Abstract
Study design
Retrospective study of a prospective clinical and radiological database of subjects with adolescent (AIS) and adult (AS) idiopathic scoliosis undergoing surgical correction by posterior approach.
Objectives
To evaluate the differences in sagittal alignment of the spine and pelvis in AIS and AS before surgery and changes after surgery in both populations.
Summary of background data
The relationship between the spine and pelvis highly influences the sagittal balance in adults and adolescents. However, the sagittal alignment of the spine and pelvis before and after surgery in idiopathic scoliosis, whatever the age, is poorly defined in the literature.
Methods
Clinical and radiological data were extracted from a prospective database of 132 AIS patients and 52 AS before and at last follow-up after surgical correction. Sagittal parameters were evaluated on AP and lateral radiographs using a custom software: pelvic incidence (PI), sacral slope (SS), pelvic tilt (PT), lumbar lordosis (LL), thoracic kyphosis (TK), C7 Barrey’s ratio, spino-sacral angle (SSA). A new algorithm of combination of balance parameters was proposed to characterize and compare the various pathological spino-pelvic settings. Based on PI subdivision in high (<55°) and low values (>55°), then on a range of PT indexed on PI giving the pelvis positioning (anteverted, normal or retroverted), the population was finally characterized by the C7 plumbline position with regard to the posterior edge of the sacrum and the center of the femoral heads, in balanced, slightly unbalanced and unbalanced. More specifically, the AIS study included the cervical shape alignment with cervical lordosis (CL) and sagittal thoracic profile assessment (hypo vs. normokyphotic). In AS, the study focused on thoraco-lumbar kyphosis (TLK) occurrence (LL length). Paired Student t tests were used for comparison (α = 0.02).
Results
Pre-operatively, in AIS there was a prevalence of lower PI (57 %). Whatever the PI, PT remained anteverted or normal. Positioning of C7 was much more unbalanced, forward of the femoral heads (50 %), than in asymptomatic population (17 %). There was a notable loss and reversal of cervical lordosis in the majority of subjects, with an average cervical kyphosis measurement of 10 ± 18°. Thoracic kyphosis values were lower than average, while lumbar lordosis values were within normal limits. After surgery, in the entire group, a slight but significant increase of PT coupled to a decrease of SS and LL was noted, while no changes could be documented in thoracic kyphosis and cervical lordosis. However, when sub-classified according to thoracic hypo versus normokyphosis pre-op, there was a significant decrease of TK coupled to a decrease of LL and CL in the normokyphotic group, while TK and CL were improved in the hypokyphotic group. A significant number of patients improved their global balance. Changes in sagittal profile between Lenke curve types were minimal. In AS there were significant differences between low and high PI populations. Severity of unbalance increased in high PI population with association of retroverted pelvis and forward unbalance. In lower PI, increasing PT was generally sufficient to balance the patients. The occurrence of TLK was strongly increased in the entire population and became the rule in those with lower PI (76 %). Post-operatively, in those with high PI, PT did not change while global balance improved slightly. The strategy of correction in higher PI was to maintain TLK. In those with low PI, PT improved while C7 did not change. Correction of TLK was obtained in eight cases.
Conclusions
A decrease of cervical lordosis and thoracic kyphosis is commonly associated with AIS. The anterior unbalance frequently found in AIS does not seem to have the same significance of severity as in AS. In AIS PI does not change the balance criterions, while in AS the severity of unbalance is increased with higher PI. TLK seems to be a way of worsening the balance in elderly, mainly in lumbar and thoraco-lumbar scoliosis with low PI. Surgical correction of the thoracic and lumbar spine in AIS induces significant changes in the sagittal spino-pelvic profile. Changes in the cervical sagittal profile vary according to the pre-op sagittal profile of the thoracic kyphosis. Cervical lordosis and thoracic kyphosis are improved by surgical correction in subjects with pre-operative hypokyphosis, but a reverse effect is noted in those with normal pre-operative kyphosis. The clinical significance of these changes in sagittal shape remains to be determined. In AS, it appears easier to restore a good balance in the lower PI population than in those with less pre-operative unbalance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The importance of sagittal spino-pelvic organization in pathology and the crucial necessity of its restoration after surgical treatment are now well recognized in the literature [1]. Parameters allowing the assessment of sagittal balance are commonly used. Geometrical parameters, described by Duval Beaupere [2, 3], characterize pelvic shape and positioning: pelvic incidence (PI), pelvis tilt (PT) and sacral slope (SS). They are linked by a remarkable mathematical relation: PI = PT + SS. Several parameters describe the different curvatures of the spine: lumbar lordosis (LL), thoracic kyphosis (TK). With regard to the global orientation of the spine, C7 positioning is generally accepted for its stability over the sacrum in balanced asymptomatic population [4].
