Abstract
We describe our experience with a new system of patient-specific template called Personal Fit®, which is unique in shoulder surgery and used in combination with Duocentric® prosthesis. The reverse prosthesis’s concept is the invention of Paul Grammont, developed with Grammont’s team of Dijon University as from 1981, which led to the first reversed total shoulder prosthesis called Trumpet in 1985. The Duocentric® prosthesis developed in 2001 is the third-generation prosthesis, coming from the Trumpet and the second-generation prosthesis Delta® (DePuy). This prosthesis provides a novel solution to the notching problem with an inferior overhang integrated onto the glenoid baseplate. Personal Fit® system is based on reconstructing the shoulder joint bones in three dimensions using CT scan data, placing a landmark on the scapula and locating points on the glenoid and humerus. That will be used as a reference for the patient-specific templates. We study the glenoid position planned with Personal Fit® software relative to native glenoid position in 30 cases. On average, the difference between the planned retroversion (or anteversion in one case) and native retroversion was 8.6°.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In this paper, we describe our experience with a new system of patient-specific templates, called Personal Fit®, which are unique in shoulder surgery and used in combination with the Duocentric® prosthesis.
This innovation adds to the original characteristics of the glenoid baseplate component:
-
Spherical inferior overhang to prevent scapular notching
-
Fixation peg of various sizes to preserve the glenoid bone stock and adjustable length to reinforce the fixation if needed (e.g., glenoid wear and revision surgery).
History of the reverse prosthesis
Paul Grammont devised and established the mechanical principle of reversal in 1981. This was a watershed moment in prosthesis surgery for the treatment for shoulder arthritis and large rotator cuff tears (rotator cuff tear arthropathy). At that point, poor results with the anatomical prosthesis in these indications had been a unanimous finding.
This principle consisted of medializing and lowering a single center of rotation, which is fixed on the surface of the glenoid [1, 2]. It appeared in Grammont’s philosophy, developed in 1975, which set out that functional shoulder surgery should not be constrained by the need to exactly reproduce the anatomy.
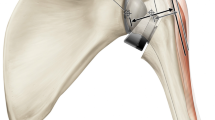
The work pursued by the Dijon team, along with the integration of comparative anatomy data, led to the principle being validated on a Strasser-type experimental model. In 1985, the first modern reverse shoulder prosthesis requiring only the deltoid muscle, called the “Trumpet,” was introduced (Fig. 1).
This prosthesis had only two components: a short, cemented humeral base made of polyethylene and a glenoid piece that consisted of two-thirds of a 44-mm sphere (the only diameter available) embedded and cemented into the glenoid.
Based on the original principle, many reverse prostheses were developed in the 1990s. Despite the unanimously recognized advantage of reversal on the range of motion, some specific problems appeared that induced a break in the survival curve for this type of prosthesis after about 7 years [3, 4]. The most common problem was scapular notching.
-
1.
Notching of the scapular pillar results from impingement of the medial edge of the humeral insert under the glenosphere during arm adduction. Even if the presence of notching does not necessarily have any negative clinical consequences [5], the incidence is high—from 49 to 70 % after an average follow-up of 10 years [6, 7]. Patients with a certain glenoid–scapular neck morphology seem to be more predisposed to this impingement—a short-neck glenoid (Fig. 2) limits motion during adduction more than a long-neck glenoid (Fig. 2) [8]. This induces polyethylene wear, bone destruction, occasional impingement with the inferior screw and can lead to loosening of the glenoid baseplate over the long-term and failure of the arthroplasty (4.1 % rate of loosening at a follow-up of 4.3 years [9] up to 17 % at an average follow-up of 10 years [7]). As a consequence, many have insisted that notching should be prevented. Some of the suggestions have included changing the glenoid position by lowering and tilting it, changing the inclination of the humeral cut or adding a glenoid graft. These proposals were not without secondary risks, such as acromion fracture, instability, and loss of medialization [6]. Last but not least, new prosthesis designs have been put forward to solve the notching problem.
-
2.
