Abstract
Purpose
It is questionable whether an annular tear (AT) is a predictor for accelerated degeneration of the intervertebral discs. The aim of the present study was to answer this question via a matched case–control study design that reliably eliminates potential confounders.
Materials
Presence or absence of AT, defined as a hyperintense lesion within the annular fibrosus on T2-weighted non-contrast MRI images, was documented in 450 intervertebral lumbar discs of 90 patients who could be followed up for at least 4 years with MRI. Discs with an AT (n = 36) were matched 1:1 to control discs according to the level, degree of initial disc degeneration on MRI (both Pfirrmann grade median 4, range 3–4), age (59.5 ± 15.0 versus 59.3 ± 14.6 years), BMI (26.7 ± 4.4 versus 26.9 ± 4.4 kg/m2) and interval to the follow-up MRI (4.8 ± 0.9 versus 5.1 ± 0.8 years). The degree of disc degeneration after a minimum of 4 years was graded on the follow-up MRI in both groups according to the Pfirrmann classification.
Results
One-fourth (25 %) of the 36 discs with an AT on the initial MRI exam progressed in degeneration. This was similar to the rate of the matched control discs with no AT, in which also around one-fourth (22 %) showed a progression of degeneration (p = 1.00), also without any difference in the degree of degeneration.
Conclusion
Discs with a Pfirrmann grade >2 with an AT, defined by a hyperintense signal intensity on MRI, are not prone to accelerated degeneration if compared to discs without an AT. Therefore, the presence of an AT per se does not predict accelerated disc degeneration.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
An annular tear (AT) is defined as a rupture of the annular fibrosus with a consequent protrusion of the nucleus pulposus and initially described as a lesion containing fluid or mucoid material [1]. While ATs of the intervertebral disc have been associated with discogenic low back pain [2–4], they can also be detected in asymptomatic individuals [5]. It has been suggested that the presence of AT influences the speed of disc degeneration [6] and should therefore be included in the clinical decision-making process; however, this is a point of debate because of an insufficient amount of evidence. This lack of evidence is in part a result of the historic challenge in identification of ATs on radiographic exams. Initially, discography was the only imaging modality able to detect AT. Subsequently, CT-discography evolved and is still considered as the most sensitive and specific imaging modality, particularly to detect AT in early stages of disc degeneration [7, 8]. CT-discography is still known as the most specific imaging modality and remains the only pain-provocative test [7, 9], but simultaneously shows high false-positive rates [7].
Today, MRI is the most commonly performed diagnostic imaging modality in early diagnostic management of back pain because of the demonstration of high soft tissue contrast, the absence of radiation dose, and its noninvasive nature. A hyperintense signal intensity zone within the annular fibrosis on water-sensitive images is considered diagnostic of AT on MRI.
Long-term follow-up studies investigating the main question of interest, namely whether or not the detected AT promote accelerated disc degeneration, are lacking. The study hypothesis was that high signal intensity zones within the annular fibrosus, which define AT on MRI, are not predictive for faster subsequent disc degeneration if compared to control discs with otherwise similar disc degeneration grade.
Materials and methods
Patients
The Institutional Review Board approved this retrospective study. Subjects who had a lumbar spine MRI performed between January and June 2012 with a previous lumbar spine MRI more than 4 years apart, were retrieved from the picture archive and communication system (PACS). Patients with prior lumbar spine surgery were excluded. A total number of 90 subjects met the inclusion criteria of the present study.
Imaging analysis
Standard MRI protocols were used and patients were scanned with either a 1.5- or 3-T MRI system (GE health care, USA). A standard 1.5-T MR image protocol is summarized in Table 1.
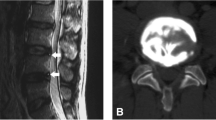
All MRI images were reviewed by one radiologist (with more than 5 years of radiology training and more than 6 months of dedicated musculoskeletal radiology training) on the PACS workstation (Sectra IDS7, Version 12.5.0.234, Sweden) who evaluated the 450 disc levels for presence or absence of AT and who graded disc degeneration according to the Pfirrmann classification [10] (Table 2). An AT was defined as a hyperintense zone within the annulus fibrosis, detectable on water-sensitive sequences only, such as T2-weighted or short tau inversion recovery (STIR) sequences (Fig. 1).