Pelvic parameters have not suffered any important contestation thanks to the easily identifiable anatomical landmarks (sacral plateau, centers of femoral heads) [5]. Pelvic incidence remains relatively constant during childhood. Thereafter, it increases significantly during adolescence, reaching its maximum value in adulthood [6]. This parameter is closely related to lumbar lordosis in normal adolescents and adults [7, 8]. Legaye et al. [3] showed a significant relationship between pelvic incidence and lumbar lordosis in scoliotic adults, but they did not observe any significant difference for PI between normal and scoliotic adults. Mac-Thiong et al. [9] reported an increased pelvic incidence in subjects with AIS.
There remains some differences as to the best method to measure and assess spinal parameters. Classically the measure of LL has respected the anatomical limits between T12 and L5 or S1 [10–12]. Some authors [13] have contested these limits, opposing that a biomechanical vision is more accurate and better describes the main curvatures by the limit were one curve transitions in another curve (inflexion point). Using this method, it is possible to introduce the notion of length of LL, and to describe thoraco-lumbar kyphosis (TLK). Another area of controversy concerns the C7 positioning. Everyone agrees that the ideal balanced position of the C7 plumbline (C7 PL) is very stable at the level of the posterior edge of the sacral plateau and that a notable forward displacement is a proof of unbalance [4, 11]. Authors have described horizontal distance between projection of C7 PL and an easily identified pelvic landmark. Lafage et al. [14] used SVA (horizontal distance with posterior limit of the sacral plateau). While easy to obtain, the measuring of a distance needs calibrated X-rays, and may be a source of error in multicenter study where different X-ray setups are used. We prefer to use comparable X-ray measurements, either with angles (SSA, spino-sacral angle between a line from C7 to the middle of the sacral plateau and the sacral plateau), or by the use of a ratio described by Barrey (distance between C7 PL and femoral heads, and distance between femoral heads and posterior limit of the sacral plateau) [4, 15].
While a typology of spino-pelvic organization seems possible [13] in an asymptomatic population, the large number of combination of parameters forbids such a simple segmentation in pathological cases. Up to now, a majority of authors have emphasized some pertinent parameters to assess the pathological status and to provide guidelines for surgical treatment.
Even if sagittal balance is a relatively new concept, a lot of studies have already focused on scoliosis sagittal balance in adolescents [16] or adults [17, 18] and on surgical effect. Up to now, there has been no study comparing the adolescent and adult pre- and post-operative status. Considering the fact that idiopathic scoliosis is a pathology beginning in childhood and, if not treated, evolving the entire life, we propose a retrospective analysis of pre- and post-operative sagittal balance in a prospectively collected and consecutive population of 132 adolescent idiopathic scoliosis (AIS) and 52 adult idiopathic scoliosis (AS). All patients were treated at the same institution by the same surgeon and recorded in the same data bank (Keops®). Pre- and post-operative long standing X-rays were analyzed using Keops analyzer by two successive observers. A new algorithm for sagittal balance analysis is proposed, mixing PI, PT and C7 positioning to characterize the different patterns of pathological balance and their evolution after corrective surgery. In post-operative AS we tried to determine if PI may influence the quality of balance correction after surgery. Specific analyzes were conducted with regard to the pre- and post-operative cervical spine status in AIS and the presence of TLK in AS. The last part of this study tried to determine if the combination of some initial frontal and sagittal features may lead to sagittal worsening when coupled with degeneration.
Material and method
Two cohorts were analyzed independently: 132 adolescents aged between 12 and 21 years, and 52 adult patients between 22 and 75 years at the time of surgery. The inclusion criteria were: (1) a diagnosis of idiopathic scoliosis, (2) no neurological deficit, (3) no previous spine surgery, and (4) no evidence of spondylolisthesis. De novo degenerative scoliosis was excluded. The whole cohort underwent reduction and fusion surgery with posterior instrumentation by one surgeon at a single institution. A unique instrumentation with translation technic was used (Colorado®) by posterior approach. In AIS, only one stage was performed. In AS, above 50 years, lumbar and thoraco-lumbar scoliosis were fused to the sacrum. If necessary a second stage of interbody lumbar and/or lumbo-sacral cages was performed. The average follow-up between the pre- and post-operative evaluation was 3 years (range 4.8–2.1).