Loosening of the glenoid component, which has an average rate of 4 % at a follow-up of 4 years [10, 11], can also result in abnormal loads being generated secondary to poor intraoperative positioning of the glenoid. Precise control over prosthesis implantation and fixation is essential [9, 12, 14].
-
3.
Dislocation is the main aseptic complication, along with glenoid loosening, of reverse total shoulder arthroplasty. Its frequency ranges from 1.6 to 8.5 % in various published studies [13]. The risk of superolateral instability is greater with a smaller neck-shaft angle (Fig. 3). Other factors such as the surgical approach, lateral humerus position, size of the humeral baseplate, or size of the glenohumeral space seem to more or less contribute to the dislocation risk.
The Duocentric® prosthesis
To get around these problems, we started developing the Duocentric® reverse prosthesis (Aston Medical) in 2001. These efforts led to the first implantation of a third-generation prosthesis called the Duocentric® prosthesis in 2003, as a follow-on to the “Trumpet” and Delta® (DePuy). After a few more improvements, the Duocentric® Expert Reversed became available in 2007.
This prosthesis provides a novel solution to the notching problem—an inferior overhang integrated onto the glenoid baseplate (Fig. 4) places a protective resurfacing shield over this critical area in the scapular pillar at the start of elevation. This overhang also increases the primary stability of the implant by counteracting the shearing forces at the implant–glenoid interface. But this modification requires a brief historical look back for context. With the first-generation reverse prosthesis (Fig. 1), notching was minimal, rare, and non-progressive since its two-thirds sphere design automatically provided this resurfacing (“prevention without knowing it…”). This complication only truly appeared once a one-half sphere was used in the second-generation, Delta-type prosthesis.
Several short- and medium-term clinical studies with the Duocentric® have already demonstrated the beneficial effect of this inferior overhang on the notching rate. The rate decreased significantly from an average of 35 % in published reverse prosthesis studies [9] to 0.5 % with a follow-up of 1–3 years according to the results of the series of Gonzalvez (Dijon Shoulder Days, 2010—unpublished data) and those of Kany [3].
Other than its unique inferior overhang, this prosthesis also has a low metaphysis volume, a cemented or cementless stem with a self-stabilizing cross-sectional shape, a 145° neck-shaft angle, which is a compromise between stability and mobility, a removable baseplate that is aligned using the 125° humeral cut and a glenoid baseplate that is fixed with a breakaway peg and three screws. The glenoid baseplate has a porous dual layer titanium–hydroxyapatite coating (Fig. 5).
These features have been devised to increase the active range of motion, limit the risks of dislocation and glenoid loosening, and meet the primary objective of reducing the notching effect.
The standard Duocentric® instrumentation also contributes to achieving these goals by making it easier to implant the glenoid baseplate in the lower part of the glenoid bone and by preparing the seat of the inferior overhang.
However, surgical experience has shown that glenoid positioning remains challenging because of difficult access, reduced intraoperative visibility, and variable anatomy [15]. The optimal areas to anchor the fixation elements (peg, screws) are also difficult to determine preoperatively based on two-dimensional imaging.
Thus, we continued to improve the Duocentric® prosthesis by coming up with a system that would more precisely adjust the position of the glenoid baseplate and its fixation elements, and also the position of the humerus relative to the glenoid. Called PERSONAL FIT®, this is the first custom template system available for total shoulder arthroplasty.
Personal Fit®, a unique planning and execution system of patient-specific templates for reverse shoulder arthroplasty
Using the Personal Fit® system allows the surgeon to not only plan the size and position of the various Duocentric® prosthesis components, but also to compare the joint geometry with and without a prosthesis in three planes, based on the chosen components. This planning triggers the manufacturing of two templates that are personalized to the patient (Patient Specific Templates or PST). One automatically positions the center of the glenoid component and the orientation of its anchoring peg; the other sets the height and retroversion of the humeral head cut.
