Abstract
Background
Intra- and juxta-articular osteoid osteoma (OO) is rare and can result in irreversible joint damage. Recently, arthroscopic surgery is being used more and more to avoid complications associated with other treatment modalities.
Methods
On October 13, 2019, we conducted a systematic review of the literature available in PubMed and EMBASE regarding the arthroscopic management of OO involving the joints of the upper extremity. Predetermined inclusion criteria were used to include any relevant article published on and before that date for further analysis. Treatment success rate and tumor recurrence rate were considered the primary outcomes in our analysis.
Results
Out of 113 studies, 19 met our inclusion criteria. Of the 32 reported cases in these 19 articles, ten involved the shoulder joint, 19 involved the elbow joint and three involved the wrist joint. Overall treatment success rate was 93.8%. Tumor recurrence rate was 0.0%. No postoperative complications (0.0%) were reported among cases involving the shoulder joint. Two out of 24 (8.3%) patients with elbow OO failed arthroscopic treatment due to incomplete excision, and two (4%) experienced minor complications. Among the three cases of wrist OO, two (66.7%) patients had residual postoperative pain and decreased hand grip strength.
Conclusion
Arthroscopic management of OO of the upper extremity joints is highly successful and results in no tumor recurrence; however, there is a risk of incomplete resection in areas more difficult to access by arthroscopy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Osteoid osteoma (OO) is commonly found in long bones of patients under the age of 30, accounting for up to 14% of all benign bone tumors [1, 2]. Approximately, one out of ten cases of OO are intraarticular [1, 3,4,5]. When a joint is involved, the patient presents with symptoms and signs mimicking inflammatory arthritis, septic arthritis, fracture and avascular necrosis [1, 3, 6,7,8,9]. Signs and symptoms include limited joint range of motion, joint effusion, nocturnal pain, and pain worsening with activities. If misdiagnosed and mistreated, intraarticular OO can result in irreversible joint damage due to long-standing inflammation and synovitis [1, 10]. Therefore, obtaining appropriate investigations should not be delayed whenever the diagnosis is suspected. Plain radiographs are usually not helpful in cases of intraarticular OO; however, computed tomography (CT) scans will show the classic calcified nidus surrounded by a lytic lesion [1, 11]. Bone scan will most often show focal tracer uptake [1].
Conservative treatment includes nonsteroidal anti-inflammatory medications (NSAID) or salicylates which often relieve symptoms [1]. If symptoms persist, definitive treatment includes radiofrequency ablation (RFA), cryo-ablation, percutaneous drilling, laser thermoregulation and surgical resection [1, 7,8,9, 12,13,14]. However, irreversible damage to the articular cartilage, or physis in younger patients, can result from any of these treatment modalities [1, 10]. To minimize such complications in the management of intraarticular OO, orthopedic surgeons are now starting to use arthroscopy to resect juxta- or intraarticular OO [7, 9, 15,16,17,18].
Osteoid osteoma most commonly affects the metaphysis or diaphysis of the femur and tibia; therefore, OO involving the joints of the upper extremity is very rare [1]. Most of the scientific papers reporting the outcomes from the arthroscopic management of OO are of small sample size, and thus, a definitive conclusion regarding the outcome of this treatment modality is lacking [9]. Therefore, we conducted a systematic review of the available literature looking at the use of arthroscopy in the management of intra- and juxta-articular OO of the upper extremity. We hypothesized that the success rate of arthroscopic OO resection in the upper extremity is on par with the current gold standard with low a recurrence rate.
Methods
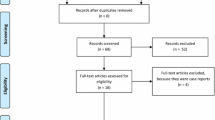
PubMed and EMBASE were searched, looking for articles related to the arthroscopic treatment for OO in the upper extremity. This was performed by two reviewers (S.G. and Y.M.) independently. Articles published on or before October 13, 2019, were included. The subject headings and their related key terms used in this review were “osteoid osteoma” and “arthroscopy” (see Fig. 1). Inclusion criteria were (1) all levels of scientific evidence, (2) human studies, (3) both genders, (4) any age-group, (5) English language, (6) intra- or juxta-articular OO and (7) arthroscopic treatment. The following criteria were used for exclusion: (1) articles published in abstract form only, (2) nonsurgical studies (e.g., review papers, cadaveric studies), (3) articles about OO not involving the upper extremity joints, (4) patients who received conventional open surgical treatment and (5) articles of nonrelated diagnosis.
