Abstract
Purpose
The X index is a measure of the antero-inferior glenoid bone loss on unilateral 2D CT-scans in the preoperative analysis of chronic anterior shoulder instability. Recurrence rate was shown to be higher after stabilization surgery if X index is superior or equal to 0.4. The objective of this study was to assess the intra- and inter-observer reliability of the X index.
Methods
Sixty patients with an X index ≥0.4 were included retrospectively. The X index was measured twice by two independent evaluators, 15 days apart. The measurement was performed on a unilateral 2D CT-scan by dividing the length of the antero-inferior glenoid defect over the maximal antero-posterior diameter of the glenoid. Reliability of X index was assessed with intra-class correlation coefficient (ICC, ρ). Two points were added to the ISIS calculation if its glenoid criterion was “zero” and we compared this modified score to the original one.
Results
The intra-observer reliability of the X index measurement was “excellent” (ρ = 0.95 ± 0.01, p < 0.0001) while the inter-observer reliability was “good” (ρ = 0.59 ± 0.08, p < 0.0001). In patients with a glenoid bone loss visualized by the X index, 48.3 % had a negative sclerotic glenoid line sign. This proportion significantly decreased with the augmentation of the X index, p = 0.02. The average original ISIS score was 3.4 ± 1.9 and became 4.3 ± 1.7 (p < 0.00001) when the X index was incorporated.
Conclusions
The X index is a reliable and simple unilateral 2D CT-scan measurement. AP shoulder radiographs significantly underestimated glenoid bony lesions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Chronic anterior shoulder instability remains a widely discussed topic in the literature. Current treatment practices vary between open surgical techniques and arthroscopic techniques. Long-term results of arthroscopic techniques remain inferior in terms of recurrence of instability than those obtained after bone block transfer procedures [6].
Antero-inferior glenoid bone loss has been associated with higher rates of failure of arthroscopic technique [7, 9, 15, 16, 19, 21, 23, 25, 30]. Burkhart et al. [11] previously reported that failure rate was higher than 50 % in patients with 25 % glenoid bony loss.
Several authors described different radiological methods of detecting and measuring these bony defects [2, 5, 20, 26, 27]. The loss of the anterior sclerotic glenoid line (SGL) in neutral rotation radiographs is currently widely used to detect anterior glenoid bone loss [20]. CT-scan measurement methods of anterior glenoid bone loss have been recently developed [4, 17, 24, 29]. Gerber et al. [15] also published a simple method of measuring antero-inferior glenoid bone loss on 2D CT-scans and entitled it the X index. Sommaire et al. [28] showed than an X index superior or equal to 0.4 results in higher failure rates of arthroscopic stabilization after 2 years follow-up.
A recent publication by Auffarth et al. [1] stresses the importance of the CT-scan versus plain radiographs in the detection of glenoid bony lesions in anterior shoulder instability. This therefore confirms the necessity of a more precise method of bone lesion detection.
Decision making in cases of chronic anterior shoulder instability is surgeon dependent. The Instability Stability Index Score (ISIS) was aimed to simplify decision making in cases of chronic anterior shoulder instability [3]. It took into consideration a great number of factors that throughout the years have shown to be predictive of success or failure of the initial stabilization [9]. The ISIS publication [3] recommended performing an arthroscopic Bankart repair in patients with a score of six or lower and a bone block transfer procedure like the Latarjet procedure [22] for those with more than six points.
We hypothesize that plain radiographic evaluation of the SGL sign is not satisfactory in definitively eliminating the loss of the inferior glenoid bone loss and that CT-scan enhancement is necessary to correctly visualize the glenoid rim.
The objective of this study was to assess the intra- and inter-observer reliability of the X index to quantify glenoid bone loss in chronic anterior shoulder instability.
Materials and methods
A mono-centric retrospective study concerned all cases presenting with chronic anterior shoulder instability treated surgically between January 2010 and January 2011.
Radiological assessment
All operated patients systematically underwent AP shoulder radiographs in internal, neutral and external rotations, supraspinatus outlet view and a CT-scan.
For the study, CT-scans of all operated patients were evaluated. Two orthopedic trauma surgeons of similar experience independently viewed the CT-scan. The second evaluation of the CT-scan was blinded and viewed in a different sequence. Both observers were blinded to the plain radiographic findings. An independent biostatistician ensured the standardization of the study protocol.
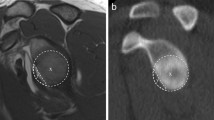
The X index was measured using the Osirix™ software. The measurements were taken on a sagittal image passing through the glenoid just after the disappearance of the humeral head. The X index was calculated by dividing the length of the anterior bone lesion over the maximal diameter of the glenoid (Fig. 1) [15].