Sagittal T2w FSE images with a small AT at the level L4/5 (open arrow) that was visible: a at the initial MRI exam and b was no more detectable (open arrow) on the follow-up MRI exam 5 years later. The same disc demonstrated an advance in degeneration with disc extrusion over time. a In contrast, another AT that was detectable at the level L5/S1 (arrow), which remained b unchanged on the follow-up MRI exam 5 years later without any progression in disc degeneration
Groups
The levels which demonstrated an AT on the initial MRI (n = 36) were matched to control discs according to their initial Pfirrmann grade (both median 4, range 3–4), level, mean interval age (59.5 ± 15.0 versus 59.3 ± 14.6 years), BMI (26.7 ± 4.4 versus 26.9 ± 4.4 kg/m2) and interval of MRI scans (4.8 ± 0.9 versus 5.1 ± 0.8 years) (Table 3). All levels which demonstrated disc degeneration grade 5 according to the Pfirrmann classification [10] at the initial MRI exam were excluded as further progression of disc degeneration would not be measurable. Also, to avoid the potential of undetected ATs in the control discs [11], herniated nucleus pulposus were excluded from the matched control cohort and further analysis.
For subgroup analysis, discs with an AT at the initial MRI, that were still present at the follow-up MRI (stable AT subgroup), were separated from those AT that were no longer detectable at the follow-up MRI exam (regression AT subgroup). Both subgroups were separately compared to their respective matched controls.
Statistical analysis
Statistical analysis was performed using the software PRISM [Version 6, Graphpad software, La Jolla (CA), USA]. Data were tested for normality with the D’Agostino and Pearson omnibus normality test. Potential differences in the matched groups were tested for significance using either Student’s t test for normally distributed data or a Man–Whitney test for non-parametric data. For binary intergroup comparison, Fischer’s exact tests or Chi-square tests were used depending on the sample sizes. Non-parametric data are reported with median and range, while parametric data are reported with mean ± standard deviation (SD). A p value of <0.05 was defined as statistically significant.
Results
AT versus controls
Of the 36 levels with AT on the initial MRI exam, only 9 (25 %) demonstrated progression in disc degeneration according to the Pfirrmann grades; 3 discs from grade 3 to 4 and an additional 6 discs from grade 4 to 5. In comparison, eight of the matched controls (22 %) also demonstrated progression in disc degeneration (p = 1.00, OR = 0.86); four from grade 3 to 4, three from grade 4 to 5, and one from grade 3 to 5.
Stable AT group versus controls
Fifteen discs demonstrated ATs on both the initial MRI exam and on the follow-up MRI exam. Of those, six showed progression of disc degeneration (three from grade 3 to 4 and three from grade 4 to 5), also not different if compared to four of the matched controls that showed progression (two from grade 3 to 4 and two from grade 4 to 5) (p = 0.70, OR = 1.83).
Regression AT group versus controls
Twenty-one ATs that were present on the initial MRI were not detectable anymore at the follow-up MRI exam. Of those, only three discs (14 %, 3/21) showed progression in degeneration (all from grade 4 to 5), also not statistically different to the matched control discs with four cases (19 %, 4/21; two from grade 3 to 4, one from grade 4 to 5 and one from grade 3 to 5) that also showed progression of degeneration (p = 0.45, OR 0.42).
Discussion
This study aimed to investigate whether the presence of an AT, defined as a hyperintense zone within the annular fibrosus, is predictive for accelerated disc degeneration or not. The results demonstrate that a high signal intensity zone within the annular fibrosus, is not predictive for faster subsequent disc degeneration if compared to matched control discs. The study design with matching of disc levels, the initial grade of degeneration, age, BMI and gender of the patient allowed to eliminate the most important confounders [12] and the long-term follow-up allowed to observe relevant degenerative changes that evolve over time. To the best knowledge of the authors, the only other available long-term study focusing on ATs and disc degeneration provides a mean follow-up period of 31.8 months [6]. It reports that ATs occur early in DD and are associated with faster disc degeneration. The discrepancy to our results might be due to the use of a non-matched study design and with a different definition of AT on MRI [6].
Although we believe that the results of the herein presented matched case–control study clearly demonstrate that the presence of an AT on non-contrast MRI is not predictive for accelerated DD, certain methodological limitations need consideration in interpretation of the results.
The interreader agreement for the detection of AT on MRI is well known [13] and was therefore not repeated in this study.
We were aware of ATs that might undergo healing processes, resulting in granulation tissue that might not be detected with non-contrast images [11]. Since non-contrast images are performed as an initial evaluation of back pain in most institutions in daily clinical routine, the aim of this study was not to detect the entire spectrum of ATs, but to determine if a detected hyperintense zone within the annular fibrosus (as detectable on standard MRI) is a predictor for accelerated progression of disc degeneration.