All patients from both consecutive cohorts were entered in the same prospective database (Keops). Characteristics of both cohorts are as follows:
AIS
We reviewed a cohort of 132 consecutive patients (16 boys, 116 girls) diagnosed with AIS and operated by one surgeon. The mean age at surgery was 15.3 ± 2.2 years (range 11–21 years) and the mean primary Cobb angle was 56.7° ± 16.2°. The patients were sub-classified based on their coronal curve type according to the Lenke classification system [19]. There were 67 Lenke type 1, 19 Lenke type 2, 9 Lenke type 3, 0 Lenke type 4, 12 Lenke type 5 and 25 Lenke type 6 patients. Patients were also sub-classified according to the magnitude of their thoracic kyphosis: the hypokyphotic group including patients with thoracic kyphosis <20º, and the normokyphotic group including patients with thoracic kyphosis ≥20º.
AS
There was a predominance of females (51) for only one male. The mean age at surgery was 52.4 ± 3.7. With regard to frontal deformity, 76 % were thoraco-lumbar and lumbar scoliosis. In older patients (>40 years) with lumbar or thoraco-lumbar scoliosis, there were 18 with TLK for 12 with long lordosis. In younger patients (<40 years) with lumbar or thoraco-lumbar scoliosis (eight cases) only one had a TLK.
Radiological measurements
Assessment of the spine was done with long AP and lateral standing X-rays just before surgery and at the latest post-operative control. Lateral X-rays were analyzed with Keops analyzer (SMAIO®). In order to avoid any controversy on the measuring quality, only very remarkable and readable anatomical landmarks were used in this study: center of femoral heads, sacral plateau, and center of C7 vertebral body. The proximal limit of the lumbar lordosis was the only landmark which needed a double advice from two senior surgeons. This proximal limit (IP of Berthonnaud) [20] is where LL transitions into TK. Sometimes, due to the scoliotic deformity, IP was not located at the level of an inter body space, and was located as the point where both curvatures are tangent.
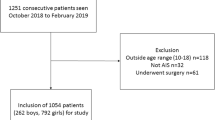
Assessment of spino-pelvic organization was determined by a combination of three sets of parameters: pelvic parameters (PI and PT), C7 positioning (spino-pelvic angle and Barrey’s ratio), and lumbar curve length and angle. An algorithm of pathological identity was designed (Fig. 1). PI was divided into low PI (<55°) and high PI (>55°), with regard to the mean value of PI in the global population (AIS + AS). In order to determine whether the pelvis positioning was pathological, three levels of PT were calculated with regard to PI value. Limits were based on a percentage of PI/2 which was given by Mac Thiong et al [21], as the maximum value of PT in an asymptomatic population. A segmentation of PT values was proposed between 0° and PI/2. The pelvis was considered anteverted when PT is less than 20 % of PI/2, normal between 20 % of PI/2 and 80 % of PI/2, and retroverted over 80 % of PI/2 (Fig. 2). C7 positioning was measured using the Barrey ratio: distance between C7 PL and posterior edge of S1 plateau on distance between posterior edge of S1 plateau and center of femoral heads. It was considered negative when behind the S plateau (well balanced), between 0 and 1 when between S plateau and femoral heads (slightly unbalance), and over 1 when forward to the femoral heads (severe unbalance). Lumbar lordosis length was identified with regard to L3. When the proximal limit of lordosis was higher than L3, it was considered as a long lordosis, and when lordosis proximal limit was L3 or below, it was considered as a short lordosis and a thoraco-lumbar kyphosis.
To assess specifically the cervico-thoracic area in AIS, measures in two steps were performed after identification of the superior plate of T3. The transitional point between cervical and thoracic spine was identified by approximation of split curves by two successive operators giving the global angle of each curve. Then, the sagittal contour of each cervical vertebra was identified by four points giving the different intra and extra angles to the precise shape and orientation of the lower cervical spine between C3 and C7-T1.