According to the ISIS, the AP shoulder radiograph in neutral position was used in order to detect a loss in the SGL [20]. This assessment was done by the surgeon as a preoperative evaluation and was collected retrospectively from the medical file.
ISIS calculations
The original ISIS was calculated for each patient [3]. The modified ISIS was recalculated by adding two points to each patient who was shown to have a bony glenoid lesion on the CT-scan (X index ≥0.4) and not on the neutral AP radiographs (loss of the SGL). Two points were chosen to reproduce the original ISIS scoring system.
Statistical analysis
Statistical analysis was performed using Stata®/IC V 10.0. The Pearson’s rank correlation coefficient (r), the Bland and Altman diagram [8] and the intra-class correlation coefficient (ICC, ρ) were used to assess the intra- and inter-observer reliability of the X index. The strength of the relationship was classified as strong (r > 0.5), medium (0.3 < r < 0.5), small (0.1 < r < 0.3) or none (r < 0.1) [12]. The strength of the agreement was classified as excellent (ρ > 0.75), good (0.40 < ρ < 0.75) or poor (ρ < 0.40) [14]. All correlations were tested for statistical significance using the p value. The Student’s t test was used for comparing groups. Nonparametric analysis was performed using the Cuzick’s nonparametric trend test. Statistical significance was set at p ≤ 0.05.
Results
During the study period, 160 patients underwent surgery for chronic anterior shoulder instability. Sixty patients with X index ≥ 0.4 were included. The mean age was 28 years (average 15–26). There were 56 men and 4 women, with 40 right and 20 left shoulders. An arthroscopic Bankart repair was performed in 14/60 patients, an arthroscopic Latarjet procedure in 22/60 patients and an open Latarjet procedure in 24/60 patients.
The intra-observer reliability of the X index was strong with a Pearson’s coefficient of correlation measured at r = 0.95 (p < 0.00001) and an excellent intra-class coefficient of correlation at ρ = 0.95 (p < 0.00001). The inter-observer reliability was strong with a Pearson’s coefficient of correlation measured at r = 0.61 (p < 0.00001) and a good intra-class coefficient of correlation at ρ = 0.59 ± 0.08 (p < 0.00001, Fig. 2).
All patients with no radiological glenoid bone loss, thus a glenoid score of “zero”, were isolated (29 patients or 48.3 %). Measurement of the X index in these patients revealed a significant reduction in number of cases with a negative SGL sign when the X index increases: 14/23 (60.9 %) with 0.40 < X < 0.60, 14/29 (48.3 %) with 0.60 ≤ X < 0.80 and 1/8 (12.5 %) with 0.80 ≤ X < 1, p = 0.02 (Table 1).
The difference between the original and recalculated ISIS (two points added if X index ≥ 0.40) was 0.9 points. The mean original ISIS was 3.4 ± 1.9 while the mean modified ISIS was 4.3 ± 1.7 (p < 0.00001).
Discussion
Multiple publications have demonstrated the importance of the failure of arthroscopic stabilization if associated with glenoid bone loss [7, 9, 10, 16, 19, 21, 23, 25, 30]. This therefore leads us to more efficiently analyze glenoid bony lesions in order to reduce recurrence. Burkhart et al. [11] has previously demonstrated the importance of the glenoid bone loss on the rates of failure of arthroscopic Bankart repair. This was seconded by Boileau et al. [9] who also stated that glenoid bone loss was an important risk factor for failure of arthroscopic treatments. This study was based on a previous publication by Sommaire et al. [28] who systematically studied and measured the X index and correlated it with rates of failure. In their study, a recurrence rate of 20 % after arthroscopic stabilization was observed if the X index was equal to or greater than 0.4.
Multiple methods of analyzing the antero-inferior glenoid bone loss exist. Radiological analysis using either plain radiographs or sophisticated methods using CT-scans has been described. Arthroscopic bare spot measurement described by Burkhart et al. [10] is another alternative that is both invasive and operator dependent.
Analysis of the loss of SGL described by Jankauskas et al. [20] is a method used to analyze antero-inferior glenoid bone loss. This method is the recommended method described in original ISIS publication. In our study, it was clearly demonstrated that more than half of the patients in the study group had a false negative on plain AP radiographs.
Alternative plain radiographic methods of antero-inferior glenoid bone loss detection include the axillary view [13] or the Bernageau view [5]. Pansard et al. [26] demonstrated the efficacy of the Bernageau view in demonstrating antero-inferior glenoid bone loss. Even though the Bernageau view shows excellent reliability, it remains a bilateral and difficult examination to correctly perform. It is also a difficult examination to perform in acute cases where the patient remains painful and could not perform the maneuver required for correct visualization.