The independent reviewers screened titles and abstracts for eligibility. Based on the abstract review, articles were included only if both reviewers independently determined that all the inclusion criteria were met. Articles were then included in further full-text review if one of the investigators believed they meet the inclusion criteria. Any disagreements were resolved by discussion and mediation by a third reviewer (F.A.), if necessary. Relevant data were then extracted and recorded by the same investigators using Microsoft Excel 2016 (Microsoft, Redmond, WA). The recorded data included background information about the articles (i.e., year of publication, authors, study design, sample size and level of evidence), clinical details (i.e., age, sex, affected joint and specific location of the lesion), arthroscopic technique (i.e., patient positioning, arthroscopic portals, tumor handling), duration of patients’ follow-up, recurrence rate and treatment complications. Success rate and recurrence rate were considered as the primary outcomes in our analyses.
A meta-analysis was not performed due to the heterogeneity of the retrieved studies. Thus, a qualitative assessment was reported. Quality assessments of each individual study were not performed because all studies were of level IV evidence.
Results
A total of 113 unique studies were found with the initial search after 80 duplicates were removed. Seventy-four studies were excluded following title review, 16 articles were removed after abstract review and four more articles were removed after full-text review (Fig. 2). Eventually, we included 19 studies in our final review for further analysis (Tables 1,2,3). A screening of the references of the included studies did not reveal any further eligible studies for inclusion in our review.
There was no disagreement throughout the stages of this systematic review in between the two reviewers. Due to the heterogeneity of the data included, and the level IV evidence of all the studies, a meta-analysis was not performed.
A total of 32 cases related to arthroscopic management of intraarticular OO of the upper extremity joints were reported in the included studies. Of these 32 cases, ten involved the shoulder joint (Table 1), 19 involved the elbow joint (Table 2) and three involved the wrist joint (Table 3).
The Shoulder (Table 1 )
In the shoulder, six (60.0%) of the ten patients were males, and the mean age was 25.9 ± 10.8 (range 12–46) years. Five (50.0%) OO lesions were found in the coracoid process, two (20.0%) in the acromion, two (20.0%) in the glenoid and one (10.0%) in the humeral head. Delay in diagnosis ranged from 3 months to 4 years. The patient position during surgery was not described in six (60.0%) patients; however, three (30.0%) of the remaining patients underwent arthroscopy in beach chair position and one (10.0%) in lateral decubitus position. Most lesions were identified under direct visualization of either an area of abnormal bone or cartilage which was de-roofed to expose the nidus. Two cases (20.0%) used preoperative planning and CT imaging to help identify the lesion. Following tumor excision, the case of OO in the humeral head lesion (1; 10.0%) required a bone graft to fill the defect. Additionally, one of the cases of OO in the coracoid (1; 10.0%) had arthroscopic-guided RFA following tumor excision. Acromioplasty and the Mumford procedure were done for one (10.0%) of the cases where the tumor was in the acromion. Four cases reported rehabilitation protocol. Three cases had sling immobilization from 2–4 weeks followed by gradual mobilization, while one proceeded to immediate mobilization. Follow-up duration was not reported in one (10.0%) case; however, the rest of the patients had a mean follow-up of 62 ± 53 (range: 3–168) months. The surgery was successful in treating the tumor in all (10; 100.0%) the cases, with no (0; 0.0%) complications or tumor recurrence being reported.
