Abstract
Study design
A retrospective clinical study.
Objective
To evaluate the outcomes of two-level (T12 and L3) pedicle subtraction osteotomy (PSO) for severe thoracolumbar kyphosis in ankylosing spondylitis (AS), and to discuss the surgical strategies of this surgery.
Background
Cases were limited on the results of two-level PSO for correction of severe kyphosis caused by AS, nor on surgical strategies of this type of surgery.
Methods
From March 2006 to December 2010, nine consecutive AS patients with severe kyphotic deformity, underwent T12 and L3 PSOs. Chin-brow vertical angle (CBVA) and radiographic assessments which contain thoracic kyphosis (TK), lumbar lordosis (LL), global kyphosis (GK), and sagittal vertical axis were carefully recorded pre and postoperatively to evaluate the sagittal balance. Intra and postoperative complications were also registered. All patients were asked to fill out Oswestry Disability Index before surgery and at the last follow-up visit.
Results
All nine patients (8M/1F), averaged 41.4 years old (range 35–51 years), were received two-level (T12 and L3) PSO, and were followed up after surgery for a mean of 39.9 months (range 24–68 months). Good cosmetic results were achieved in all patients. Mean correction at two-level PSO was 67.9 ± 5.5°. All CBVA, TK, LL, and GK were changed significantly after surgery (P < 0.05), the mean amount of correction of which were 59.5 ± 13.8, 34.7 ± 3.8, 33.2 ± 2.4, and 54.0 ± 14.8 degrees, respectively, and with a small loss of correction at the last follow-up visit. Sagittal imbalance was significantly improved from 27.3 ± 4.4 to 3.4 ± 0.7 cm postoperatively. Neither mortalities nor any major neurological complications were found. The mean ODI score was significantly improved from 53.4 ± 15.5 before surgery to 8.2 ± 4.7 at the last visit.
Conclusion
The outcomes of follow-up showed that two-level (T12 and L3) PSO can effectively and safely correct severe thoracolumbar kyphosis in AS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ankylosing spondylitis (AS) is a common inflammatory rheumatic disease predominantly affecting the sacroiliac joints and spine [1, 2]. The interaction between chronic inflammation and spine is primarily characterized by progressive ossification of the spinal ligaments and facet joints, which eventually leads to a fixed and stiff spine accompanying with vertebral osteoporosis [3–6]. In late stage, AS is often associated with a sagittal deformity, resulting in deformed appearance cosmetically and a high degree of functional handicap of daily activity. This kyphotic deformity may make spine muscles under continuous strain and generate increasing back pain attributable to muscle fatigue [5]. The deteriorated thoracolumbar kyphosis even involves visceral compression resulting in intra-abdominal complications or impaired respiratory function [7].
Surgical treatment is always adopted to correct kyphosis in advanced AS, to reconstruct the spine sagittal balance and to restore the patient’s capacity to look straight ahead [5, 8]. Smith-Petersen osteotomy (SPO), pedicle subtraction osteotomy (PSO) and vertebral column resection (VCR) have been advocated and extensively used in orthopedic surgery, all of which manipulate the position of the spine by either lengthening or shortening a designated spinal column (anterior or posterior), for achieving a specific amount of correction. In 1945, Smith-Petersen first described SPO as an operative technique to correct kyphotic deformity secondary to AS [9], where once the appropriate osteotomy level is identified, the segmental structures of posterior column are removed bilaterally. Generally, approximately 10 degrees of correction can be obtained at each osteotomy level. And PSO, a V-shaped wedge resection of the vertebral body, involving bilateral pedicles and posterior elements, was first introduced to correct AS kyphosis by Thomasen in 1985 [10]. This type of osteotomy, typically performed at L2 or L3, which is the normal apex of lumbar lordosis, can obtain a correction of 30–40° at one osteotomized segment [3–5, 11–14]. While VCR is a formidable last resort technique reserved for the most tenacious spinal deformities which are not amenable to other osteotomy techniques such as the SPO or the PSO, it has been suggested for the treatment of spinal tumor, congenital kyphoscoliosis as well as for hemivertebrae excision [15].
