Abstract
Background
We established a method in which patients are instructed before total knee arthroplasty (TKA) in a differentiated way without the necessity of reading any self-orientation, which can be applied even for illiterate patients
Methods
We developed a multidisciplinary approach to improve patient education in TKA comprising of a differentiated orientation conducted by an orthopedic surgeon, a nurse and a physiotherapist. It consists of standardized lectures regarding on pre-, intra- and postoperative issues in a randomized controlled trial of 79 consecutive patients undergoing primary TKA. Thirty-four patients received the standard education (control group), and 45 patients received the differentiated education (intervention group). The patients were evaluated during at least 6 months.
Results
After a 6-month follow-up period, the Short Form Health Survey (SF-36), the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), the visual analogue pain scale (VAS) and knee range of motion (ROM) improved significantly in both groups. Range of motion was better in the intervention group (mean and SD—106.9 ± 5.7 versus 92.5 ± 12.1 degrees, p = 0.02). Moreover, walk ability (more than 400 m) was better in the intervention group compared with the control group (97.4% versus 72.4%, p = 0.003). In the intervention and control groups, respectively, 10.5% and 31% of patients reported the need for some walking devices (p = 0.03).
Conclusions
A differentiated educational program with a multidisciplinary team had a positive impact on functional outcomes, improving ROM and walk ability of patients undergoing TKA in a short-term evaluation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Osteoarthritis (OA) is a chronic and potentially disabling condition related to complex etiology. Its incidence has increased in the last few years, mainly due to population aging and an increased rate of obesity and sports injuries [1,2,3]. Imbalance between anabolic and catabolic pathways usually leads to gradual cartilage damage [3]. During this process, patients might experience functional impairment, pain and mechanical symptoms, which can impact their quality of life [4].
The knee is the second joint most affected by OA, i.e., approximately 37% of all patients seek medical assistance [5]. Moreover, social and mental distress can be related to knee OA, impacting outcome negatively [6]. Usually surgical treatment is recommended when conservative measures have failed [5]. Total knee arthroplasty (TKA) has proved to be a successful treatment with predictable results [7,8,9]. However, up to 20% of patients after their TKA complain of residual pain, functional impairment or subjective dissatisfaction [9]. Mismatch between medical and patient expectations is one of the possible causes leading to dissatisfaction after TKA. Therefore, educating patients about the disease and the treatment process is an important measure in health assistance.
Patient education refers to any intervention delivered during health assistance which aims to improve knowledge, health behaviors and health outcomes. As patients often forget verbal orientation, written and illustrated materials are effective in maximizing knowledge and adhesion to treatment. However, there are some patients in public hospitals who are illiterate, which hinders this process. The recommended content of education varies across settings, but should comprise of discussion about preoperative procedures, important surgical points, postoperative care, potential stressful scenarios, potential complications, pain management, discharge criteria and also postoperative rehabilitation [10]. Although this preoperative education seems obvious and embedded in the consent process, recent data questioned its efficacy to improve postoperative functional scores [11]. Moreover, when treating illiterate patients, a reinforced educational approach should be applied.
Our hypothesis is that a new educational preoperative approach would improve the TKA results. The purpose of this study is to compare the clinical outcomes for two groups of patients who received different educational approaches before TKA. The groups were compared for function and clinical data.
Methods
A prospective randomized clinical trial was conducted from November 2017 to July 2018. An institutional review board approval from the Ethics Committee of the Universidade Federal de Minas Gerais was obtained for our research protocol to prospective data acquisition (CAAE:11,677,714.4.0000.5149), and an informed consent was signed by all the participants or one person responsible for them.
The sample size was calculated to test the hypothesis that a differentiated education would increase postoperative range of motion (ROM) of the knee joint (primary outcome). Trying to detect a difference of 10 degrees in ROM of the knee joint between groups and based on a power test of 80% and a confidence interval of 5% after assuming a possible 10% lost in follow-up, 15 patients in each group were considered the minimum number of participants.
Secondary outcomes were:
-
The Short Form Health Survey (SF-36), which includes questions about patients’ general health
-
The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC)—results range from 0 to 96. It evaluates pain intensity (0–20), stiffness (0–8) and function (0–68)
-
The visual analogue pain scale (VAS)—ranging from 0 to 10
-
The distance the patients were able to walk and in the last follow-up if they were able to walk 400 m or more
-
The capacity to climb and descend stairs.
All variables were collected in the preoperative appointment which occurred at least 2 weeks before surgery and in the postoperative evaluations.
Inclusion criteria: patients with unilateral symptomatic primary or secondary OA of the knee, older than 45 years, with indication of a primary TKA, who signed the informed consent form. Randomization, clinical examination and functional tests were applied to all participants by two investigators (DGKB, DSL).