Furthermore, since our cohort only included disc degeneration grades 3 or higher according to the Pfirrmann classification [10] showing AT, it remains still unknown if an AT might be seen in the setting of disc degeneration of grade 2 or lower according to the Pfirrmann classification [10]. As an AT causes disruption of the annular fibrosus, it seems plausible that some sort of protrusion and therefore some disc height loss must be associated, and as disc degeneration grade 1 and 2 show no disc height loss according to the Pfirrmann classification, we believe that ATs are not common in the setting of grade 1 and 2 disc degeneration.
Finally, all subjects of this study received an MRI because of either lower back pain or radiculopathic symptoms. As a result, this study cannot make any statements regarding the association of presence of ATs and disc degeneration in asymptomatic patients. This can also be considered as a minor limitation in the importance of the findings as the study aimed to answer a common question of clinicians, namely whether the presence of a detected AT predicts faster disc degeneration in a patient with a disc degeneration or not. Further, the aim of this study was not to answer whether the presence of ATs predict accelerated deterioration of clinical symptoms. Neither ATs nor disc degeneration present with a biunique clinical sign and therefore, quantification of the symptomatic consequence would be subject of multiple biases.
Conclusion
A high signal intensity zone within an annulus fibrosus, namely an AT on standard MRI, is not a predictor for accelerated disc degeneration and should therefore per se not affect clinical decision-making.
References
Yu SW, Sether LA, Ho PS et al (1988) Tears of the anulus fibrosus: correlation between MR and pathologic findings in cadavers. AJNR Am J Neuroradiol 9:367–370
Park WM, McCall IW, O’Brien JP, Webb JK (1979) Fissuring of the posterior annulus fibrosus in the lumbar spine. Br J Radiol 52:382–387. doi:10.1259/0007-1285-52-617-382
DePalma MJ, Lee J-E, Peterson L et al (2009) Are outer annular fissures stimulated during diskography the source of diskogenic low-back pain? An analysis of analgesic diskography data. Pain Med 10:488–494. doi:10.1111/j.1526-4637.2009.00602.x
Peng B, Hou S, Wu W et al (2006) The pathogenesis and clinical significance of a high-intensity zone (HIZ) of lumbar intervertebral disc on MR imaging in the patient with discogenic low back pain. Eur Spine J 15:583–587. doi:10.1007/s00586-005-0892-8
Carragee EJ, Paragioudakis SJ, Khurana S (2000) 2000 Volvo Award winner in clinical studies: lumbar high-intensity zone and discography in subjects without low back problems. Spine 25:2987–2992
Sharma A, Pilgram T, Wippold FJ (2009) Association between annular tears and disk degeneration: a longitudinal study. AJNR Am J Neuroradiol 30:500–506. doi:10.3174/ajnr.A1411
Bernard TNJ (1990) Lumbar discography followed by computed tomography: refining the diagnosis of low-back pain. Spine 15:690
Osti OL, Fraser RD (1992) MRI and discography of annular tears and intervertebral disc degeneration. A prospective clinical comparison. Bone Joint J 74:431–435
Kornberg M (1989) Discography and magnetic resonance imaging in the diagnosis of lumbar disc disruption. Spine 14:1368
Pfirrmann CW, Metzdorf A, Zanetti M et al (2001) Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine 26:1873–1878
Ross JS, Modic MT, Masaryk TJ (1990) Tears of the anulus fibrosus: assessment with Gd-DTPA-enhanced MR imaging. AJR Am J Roentgenol 154:159–162
Hilton RC, Ball J, Benn RT (1980) Annular tears in the dorsolumbar spine. Ann Rheum Dis 39:533–538. doi:10.1136/ard.39.6.533
Smith BMB, Hurwitz ELE, Solsberg DD et al (1998) Interobserver reliability of detecting lumbar intervertebral disc high-intensity zone on magnetic resonance imaging and association of high-intensity zone with pain and anular disruption. Spine 23:2074–2080
Acknowledgments
The following Grant supports are acknowledged: Department fund of the MRI Department, Hospital for Special Surgery, USA, and individual funding of Swiss National Foundation (N.F. PBZHP3_143674); individual funding of Swiss National Foundation (N.F. PBZHP3_143674).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Farshad-Amacker, N.A., Hughes, A.P., Aichmair, A. et al. Is an annular tear a predictor for accelerated disc degeneration?. Eur Spine J 23, 1825–1829 (2014). https://doi.org/10.1007/s00586-014-3260-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-014-3260-8