Abstract
Background
Trapeziectomy with ligament reconstruction and tendon interposition (LRTI) is currently the most popular technique for treating primary osteoarthritis of the thumb carpometacarpal joint. However, reduced trapezial height has sometimes been reported after LRTI. Longer immobilization and delayed rehabilitation times are also problematic. In this study, we evaluated the clinical and radiological outcomes of patients who underwent our modified LRTI procedure.
Methods
Retrospective study included 26 thumbs in 24 cases with advanced stages. Our modified Burton’s procedure was as follows: (1) trapeziectomy was limited to distal-half, (2) the entire flexor carpi radialis (FCR) was harvested from the forearm, and (3) half-slip of the FCR tendon was stabilized by interference screw in the first metacarpal bone tunnel.
Results
Pain on the visual analogue scale (VAS), the quick Disabilities of the Arm Shoulder and Hand score, tip pinch strength significantly improved postoperatively. The preoperative height of the trapezial space was well-maintained at final follow-up. Magnetic resonance imaging at the one-year follow-up showed the existence of FCR tendon ball in 15 cases. Eighteen housewives resumed their daily activities after a mean period of 10 days postoperative, while another 6 patients returned to their original jobs after 3 weeks.
Conclusions
Our modified LRTI method involves distal-half trapeziectomy and entire FCR interposition. A sewn FCR tendon ball always provide enough volume to fill the trapeziectomy space, which helps to prevent sinking of the metacarpal bone. Our technique produced sufficient ligamentoplasty and allowed early mobilization after surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The thumb carpometacarpal (CMC) joint is the second most common site of osteoarthritis in the hand after the distal interphangeal joint. It is also the most common surgical site for arthroplasty or arthrodesis [21]. The purpose of treatment for CMC arthritis is to reduce pain and to preserve functionality of the thumb. Patients with Eaton stage II to IV [5, 12] CMC arthritis are considered for surgery if conservative treatments have failed.
Simple trapeziectomy was first introduced by Gervis in 1949 [9]. Since then numerous other procedures have also been proposed [11, 22]. The first suspension arthroplasty of the thumb CMC joint was reported by Eaton et al. [6] Of the available procedures, such as abductor pollicis longus suspensionplasty or suture-button suspensionplasty [19, 23], trapeziectomy with ligament reconstruction and tendon interposition (LRTI) is currently the most popular technique. Burton et al. introduced LRTI in 1986 [2] as a modification of Eaton’s procedure. It is generally believed that ligament reconstruction confers greater joint stability and addresses anatomical problems inherent to CMC osteoarthritis, while fibrous tendon interposition preserves the trapezial height postoperatively [24]. However, reduced trapezial height has sometimes been reported after LRTI [4, 18]. Longer immobilization and delayed rehabilitation times are also problematic, especially in highly demanding patients. Previous studies suggest that maintenance of the arthroplasty space between the thumb metacarpal and the scaphoid may positively influence the functional outcome [21].
In an attempt to resolve the above issues with LRTI, we modified Burton’s procedure as follows: (1) trapeziectomy was limited to distal-half, (2) the entire flexor carpi radialis (FCR) was harvested from the forearm, and (3) half-slip of the FCR tendon was stabilized by interference screw in the first metacarpal bone tunnel. (Table 1) The purpose of this study was thus to evaluate the clinical and radiological outcomes of patients who underwent our modified LRTI procedure. We also discuss the results from early postoperative rehabilitation.
Patients and methods
Ethics statement
This study was approved by the ethics committee of the General Hospital.
Patients
Consecutive female patients between 2012 and 2018 who had failed to respond to conservative treatments at least for three months for advanced thumb CMC joint osteoarthritis were included in this study. There was 26 thumbs in 24 cases, with 12 thumbs in the dominant hand and 14 in the non-dominant hand. The mean patient age was 67 years (range, 50–87 years), and all cases were classified as Eaton stage 3. Surgical treatment was allowed in healthy elderly patients in good medical condition. The mean follow-up period was 20 months and ranged from 12 to 48 months.