The measurement method published by Sugaya et al. [29] uses a unilateral 3D CT-scan to analyze bone loss. The Sugaya method was shown to have a good inter- and intra-observer reliability by a cadaveric study performed by Huysmans et al. [18]. The Griffith method [17] is another well known and commonly used CT-scan based measurement that requires a CT-scan of the contralateral shoulder. No studies have been performed to show its inter- and intra-observer reliability.
The Pico method described by Magarelli et al. [24] shows very good inter- and intra-observer reliability using a 2D CT-scan that requires scanning the contralateral shoulder. The X index can be measured on 2D CT-scan without the necessity of the contralateral shoulder using conventional free software. We have also demonstrated very good and excellent inter- and intra-observer reliability, respectively.
Results clearly show that if the CT-scan is taken into consideration, the ISIS significantly increases therefore potentially altering treatment technique. A more precise analysis of antero-inferior glenoid bone loss would probably increase the indication for a Latarjet procedure, as detection of even smaller lesions will be performed. Since the realization of this study, all patients who suffer from anterior shoulder instability systematically perform a CT-scan of the affected shoulder. The measurement of X index is routinely performed and helps in the decision making.
Even though we showed the superiority of the CT-scan based X index over the AP radiograph, a prospective study that compares the recurrence rate of patient’s chosen according to the ISIS versus those chosen using the ISIS and X index should be performed.
Study limitations include its retrospective design and the lack of clinical results concerning the subject.
To conclude, the X index performed on a unilateral 2D CT-scan helps in the detection of small but significant antero-inferior glenoid bone loss. Furthermore, it has shown to have an excellent and very good intra- and inter-observer reliability, respectively.
References
Auffarth A, Mayer M, Kofler B, Hitzl W, Bogner R, Moroder P, Korn G, Koller H, Resch H (2013) The interobserver reliability in diagnosing osseous lesions after first-time anterior shoulder dislocation comparing plain radiographs with computed tomography scans. J Shoulder Elbow Surg 22(11):1507–1513. doi:10.1016/j.jse.2013.04.020
Bachy M, Lapner PLC, Goutallier D, Allain J, Hernigou P, Bénichou J, Zilber S (2013) Coracoid process x-ray investigation before Latarjet procedure: a radioanatomic study. J Shoulder Elbow Surg 22:e10–e14. doi:10.1016/j.jse.2013.06.016
Balg F, Boileau P (2007) The instability severity index score. A simple pre-operative score to select patients for arthroscopic or open shoulder stabilisation. J Bone Joint Surg Br 89(11):1470–1477. doi:10.1302/0301-620X.89B11.18962
Barchilon VS, Kotz E, Barchilon ben-Av M, Glazer E, Nyska M (2008) A simple method for quantitative evaluation of the missing area of the anterior glenoid in anterior instability of the glenohumeral joint. Skelet Radiol 37(8):731–736. doi:10.1007/s00256-008-0506-8
Bernageau J, Patte D, Debeyre J, Ferrane J (1976) Value of the glenoid profile in recurrent luxations of the shoulder. Rev Chir Orthop Reparatrice Appar Mot 62(2 Suppl):142–147
Bessiere C, Trojani C, Pelegri C, Carles M, Boileau P (2013) Coracoid bone block versus arthroscopic Bankart repair: a comparative paired study with 5-year follow-up. Orthop Traumatol Surg Res OTSR 99(2):123–130. doi:10.1016/j.otsr.2012.12.010
Bigliani LU, Newton PM, Steinmann SP, Connor PM, McLlveen SJ (1998) Glenoid rim lesions associated with recurrent anterior dislocation of the shoulder. The Am J Sports Med 26(1):41–45
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1(8476):307–310
Boileau P, Villalba M, Hery JY, Balg F, Ahrens P, Neyton L (2006) Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am 88(8):1755–1763. doi:10.2106/JBJS.E.00817
Burkhart SS (2007) The bare spot of the glenoid. Arthrosc J Arthrosc Rel Surg 23(4):449. doi:10.1053/jars.2000.7794 author reply 449–450
Burkhart SS, Danaceau SM (2000) Articular arc length mismatch as a cause of failed Bankart repair. Arthrosc J Arthrosc Rel Surg 16(7):740–744. doi:10.1053/jars.2000.7794