In the clinical practice, for some AS patients presenting late to hospital with severe global thoracolumbar kyphotic deformity, one-level PSO usually cannot achieve the expected correction. Although VCR could obtain enough correction, it is not fully suitable for the treatment of global sagittal imbalance. Thus, some authors recommended two-level PSO to complement the correction insufficiency [5, 11, 12]. Yet still, these articles did not talk about surgical strategies of two-level PSO for severe AS kyphosis in detail. Therefore, we aim to evaluate the clinical outcomes regarding this procedure and discuss the surgical strategies of this orthopedic surgery.
Materials and methods
Patients
Nine AS patients (8M/1F), averaged 41.4 ± 5.7 years old (range 35–51), with a minimum 2-year follow-up after two-level (T12 and L3) PSO for AS-related kyphotic deformity, were reviewed between March 2006 and December 2010 (Table 1). Patients with pseudoarthrosis, fractures, or serious comorbidities were excluded. The chief complaint from patients was low back pain or inability to look straight ahead. Some patients with low bone mineral density acquired anti-osteoporosis treatment for 1–3 months before and after operation.
Radiologic and clinical assessment
Standing anteroposterior and lateral radiographs were performed before and immediately after operation, and at every follow-up visit (3 months, 6 months, 1 year, and 2 years after surgery). Radiologic measurements included: thoracic kyphosis (TK), lumbar lordosis (LL), global kyphosis (GK) and sagittal vertical axis (the horizontal distance from a vertical plumb line centered in the middle of the C-7 vertebra body to the posterosuperior corner of the S-1 endplate).
Chin-brow vertical angle (CBVA), defined as an angle measured between a line from the brow to the chin to the vertical while the patient stood with hips and knees extended [16], was registered using pre and postoperative clinical photographs of the patients.
Clinical outcome was assessed preoperatively and at the last follow-up visit using the Oswestry disability index (ODI) questionnaire [17].
Statistics analysis
The statistical analysis was performed using GraphPad Prism (Version 5.0 GraphPad software Inc, California, USA). Paired Sample t test was used to compare the pre and postoperative clinical and radiographic data with a significance level of 0.05 (P value). The results are reported as mean ± standard deviation (SD).
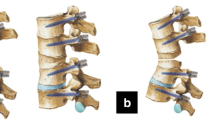
Surgical techniques
Fiberoptic intubation preceded the introduction of general anesthesia. Patients were placed in prone position on a special operating table (Fig. 1), which was flexed in a reverse V shape, to accommodate the severe kyphotic spine and to adapt simultaneously to the correction of kyphotic deformity while surgery proceeded. The spine was exposed through a standard posterior midline approach centering over the level of the osteotomy. The posterior elements were exposed by subperiosteal dissection as far laterally as the transverse processes. Transpedicular screws were inserted into at least two adjacent vertebrae levels proximal and distal to the osteotomy. T12 osteotomy was performed firstly. Meanwhile, the incision below the next osteotomy segment was temporarily closed with towel clip to reduce patients’ body temperature and blood loss as possible. The ribs on the affected level were transected 3–4 cm lateral to the costotransverse joint, and the pleura was bluntly separated from the vertebrae. The rib heads at the corresponding level, as well as the transverse process, were also carefully excised, remaining extrapleural. The posterior elements and pedicles were then resected (Fig. 2a). Partial laminectomy was performed at the adjacent vertebra to minimize any dural impingement at the time of PSO closure. Then the dura and bilateral nerve roots were exposed. A unilateral temporary short rod was mounted upon the pedicle screws opposite the osteotomy side to prevent sudden translation and inadvertent displacement. The dura and nerve root were gently retracted and protected with a nerve