Surgical technique and postoperative rehabilitation
All procedures were performed under general anesthesia by one surgeon (K.M.) and were completed within one air tourniquet time. The trapeziometacarpal joint was exposed through a longitudinal incision between the extensor pollicis brevis and longus tendons. (Fig. 1) The capsule and periosteum were sharply dissected as far as possible. The superficial branch of the radial nerve was carefully protected. The distal half of the trapezium was resected using a microbone saw and small rongeur. Under image intensifier, the direction of osteotomy was confirmed to be parallel to the scaphotrapezial joint.
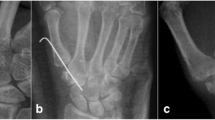
The FCR tendon can be identified in the trapezial void with traction of the thumb. Approximately, 8–10 cm of FCR tendon was harvested from the forearm using a tendon stripper. An oblique bone canal was created in the first metacarpal base with a 3.2 mm bar. The canal began dorsoradially at a distance of 1 cm from the metacarpal base and ran in a palmer-ulnar direction to the center of the articular surface of the metacarpal base. One half of the FCR was routed into the canal. (Fig. 2) With gentle traction applied to the thumb, the first and second metacarpal bone was temporarily stabilized by a 1.2-mm Kirschner wire. The tendon strip was fixed by impacting cancellous bone harvested from the distal half of the trapezium and inserting a metal interference screw (T J screw; MEIRA Corporation, Japan). (Fig. 3) The diameter of the screw was 5 or 7 mm. The remaining tendon and another half split were rolled up and placed into the trapezial void to act as a spacer. (Fig. 4a, b) The joint capsule was tightly closed to prevent displacement of the tendon ball.
Following surgery, the operated thumb was protected by a small made-to-order splint. (Fig. 5) The Kirschner wire was removed after 1 week and active range-of-motion exercise was started. Patients were allowed to return to their original jobs three weeks postoperatively. The splint was used for up to 4 weeks in total after operation.
Evaluation
Outcomes were assessed using visual analog scale (VAS), quick Disabilities of the Arm Shoulder and Hand (DASH), and tip pinch power using a Baseline dynamometer. For radiologic evaluation, the height of trapezial space was estimated. CMC space in the anteroposterior view was measured as the distance between the base of the metacarpal and the distal scaphoid. (Fig. 6a) This was measured preoperatively, one week after operation (following removal of temporary fixation) and one year after operation. (Fig. 6b) At one-year follow-up, the existence and position of FCR tendon ball was investigated by magnetic resonance imaging (MRI) in 15 cases who accepted the evaluation plan.
Measurement of CMC space in the anteroposterior view. A line is projected the articular surface of the base of the first metacarpal and another parallel line is the distal scaphoid. The distance of these two lines is measured as height of the trapezial space. a Before operation. b 1 year after operation
All statistical analyses were carried out using Student t test. Significance was set at p < 0.05.
Results
Clinical outcome
Pain on the VAS in activity of daily living was significantly improved with a mean preoperative score of 7.5 (7–9) compared to 1.8 (0–5) postoperatively. The quick DASH score also showed significant improvement, with a mean of 44 points preoperatively compared to 13 postoperatively. Tip pinch strength also significantly improved from 3.1 kg preoperatively to 5.1 kg postoperatively and equal to the contralateral side. In three cases, the improvement in VAS was less than 25% and the result judged to be fair. Neither ulnar deviation of the wrist nor metacarpophalangeal joint hyperextension were observed before operation and following our procedure. (Table 2).
Image evaluation
At the final follow-up, dorsoradial subluxation had been corrected in all cases. Except for the three cases scored as fair, the preoperative height of the trapezial space (mean 10.8 mm) was well-maintained at 1 week (13.3 mm) and at final follow-up (10.5 mm). (Table 2) The three fair cases showed sinking of the metacarpal base to 5 mm postoperatively. Impingement between the first and second metacarpal base was not observed in any of the cases. Back-out of the metal inference screw and scaphotrapezium joint arthritis were not observed in any of the cases at final follow-up.
