diamond-like carbon (DLC) is an ideal coating for implants as they are wear-resistant, corrosion-resistant, inert, and have a low friction coefficient and, therefore, has the potential to increase the life of the implant and benefit patients [6, 7]. These coatings can be introduced to a surface via two methods: plasma-based immersion ion implantation and deposition (PBIIID), which can coat a 3D surface or filtered cathodic vacuum arc (FCVA) which coats a planar surface [7]. These coatings have been tested for their wear-resistance, corrosive-resistance, biocompatibility, and inertness with various types of orthopaedic-related metals including cobalt chromium, titanium alloy, steel, and ultra-high molecular weight polyethylene (UHMWPE) [6,7,8,9,10].
These DLC coatings have intrinsic antibacterial properties by decreasing bacterial adhesion and can also be carriers for metal ions for increased antibacterial and antibiofilm effectiveness with implications in both primary and revision joint replacements [11]. DLC composites including silver [12], copper [12], silicone [13], titanium [14], etc., have also shown antibacterial effectiveness, and this effectiveness is not limited to metals as it can also be utilized on other materials such as polyurethane catheters [15], polyethylene [16], and textile silk bandages [17].
The purpose of this study is to test the efficacy of DLC surface treatment in prevention of biofilm on titanium discs infected with Staphylococcus aureus (S. aureus) in vitro.
Methods
Disc manufacturing
Discs were manufactured by Signature Orthopaedics. Discs were made of Grade 5 Ti-6Al-4 V ASTM B348. Discs were manufactured with solid carbide tooling using a Haas CNC machine and flat sanded on 600 grit aluminium oxide sandpaper. The disc dimensions were as follows: 12 mm major axis and 8 mm minor axis with 2.5 mm thickness. All finishes were machined finishes. Implants were gamma sterilized at Signature prior to shipment and use.
Bacteria preparation
Staphylococcus aureus (ATCC 49525, ATCC, Manassas, VA) were cultured overnight in kanamycin sulphate (200 µg mL−1) Luria broth (LBK) with agitation at 200 rpm at 37 °C. Aliquots for experimentation were taken during the log-phase of growth based on optical density (OD).
Biofilm culturing
Discs were placed into a 12-well dish with 5 × 105 CFU S. aureus in 4 mL media. Samples were incubated at 37 °C with air supplement, without agitation. Two mL of media was replaced every other day without mixing the media prior to aspiration. For this pilot experiment, n = 4 non-coated discs and n = 4 DLC-coated discs were cultured for biofilm growth and separated for analysis into n = 2/group for crystal violet biofilm assay quantification and n = 2/group for scanning electron microscopy (SEM) imaging analysis.
Crystal violet assay
Media was aspirated from each well and gently washed using PBS to remove any non-adherent planktonic bacteria. Discs were submerged in 1 mL of 5% crystal violet solution for 20 min then aspirated and rinsed. Discs were left to dry and photographed for qualitative analysis. To quantify biofilm, discs were submerged in 1 mL of 30% acetic acid to solubilize the crystal violet for 15 min, diluted 8 × with deionized water, and OD was measured at 595 nm.
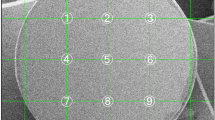
Scanning electron microscopy
SEM processing, imaging, and analysis were completed based on standardized methods done previously [18]. In short, discs were fixed with 4% paraformaldehyde and dehydrated using an ethanol soaking series. Samples were dried and sputter coated with 25 nm of gold and analysed using a Zeiss SIGMA VP-FESEM (White Plains, NY) using a custom script written in DigitalMicrograph software (Gatan Inc., Pleasanton, CA) to automate the SEM stage and image capture. Twenty images were collected at 1500 × magnification and 5 kV from the top surface of the disc.
Each SEM image was segmented using the Trainable Weka Segmentation plugin in Fiji (distribution of ImageJ, NIH, Bethesda, MD). Classifier was previously trained on 25 images to distinguish biofilm-present and biofilm-absent sections. The segmentation result was generated and analysed by the per cent area coverage calculator on Fiji [18].
Statistics
Not all groups were normally distributed (based on Shapiro–Wilk test). Therefore, nonparametric Kruskal–Wallis ANOVA with Dunn’s post-test was done using GraphPad Prism 8.0 (San Diego, CA).