Foundations of Personal Fit®
Personal Fit® is based on reconstructing the shoulder joint bones in three dimensions using CT scan data, placing a landmark on the scapula, and locating points on the glenoid and humerus that will be used as a reference when the user positions the prosthesis components (Figs. 6, 7, 8, 9, 12, 13).
The center of the glenoid (CG) is obtained by establishing a point, GA or GP (depending on the glenoid wear), then tracing a line perpendicular to GS-GI that goes through this point.
These landmarks are used to calculate the inclination and retroversion of the native glenoid and the glenoid prosthesis component (Figs. 10, 11, 12, 13, 14, 15, 16).
Planning steps
The planning for a reverse prosthesis and the preparation of personalized templates with the Personal Fit® system consist of the following steps:
-
1.
If this is the surgeon’s first time using the system, he/she will log on to the www.duocentric-expert.com Web site to create a user account.
-
2.
Creation of surgical procedure for patient: patient information and surgery information; planning and templates can be made for the glenoid only or for the glenoid and humerus.
-
3.
Patient gets CT scan according a specific Aston Medical protocol that is sent to the radiologist; upload of digital image files onto a secure external server; three-dimensional reconstruction of the joint by Aston Medical.
-
4.
Surgeon receives email notification that the planning can be performed.
-
5.
Planning for glenoid component (Fig. 17): on the screen, the surgeon can see a glenoid baseplate in the “zero” position, which corresponds to the center of the baseplate being superimposed over the center of the native glenoid (Fig. 6) and with zero degrees of inclination and retroversion; the user can successively change the size of the glenoid baseplate and the length of the central peg, its inclination, and retroversion (while using the inclination and retroversion of the native glenoid as a reference, Figs. 10, 11) along with its depth and height, to find the best location for the inferior overhang and fixation points (peg and screws).
-
6.
Approval of glenoid planning if only a glenoid template is being made; if both glenoid and humerus templates are being made, this planning will be approved on the final analysis screen (Fig. 19).
-
7.
Planning for humeral component (Fig. 18): on the humeral planning screen, the surgeon can see the humeral stem in the “zero” position, which corresponds to a 125° humeral resection through the lowest part of the humeral head (Fig. 16) and zero degrees of inclination and retroversion. The humeral baseplate is also in its default neutral position; the user can progressively set the size of the stem, height, and position of the baseplate (for best coverage of the humeral cut surface) and the retroversion and height of the humeral cut (Figs. 15, 16).
Once both the humeral and glenoid parameters have been set, the full prosthesis configuration will be visible on the analysis screen (Fig. 19).
-
8.
Mathematical calculation of the relative position of the entire bone-prosthesis unit as planned (Fig. 19): this screen shows the distance in the three planes between the position of the planned joint center (the center of the glenoid baseplate) and the native joint center without the prosthesis (center of the humeral head); it also gives the amount of humerus lateralization between its initial position and its planned position, with the latter being based on an analysis with the default standard insert; the surgeon can change the amount of lateralization by changing the thickness of the insert.
-
9.
If the final analysis is suitable, the surgeon approves the glenoid and humeral planning simultaneously on this screen.
-
10.
An email is sent with the planning report that indicates the planned implant size and position; this planning report serves as a medical prescription for two patient-specific templates being made as a result of this planning.
-
11.
Once this signed document is received by Aston Medical, manufacturing of the custom templates is initiated (Fig. 20). The glenoid template will automatically show the planned center of the glenoid baseplate, which will become the joint center of rotation. The humeral template will allow fixation of the humeral cutting guide at the height and orientation chosen in the transverse plane.
-
12.
Custom templates delivered to the health facility in non-sterile bags; autoclave sterilization is required.
The full process of planning and preparing the custom templates requires at least 5 weeks from the date the CT scan files are uploaded to when the templates are delivered to the health facility.
Surgery
Humeral phase
After the humeral head is exposed, the humeral template is put into place on its lone possible position before any osteophytes are removed. The cutting guide will be placed up against the template and then fixed, which automatically places it at the appropriate height and orientation (Fig. 21). The humeral template thus replaces the invasive centromedullary guide and the need to visually align the cutting guide when using the standard technique. The template is then removed, while leaving the cutting guide in place. The humeral cut is then performed and the surgical technique resumes using the standard Duocentric® instrumentation.