The Elbow (Table 2 )
Sixteen (84.2%) out of the 19 patients with elbow OO were males. The mean age of the patients was 26.3 ± 9.2 (range 12–48) years. The most common location for the OO about the elbow joint was the olecranon fossa or coronoid fossa (10; 52.6%), followed by the radial head (3; 15.8%), capitellum (2; 10.5%) and trochlea (2; 10.5%). Delay in diagnosis ranged from 6 months to 3 years. Two cases did not specify the location of the lesion in the distal humerus. Twelve (63.2%) cases used fluoroscopy to assist in lesion localization. Twelve cases reported rehabilitation protocol, all of which included immediate mobilization. The mean postoperative follow-up was 30.6 ± 22.6 (range: 1.5–78) months. Two (10.5%) patients failed arthroscopic treatment and required open surgical excision of the tumor. There was no tumor recurrence in any reported cases (0; 0.0%). Minor complications were reported in two (10.5%) patients; one had limited elbow flexion–extension requiring open surgical release, and the other had residual pronation contracture at final follow-up.
The Wrist (Table 3 )
Wrist arthroscopy was used to treat three cases of OO. One (33.3%) of the cases was males, and the mean age was 33.3 ± 12.9 (range: 21–45) years. Lesions were found in the ulnar side of the lunate (1; 33.3%), the distal pole of the scaphoid (1; 33.3%) and the radial styloid (1; 33.3%). Delay in diagnosis ranged from 2 months to 1.5 years. For the lunate and the radial styloid, portals 3–4 and 4–5 were used to excise the lesion, while the mid-carpal ulnar (MCU) and the mid-carpal radial (MCR) portals were used for the scaphoid OO. Two cases (66.7%) used fluoroscopy to assist in lesion localization. The mean follow-up was 13.7 ± 3.8 (range 11–18) months. No information was provided regarding rehabilitation protocol. Treatment was successful in all cases (3; 100%), and no tumor recurrence occurred (0; 0.0%). Two patients had persistent pain postoperatively (66.67%). The patient with the scaphoid lesion had persistent tenderness in the radial side of the wrist and pain during full force pinching, and the patient with the lunate lesion had pain with deep palpation of the dorsal surface of the wrist. Both patients had weaker hand grip strength compared to the contralateral side.
Discussion
This study presents a systematic review regarding the use of arthroscopy to treat intra- and juxta-articular OO of the upper extremity. In our cases, delay in diagnosis ranged from 2 months to 4 years with several patients undergoing other procedures prior to coming to the diagnosis of OO. In most cases, an area of abnormal bone or cartilage could be visualized directly during arthroscopy and was de-roofed to expose the nidus. Some used preoperative CT images and fluoroscopy to assist in localization or confirm location of lesion. Failure rate in eradicating the tumor was very low and success rate ranged from 100% for the shoulder and wrist to 89.5%% for the elbow regardless of the specific location of the lesion and the arthroscopic technique used. Failure was due to incomplete excision. In one of the failed cases, the tumor was in the extraarticular portion of the radial head with the nidus being beneath the annular ligament, making it difficult to reach by arthroscopy. No complications were seen among the cases with shoulder OO. There were only mild complications with this treatment modality. In the elbow, one of the 19 patients had a pronation contracture following arthroscopic management, and another had limited elbow flexion–extension requiring surgical release. In addition, two of the three patients with wrist OO had pain with specific wrist and hand activities, as well as weaker hand grip strength. This rate of complications is likely similar or better to open surgical resection but further comparative studies will have to be undertaken [37, 40]. No tumor recurrence following arthroscopy was reported in the available literature.
Intra- and juxta-articular OO is rare and difficult to diagnose, leading to delay in appropriate treatment [3, 10, 19]. An average delay of 4 years for the initial diagnosis of OO in such locations was previously reported [3]. NSAID usually controls the symptoms of OO and can eventually lead to resolution of the pain [1, 12, 20]. However, the average time to achieve these favorable results is 33 to 36 weeks [12, 20]. With intra- or juxta-articular OO, any delay in treatment, or the response to it, could result in irreversible joint damage [3, 41,42,43].