MRI was performed in 15 cases at the one-year follow-up. All showed a mass in the trapezial space with low signal density in both T1 and T2 weighted image. These findings indicate the existence of fibrous tissue, probably representing FCR tendon ball. (Fig. 7).
Return to daily activity
Eighteen housewives resumed their daily activities after a mean period of 10 days postoperative, while another six patients returned to their original jobs (nurse, desk work etc.) after a mean period of 3 weeks following the procedure.
Discussion
Subjective outcomes achieved following arthroplasty procedures for thumb CMC arthritis have proven mostly satisfactory [15, 21]. Preservation of trapezial height is widely thought to be important for thumb strength [4, 18]. However, recent studies failed to show a correlation between thumb key and tip strengths and the height of the pseudoarthrosis formed after trapeziectomy alone, or even with the addition of tendon interposition [3, 7, 13, 15]. Based on our study, we propose that the ideal arthroplasty for advanced thumb CMC arthritis includes: (1) appropriate alignment, stability and movability; (2) maintenance of original thumb length; (3) a minimum period of thumb immobilization and early return to original daily activity.
Partial trapeziectomy
Several technical variations of LRTI have been described in the literature [13, 22, 24]. The original LRTI procedure involved total excision of the trapezium, which results in good pain relief but also in substantial loss of thumb strength and stability [1]. Partial distal-half trapeziectomy allows the remaining trapezium to act as a spacer and buttress and to address only the arthritic joint space [8]. In theory, this would improve stability and thumb strength and lead to less proximal migration of the thumb ray.
Our study patients were all classified as Eaton’s stage III [5, 12]. Because the scapho-trapezial joints showed no osteoarthritic changes, proximal half trapeziectomy was deemed not necessary. None of the cases showed progression of osteoarthritis in the scapho-trapezial joint following distal half trapeziectomy and tendon interposition. If patients had concomitant scapho-trapezial joint arthritis (Eaton’s stage IV), our procedure may be not indicated. A disadvantage of distal half trapeziectomy is that it is technically demanding. The FCR tendon can be difficult to find and may sometimes be injured. We always use an image intensifier to check the osteotomy line and depth before use of the bone saw during operation.
Sinking of the first metacarpal and harvesting the entire FCR tendon
Metacarpal sinking following trapeziectomy has always been a complication when treating thumb CMC arthritis [4, 10, 18]. Reduced trapezial height has been reported even after LRTI. Kriegs-Au et al. [13] compared ligament reconstruction using a half-slip of FCR tendon with or without tendon interposition procedures following entire trapezium excision. In total, 52 thumbs in 43 patients were randomized to undergo either of the two procedures. They concluded that proximal migration occurred in both groups but was significantly more frequent in the group without tendon interposition.
Suggested reasons for metacarpal sinking include volume loss, i.e., the entire trapezial space cannot be completely filled with a half-slip of FCR tendon ball. Another possible reason is insufficient ligamentoplasty, i.e., fixation of FCR is not secured in the metacarpal tunnel. Use of the entire FCR tendon seems the better option with respect to filling the volume of trapezial space. Moreover, harvesting of the entire FCR compared to just half did not result in increased morbidity in terms of wrist strength [16, 17]. Wang et al. described a similar modified LRTI procedure to ours [22]. The authors resected whole trapezium and harvested the entire FCR tendon. One-half of the FCR tendon was passed through the metacarpal canal and tied to another half FCR tendon. These authors did not observe any reduction in the height of the trapezial space. The wrist flexion strength weakened slightly from 20.5 to 19.7 kg after harvesting the entire FCR, but this difference was not statistically significant. Naidu et al. [17], Tomaino and Coleman [20], and Marenghi et al. [16] also described the use of entire FCR tendon harvest for thumb LRTI. Their findings showed neither subjective nor objective impairment of wrist motion, with the flexion strength returning almost to baseline. From these reports it appears that harvesting of entire FCR tendon produces no noticeable morbidity to wrist function.