Results
Qualitative assessment of biofilm via crystal violet showed a less uniform, clumpier biofilm coverage on DLC-coated discs compared to non-coated discs (Fig. 1A). Of note, DLC-coated discs were darker in colour compared to non-coated discs. Quantitative assessment of biofilm via optical density showed no difference in OD between groups (non-coated OD = 0.304 and DLC-coated OD = 0.272; Fig. 1B).
Crystal violet biofilm analysis yields no difference in biofilm. Discs were incubated with 5 × 105 CFU S. aureus for 2 weeks. (A) Discs were washed with saline and stained with crystal violet for biofilm visualization. (B) Discs were subsequently soaked in acetic acid for crystal violet quantification. NS = not significant
Baseline SEM imaging on non-infected discs showed that DLC coating did modify the surface of the discs where surface was smoother, and crevices were not as apparent compared to non-coated (Fig. 2). Upon infection, qualitative assessment did show differences in appearance of the biofilm between groups where biofilm on DLC-coated discs did not look as densely packed (Fig. 3A). Indeed, when imaged and quantified, areas of biofilm coverage were significantly decreased in the DLC-coated discs compared to the non-coated discs when all images were analysed separately (non-coated biofilm coverage = 81.78% ± 4.34% vs. DLC-coated biofilm coverage = 54.17% ± 18.66%; p < 0.0001; Fig. 3B) or averaged per disc (non-coated biofilm coverage = 81.78% ± 1.32% vs. DLC-coated biofilm coverage = 54.17% ± 1.690%; p = 0.0030; Fig. 3C).
SEM biofilm analysis yields significant difference biofilm coverage. Discs cultured with S. aureus for 2 weeks were washed after incubation, fixed, and dehydrated. Samples were gold sputtered, and 20 images were taken at specified locations on the top of the disc (accounting for ~ 0.5% of the total area of the disc). A Representative images taken at 1500 × magnification. Per cent depicted is mean ± standard deviation. B Per cent coverage of each individual image. All green symbols were results from images acquired from disc #1, and the blue symbols were images acquired from disc #2 from each group. C Average biofilm coverage of all images taken per disc. ****p < 0.0001 and **p < 0.01
Discussion
With the increasing volumes of joint replacement surgeries globally, accompanied by persistent gaps in infection prevention strategies and the need for more effective treatments, addressing PJI has become an urgent priority in orthopaedic practice [19]. With high failure rates during PJI treatment, novel prophylactic treatments like antibacterial implant coatings are needed to decrease the risk of infection outside the perioperative window [20]. In this study, we have shown in vitro that DLC surface modification on titanium alloy can significantly decrease S. aureus biofilm coverage after 2 weeks of culture.
Applications for DLC coatings are appealing due to their mechanical, bio-inert, and antibacterial properties. DLC’s anti-wear and non-corrosive characteristics have the potential to lengthen the life of implants and decrease cellular reactivity to wear particles. Their use has been shown to be biologically inert, non-toxic towards osteoclasts, and promote bone mineralization in vitro providing rationale of its usefulness clinically without negative biological side effects. Of note, the previous reports on wear resistance with DLC and UHMWPE used an old formulation of UHMWPE where newer formulations have optimized its shortcoming and, therefore, do require additional testing with the new formulation to assess its wear resistance in combination [7].
Various ions can be supplemented during DLC coating manufacturing to increase antibacterial efficacy [11]. Both silver and copper nanoparticle-impregnated DLC leads to rapid release of silver and copper ions, respectively, leading to a reduction of both surface-bound and planktonic bacterial species in vitro via metabolism disturbance and membrane destabilization mechanisms [12, 21]. Fluorine-DLC and silicone-DLC coating creates a hydrophobic surface thus reduces the surface free energy and bacterial adhesion [11]. Zinc oxide nanoparticles embedded into DLC antibacterial coatings produce an adaptive release of Zn2+ ions when in an aqueous environment leading to acidosis and toxicity to Staphylococci species [22]. Titanium dioxide-doped DLC has bactericidal effects via oxidative damage to the cell wall and decreases the interfacial energy of bacterial adhesion in a dose-dependent manner [23].