Open surgical excision and percutaneous CT-guided excision or RFA provide excellent outcomes for OO [1, 8, 13, 14, 21]. Nevertheless, open surgical techniques require a thorough soft tissues dissection, which can lead to surgical site morbidity, in addition to longer postoperative rehabilitation [1]. Also, en bloc resection of the tumor often results in bony defects requiring stabilization or grafting [1]. Percutaneous techniques, on the other hand, have less surgical site morbidity. However, it can be difficult to access areas such as the smaller joints of the upper extremity. Moreover, these minimally invasive procedures in areas such as the coracoid process or anterior elbow may lead to neurovascular injuries in areas that are near important anatomic structures [34]. There have also been reports of devitalization of the articular cartilage surrounding intraarticular tumors secondary to thermal injury from poor targeting and needle placement in these minimally invasive procedures [14, 21]. Another disadvantage of performing percutaneous RFA is that histological confirmation of OO is not always possible [16].
There are potential limitations with this systematic review. Most the included studies had a sample size of one patient; there was a lack of studies with a high level of evidence. This, though, was expected due to the scarcity of patients with intra- or juxta-articular OO in the upper extremities. In addition, there is missing and inconsistent reporting of lesion locations and the surgical techniques used. The duration of postoperative follow-up also varied across the studies. Some studies with a shorter follow-up make it difficult to catch possible late recurrences, as well as resolution of postoperative symptoms such as stiffness and pain which we documented as complications. Moreover, late onset complications following the surgical treatment of intraarticular pathology (e.g., early osteoarthritis) may also be missed. Outcome following arthroscopic surgery also depends on surgeon’s expertise and experience; therefore, some treatment failure could be related to surgeon factors rather than treatment modality.
Conclusion
Arthroscopic management of OO of the upper extremity joints is highly successful, with low rate of minor complications. Patients who underwent this treatment did not have any tumor recurrence at final follow-up; however, there is a risk of incomplete excision in areas more difficult to access by arthroscopy. Larger case series and studies of higher level of evidence regarding the use of arthroscopy for intra- and juxta-articular OO are needed.
References
Boscainos PJ, Cousins GR, Kulshreshtha R, Oliver TB, Papagelopoulos PJ (2013) Osteoid osteoma. Orthopedics 36:792–800
Jackson RP, Reckling FW, Mants FA (1977) Osteoid osteoma and osteoblastoma. Similar histologic lesions with different natural histories. Clin Orthop Relat Res 128:303–313
Franceschi F, Marinozzi A, Papalia R, Longo UG, Gualdi G, Denaro E (2006) Intra- and juxta-articular osteoid osteoma: a diagnostic challenge: misdiagnosis and successful treatment: a report of four cases. Arch Orthop Trauma Surg 126:660–667
Gamba JL, Martinez S, Apple J, Harrelson JM, Nunley JA (1984) Computed tomography of axial skeletal osteoid osteomas. AJR Am J Roentgenol 142:769–772
Swee RG, McLeod RA, Beabout JW (1979) Osteoid osteoma. Detection, diagnosis, and localization. Radiology 130:117–123
Alani WO, Bartal E (1987) Osteoid osteoma of the femoral neck simulating an inflammatory synovitis. Clin Orthop Relat Res 223:308–312
Marwan YA, Abatzoglou S, Esmaeel AA, Alqahtani SM, Alsulaimani SA, Tanzer M, Turcotte RE (2015) Hip arthroscopy for the management of osteoid osteoma of the acetabulum: a systematic review of the literature and case report. BMC Musculoskelet Disord 16:318
Daniilidis K, Martinelli N, Gosheger G, Hoell S, Henrichs M, Vogt B, Hardes J, Vieth V (2012) Percutaneous CT-guided radio-frequency ablation of osteoid osteoma of the foot and ankle. Arch Orthop Trauma Surg 132(12):1707–1710