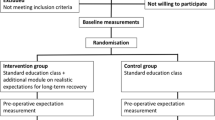
Patients were then randomized into two groups: differentiated orientation or usual orientation. Randomization comprised choosing one of the 100 closed opaque envelopes, 50 of them with the word “usual” and 50 with the word “differentiated,” referring to the approach it would be done. As we had planned 8 months to stop randomization, and considering that 15 patients in each group were considered sufficient to answer the question of the study, we had at that point:
Intervention group (45 patients): after medical appointment, patients received a new multidisciplinary reinforced orientation that included scheduled sessions of lectures done by an orthopedic surgeon, a nurse and a physiotherapist concerning the pre- and postoperative care, pain management, rehabilitation exercises to gain ROM, the basic steps of the surgical procedure and the importance of walking with a walker. This intervention was done 2 weeks before surgery during office consultation. Patients were invited to attend a collective oral session, which included a standardized sequence of slides and images regarding the preoperative preparation, the procedure itself and the rehabilitation with 1) a 15-min lecture done by a nurse, 2) a 15-min lecture done by a physiotherapist and 3) a 15-min lecture done by an orthopedic surgeon, followed by additional time for patients to ask questions. Researchers also provided a phone contact number in case patients had further questions. The cost of this intervention method is low, which turns it feasible to be applied more widely (Fig. 1).
Control group (34 patients): patients were oriented during conventional medical appointments, in which any doubts were clarified. A phone contact of researchers was provided for the patients.
The difference in the number of participants between groups was due to the study closure before 50 patients in each group were reached, considering that the minimal number to confirm our hypothesis was 15 patients.
The postoperative clinical and functional evaluation was performed by three blinded investigators (MVTR, TFGM, FSM). The study was conducted at the Orthopaedic Department of the Federal University of Minas Gerais—Brazil.
Seventy-nine patients were eligible for the study. Twelve were excluded during follow-up—5 in the control group and 7 in the intervention group: one patient died (myocardial infarction), three patients had periprosthetic joint infection and eight did not return for control and were excluded. After exclusions, the control group and the intervention group remained with 29 and 38 patients, respectively (Fig. 2).
All patients were operated on in the same Institution by three different surgeons (MAPA, GMAS, TVOC) who followed the same protocol. Patients received a peridural anesthesia with bupivacaine (0,5%) and intravenous sedation (Diprivan® AstraZeneca). Tourniquet was applied in all cases set to 300 mmHg. Primary TKA was performed through a classical medial arthrotomy with patellar eversion. A cruciate retained implant (Nexgen® Zimmer—Warsaw, IN), with patellar substitution, fixed with a non-impregnated antibiotic cement was used in all cases. Postoperative multimodal pain control protocol was made in both groups and started on the same day of the procedure. It consisted of scheduled 1) acetaminophen 133 mg every 6 h, 2) metamizole 500 mg every 6 h, 3) tramadol 50 mg every 8 h for 24 h and 4) morphine 2 to 6 mg every 4 h, as needed. Patients were encouraged to start early ROM and weight bearing with a walker on the first day. Patients were discharged from hospital on day 2 or 3 and were evaluated in 15 days, 1 month, 3 months and 6 months after surgery, and in each session, the scores and the VAS were applied, ROM was evaluated with a calibrated goniometer, and specific questions such as the use of walker or cane, their ability in climbing or descending stairs and the distance they were able to walk were asked.
Statistical analysis was performed to determine statistically significant differences between the 2 groups (p < 0.05), using appropriate software (G*Power Version 3.1.9.2) and included analysis of distribution by Kolmogorov–Smirnov test. Independent t test was used to analyze numerical, continuous and normally distributed variables. Qui-square test was used for categorical data. No crossover was observed, so intention-to-treat analysis was not performed.
Results
The two groups were comparable on demographics, clinical and functional tests (Table 1). After a 6-month follow-up period, VAS, WOMAC and SF-36 scores significantly improved in both groups, and no difference was observed between groups. Knee range of motion was higher in the intervention group (mean flexion 106.9 ± 5.7 versus 92.5 ± 12.1°, p = 0.02). Moreover, at 6 months, 97.4% of patients in the intervention group and 72.4% of patients in the control groups reported an improvement in their ability to walk more than 400 m after surgery (p = 0.003). At 6-month follow-up-period, walk assistance was needed in 10.5% of the patients in the intervention group and in 31% in the control group (p = 0.03) (Table 2). No significant missing data were observed during this short-term study.