Indeed, other implant coatings are also under investigation. Antifouling or antiadhesion coatings are being developed that focus on the surface hydrophilic/hydrophobic properties, conductivity, and surface energy. Polymers such as polyethylene glycol (PEG), zwitterionic polymers, hyaluronic acid (HA), and sodium alginate increase hydrophilicity and, therefore, decrease the binding sites for bacteria [11]. Zwitterionic polymers contain isoelectric characteristics that repel charged proteins and bacteria, and their quaternary ammonium salts such as phosphorous, pyridine, and imidazole also have antibacterial properties. Polysaccharides such as HA and sodium alginate inhibit bacterial adhesion through electrostatic repulsion interactions [11]. Topographic 3D nanostructures such as blunt nanopillars, spikes, and nanoedges have shown success where bacteria adhesion is disrupted, causing stress and rupture of the cell membrane [24]. Of note, this may not work on all bacteria with thicker cell membranes. Recently, a point-of-care antibiotic-loaded antimicrobial coating that is applied during surgery that couples PEG with poly(allyl mercaptan) (PEG-PAM) polymers prevented in vivo infection in both mouse models of arthroplasty and spine surgery without inhibiting osseointegration [25]. Hydrophobic coatings like fluorinated polymers produce a low surface energy coating that reduces interactions between bacteria and the surface [26]. Use of metal oxides such as TiO2, CuO, AgO, and ZnO that release reactive oxygen species upon irradiation and metal ion release can inhibit bacterial adhesion without affecting osteogenesis [14, 27]. Indeed, coatings using of immobilized silver ions on hydroxyapatite film on polymers have also shown bactericidal and anti-biofilm effects without high-temperature processing for coating application [28]. Of note, majority of the DLC composite literature has focused on antibacterial effects associated with metal ion mechanisms and have not explored composites with alternative bactericidal agents.
Addition of bactericidal agents to implant coatings is also another area of active research. In this case, adhered bacteria are destroyed via an active substance covalently linked or adsorbed in the coating including chitosan, antimicrobial peptides (AMPs), or quaternary ammonium compounds (QACs) [11]. A majority of AMPs and QACs are cationic and can rapidly penetrate the negatively charged bacterial cell membrane causing autolysis and cell death, efficiently killing bacteria regardless of antibiotic susceptibility with low toxicity [29,30,31]. Chitosan is a cationic polysaccharide where its positively charged amino groups generate electrostatic interactions with bacteria thus altering permeability of the cell wall and lysis [32]. Indeed, while this method directly kills bacteria, accumulation of dead bacteria and their intracellular products may potentially limit these coatings long term by forming a barrier between the surface and subsequent bacteria thus giving bacteria an opportunity to adhere and create a biofilm.
Controlled-release antibacterial agents in coatings have the potential to be used over an extended period post-implantation. These coatings can be carriers of antibacterial agent which can be released through diffusion or degradation including antibiotics, metal ions, fluorine, and iodine24. Additionally, these nanomaterials can be responsive to external stimuli including magnetic fields, light, or temperature creating a temporal effect when needed. Hydrogels, hydrophilic 3D polymeric structures, and polyelectrolyte multilayers (PEMs) are made with biologically relevant materials such as chitosan, collagen, and hyaluronic acid and can be loaded with various antibacterial agents that can be used as coatings on implant surfaces with sustained release of its load but still needs further characterization [31]. Nevertheless, additional characterization of the coating process needs to be investigated to ensure that the implant’s mechanical and osseointegrative integrity is still maintained.
This study is not without limitations. This pilot study had a small sample size of n = 2 per group and was completed in a single experiment. This study will need to be repeated to confirm reproducibility. This study only had a single timepoint for biofilm readout. Whether attachment and kinetics of biofilm growth is altered at earlier timepoints needs to be addressed. This study also used a higher CFU than would be required for infection seeding in clinical settings. Nevertheless, results did show a difference in biofilm coverage at this high CFU, suggesting that larger differences may be apparent with smaller inoculum. Additionally, these experiments were completed in static conditions and whether different results will be obtained under constant flow conditions needs to be investigated.
Conclusion
Although many studies have been published on DLC coating of metal implant materials in the context of joint arthroplasty, this is the first evidence showing that DLC surface treatment significantly decreases S. aureus biofilm coverage on titanium discs after 2 weeks of culture via systematic SEM analysis. Although its effect was not readily apparent via crystal violet analysis, its growth differences and seeding on the surface of the implant were apparent with SEM analysis. These data have warranted further investigation into the usefulness of DLC coating in orthopaedic implants to prevent PJI.