retractor. Then, a hole was drilled down through the identified pedicle into the vertebral body on the osteotomized side. The cancellous bone within the vertebral body was removed bilaterally with curettes and rongeurs in a wedge-shaped fashion, where the base and the apex were the posterior wall and the mid-point of anterior surface of the vertebra, respectively. Subsequently, the posterior wall of the osteotomized vertebra was pushed down into the wedge-shaped cavity with reversed-angle curette. Under direct vision of the dura and nerve roots, the osteotomy closure was carried out with the anterior cortex acting as a hinge. By repeatedly loosening and tightening the pedicle screws on the temporary rods and applying compressive forces on the adjacent screws, the osteotomy gap was completely obliterated (Fig. 2b). In the process of osteotomy closure, the operative table was gradually straightened. More attention was taken to check whether there was inadvertent translation of the vertebral column, or excessive dura buckling. Evaluate the residual degree of deformity correction assisted by X-ray fluoroscope. The same operative procedure was performed in next osteotomy level. In the end, the long permanent titanium rods were fixed with pedicle screws instead of temporary ones. During the entire process of osteotomy, effective use of thrombin-soaked gauze, gel foam or bone wax on the raw surface was critical if it bleeded profusely. Bone grafting was performed after bilateral laminae, transverse processes and facet joints above and below the osteotomy levels had been decorticated. Somatosensory-evoked and motor-evoked potentials were continuously monitored during operation. All patients underwent the intraoperative wake-up test after completing instrumentation. The patients were allowed to start walking 2 weeks after surgery and should entail immobilization with thoracolumbosacral orthosis for 3–6 months until the bony union.
Surgical decision making
Decision-making of two-level PSO was primarily dependent on the preoperative planning and intraoperative assessment. Preoperatively, the clinical examination could provide more valuable information than radiographs, of how much correction was desired to restore a balanced upright position, due to the compensation not inevitably observed on films. Correction of 30–40 degrees could usually be achieved by single-level PSO, as more correction was needed, two-level PSO was suggested and considered better. The designated osteotomy sites were located considering the type of kyphotic deformity, the location of the apical vertebrae, SVA, as well as the required correction. During the surgery, the amount of correction was first estimated after T12 osteotomy with an intraoperative lateral radiograph. Residual amount of correction was accomplished by L3 osteotomy. Proximally the instrumentation was always extended two levels above the most proximal level of osteotomy. And the instrumentation was stopped at L5 in patients with well-preserved L5-S1 disc. Otherwise, the instrumentation was extended to sacrum.
Results
Operative results
Two-level (T12 and L3) PSO was performed in all patients. The median operation time was 402.8 ± 50.3 min (range 320–490 min). The median bleeding was 3311 ± 523.1 ml (range 2100–3900 ml) (Table 2). All patients required 2–4 units of packed red blood cells transfusion and autologous blood transfusion intraoperatively.
Radiographic and clinical results
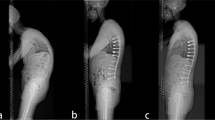
Radiological fusion was achieved in all patients at the final follow-up (Figs. 3c, 4c). Evidence of bridging trabeculae and absence of motion on dynamic films were regarded as conclusive evidence of fusion. No pseudarthrosis at the osteotomy sites, secondary junctional kyphosis at segment above proximal instrumented vertebrae or instrumentation failure were observed. The clinical and radiographic results were listed in Table 3. TK, LL, GK, SVA, and CBVA significantly differed between pre and postoperative images. At the final follow-up, all patients could look straight ahead but with some loss of sagittal balance (Figs. 3, 4).