Results
AIS study
Table 1 details the mean pre- and post-operative values for all radiological variables with their standard deviations (SD) and the p value of the paired Student test between each pair of variables in the cohort of 132 subjects. Negative angular measures for CL, TK or LL indicate kyphosis, while positive values indicate lordosis. The most striking anomaly detected in baseline measurements is the cervical lordosis which was in fact reversed to a cervical kyphosis in the majority of the cohort, averaging 10° ± 16°. Thoracic kyphosis appeared lower than normal, averaging 28° ± 19º of kyphosis.
With respect to pre- and post-op changes in spino-pelvic alignment, no important differences could be detected for PI, LSA, IL5, KT, CL, S1C7, SPC7 and SSA. In contrast, a significant increase in pelvic tilt of 1.8° coupled to a decrease in sacral slope of 1.3° and in lumbar lordosis of 1.8° was found after surgery. Important curve correction in the frontal plane averaging 60 % for the primary curve and 56 % for the secondary curve was documented. Sub-grouping with respect to Lenke curve types did not reveal changes, except for significant increases in pelvic tilt of 3° in Lenke 3 and 6 curve types.
Table 2 details the mean pre- and post-operative values for all radiological variables with their SD and the p value of the paired Student test between each pair of variables in the subgroup of 94 subjects with a thoracic kyphosis ≥20º (normokyphotic sub-group). In contrast to the results in Table 1 for the entire group, it can be seen that significant differences are now seen in the sagittal alignment of the spine: the thoracic kyphosis averaging 36° ± 13º pre-op is decreased to 30° ± 11º after surgery, and this change is coupled to an increase in cervical kyphosis from 4° ± 14º to 8° ± 14º and a decrease in lumbar lordosis from 56° ± 9º to 53° ± 9º.
Table 3 details the mean pre- and post-operative values for all radiological variables with their standard deviations (SD) and the p value of the paired Student test between each pair of variables in the subgroup of 38 subjects with a thoracic kyphosis <20º (hypokyphotic sub-group). Again, negative angular measures for CL, TK or LL indicate kyphosis, while positive values indicate lordosis. It can be seen that PI values are unchanged in both groups. In contrast to the results in Table 1 for the entire group, it can also be noted that significant differences are also seen in the sagittal alignment of the spine, but in a reverse direction from those seen in the normokyphotic sub-group: the thoracic kyphosis averaging 6 ± 11º pre-op is increased to 16 ± 10º after surgery, and this change is now coupled to a decrease in cervical kyphosis from 26° ± 11º to 20° ± 14º and no measurable change in lumbar lordosis.
Table 4 details the AIS population after segmentation into high (>55°) and low PI (<55°). In both populations we found a high number of unbalanced C7 PL (48 %), significantly improved post-operatively (31 %). Association of unbalanced C7 PL and anteverted pelvis was more frequent in the low PI population. Association with a retroverted pelvis is exceptional (1 case). Post-operatively, the number of retroverted pelvis in the global population increased (from 2 cases to 9 cases).
TLK with a short LL was exceptional in high PI (1 case) and was found only five times in smaller PI. Post-operatively it remained only three cases with TLK.
AS study
With regard to frontal deformity, lumbar (apex L2, L3) and thoraco-lumbar (apex T11, T12) curves were dominant (69 %); the proportion increased with age (80 % with age >40).
Pelvic parameters were significantly different compared with an asymptomatic population: increased PI and PT (respectively 56.9° and 22.5°) and decreased SS (34.2°).
Table 5 details the AS population after segmentation into high and low PI. Only two patients in each group may be considered as well balanced (normal PT, balanced C7). The majority of cases were slightly unbalanced. The worse situation (retroverted and unbalanced) was found only with greater PI (seven cases). There were unbalanced with non-retroverted pelvis in both groups (eight cases). Proportion of unbalanced cases was greater in higher PI (39 %) than in smaller (16 %). Post-operatively, the smaller PI population was slightly improved on PT values and C7 PL. In the higher PI population PT did not change and C7 PL improved poorly.
Table 6 details a superior segmentation with and without TLK. In the global population the number of patients with TLK was 25 (48 %). The ratio of TLK with greater PI (25 %) was dramatically lower than that in the smaller PI population (75 %). After surgery the lumbar shape was not changed in high PI. In lower PI the number of TLK decreased, eight cases changing for a longer LL. It was unchanged in the high PI population.
When compared with the frontal deformity, only one case of TLK was found in a non-thoraco-lumbar or lumbar scoliosis.