References
Patel R (2023) Periprosthetic Joint Infection. N Engl J Med 388:251–262. https://doi.org/10.1056/NEJMra2203477
Premkumar A, Kolin DA, Farley KX et al (2021) Projected economic burden of periprosthetic joint infection of the hip and knee in the United States. J Arthroplasty 36:1484-1489.e3. https://doi.org/10.1016/j.arth.2020.12.005
Zmistowski B, Parvizi J (2013) A quarter of patients treated for PJI dead within 5 years. Orthop. Today
Piuzzi NS, Klika AK, Lu Q et al (2024) Periprosthetic joint infection and immunity: current understanding of host-microbe interplay. J Orthop Res 42:7–20. https://doi.org/10.1002/jor.25723
Jackson LMD, Kroukamp O, Yeung WC et al (2019) Species interaction and selective carbon addition during antibiotic exposure enhances bacterial survival. Front Microbiol 10:2730. https://doi.org/10.3389/fmicb.2019.02730
Love CA, Cook RB, Harvey TJ et al (2013) Diamond like carbon coatings for potential application in biological implants - a review. Tribol Int 63:141–150. https://doi.org/10.1016/j.triboint.2012.09.006
Roy A, Bennett A, Pruitt L (2024) Feasibility of using diamond-like carbon films in total joint replacements: a review. J Mater Sci Mater Med 35:47. https://doi.org/10.1007/s10856-024-06814-x
Oate JI, Comin M, Braceras I et al (2001) Wear reduction effect on ultra-high-molecular-weight polyethylene by application of hard coatings and ion implanation on cobalt chromium ally, as measured in a knee wear simulation machine. Surf Coatings Technol 142–144:1056–1062. https://doi.org/10.1016/S0257-8972(01)01074-X
Rothammer B, Neusser K, Bartz M et al (2023) Evaluation of the wear-resistance of DLC-coated hard-on-soft pairings for biomedical applications. Wear 523:204728. https://doi.org/10.1016/j.wear.2023.204728
Saikko V, Ahlroos T, Calonius O, Keränen J (2001) Wear simulation of total hip prostheses with polyethylene against CoCr, alumina and diamond-like carbon. Biomaterials 22:1507–1514. https://doi.org/10.1016/S0142-9612(00)00306-9
Cumont A, Pitt AR, Lambert PA et al (2021) Properties, mechanism and applications of diamond as an antibacterial material. Funct Diam 1:1–28. https://doi.org/10.1080/26941112.2020.1869434
Birkett M, Zia AW, Devarajan DK et al (2023) Multi-functional bioactive silver- and copper-doped diamond-like carbon coatings for medical implants. Acta Biomater 167:54–68. https://doi.org/10.1016/j.actbio.2023.06.037
Swiatek L, Olejnik A, Grabarczyk J et al (2016) Multi-doped diamond like-carbon coatings (DLC-Si/Ag) for biomedical applications fabricated using the modified chemical vapour deposition method. Diam Relat Mater 67:54–62. https://doi.org/10.1016/j.diamond.2016.03.005
Travnickova M, Filova E, Slepicka P et al (2024) Titanium-doped diamond-like carbon layers as a promising coating for joint replacements supporting osteogenic differentiation of mesenchymal stem cells. Int J Mol Sci 25:2837. https://doi.org/10.3390/ijms25052837
Kuwada N, Fujii Y, Nakatani T et al (2023) Diamond-like carbon coating to inner surface of polyurethane tube reduces Staphylococcus aureus bacterial adhesion and biofilm formation. J Artif Organs. https://doi.org/10.1007/s10047-023-01403-1
Harrasser N, Jüssen S, Obermeir A et al (2016) Antibacterial potency of different deposition methods of silver and copper containing diamond-like carbon coated polyethylene. Biomater Res 20:17. https://doi.org/10.1186/s40824-016-0062-6
Juknius T, Ružauskas M, Tamulevičius T et al (2016) Antimicrobial properties of diamond-like carbon/silver nanocomposite thin films deposited on textiles: towards smart bandages. Materials (Basel) 9:371. https://doi.org/10.3390/ma9050371
Visperas A, Santana D, Ju M et al (2022) Standardized quantification of biofilm in a novel rabbit model of periprosthetic joint infection. J bone Jt Infect 7:91–99. https://doi.org/10.5194/jbji-7-91-2022
Siddiqi A, Warren JA, Manrique-Succar J et al (2021) Temporal trends in revision total hip and knee arthroplasty from 2008 to 2018: gaps and opportunities. J Bone Joint Surg Am 103:1335–1354. https://doi.org/10.2106/JBJS.20.01184