Werthel et al. [24] also used entire FCR tendon for the LRTI procedure. The tendon was passed through the osseous tunnel at the bottom of the first metacarpal. The remaining tendon was inserted into the space created by complete trapezium resection. They operated on 49 thumbs in 43 patients and concluded the dorsoradial subluxation could be corrected in all cases. However, passage and fixation of the entire FCR through the bone tunnel made at the base of the first metacarpal seems very difficult in light of the variation in FCR tendon width between patients.
Our modified LRTI method involves distal-half trapeziectomy and entire FCR interposition. A sewn FCR tendon ball is always more bulky than the space created in the trapeziectomy void. This helps to retain the height of the trapezial space and to prevent sinking of the metacarpal bone. To our knowledge, there have been no studies to date on the fate of the FCR tendon ball after LRTI. From our MRI investigation, the FCR tendon ball remained within the trapezial space and showed low signal intensity in both T1 and T2 weighted image. However, three cases showed a lowered trapezial height after LRTI. We hypothesized the FCR tendon balls were dislodged from the space because of unmatched bulky volume. Tight and careful closing of the capsule and soft tissue over the trapezial space is necessary to prevent this possible complication.
Use of interference screw and early mobilization after LRTI
Postoperative rehabilitation is an important component for the success of this procedure. Longer immobilization after LRTI can delay the return to original activities of the patient. In theory, superior tendon graft fixation strength allows early mobilization. Kreigs-Au et al. [14] described the LRTI procedure in detail. They sutured the end of the tendon strip to the periosteum at the base of the first metacarpal. Kreigs-Au et al. [14] and most other authors immobilized the operated thumb by short arm thumb-spica cast for 5–6 weeks. Active range-of-motion and thenar muscle strengthening exercises are started after removal of the cast.
Few LRTI surgical techniques allow early postoperative mobilization. Only one paper has to our knowledge used an interferential screw to secure the FCR tendon within the first metacarpal base. Brunton and Wittstadt [2] used an absorbable interference screw and started physical therapy two weeks after LRTI. We used a metal interference screw to secure tendon fixation. Temporary fixation wire was removed one week after operation and physical therapy was then started. Dorsal subluxation was corrected to anatomical alignment and maintained in the mean follow-up of 20 months. Our modified technique produced sufficient ligamentoplasty and allowed early mobilization after surgery.
Although this study provided several novel findings, it has some limitations. First, this was a retrospective and single-center study. The number of cases is limited. Second, we did not compare our modified LRTI against other procedures. Further comparative studies are needed for this purpose.
References
Brunton LM, Wittstadt RA (2011) Thumb carpometacarpal arthroplasty using an absorbable interference screw for flexor carpi radialis ligament reconstruction. Tech Hand Up Extrem Surg 15:115–118
Burton RI, Pellegrini VD (1986) Surgical management of basal joint arthritis of the thumb. Part II: ligament reconstruction with tendon interposition arthroplasty. J Hand Surg Am 11:324–332
Davis TR, Pace A (2009) Trapeziectomy for trapeziometacarpal joint osteoarthritis: is ligament reconstruction and temporary stabilisation of the pseudarthrosis with a Kirschner wire important? J Hand Surg Eur 34:312–321
Downing ND, Davis TR (2001) Trapezial space height after trapeziectomy: mechanism of formation and benefits. J Hand Surg Am 26:862–868
Eaton RG, Glickel SZ (1987) Trapeziometacarpal osteoarthritis: staging as a rationale for treatment. Hand Clin 3:455–471
Eaton RG, Lane LB, Littler JW, Keyser JJ (1984) Ligament reconstruction for the painful thumb carpometacarpal joint: a long-term assessment. J Hand Surg Am 9:692–699