Kamrani RS, Moradi A, Sharafat Vaziri A, Nabian MH, Ghane B (2017) Arthroscopic ablation of an osteoid osteoma of the elbow: a case series with a minimum of 18 months' follow-up. J Shoulder Elbow Surg 26(5):e122–e127
Song MH, Yoo WJ, Cho TJ, Chung CY, Park MS, Cheon JE, Choi IH (2015) Clinical and radiological features and skeletal sequelae in childhood intra-/juxta-articular versus extra-articular osteoid osteoma. BMC Musculoskelet Disord 16:3
Klein MH, Shankman S (1992) Osteoid osteoma: radiologic and pathologic correlation. Skeletal Radiol 21:23–31
Kneisl JS, Simon MA (1992) Medical management compared with operative treatment for osteoid-osteoma. J Bone Joint Surg Am 74:179–185
Parlier-Cuau C, Nizard R, Champsaur P, Hamze B, Quillard A, Laredo JD (1999) Osteoid osteoma of the acetabulum. Three cases treated by percutaneous resection. Clin Orthop Relat Res 365:167–174
Akhlaghpoor S, Aziz Ahari A, Arjmand Shabestari A, Alinaghizadeh MR (2010) Radiofrequency ablation of osteoid osteoma in atypical locations: a case series. Clin Orthop Relat Res 468:1963–1970
Abnousi F, Saliman JD, Fanton GS (2008) Arthroscopic visualization and assisted excision of osteoid osteoma at the knee: a case report and review. Am J Sports Med 36(2):375–378
Gao K, Hua Y, Chen S, Li Y, Xin Q (2013) Arthroscopic excision of juxtaarticular cancellous osteoid osteoma in the talar neck. Knee Surg Sports Traumatol Arthrosc 21(6):1300–1303
Dimnjaković D, Bojanić I, Smoljanović T, Mahnik A (2015) Periarticular osteoid osteoma of the ankle: a report of nine arthroscopically treated patients. J Foot Ankle Surg 54(1):89–93
Jurina A, Dimnjaković D, Smoljanović T, Bojanić I (2017) Removal of Osteoid Osteoma of the Calcaneus Using Subtalar Arthroscopy. Foot Ankle Spec 10(4):359–363
Pikoulas C, Mantzikopoulos G, Thanos L, Passomenos D, Dalamarinis C, Glampedaki-Dagianta K (1995) Unusually located osteoid osteomas. Eur J Radiol 20:120–125
Goto T, Shinoda Y, Okuma T, Oqura K, Tsuda Y, Yamakawa K, Hozumi T (2011) Administration of nonsteroidal anti-inflammatory drugs accelerates spontaneous healing of osteoid osteoma. Arch Orthop Trauma Surg 131:619–625
Rosenthal DI, Hornicek FJ, Wolfe MW, Jennings LC, Gebhardt MC, Mankin HJ (1998) Percutaneous radiofrequency coagulation of osteoid osteoma compared with operative treatment. J Bone Joint Surg Am 80:815–821
Chojecki Ł, Płomiński J, Pepłoński A (2017) Unusual Location of Osteoid Osteoma in the Acromion. Ortop Traumatol Rehabil 19(1):67–73
Glanzmann MC, Hinterwimmer S, Woertler K, Imhoff AB (2011) Osteoid osteoma of the coracoid masked as localized capsulitis of the shoulder. J Shoulder Elbow Surg 20(8):e4–e7
Glanzmann MC, Imhoff AB, Schwyzer HK (2013) Osteoid osteoma of the shoulder and elbow: from diagnosis to minimally invasive removal. Int Orthop 37(12):2403–2408
Goyal S, Said HG (2015) Osteoid osteoma (OO) of the coracoid: a case report of arthroscopic excision and review of literature. SICOT J 1:17
Kelly AM, Selby RM, Lumsden E, O'Brien SJ, Drakos MC (2002) Arthroscopic removal of an osteoid osteoma of the shoulder. Arthroscopy 18(7):801–806
Malavolta EA, Assunção JH, Rebolledo DC, Gracitelli ME, Correia LF, Ferreira Neto AA, de Camargo OP (2015) Osteoid osteoma of the glenoid: Arthroscopic treatment. Orthop Traumatol Surg Res 101(8):977–980
Miller SL, Hazrati Y, Klein MJ, Springfield DS, Flatow EL (2003) Intraarticular osteoid osteoma of the proximal humerus: A case report. J Shoulder Elbow Surg 12(1):94–96
Miyazaki AN, Fregoneze M, Santos PD, da Silva LA, do ValSellaNeto GDL, MuchiutiJunior M, Checchia SL (2014) Osteoid osteoma of the acromion simulating acromioclavicular pain. Rev Bras Ortop 49(1):82–85
Ueyama H, Ito Y, Manaka T, Matsumoto I, Ichikawa K, Nakamura H (2016) Arthroscopic treatment of an osteoid osteoma at the base of the coracoid process: A case report. J Orthop Sci 21(2):245–249
Akpinar S, Circi E (2017) Arthroscopic excision of an intra-articular osteoid osteoma in the elbow joint. BMJ Case Rep 2017.