Glenoid phase
The glenoid is exposed. Osteophytes are not removed before placing the glenoid template in the lone possible position. A drill bit is passed through this template (Fig. 22) to reproduce the center of rotation corresponding to the chosen center of the final glenoid baseplate. This replaces the metal gauge in the instrumentation that had to be visually aligned on the glenoid when using the standard technique. The glenoid preparation resumes with the reamer and the inferior cutting gauge; both are automatically centered on the point designated by the template.
Since the planning software was made available in September 2011, about fifty shoulder arthroplasty cases have been performed using the glenoid template; the humeral template has been available since September 2012.
Initial data from the Personal Fit® system
Because the Personal Fit® system is so new, we obviously cannot determine its contribution to the clinical results with the Duocentric® prosthesis.
However, the available database can be explored to determine the following:
-
Planned position of the prosthesis based on the three-dimensional information available on the native glenoid; position compared with the one the surgeon would naturally have chosen during the surgery without the aid of the three-dimensional planning system [10].
-
Distance between the position of the final glenoid baseplate and the position of the planned glenoid baseplate.
Study of glenoid position planned with the Personal Fit® software relative to native glenoid position in 30 cases
Inclination results (Fig. 23):
-
1.
The average native inclination was 6.5° upwards. The average planned inclination was 4.2° upwards. Thus, in most cases, the surgeons planned to reduce the native glenoid inclination.
-
2.
In 10 cases (shown in red numbers on histogram below), the planning was performed to tilt the prosthesis upwards relative to the patient’s anatomy. In half of these cases, the native inclination was either downward or neutral (blue numbers on histogram below).
-
3.
On average, there was a 5.3° difference between the planned inclination and the native inclination.
Retroversion results (Fig. 24):
-
1.
The native glenoids are all retroverted, with an average of 10.7° retroversion.
-
2.
In most cases, the surgeons planned to reduce the retroversion angle since they refer themselves to the scapular plane, while they intuitively position themselves at the visible glenoid plane and, for 17 cases, planned for a neutral retroversion (red numbers on histogram below). The average planned retroversion was 2.1°.
-
3.
One prosthesis was planned with 5° of anteversion (blue number on histogram below).
-
4.
On average, the difference between the planned retroversion (or anteversion in one case) and native retroversion was 8.6°.
Conclusion for this study: Having three-dimensional information available for the glenoid led us to plan a slightly lower and slightly less retroverted component position than the native glenoid to optimize the anchoring areas for the baseplate (peg) and screws. Because of the inferior overhang on the glenoid baseplate, the baseplate does not need to be tilted downward.
Study of the distance gap between the true position of the glenoid implant and its planned position in five cases
This study required a postoperative CT scan of the shoulder to be performed and special image processing to be carried out to remove the artifacts induced by the metal prosthesis. Thus, it was performed on a smaller cohort of patients.
Results of the implant size and position
-
1.
For the five cases in question, the size of the implanted glenoid baseplate and the length of its peg corresponded to the ones planned.
-
2.
The center of the implanted glenoid baseplate is horizontally and vertically positioned within 1 mm of the position determined during the planning.
-
3.
The retroversion between the implanted baseplate and the planned baseplate differed by an average of 2.5°, either by decreasing or increasing the native retroversion.
-
4.
The inclination (tilt) differed by 4° on average.
To summarize this part of the study, the Personal Fit® system provided good repeatability of the implant size and especially of the position of the joint center between the planning stage and actual implantation.
Conclusions and future perspectives
Through its design, the Duocentric® prosthesis is the first to provide an effective solution to the impingement that leads to notching. It is also the first one up to now that can be implanted using patient-specific templates that are intended to optimize placement of the prosthesis components, thus contribute to reducing the risk of glenoid loosening and dislocation. The system will be even more useful in cases of severe shoulder deformity or significant glenoid bone defects.