Discussion
This study showed that additional education improves functional results after TKA. Studied parameters were applied differently to both groups with no additional costs. The same infrastructure and health team was utilized in the intervention method. As a result of this intervention, patients who received a reinforced orientation protocol achieved better ROM and could walk more frequently without assistance. Regarding postoperative functional scores and pain, no difference was observed between groups.
Achieving good results after total knee replacement depends on many factors, such as patient selection, implant design, surgical technique and postoperative care [12]. However, more than 20% of patients can still have some dissatisfaction after the procedure [13, 14]. It is well known that ROM has correlation with better functional scores after TKA [15].
Biomechanical studies showed that patients require at least 83° of flexion to climb stairs, 100° to descend stairs and 67° to walk normally [16]. Ritter et al. [15] observed worse functional outcomes in patients with less than 118 degrees of flexion. Kotani et al. [17] noted that more than 110° of knee flexion would improve daily living activities. Thereby, a method that could help improving range of motion might favorably impact TKA outcomes.
On the other hand, the role of patient education was questioned due to low-quality evidence of available data [11], but these findings do not invalidate its use and the present study confirms its importance.
ROM evaluation as an independent predictor in TKA had not been clearly studied. Two studies depicted no difference in ROM between oriented and non-oriented patients after hip replacement [18, 19]. Our study shows that a new reinforced education with a team approach improved ROM when compared to the traditional orientation method. This reinforced education would avoid oversights during orientation by improving the understanding of the patient about the procedure. Al-Rub et al. [20] in a cohort study showed that 85% of patients did not know the composition of the implant and only 39% of patients had received advice about dental work after arthroplasty. Educating patients before surgery leads to decreased anxiety, which can be expressed by better ROM and walk ability after surgery [21]. Our method may be applied on illiterate patients with a positive effect. Ayers et al. [22] showed that more than 30% of patients going through TKA have depression or anxiety symptoms, which can be minimized by better orientation. Illiteracy is still highly predominant in developing countries, and therefore, booklets do not prove very effective. The proposed new approach is easy to apply, has low cost and leads to positive outcomes.
There are limitations in this study, and a follow-up evaluation for a short period of time (6 months) can be considered a point of weakness. However, ROM and walk capacity after 6 months can clearly predict long-term results [23, 24]. Subsequently, function improvement is less likely without some medical intervention (manipulation under anesthesia, arthrolysis or revision) [25].
Conclusion
After a mean 6-month period, a new reinforced orientation method comprising multidisciplinary oral presentations with instructional lectures improved the final ROM and also the walking capacity after TKA. This method can be applied even to illiterate patients.
Trial registration
This study adheres to CONSORT guidelines Trial registration: ReBEC (Registro Brasileiro de Ensaios Clínicos) RBR-588cfq Retrospectively registered on 03/06/2020. Trial URL: http://www.ensaiosclinicos.gov.br/rg/RBR-588cfq/.
Availability of data and materials
Abbreviations
- TKA:
-
Total knee arthroplasty
- SF-36:
-
Medical Study 36-item Short-Form Health Survey
- WOMAC:
-
Western Ontario and McMaster Universities Osteoarthritis Index
- ROM:
-
Range of motion
- OA:
-
Osteoarthritis
- VAS:
-
Visual analog scale
References
Buckwalter JA (1995) Osteoarthritis and articular cartilage use, disuse, and abuse: experimental studies. J Rheumatol Suppl 43:13–15
Neogi T, Zhang Y (2013) Epidemiology of osteoarthritis. Rheum Dis Clin North Am 39(1):1–19
Murphy L, Schwartz TA, Helmick CG, Renner JB, Tudor G, Koch G et al (2008) Lifetime risk of symptomatic knee osteoarthritis. Arthritis Rheum 59(9):1207–1213
Arden N, Nevitt MC (2006) Osteoarthritis: epidemiology. Best Pract Res Clin Rheumatol 20(1):3–25
Senna ER, De Barros AL, Silva EO, Costa IF, Pereira LV, Ciconelli RM et al (2004) Prevalence of rheumatic diseases in Brazil: a study using the COPCORD approach. J Rheumatol 31(3):594–597
Utrillas-Compaired A, De la Torre-Escuredo BJ, Tebar-Martínez AJ, Asúnsolo-Del BÁ (2014) Does preoperative psychologic distress influence pain, function, and quality of life after TKA? Clin Orthop Relat Res 472(8):2457–2465