Discussion
This study evaluated the sagittal alignment of the spine and pelvis in AIS and AS after surgical correction in a prospective and consecutive cohort of patients operated by the same surgeon with the same instrumentation and surgical technique.
AIS features
Baseline values for sagittal alignment found in this study are consistent with previous work and confirm that spinal alignment is abnormal in AIS, but that pelvic alignment is only minimally disturbed. When compared to measurements in an historical control cohort of adolescents published by Mac-Thiong et al. using the same radiographic protocol and software analysis [8], PI was only slightly elevated in the present study (53° ± 12º vs. 49° ± 11°), PT was slightly elevated (11° ± 8º vs. 8° ± 8º), and SS similar (42° ± 9º vs. 41° ± 9º). In clear contrast, a reversal of the physiologic cervical lordosis was associated with AIS, with an average cervical kyphosis of 10° ± 16°.
Hilibrand et al. [22] were the first to confirm on X-rays a relationship between the thoracic and cervical spine in the sagittal plane. They noted an inverse relationship between cervical and thoracic kyphosis in AIS. It is hypothesized that changes in cervical alignment are compensatory mechanisms in response to thoracic alignment permitting the maintenance of vision parallel to the horizon.
A decrease in thoracic kyphosis was also documented in this study, when compared to the control population of Mac-Thiong et al. [6, 8] (28 ± 19° vs. 44 ± 10º), while lumbar lordosis was relatively similar (53 ± 10º vs. 49 ± 12º). Some authors [23] state a normal TK range of 20°–40°, although reference values of 30°–50° and 20°–50° are also suggested [24]. Furthermore, the measurement of the TK with the Cobb method on lateral radiographs tends to underestimate the loss of TK in patients with a thoracic scoliotic curve. For these patients, the TK may be smaller when it is seen from a true lateral view at the apex, due to vertebral rotation and wedging. Many authors have already demonstrated that the TK is smaller for thoracic curves as compared to controls [25]. The findings for the TK in this study support the hypothesis that hypokyphosis is involved in the development of thoracic AIS [26].
The high rate of C7 plumbline positioning in front of the femoral heads seems abnormal in comparison with an asymptomatic population [21]. Its association with anteverted pelvis in low grade PI is relevant in younger population and does not seem to have the same pathological significance as in adults. Even with a bad position of C7 the compensation by increasing PT was exceptional (only one case). This supports the contention that the appearance of unbalance in young population is well tolerated and probably differs from the unbalance of the older population due to a lack of lordosis.
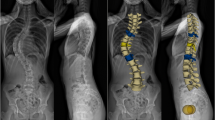
With respect to pre- and post-op changes in spino-pelvic alignment, this study has shown that corrective surgery using modern instrumentation and hybrid constructs can alter pelvic alignment, creating slight pelvic retroversion, as manifested by an increase in PT, coupled to a slight decrease in SS. More importantly, corrective surgery can significantly modify the sagittal alignment of the cervical spine, but this effect is different depending on the underlying configuration of the pre-op sagittal thoracic spine. In normokyphotic thoracic spines, corrective surgery appears to decrease TK with a coupling effect of increased cervical kyphosis, while in hypokyphotic thoracic spines, corrective surgery improves TK with a coupling effect of decreased cervical kyphosis. Figures 3 and 4 illustrate these two different mechanisms of correction in the sagittal plane.
In AIS, little has been published about the consequences of spinal fusion on cervical spine alignment. Hwang et al. [27] have recently reported in a sample of 22 patients that the sagittal profile of the thoracic spine is related to that of the cervical spine in AIS. The surgical treatment of Lenke type 1 and 2 curves by using all pedicle screw constructs was shown to have a significant hypokyphotic effect on thoracic sagittal plane alignment and if post-operative thoracic kyphosis was excessively decreased, the cervical spine may decompensate into significant kyphosis. The present study adds to these findings by distinguishing the effects of surgical correction based on the pre-op configuration of the thoracic spine. It is unclear at the present time why the same surgical maneuvers used in AIS produce different corrective effects in the sagittal plane depending on whether the thoracic spine is hypo or normokyphotic, but it is hypothesized that coupled motions produced by these maneuvers may be responsible.