A 38-year-old man with c-shaped thoracolumbar kyphosis and mild scoliosis underwent T12 and L3 PSOs and posterior fusion from T9 to L5. Note the marked improvement in both global sagittal balance and clinical appearances when comparing his pre and postoperative films. a Preoperative standing anteroposterior and lateral radiographs. b Standing anteroposterior and lateral radiographs immediately after operation. c Radiographic films at the final follow-up of 48 months. d Preoperative and ultimate postoperative clinical appearances
Images in a 35-year-old man with severe global thoracolumbar kyphotic deformity. a Preoperative lateral radiograph demonstrates that the patient with severe flexion kyphosis, lost the capacity to look straight ahead. b Postoperative lateral radiograph shows correction of kyphosis with T12 and L3 PSOs. c Postoperative imaging reveals stable sagittal correction at 3-year follow-up. d Clinical appearances after two-level PSO show correction of the thoracolumbar deformity and restoration of horizontal gaze
Complications
Neither neurologic nor vascular complications were found in our series. Perioperative complications included dural tear, subluxation of the osteotomy site and paralytic ileus (Table 4). Two dural tears occurred due to adhesion to the ossified ligamentum flavum. In these two cases, dura was sutured with spongostan placed on and full recovery was achieved at last. Sagittal subluxation was observed in one patient during the closure of L3 osteotomy. The spine was immediately stabilized with a temporary pre-bent rod to prevent further translocation at the osteotomy site. Then, reduction maneuvers were performed after checking the tension of the dura and nerve roots. Postoperatively, no complications were found in this patient. Four patients developed paralytic ileus, which resolved after gastric intubation and restriction of oral intake.
Clinical outcome
The mean ODI improved from 53.4 ± 15.5 before surgery to 8.2 ± 4.7 at the last visit (Fig. 5).
Discussion
Ankylosing spondylitis commonly affects the axial skeleton, leading to flattening of the normal lumbar lordosis and an exaggeration of the thoracic kyphosis. This deformity is functionally and psychologically disabling [18]. Therefore, surgical intervention should be adopted to correct deformity, to help the patient walk erect, and to improve balance and gait efficiency. Nowadays, PSO is a traditional and popular surgical technique for treatment of fixed sagittal deformity secondary to AS [3–5, 11–13, 19]. This type of osteotomy is carried through all three columns of the spine, obviating the need for anterior exposure and its associated complications. With its indications growing, PSO has been modified to treat some fixed sagittal plane deformities for a variety of disease states including tuberculosis, trauma, and postsurgical conditions [12, 20, 21]. In general, the mean correction of a standard lumbar PSO is about 35° [5]. Some authors have reported that more than 50° of correction for severe kyphotic deformity could be achieved with modified PSO [20, 22]. To date, however, only a few articles have reported the results of two-level PSO for AS kyphosis. In 2001, Chen et al. [11] reported the results of 14 two-level PSOs as a subset of a large cohort of primarily one-level PSOs. These investigators obtained a mean correction of 62.6° in these 14 cases. In another article describing the outcomes of PSO for correction of AS-related kyphosis, Kiaer et al. [5] reported the results of 15 two-level PSOs, also only as part of a large series of one-level PSOs. However, until now, there is a paucity of information describing the surgical strategies of two-level PSO.
In our cohort, patients with severe global thoracolumbar kyphosis in advanced AS, if the overall correction of 60° or more was expected, were given two-level (T12 and L3) PSO. This intervention offers several advantages. First, comparing with a single lumbar PSO, two-level PSO can produce more improvements in global sagittal balance and general contour. Second, in a harmonious manner, not only can it spread the cord-level correction over multiple segments, thereby minimizing the potential hazard of focal neurological injury during correction, but also can maintain segmental control at intervening levels, as well as decrease the risk of pedicle screw loosening or migration when a compressive force onto the head of the screw was applied to close the osteotomy site.
The effect level of osteotomy has been discussed in the literature [5, 11, 13, 14]. Several surgeons [5, 11, 14] deem that the lower the osteotomy site is, the more correction by PSO is produced. Chen et al. [11] observed that the maximal correction could be obtained when the osteotomy was performed at L2 or L3, by comparing correction ability of PSO at different osteotomy sites for AS-related thoracolumbar kyphosis. In this series, considering the type of kyphotic deformity, we chose T12 and L3 as the osteotomy sites. T12 and L3 were the apical vertebrae of global thoracolumbar kyphosis and the normal lumbar lordosis in AS, respectively, which were tailored to the specific anatomic biomechanical considerations present in our cases. Therefore, as two angular lesions, these two vertebrae were attacked directly to achieve a favorable general appearance. Besides, L1 and L2 were left intact in between thus making the surgery procedure in a more harmonious pattern.