Pagnano MW, McLamb LA, Trousdale RT (2004) Total knee arthroplasty for patients 90 years of age and older. Clin Orthop Relat Res 418:179–183
Ethgen O, Bruyère O, Richy F, Dardennes C, Reginster JY (2004) Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am. 86(A5):963–974
Shan L, Shan B, Suzuki A, Nouh F, Saxena A (2015) Intermediate and long-term quality of life after total knee replacement: a systematic review and meta-analysis. J Bone Joint Surg Am 97(2):156–168
Louw A, Diener I, Butler DS, Puentedura EJ (2013) Preoperative education addressing postoperative pain in total joint arthroplasty: review of content and educational delivery methods. Physiother Theory Pract 29(3):175–194
McDonald S, Page MJ, Beringer K, Wasiak J, Sprowson A (2014) Preoperative education for hip or knee replacement. Cochrane Database Syst Rev. 5:CD 003526
Sanz-Ruiz P, Carbo-Laso E, Alonso-Polo B, Matas-Diez JA, Vaquero-Martín J (2016) Does a new implant design with more physiological kinematics provide better results after knee arthroplasty? Knee 23:399–405
Noble PC, Conditt MA, Cook KF, Mathis KB (2006) The John Insall Award: Patient expectations affect satisfaction with total knee arthroplasty. Clin Orthop Relat Res 452:35–43
Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD (2010) Patient satisfaction after total knee arthroplasty: Who is satisfied and who is not? Clin Orthop Relat Res 468(1):57–63
Ritter MA, Lutgring JD, Davis KE, Berend ME (2008) The effect of postoperative range of motion on functional activities after posterior cruciate-retaining total knee arthroplasty. J Bone Joint Surg Am 90(4):777–784
Laubenthal KN, Smidt GL, Kettelkamp DB (1972) A quantitative analysis of knee motion during activities of daily living. Phys Ther 52(1):34–43
Kotani A, Yonekura A, Bourne RB (2005) Factors influencing range of motion after contemporary total knee arthroplasty. J Arthroplasty 20(7):850–856
Gocen Z, Sen A, Unver B, Karatosun V, Gunal I (2004) The effect of preoperative physiotherapy and education on the outcome of total hip replacement: a prospective randomized controlled trial. Clin Rehabil 18(4):353–358
Vukomanović A, Popović Z, Durović A, Krstić L (2008) The effects of short-term preoperative physical therapy and education on early functional recovery of patients younger than 70 undergoing total hip arthroplasty. Vojnosanit Pregl 65(4):291–297
Abu Al-Rub Z, Hussaini M, Gerrand CH (2014) What do patients know about their joint replacement implants? Scott Med J 59(3):158–161
Demir F, Ozsaker E, Ilce AO (2008) The quality and suitability of written educational materials for patients*. J Clin Nurs 17(2):259–265
Ayers DC, Franklin PD, Trief PM, Ploutz-Snyder R, Freund D (2004) Psychological attributes of preoperative total joint replacement patients: implications for optimal physical outcome. J Arthroplasty 19(7 Suppl 2):125–130
Nilsdotter AK, Toksvig-Larsen S, Roos EM (2009) A 5 year prospective study of patient-relevant outcomes after total knee replacement. Osteoarthritis Cartilage 17(5):601–606
Papakostidou I, Dailiana ZH, Papapolychroniou T, Liaropoulos L, Zintzaras E, Karachalios TS et al (2012) Factors affecting the quality of life after total knee arthroplasties: a prospective study. BMC Musculoskelet Disord 13:116
Fitzgerald JD, Orav EJ, Lee TH, Marcantonio ER, Poss R, Goldman L et al (2004) Patient quality of life during the 12 months following joint replacement surgery. Arthritis Rheum 51(1):100–109
Acknowledgements
No further acknowledgements.
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
MAPA conceptualized the study and design. DGKB, DSL, MVTR, TFGM and FSM recruited the participants and collected the data. MAPA, GMAS and TVOC prepared the first draft of the manuscript and all authors contributed to writing, as well as review and approval of the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest regarding this research.
Ethics approval and consent to participate
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments. The consent obtained from study participants was written and approved by the Ethics Committee. An institutional review board approval from the Ethics Committee of the Universidade Federal de Minas Gerais was obtained for our research protocol to prospective data acquisition of 39 (79) patients undergoing TKA (CAAE:11677714.4.0000.5149), and an informed consent was signed by all the participants or one person responsible for them.
Consent for publication
Not Applicable.
Competing interests
Authors declare that they do not have any financial and non-financial competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Percope de Andrade, M.A., Moreira de Abreu Silva, G., de Oliveira Campos, T.V. et al. A new methodology for patient education in total knee arthroplasty: a randomized controlled trial. Eur J Orthop Surg Traumatol 32, 107–112 (2022). https://doi.org/10.1007/s00590-021-02936-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-021-02936-y