Gangopadhyay S, McKenna H, Burke FD, Davis TR (2012) Five- to 18-year follow-up for treatment of trapeziometacarpal osteoarthritis: a prospective comparison of excision, tendon interposition, and ligament reconstruction and tendon interposition. J Hand Surg Am 37:411–417
García-Mas R, Solé Molins X (2009) Partial trapeziectomy with ligament reconstruction–tendon interposition in thumb carpo-metacarpal osteoarthritis. A study of 112 cases. Chir Main 28:230–238
Gervis WH (1949) Excision of the trapezium for osteoarthritis of the trapeziometacarpal joint. J Bone Joint Surg 31B:537–539
Gray KV, Meals RA (2007) Hematoma and distraction arthroplasty for thumb basal joint osteoarthritis: minimum 6.5-year follow-up evaluation. J Hand Surg Am 32:23–29
Hartigan BJ, Stern PJ, Kiefhaber TR (2001) Thumb carpometacarpal osteoarthritis: arthrodesis compared with ligament reconstruction and tendon interposition. J Bone Joint Surg Am 83:1470–1478
Kennedy CD, Manske MC, Huang JI (2016) Classifications in brief: the eaton-littler classification of thumb carpometacarpal joint arthrosis. Clin Orthop Relat Res 474:2729–2733
Kriegs-Au G, Petje G, Fojtl E, Ganger R, Zachs I (2004) Ligament reconstruction with or without tendon interposition to treat primary thumb carpometacarpal osteoarthritis. A prospective randomized study. J Bone Joint Surg Am 86:209–218
Kriegs-Au G, Petje G, Fojtl E, Ganger R, Zachs I (2005) Ligament reconstruction with or without tendon interposition to treat primary thumb carpometacarpal osteoarthritis. Surgical technique. J Bone Joint Surg Am 87(Supl1 1(1)):78–85
Li YK, White C, Ignacy TA, Thoma A (2011) Comparison of trapeziectomy and trapeziectomy with ligament reconstruction and tendon interposition: a systematic literature review. Plast Reconstr Surg 128:199–207
Marenghi L, Paterlini M, Tocco S, Corradi M (2016) Trapeziectomy with ligament reconstruction and tendon interposition arthroplasty with the entire width of the flexor carpi radialis tendon. Tech Hand Up Extrem Surg 20:67–70
Naidu SH, Poole J, Horne A (2006) Entire flexor carpi radialis tendon harvest for thumb carpometacarpal arthroplasty alters wrist kinetics. J Hand Surg Am 31:1171–1175
Salem HM, Davis TR (2014) Degenerative change at the pseudarthrosis after trapeziectomy at 6-year follow up. Clin Orthop Relat Res 472:1160–1165
Thompson JS (1989) Suspensionplasty J Orthop Surg Tech 4:1–13
Tomaino MM, Coleman K (2000) Use of the entire width of the flexor carpi radialis tendon for the ligament reconstruction tendon interposition arthroplasty does not impair wrist function. Am J Orthop (Belle Mead NJ) 29:283–284
Vermeulen GM, Slijper H, Feitz R, Hovius SE, Moojen TM, Selles RW (2011) Surgical management of primary thumb carpometacarpal osteoarthritis: a systematic review. J Hand Surg Am 36:157–169
Wang T, Zhao G, Rui YJ, Mi JY (2018) Outcomes of modified trapeziectomy with ligament reconstruction tendon interposition for the treatment of advanced thumb carpometacarpal arthritis: two-year follow-up. Medicine (Baltimore) 97:e0235
Weiss AC, Kamal RN, Paci GM, Weiss BA, Shah KN (2019 Apr) Suture suspension arthroplasty for the treatment of thumb carpometacarpal arthritis. J Hand Surg Am 44(4):296–303
Werthel JD, Dubert T (2016) Use of the entire flexor carpi radialis tendon for basal thumb ligament reconstruction interposition arthroplasty. Hand Surg Rehabil 35:107–113
Funding
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no potentrial conflict of interest with respect to the research, authorship and publication of this article.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Muramatsu, K., Tani, Y., Seto, T. et al. Partial trapeziectomy for Eaton stage III thumb carpometacarpal arthritis: ligament reconstruction with tendon interposition using the entire flexor carpi radialis and interference screw fixation. Eur J Orthop Surg Traumatol 32, 151–157 (2022). https://doi.org/10.1007/s00590-020-02863-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-020-02863-4