The clinical significance of these changes remains to be determined, but surgeons should be aware of these effects when performing corrective surgery in AIS. Other authors have noted 17.6–57 % rates of associated cervical pain with long-term follow-up after AIS instrumentation [28]. Ofiram et al [29] noted increasing degenerative changes in the spine adjacent to AIS fusions with 8.5 years of follow-up, but they also noted that the degenerative changes were greater than those in the normal counterparts at baseline. Some authors have not found a correlation strictly between cervical spine alignment and pain in adults [30], although the general sagittal profile has been strongly correlated with function and pain [1].
The current study presents the same limitation as any cross-sectional study. It cannot precisely ascertain the evolution of the deformities over time because the evaluated spinal and pelvic parameters were fixed in time. A longitudinal study is required to confirm the influence of the corrective surgery on the spino-pelvic alignment.
AS features
Frontal deformity in AIS seems to change mainly the sagittal contour of the whole spine, without disturbing strongly the global balance; in AS the combined effect of the scoliotic deformity and degeneration in aging induces severe disturbances in global balance and pelvis compensation.
General patterns of alteration of sagittal balance in pathology and their functional effect have been well described in the literature [10, 31]. A combination of various sagittal parameters has been proposed to assess pathological status and to predict an ideal correction. Rose [11] proposed a formula combining PI, LL, and TK which determined a balanced correction when PI + LL + TK <45°. It was difficult to assert if important parameters like PT or C7 PL were concerned with this formula. Kim [32] found that patients with optimal pre-operative sagittal balance had smaller PI and a larger difference between LL and TK.
More recently, Lafage [18] introduced a range of normal values to differentiate balanced and unbalanced spine. The authors combined C7 PL positioning with SVA (limit = 5 cm) and PT (limit 25°). They found a good correlation in unbalanced spine (SVA > 5CM; PT > 25°) when it was less ideal in so called “balanced spine”.
Up to now, an identification of the sagittal contour by a combination of the classical sagittal parameters has not been done. While it has been possible to define four main types of spino-pelvic organization in asymptomatic persons [13], it seems that in pathology the various combinations do not allow such a simple segmentation. On the other hand, if we know that a pathological position is identified by a variation of positional parameters such as PT, it is necessary to define the limits where the value of one parameter becomes abnormal. Analysis of an asymptomatic population was insufficient to provide pathological limits of PT. The relation PI = PT + SS does not allow a proportional correlation between PI and SS which is confirmed by a correlation between PI and PT around 0.65. We may accept that there is a range of normality of PT depending on the value of PI. In their study on 709 asymptomatic subjects, Mac Thiong et al. found a maximal value of PT of PI/2, but the fact that the subjects were asymptomatic is not a proof of normality. This is the reason why we chose a lower than PI/2 limit to determine an excessive abnormal retroversion, at PI/2-20 % of PI/2. With regard to the lower acceptable limit of PT for defining an excessively anteverted pelvis, we selected a value of 0° + 20 % of PI/2. We understand that even if the choice of these limits seems empirical, we do not have other scientific ways to characterize PT without any doubt. This range of normality of PT is important because it determines the corresponding range of SSA. For one given PI and PT corresponds one given SS and its ideal SSA.
Lafage [14] has shown that in an elderly population, PT was increased demonstrating the progressive loss of lumbar lordosis with age but this study did not made the difference between a population with high PI and one with low PI. Due to its constant value through life, PI, as a morphological parameter, is the only parameter we have to determine in the post-operative strategy of sagittal correction. For this reason we divided our population with respect to an average value of PI of 55°, which was the average value of PI of both populations. With regard to age, we found the same observation as Lafage: in the global population the older the patients, the more the increase in PT. With regard to the difference between high and low PI, the ratio between normal and retroverted pelvis was the same. But if we refer to the C7 plumbline, 39 % were unbalanced (in front of the femoral heads) in high PI when only 16 % were unbalanced in low PI with a lower Barrey’s ratio. It was possible to find patients with anteverted or normal PI with unbalanced C7 plumbline as if the pelvis positioning contributed to the unbalance. The retroversion mechanism of increasing PT was efficient enough to balance the spine in the low PI population, but in half of the cases, the increasing PT was unable to compensate the C7 unbalance. It seems that the unbalance severity was higher in higher PI and better compensated in lower PI by the retroversion mechanism.