The limitations of the current system revolve around the standard instrumentation not making use of all the parameters resulting from the planning. In particular, the reaming and implantation of the glenoid baseplate are not guided by the orientation of the glenoid plane. Thus, the Duocentric®/Personal Fit® concept will continue to be refined along these lines.
Another improvement will consist of adding a kinematics module to the planning software that will automatically calculate the range of motion of the shoulder with the prosthesis (particularly external rotation because it is often reduced with a reverse prosthesis) and potential implant–scapula impingement areas during the last planning step.
Regular follow-up of patients with an implanted Duocentric® Expert Reversed prosthesis that was implanted with and without customized templates will allow us to:
-
provide longer-term validation of the soundness our implant-related choices, and
-
measure the true contribution of the new technology (personalized templates) to shoulder arthroplasty surgery.
References
Grammont P, Trouilloud P, Laffay JP, Deries X (1987) Study and production of a new shoulder prosthesis. Rhumatologie 39:17–22 (Article in French)
Grammont P, Baulot E (1993) Delta shoulder prosthesis for rotator cuff rupture. Orthopedics 16:65–68
Kany J, Gonzalvez M, Trouilloud P, Baulot E, Handelberg F (2008) Predictive factors for the occurrence of notching in reverse total prosthesis. 82th annual meeting of the S.O.F.C.O.T (Abstract in French)
Nyffeler R (2010) Personal experiences with inverse shoulder arthroplasty. Lead Opin Orthop Rheumatol 4
Zumstein A, Pinedo M, Old J, Boileau P (2011) Problems, complications, reoperations, and revision in reverse total shoulder arthroplasty: a systematic review. JSES 20(1):146–157
Smith D, Guyver T, Bunker TD (2012) Indications for reverse shoulder replacement. JBJS (Br) 94-B(5):577–583
Baulot E, Bouacida A, Labattut L, Trouilloud P (2011) Glenoid fixation and scapular pillar notching in reverse shoulder arthroplasty: radiology results with an average 10-year follow-up of the Delta prosthesis. Rev Chir Orthop 97(suppl no 7):S291 (Abstract in French)
Baulot E, Trost O, Demangel A, Trouilloud P (2006) Scapular neck: myth or reality? Application to glenoid cavity surgery. Morphologie 90:289 (Article in French)
Mole D, Favard L (2006) Eccentric glenohumeral OA. Symposium, 80th annual meeting of the S.O.F.C.O.T (Article in French)
Favard L, Oudet D, Huguet D, Sirveaux F, Mole D (2008) Results of anatomical and reverse prostheses for eccentric glenohumeral OA. Instructional courses, 82th annual meeting of the S.O.F.C.O.T (Article in French)
Augereau B (2010) Total prosthesis for degenerative shoulder pathologies. E-Mémoires de l’Académie nationale de chirurgie 9(2):69–75 (Article in French)
Valenti PH, Katz D (2005) How to implant a reverse shoulder prosthesis. Maitrise Orthopédique No. 148 (Article in French)
Valenti PH (2009) Unstable reverse prosthesis: diagnosis, treatment, prevention. Venus Course, Lorient (Article in French)
Frankle MA, Teramoto A, Luo ZP, Levy JC (2009) Glenoid morphology in reverse shoulder arthroplasty; classification and surgical implication. J Shoulder Elbow Surg 18(6):874–885
Landau JP, Hoenecke HR (2009) Genetic and biomechanical determinants of glenoid version: implications for glenoid implant placement in shoulder arthroplasty. J Shoulder Elbow Surg 18:661–667
Conflict of interest
No funds were received in support of this study. The authors, except P. Martz, are designers and inventors of the Duocentric® reverse prosthesis.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Trouilloud, P., Gonzalvez, M., Martz, P. et al. Duocentric® reversed shoulder prosthesis and Personal Fit® templates: innovative strategies to optimize prosthesis positioning and prevent scapular notching. Eur J Orthop Surg Traumatol 24, 483–495 (2014). https://doi.org/10.1007/s00590-013-1213-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-013-1213-2