Shichman I, Ward SA, Lu L et al (2023) Failed 2-stage revision knee arthroplasty for periprosthetic joint infection—patient characteristics and outcomes. J Arthroplasty. https://doi.org/10.1016/j.arth.2023.04.063
Gorzelanny C, Kmeth R, Obermeier A et al (2016) Silver nanoparticle-enriched diamond-like carbon implant modification as a mammalian cell compatible surface with antimicrobial properties. Sci Rep 6:22849. https://doi.org/10.1038/srep22849
Buchegger S, Kamenac A, Fuchs S et al (2019) Smart antimicrobial efficacy employing pH-sensitive ZnO-doped diamond-like carbon coatings. Sci Rep 9:17246. https://doi.org/10.1038/s41598-019-53521-7
Marciano FR, Lima-Oliveira DA, Da-Silva NS et al (2009) Antibacterial activity of DLC films containing TiO2 nanoparticles. J Colloid Interface Sci 340:87–92. https://doi.org/10.1016/j.jcis.2009.08.024
Wu Z, Chan B, Low J et al (2022) Microbial resistance to nanotechnologies: an important but understudied consideration using antimicrobial nanotechnologies in orthopaedic implants. Bioact Mater 16:249–270. https://doi.org/10.1016/j.bioactmat.2022.02.014
Xi W, Hegde V, Zoller SD et al (2021) Point-of-care antimicrobial coating protects orthopaedic implants from bacterial challenge. Nat Commun 12:5473. https://doi.org/10.1038/s41467-021-25383-z
Wang J, Sun J, Zhou J et al (2017) Fluorinated and thermo-cross-linked polyhedral oligomeric silsesquioxanes: new organic-inorganic hybrid materials for high-performance dielectric application. ACS Appl Mater Interface 9:12782–12790. https://doi.org/10.1021/acsami.7b01415
Shirai R, Miura T, Yoshida A et al (2016) Antimicrobial effect of titanium dioxide after ultraviolet irradiation against periodontal pathogen. Dent Mater J 35:511–516. https://doi.org/10.4012/dmj.2015-406
Ishihama H, Ishii K, Nagai S et al (2021) An antibacterial coated polymer prevents biofilm formation and implant-associated infection. Sci Rep 11:3602. https://doi.org/10.1038/s41598-021-82992-w
Melo MN, Ferre R, Castanho MARB (2009) Antimicrobial peptides: Linking partition, activity and high membrane-bound concentrations. Nat Rev Microbiol 7:245–250. https://doi.org/10.1038/nrmicro2095
Ahlstrom B, Thompson R, Edebo L (1999) The effect of hydrocarbon chain length, pH, and temperature on the binding and bactericidal effect of amphiphilic betaine esters on Salmonella tvphimurium. APMIS 107:318–324. https://doi.org/10.1111/j.1699-0463.1999.tb01560.x
Akay S, Yaghmur A (2024) Recent advances in antibacterial coatings to combat orthopedic implant-associated infections. Molecules 29:1172. https://doi.org/10.3390/molecules29051172
Hu X, Neoh KG, Shi Z et al (2010) An in vitro assessment of titanium functionalized with polysaccharides conjugated with vascular endothelial growth factor for enhanced osseointegration and inhibition of bacterial adhesion. Biomaterials 31:8854–8863. https://doi.org/10.1016/j.biomaterials.2010.08.006
Funding
Financial Interests: This research study was funded by Signature Orthopaedics. Nicolas Piuzzi has received research support from Signature Orthopaedics, Osteal Therapeutics, Peptilogics, Regenlab, and Zimmer, and is a paid consultant for Pacira and Stryker. All other authors have no financial interests. Non-financial Interests: Nicolas Piuzzi is a board or committee member of the American Association of Hip and Knee Surgeons, International Society for Cell & Gene Therapy, and Orthopaedic Research Society, and on the editorial board/governing board of Journal of Hip Surgery and Journal of Knee Surgery. All other authors have no non-financial interests.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Anna Cristina Samia and Nicolas S. Piuzzi are co-senior authors on this manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Visperas, A., Cui, K., Alam, M.M. et al. Diamond-like carbon (DLC) surface treatment decreases biofilm burden by S. aureus on titanium alloy in vitro— a pilot study. Eur J Orthop Surg Traumatol (2024). https://doi.org/10.1007/s00590-024-04093-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00590-024-04093-4