Goyal T, Pandita N, Paul S (2018) Arthroscopic excision of intra-articular sub-periosteal osteoid osteoma of elbow: a case report. SICOT J 4:25
Hatta T, Hosaka M, Watanuki M, Yano T, Yoshida S, Watanabe M et al (2019) Arthroscopic Excision of Intra-Articular Osteoid Osteoma at the Elbow. Case reports in orthopedics 2019:8505382
Nourissat G, Kakuda C, Dumontier C (2007) Arthroscopic excision of osteoid osteoma of the elbow. Arthroscopy 23(7):799.e1–e4
Segura JF, Barrera-Ochoa S, Gargallo-Margarit A, Correa-VázquezE I-T, Bullo XM (2013) Osteoid Osteoma of the Distal Humerus Mimicking Sequela of Pediatric Supracondylar Fracture: Arthroscopic Resection—Case Report and A Literature Review. Case Rep Med 2013:247328
Trebse R, Poberaj B, Cör A, Levasic V (2007) Arthroscopic removal of an osteoid osteoma in the radial head: a case report. Arthroscopy 23(12):1361.e1–e3
Zupanc O, Sarabon N, Strazar K (2007) Arthroscopic removal of juxtaarticular osteoid osteoma of the elbow. Knee Surg Sports Traumatol Arthrosc 15(10):1240–1243
Kamrani RS, Farhadi L, Emamzadehfard S (2013) Arthroscopic ablation of osteoid osteoma in the wrist. Arch Bone Jt Surg 1(1):38–40
Nishio J, Ishiko T, Minamikawa T, Naito M (2012) Arthroscopic removal of an intra-articular osteoid osteoma of the radial styloid. J Hand Surg Am 37(1):68–71
Weber KL, Morrey BF (1999) Osteoid osteoma of the elbow: a diagnostic challenge. J Bone Joint Surg Am 81(8):1111–1119
Brabants K, Geens S, van Damme B (1986) Subperiosteal juxta-articular osteoid osteoma. J Bone Joint Surg Br 68(2):320–324
Sherman MS (1947) Osteoid osteoma associated with changes in adjacent joint; report of two cases. J Bone Joint Surg Am 29(2):483–490
Norman A, Abdelwahab IF, Buyron J, Matzkin E (1986) Osteoid osteoma of the hip stimulating an early onset of osteoarthritis. Radiology 158(2):417–420
Funding
No external source of funding was used.
Author information
Authors and Affiliations
Contributions
Ge was involved in data collection, manuscript writing and manuscript revision. Marwan was also involved in data collection in addition to conception, manuscript writing and revision. Abduljabbar was involved in manuscript revision. Morelli contributed to manuscript revision and supervision. Turcotte contributed to manuscript revision and supervision.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
They can be provided upon request.
Code availability
Not applicable.
Ethics approval
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ge, S.M., Marwan, Y., Abduljabbar, F.H. et al. Arthroscopic management of intra- and juxta-articular osteoid osteoma of the upper extremity: a systematic review of the literature. Eur J Orthop Surg Traumatol 30, 1333–1344 (2020). https://doi.org/10.1007/s00590-020-02710-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-020-02710-6