With regard to the shape of lordosis, it was amazing to observe that 48 % of the global population had a thoraco-lumbar kyphosis, when in the asymptomatic population this proportion is 6 %. This ratio increases dramatically to 75 % in cases with low PI. It seems that, in the aging population, the relation between scoliosis localization in thoraco-lumbar and lumbar area and TLK increased significantly. The torsional effect of scoliosis with degenerative loss of disc height may be a coupling factor producing TLK. Combination with a low PI is an additional factor with lumbar and thoracolumbar scoliosis to produce late TLK (Fig. 5).
After surgical correction in AS, balance improvement was significantly different in high versus low PI. In high PI, it was more difficult to improve balance than in low PI. In cases of unbalance with high PI, PT is strongly increased and LL decreased. Restoration of balance needs restoration of a much LL which may be technically difficult to obtain. This partial reduction is sufficient enough to reach a better global balance but insufficient to improve PT (Figs. 6, 7). It is different in patients with low PI where the loss of LL is lower and, by the way, easier to reduce and to obtain a good balance by surgical treatment.
Conclusion
Sagittal balance criterions in AIS and AS are very different. In AIS, the frontal scoliotic deformity affects the sagittal contours of the spine by flattening the thoracic kyphosis with a consequence on cervical sagittal orientation. If C7 PL is frequently in front of the femoral heads, this does not have the same impact as in AS, and does not seem to be associated with a worse spino-pelvic balance situation. On the contrary in AS, the same positioning of C7 PL is a proof of severe unbalance accompanying the increased PT. If a high PI has been considered as allowing more compensation to retroverse the pelvis in pathologies such as spondylolisthesis, or to better compensate for a severe kyphosis, our study demonstrates that, in fact, a smaller PI in AIS is generally associated with a better balance and a better post-operative result. With regard to the relation with the frontal scoliotic deformity, it seems that the high number of TLK is a consequence of a combination between lumbar and thoraco-lumbar scoliosis coupled with disc degeneration in aging.
References
Glassman SD, Berven S, Bridwell K, Horton W, Dimar JR (2005) Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976) 30:682–688
Duval-Beaupère G, Schimdt C, Cosson P (1992) A barycentremetric study of the sagittal shape of spine and pelvis: the conditions required for an economic standing position. Ann Biomed Eng 20:451–462
Legaye J, Duval-Beaupère G, Hecquet J et al (1998) Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 7:99–103
Roussouly P, Gollogly S, Noseda O, Berthonnaud E, Dimnet J (2006) The vertical projection of the sum of the ground reactive forces of a standing patient is not the same as the C7 plumb line: a radiographic study of the sagittal alignment of 153 asymptomatic volunteers. Spine 31(11):E320–E325
Dimar JR 2nd, Carreon LY, Labelle H, Djurasovic M, Weidenbaum M, Brown C, Roussouly P (2008) Intra- and inter-observer reliability of determining radiographic sagittal parameters of the spine and pelvis using a manual and a computer-assisted methods. Eur Spine J 10:1373–1379
Mac-Thiong JM, Labelle H, Berthonnaud E, Dimar J, Betz R (2004) Sagittal Alignment of the Spine and Pelvis during Growth. Spine 29(15):1642–1647
Vaz G, Roussouly P, Berthonnaud E et al (2002) Sagittal morphology and equilibrium of pelvis and spine. Eur Spine J 11:80–87
Mac-Thiong JM, Labelle H, Berthonnaud E, Betz RR, Roussouly P (2007) Sagittal spinopelvic balance in normal children and adolescents. Eur Spine J 16(2):227–234
Mac-Thiong JM, Labelle H, Charlebois M, Huot MP, de Guise JA (2003) Sagittal plane analysis of the spine and pelvis in adolescent idiopathic scoliosis according to the coronal curve type. Spine 28:1404–1409
Takeda N, Kobayashi T, Atsuta Y, Matsuno T, Shirado O, Minami A (2009) Changes in the sagittal spinal alignment of the elderly without vertebral fractures: a minimum 10-year longitudinal study. J Orthop Sci 14(6):748–753