Cohen J (1988) Statistical power analysis for the behavioral sciences, 2nd edn. L. Erlbaum Associates, Hillsdale
Edwards TB, Boulahia A, Walch G (2003) Radiographic analysis of bone defects in chronic anterior shoulder instability. Arthrosc J Arthrosc Rel Surg 19(7):732–739
Fleiss JL, Levin B, Paik MC (2003) Statistical methods for rates and proportions. Wiley series in probability and statistics, 3rd edn. Wiley, Hoboken
Gerber C, Nyffeler RW (2002) Classification of glenohumeral joint instability. Clin Orthop Relat Res 400:65–76
Greis PE, Scuderi MG, Mohr A, Bachus KN, Burks RT (2002) Glenohumeral articular contact areas and pressures following labral and osseous injury to the anteroinferior quadrant of the glenoid. J Shoulder Elbow Surg 11(5):442–451
Griffith JF, Yung PS, Antonio GE, Tsang PH, Ahuja AT, Chan KM (2007) CT compared with arthroscopy in quantifying glenoid bone loss. AJR Am J Roentgenol 189(6):1490–1493. doi:10.2214/AJR.07.2473
Huysmans PE, Haen PS, Kidd M, Dhert WJ, Willems JW (2006) The shape of the inferior part of the glenoid: a cadaveric study. J Shoulder Elbow Surg 15(6):759–763. doi:10.1016/j.jse.2005.09.001
Itoi E, Lee SB, Berglund LJ, Berge LL, An KN (2000) The effect of a glenoid defect on anteroinferior stability of the shoulder after Bankart repair: a cadaveric study. J Bone Joint Surg Am 82(1):35–46
Jankauskas L, Rudiger HA, Pfirrmann CW, Jost B, Gerber C (2010) Loss of the sclerotic line of the glenoid on anteroposterior radiographs of the shoulder: a diagnostic sign for an osseous defect of the anterior glenoid rim. J Shoulder Elbow Surg 19(1):151–156. doi:10.1016/j.jse.2009.04.013
Kim SH, Ha KI, Cho YB, Ryu BD, Oh I (2003) Arthroscopic anterior stabilization of the shoulder: two to six-year follow-up. J Bone Joint Surg Am 85-A(8):1511–1518
Latarjet M (1958) Technic of coracoid preglenoid arthroereisis in the treatment of recurrent dislocation of the shoulder. Lyon Chir 54:604–607
Lazarus MD, Sidles JA, Harryman DT, Matsen FA (1996) Effect of a chondral-labral defect on glenoid concavity and glenohumeral stability. A cadaveric model. J Bone Joint Surg Am 78(1):94–102
Magarelli N, Milano G, Sergio P, Santagada DA, Fabbriciani C, Bonomo L (2009) Intra-observer and interobserver reliability of the ‘Pico’ computed tomography method for quantification of glenoid bone defect in anterior shoulder instability. Skelet Radiol 38(11):1071–1075. doi:10.1007/s00256-009-0719-5
Mologne TS, Provencher MT, Menzel KA, Vachon TA, Dewing CB (2007) Arthroscopic stabilization in patients with an inverted pear glenoid: results in patients with bone loss of the anterior glenoid. Am J Sports Med 35(8):1276–1283. doi:10.1177/0363546507300262
Pansard E, Klouche S, Billot N, Rousselin B, Kraus TM, Bauer T, Hardy P (2013) Reliability and validity assessment of a glenoid bone loss measurement using the Bernageau profile view in chronic anterior shoulder instability. J Shoulder Elbow Surg 22(9):1193–1198. doi:10.1016/j.jse.2012.12.032
Pavlov H, Warren RF, Weiss CB Jr, Dines DM (1985) The roentgenographic evaluation of anterior shoulder instability. Clin Orthop Relat Res 194:153–158
Sommaire C, Penz C, Clavert P, Klouche S, Hardy P, Kempf JF (2012) Recurrence after arthroscopic Bankart repair: Is quantitative radiological analysis of bone loss of any predictive value? Orthop Traumatol Surg Res OTSR 98(5):514–519. doi:10.1016/j.otsr.2012.03.015
Sugaya H, Moriishi J, Dohi M, Kon Y, Tsuchiya A (2003) Glenoid rim morphology in recurrent anterior glenohumeral instability. J Bone Joint Surg Am 85-A(5):878–884
Tauber M, Resch H, Forstner R, Raffl M, Schauer J (2004) Reasons for failure after surgical repair of anterior shoulder instability. J Shoulder Elbow Surg 13(3):279–285. doi:10.1016/S1058274604000254
Conflict of interest
No funds were received in support of this study. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maqdes, A., Chammai, Y., Lengert, R. et al. The intra- and inter-observer reliability of the CT-scan based X index to quantify glenoid bone loss in chronic anterior shoulder instability and its impact on decision making. Eur J Orthop Surg Traumatol 25, 699–703 (2015). https://doi.org/10.1007/s00590-014-1546-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-014-1546-5