The key of surgical intervention is to restore spinal sagittal balance and return the gaze to the horizontal. In another word, the desired amount of correction is needed to bring the center of C7 vertebral body directly over S1 endplate with patients’ lower extremities in extension, as well as to correct the CBVA. In addition, it is noted that, in AS-related kyphotic deformity, spinal sagittal imbalance is partly compensated by movements in the lower extremities (hips in extension, knee, and ankle joints in flexion), which exert a strong effect on the value of SVA [23, 24]. So to avoid correction insufficient, we will consider the compensatory effect before corrective procedure. Besides, we authors observed that the cervical flexion–extension range of motion, to some extent, can offer more choices for strategy correction. With all considerations above, in this series, the patients with two-level PSO obtained a mean correction of 67.9° and returned the gaze to the horizontal without deformity recurrence.
Osteoporosis, which is now a well-recognized feature in AS patients, may result in implant loosening and pain [11]. If unaddressed, it may compromise the stability of the construct. Therefore, to reduce the risk of fixation failure and poor results, in our series the patients with severe low bone mineral density have been given calcitonin for treatment of osteoporosis for 1–3 months before and after surgery.
Blood loss during the osteotomy has been deemed as a matter of concern. In order to reduce the blood loss during the procedure, we take the following actions. First, patients were routinely given vitamin K and tranexamic acid for 2 or 3 days after surgery to reduce perioperative blood loss. Second, because the substantial bleeding was not only from the raw bony surfaces attributable to resection of pedicles and the osteotomy through the vertebrae, but also from rupture of epidural venous plexus, we found it critical to effectively use bipolar electrocautery, gel foam, bone wax and thrombin to control bleeding. Third, minimize the blood loss during the surgical exposure as much as possible. For example, rather than a large incision at the very beginning, we recommended using ‘extensile’ incisions that can at anytime be increased in length if more access was required. In addition, as extensively exposed incision can easily result in surface temperature and blood loss of the patients in subcutaneous tissue, when the first PSO was performed, the incision below the next osteotomy segment was temporarily closed with towel clip to prevent it.
In our series, the incidence of paralytic ileus was higher than other complications and was assumed to be associated with elongation of the anterior spinal column, which might have caused tension on the abdominal mesentery vessels or organs. Especially, this effect would be more marked in cases of long-standing spinal kyphotic deformity and continual compression of the upper abdominal viscera by the rib margin. During the observation period, there was no case of secondary junctional kyphosis at segment above proximal instrumented vertebra. These patients benefit from sticking with the treatment of osteoporosis and good compliance with medical supervision. Incidence of neurological deficits has been reported to be high after PSO [25]. Neurologic deficits mainly occur from compression due to translation of a vertebral body, excessive dural kink and central canal compromise [11, 26]. There were no neurologic complications in our series. We accredit this achievement to the meticulous surgical technique and complete spinal decompression. Of note, remove enough bone to accommodate the redundant dural sac. On the other hand, obviate dorsal nerve compression was created by the closure of osteotomy. Perform wake-up test after closure of the second osteotomy.
In conclusion, two-level (T12 and L3) PSO can produce sufficient correction and help the patients gain improvements in either cosmetic or function for severe global thoracolumbar kyphosis resulting from AS. Of course, this study has its own limitations: SVA as the only main spinal parameter was adopted to evaluate the sagittal balance after surgery, without using any pelvic parameters (pelvic incidence, pelvic tilt, sacral slope) to assess pre and postoperative sagittal spinopelvic alignment. Another potential weakness of our study is that as it was a small group study, more cases or a controlled study are needed to be reviewed to further confirm the feasibility, reliability, and complications of this method.