Rose PS, Bridwell KH, Lenke LG, Cronen GA, Mulconrey DS, Buchowski JM, Kim YJ (2009) Role of pelvic incidence, thoracic kyphosis, and patient factors on sagittal plane correction following pedicle subtraction osteotomy. Spine 34(8):785–791
Schwab F, Lafage V, Farcy JP, Bridwell K, Glassman S, Ondra S, Lowe T, Shainline M (2007) Surgical rates and operative outcome analysis in thoracolumbar and lumbar major adult scoliosis: application of the new adult deformity classification. Spine 32(24):2723–2730
Roussouly P, Gollogly S, Berthonnaud E, Dimnet J (2005) Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine 30(3):346–353
Lafage V, Schwab F, Skalli W, Hawkinson N, Gagey PM, Ondra S, Farcy JP (2008) Standing balance and sagittal plane spinal deformity: analysis of spinopelvic and gravity line parameters. Spine 33(14):1572–1578
Barrey C, Roussouly P, Perrin G, Le Huec JC (2011) Sagittal balance disorders in severe degenerative spine. Can we identify the compensatory mechanisms? Eur Spine J 20(Suppl 5):626–633
De Jonge T, Dubousset JF, Illés T (2002) Sagittal plane correction in idiopathic scoliosis. Spine 27:754–761
Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G (2006) An analysis of sagittal spinal alignment following long adult lumbar instrumentation and fusion to L5 or S1: can we predict ideal lumbar lordosis? Spine 31(20):2343–2352
Lafage V, Schwab F, Vira S, Patel A, Ungar B, Farcy JP (2011) Spino-pelvic parameters after surgery can be predicted: a preliminary formula and validation of standing alignment. Spine (Phila Pa 1976) 36(13):1037–1045
Lenke LG, Betz RR, Harms J et al (2001) Adolescent idiopathic scoliosis. A new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am 83:1169–1181
Berthonnaud E, Dimnet J, Roussouly P, Labelle H (2005) Analysis of the sagittal balance of the spine and pelvis using shape and orientation parameters. J Spinal Disord Tech 18(1):40–47
Mac-Thiong JM, Roussouly P, Berthonnaud E, Guigui P (2010) Sagittal parameters of global spinal balance: normative values from a prospective cohort of seven hundred nine Caucasian asymptomatic adults. Spine 35(22):E1193–E1198
Hilibrand AS, Tannenbaum DA, Graziano GP, Loder RT, Hensinger RN (1995) The sagittal alignment of the cervical spine in adolescent idiopathic scoliosis. J Pediatr Orthop 15:627–632
De Jonge T, Dubousset JF, Illés T (2002) Sagittal plane correction in idiopathic scoliosis. Spine 27:754–761
Hagglund G, Karlberg J, Willner S (1992) Growth in girls with adolescent idiopathic scoliosis. Spine 17:108–111
Archer IA, Dickson RA (1985) Stature and idiopathic scoliosis: a prospective study. J Bone Joint Surg Br 67:185–188
Dickson RA, Lawton JO, Archer IA et al (1984) The pathogenesis of idiopathic scoliosis: biplanar spinal asymmetry. J Bone Joint Surg Br 66:8–15
Hwang SW et al (2011) Cervical sagittal plane decompensation after surgery for adolescent idiopathic scoliosis: an effect imparted by postoperative thoracic hypokyphosis. J Neurosurg Spine 15:491–496
Edgar MA, Mehta MH (1988) Long-term follow-up of fused and unfused idiopathic scoliosis. J Bone Joint Surg Br 70:712–716
Ofiram E, Garvey TA, Schwender JD, Wroblewski JM, Winter RB (2009) Cervical degenerative changes in idiopathic scoliosis patients who underwent long fusion to the sacrum as adults: incidence, severity, and evolution. J Orthop Traumatol 10:27–30
Grob D, Frauenfelder H, Mannion AF (2007) The association between cervical spine curvature and neck pain. Eur Spine J 16:669–678
Bess S, Boachie-Adjei O, Burton D, Cunningham M, Shaffrey C, Shelokov A, Hostin R, Schwab F, Wood K, Akbarnia B; International Spine Study Group (2009) Pain and disability determine treatment modality for older patients with adult scoliosis, while deformity guides treatment for younger patients. Spine 34(20):2186–2190
Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G (2006) An analysis of sagittal spinal alignment following long adult lumbar instrumentation and fusion to L5 or S1: can we predict ideal lumbar lordosis? Spine 31(20):2343–2352
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Roussouly, P., Labelle, H., Rouissi, J. et al. Pre- and post-operative sagittal balance in idiopathic scoliosis: a comparison over the ages of two cohorts of 132 adolescents and 52 adults. Eur Spine J 22 (Suppl 2), 203–215 (2013). https://doi.org/10.1007/s00586-012-2571-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-012-2571-x