Abbreviations
- AS:
-
Ankylosing spondylitis
- PSO:
-
Pedicle subtraction osteotomy
- CBVA:
-
Chin-brow vertical angle
- GK:
-
Global kyphosis
- LL:
-
Lumbar lordosis
- TK:
-
Thoracic kyphosis
- SVA:
-
Sagittal vertical axis
- ODI:
-
Oswestry disability index
- SPO:
-
Smith-Petersen osteotomy
- VCR:
-
Vertebral column resection
References
El-Sharkawi MM, Koptan WM, El-Miligui YH, Said GZ (2011) Comparison between pedicle subtraction osteotomy and anterior corpectomy and plating for correcting post-traumatic kyphosis: a multicenter study. Europ spine j off publn Europ Spine Soc, Europ Spinal Deform Soc, Europ Sec Cervi Spine Res Soc 20:1434–1440. doi:10.1007/s00586-011-1720-y
Feldtkeller E, Vosse D, Geusens P, van der Linden S (2006) Prevalence and annual incidence of vertebral fractures in patients with ankylosing spondylitis. Rheumatol Int 26:234–239. doi:10.1007/s00296-004-0556-8
Debarge R, Demey G, Roussouly P (2010) Radiological analysis of ankylosing spondylitis patients with severe kyphosis before and after pedicle subtraction osteotomy. Europ spine j off publtn Europ Spine Soc, Europ Spinal Deform Soc, Europ Sec Cervic Spine Res Soc 19:65–70. doi:10.1007/s00586-009-1158-7
Debarge R, Demey G, Roussouly P (2011) Sagittal balance analysis after pedicle subtraction osteotomy in ankylosing spondylitis. Europ spine j off publtn Europ Spine Soc, Europ Spinal Deform Soc, Europ Sec Cervic Spine Res Soc 20(Suppl 5):619–625. doi:10.1007/s00586-011-1929-9
Kiaer T, Gehrchen M (2010) Transpedicular closed wedge osteotomy in ankylosing spondylitis: results of surgical treatment and prospective outcome analysis. Europ spine j off publtn Europ Spine Soc, Europ Spinal Deform Soc, Europ Sec Cervic Spine Res Soc 19:57–64. doi:10.1007/s00586-009-1104-8
Mitra D, Elvins DM, Speden DJ, Collins AJ (2000) The prevalence of vertebral fractures in mild ankylosing spondylitis and their relationship to bone mineral density. Rheumatology 39:85–89
Ragnarsdottir M, Geirsson AJ, Gudbjornsson B (2008) Rib cage motion in ankylosing spondylitis patients: a pilot study. Spine j off j North American Spine Soc 8:505–509. doi:10.1016/j.spinee.2006.12.009
Pigge RR, Scheerder FJ, Smit TH, Mullender MG, van Royen BJ (2008) Effectiveness of preoperative planning in the restoration of balance and view in ankylosing spondylitis. Neurosurg Focus 24:E7. doi:10.3171/FOC/2008/24/1/E7
Smith-Petersen MN, Larson CB, Aufranc OE (1969) Osteotomy of the spine for correction of flexion deformity in rheumatoid arthritis. Clin Orthop Relat Res 66:6–9
Thomasen E (1985) Vertebral osteotomy for correction of kyphosis in ankylosing spondylitis. Clin Orthop 194:142–152
Chen IH, Chien JT, Yu TC (2001) Transpedicular wedge osteotomy for correction of thoracolumbar kyphosis in ankylosing spondylitis: experience with 78 patients. Spine 26:E354–E360
Kim KT, Lee SH, Suk KS, Lee JH, Jeong BO (2012) Outcome of pedicle subtraction osteotomies for fixed sagittal imbalance of multiple etiologies: a retrospective review of 140 patients. Spine 37:1667–1675. doi:10.1097/BRS.0b013e3182552fd0
Kim KT, Suk KS, Cho YJ, Hong GP, Park BJ (2002) Clinical outcome results of pedicle subtraction osteotomy in ankylosing spondylitis with kyphotic deformity. Spine 27:612–618
Qian BP, Wang XH, Qiu Y, Wang B, Zhu ZZ, Jiang J, Sun X (2012) The influence of closing–opening wedge osteotomy on sagittal balance in thoracolumbar kyphosis secondary to ankylosing spondylitis: a comparison with closing wedge osteotomy. Spine 37:1415–1423. doi:10.1097/BRS.0b013e318250dc95
Bridwell KH (2006) Decision making regarding Smith-Petersen versus pedicle subtraction osteotomy versus vertebral column resection for spinal deformity. Spine 31:S171–S178. doi:10.1097/01.brs.0000231963.72810.38
Suk KS, Kim KT, Lee SH, Kim JM (2003) Significance of chin-brow vertical angle in correction of kyphotic deformity of ankylosing spondylitis patients. Spine 28:2001–2005. doi:10.1097/01.BRS.0000083239.06023.78
Fairbank JC, Couper J, Davies JB, O’Brien JP (1980) The Oswestry low back pain disability questionnaire. Physiotherapy 66:271–273
Chang KW, Chen HC, Chen YY, Lin CC, Hsu HL, Cai YH (2006) Sagittal translation in opening wedge osteotomy for the correction of thoracolumbar kyphotic deformity in ankylosing spondylitis. Spine 31:1137–1142. doi:10.1097/01.brs.0000216479.09250.96
Qian BP, Qiu Y, Wang B, Sun X, Zhu ZZ, Jiang J, Ji ML (2012) Pedicle subtraction osteotomy through pseudarthrosis to correct thoracolumbar kyphotic deformity in advanced ankylosing spondylitis. Europ spine j off publtn Europ Spine Soc, Europ Spinal Deform Soc, Europ Sec Cervic Spine Res Soc 21:711–718. doi:10.1007/s00586-011-2054-5
Boachie-Adjei O, Ferguson JA, Pigeon RG, Peskin MR (2006) Transpedicular lumbar wedge resection osteotomy for fixed sagittal imbalance: surgical technique and early results. Spine 31:485–492. doi:10.1097/01.brs.0000199893.71141.59
Gavaskar AS, Naveen Chowdary T (2011) Pedicle subtraction osteotomy for rigid kyphosis of the dorsolumbar spine. Arch Orthop Trauma Surg 131:803–808. doi:10.1007/s00402-010-1224-y
Wang Y, Zhang Y, Mao K, Zhang X, Wang Z, Zheng G, Li G, Wood KB (2010) Transpedicular bivertebrae wedge osteotomy and discectomy in lumbar spine for severe ankylosing spondylitis. J spinal disord tech 23:186–191. doi:10.1097/BSD.0b013e3181a5abde
Van Royen BJ, Toussaint HM, Kingma I, Bot SD, Caspers M, Harlaar J, Wuisman PI (1998) Accuracy of the sagittal vertical axis in a standing lateral radiograph as a measurement of balance in spinal deformities. Europ spine j off publtn Europ Spine Soc, Europ Spinal Deform Soc, Europ Sec Cervic Spine Res Soc 7:408–412
Van Royen BJ, De Gast A, Smit TH (2000) Deformity planning for sagittal plane corrective osteotomies of the spine in ankylosing spondylitis. Europ spine j off publtn Europ Spine Soc, Europ Spinal Deform Soc, Europ Sec Cervic Spine Res Soc 9:492–498
Yang BP, Ondra SL, Chen LA, Jung HS, Koski TR, Salehi SA (2006) Clinical and radiographic outcomes of thoracic and lumbar pedicle subtraction osteotomy for fixed sagittal imbalance. J neurosurg Spine 5:9–17. doi:10.3171/spi.2006.5.1.9
Arun R, Dabke HV, Mehdian H (2011) Comparison of three types of lumbar osteotomy for ankylosing spondylitis: a case series and evolution of a safe technique for instrumented reduction. Europ spine j off publtn Europ Spine Soc, Europ Spinal Deform Soc, Europ Sec Cervic Spine Res Soc 20:2252–2260. doi:10.1007/s00586-011-1894-3
Acknowledgments
The study was supported by the Hunan Province Institute of Science and Technology Fund (2009SK2012) and the Fundamental Research Funds for the Central Universities (2012QNZT126).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, H.Q., Huang, J., Guo, C.F. et al. Two-level pedicle subtraction osteotomy for severe thoracolumbar kyphotic deformity in ankylosing spondylitis. Eur Spine J 23, 234–241 (2014). https://doi.org/10.1007/s00586-013-2867-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-013-2867-5