Abstract
Purpose
To compare the positions of the aorta relative to vertebral bodies and the potential risk of the aorta impingement for pedicle screw (PS) placement between right-sided and left-sided thoracolumbar/lumbar curves of adolescent idiopathic scoliosis (AIS).
Methods
Thirty-nine AIS patients with a main thoracolumbar or lumbar curve were recruited. The Lenke’s classification was type 5C in all patients. According to the convexity of the thoracolumbar or lumbar curves, the patients were divided into either group R or Group L. The patients in Group R had a main right-sided thoracolumbar/lumbar curve, and the patients in Group L had a main left-sided thoracolumbar/lumbar curve. Axial CT images from T12 to L4 at the midvertebral body level were obtained to evaluate Aorta-vertebra angle (α), Vertebral rotation angle (β), Lefty safety distance (LSD), and Right safety distance (RSD). The risks of the aorta impingement from T12 to L4 were calculated and then compared between the two groups.
Results
The α increased from T12 through L4 in Group R, increased from T12 through L1, and then decreased from L1 through L4 in Group L. The β decreased from T12 through L4 in both groups. The LSD constantly increased from T12 through L4 in Group R, increased from T12 through L3, and then decreased from L3 through L4 in Group L. The RSD increased from T12 through L3 and then decreased from L3 through L4 in both groups. With the increment of the lengths of the simulated screws, the aorta impingement risks were constantly elevated at all levels in both groups. The aorta was at a high risk of impingement from left PS regardless of the diameters of the simulated screws in Group R (80–100 % at T12 and 53.3–100 % at L1). In Group L, the aorta was completely safe when using 35 mm (0 at all levels) PS and at high risks of the aorta impingement on the right side from 45 mm PSs (31.8–72.7 %). In all, the risks of the aorta impingement were mainly from left PS in Group R and from right PS in Group L, and the risk of the aorta impingement from PS placement was generally higher in right thoracolumbar or lumbar curves when compared with that of the left.
Conclusions
The present study illustrated different changed positions of the aorta relative to vertebrae between thoracolumbar/lumbar curves with different convexities. In right-sided curve, the risks of the aorta impingement were mainly from left PS while in left-sided curves, from right PS. The aorta was more proximal to entry points in right-sided lumbar curve when compared with left-sided curve; thus placing PS carries more risks in right-sided thoracolumbar/lumbar curve. Surgeons should be more cautious when placing PSs on the concave sides of T12 and L1 vertebrae of right-sided thoracolumbar/lumbar curves.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pedicle screw (PS) has been widely used in the treatment of thoracolumbar/lumbar scoliosis [1]. However, the risks of neural, vascular, and visceral injuries from malpositioned pedicle screws have raised some concerns in this region [2–4]. The aorta may be at the risk of impingement and even perforation, if it is located at the trajectory of PS and when the PS perforates the anterior or lateral wall of vertebral body.
Several studies have been conducted regarding the position of the aorta in either normal subjects or scoliotic patients [5–7]. These studies demonstrated that the aorta is always located on the left side of the thoracic spine and stays in front of the lumbar spine in normal subjects [5] while tending to reside on the lateral side of the spine in scoliotic patients, and this change may elevate the risk of the aorta impingement when placing screws on the concave side of the thoracic spine [6–9]. However, the majority of such studies have always paid attention to the relative position of the aorta to thoracic vertebrae, and there was little information concerning the relative position of the aorta to thoracolumbar or lumbar vertebrae [6–10]. Moreover, these studies did not include curve pattern into consideration as most studies were performed on patients with right-sided thoracic curves and did not compare the risk of the aorta impingement among different curve patterns. We postulated that the position of and the impingement risk of the aorta might be different among various curve patterns of AIS. The purpose of this study was to compare the positions of the aorta relative to vertebral bodies and the potential risk of the aorta impingement for PS placement between right- and left-sided thoracolumbar/lumbar curves of AIS.
Materials and methods
A retrospective review of AIS patients from our hospital database who had CT images of the lower thoracic and lumbar spine from January 2009 through October 2011 was performed. The following inclusion criteria were applied: (1) a single main thoracolumbar or lumbar curve with thoracic curves <25°; (2) Cobb angle: 40° ~ 70°; (3) normal thoracic kyphosis without thoracolumbar junctional kyphosis, and (4) no previous spinal or/and cardiothoracic surgery. Patients with a known congenital vascular abnormality were excluded from the study. Thirty-nine patients were recruited. The Lenke’s classification was type 5C in all patients. According to the convexity of the thoracolumbar/lumbar curve, the patients were divided into either Group R or Group L. The patients in Group R had a main right-sided thoracolumbar/lumbar curve, and those in Group L had a main left-sided thoracolumbar/lumbar curve. In both groups, the curves were measured on standard standing posterior-anterior X-ray radiographs according to the Cobb method, and the heights of subjects were measured. The corrected heights were calculated using Bjure formula (Log y = 0.011x + 0.177, where y is the loss of trunk height (cm) caused by the spinal deformity, and x is the Cobb angle of the primary curve) [11].
CT measurements
The CT scans were performed using a spiral CT scanner (LightSpeed, GE Healthcare) with the following parameters: 320 mAs, 120 kVP,, and 5-mm thickness with a 5-mm gap between the slices. To quantify the relative positions of the aorta to vertebrae, the following radiographic parameters were measured from the CT imagines of the middle transverse planes of vertebrae from T12 through L4:
-
1.
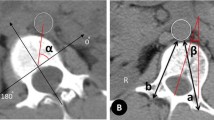
Aorta-vertebra angle (α) (Fig. 1): subtended by the tangent line of the anterior margin of vertebral canal and the line from the posterior midpoint of the vertebral body to the midpoint of the aorta. The angle was defined as 0° when the aorta was located directly laterally to the left, 90° when it was located strictly anteriorly, and 180° when it was located directly laterally to the right [8].
Fig. 1 Illustration of parameters measured on the CT images. A A 16-year-old female patient with AIS had a left lumbar curve of 53°. α: Aorta-vertebra angle. B A 15-year-old female patient with AIS had a right lumbar curve of 49°. βo Vertebral rotation angle a Left safety distance (LSD) b Right safety distance (RSD)
-
2.
Vertebral rotation angle (β) (Fig. 1): formed between a perpendicular line starting from the posterior central aspect of the spinal canal and a straight line through the posterior central aspect of the spinal canal and the middle of the vertebral body [12].
-
3.
Left safety distance (LSD) (Fig. 1): the line connecting the ideal entry point of the left PS (middle of the base of the left superior facets) and the posterior edge of the aorta.
-
4.
Right safety distance (RSD) (Fig. 1): the line connecting the ideal entry point of the right PS (middle of the base of the right superior facets) and the posterior edge of the aorta.
Potential risk of aorta impingement from PS placement
We simulated placements of the PSs. The lengths of screws were 35, 40, and 45 mm (three scenarios). The aorta was considered at a potential risk of impingement when the safety distance (LSD or RSD) was less than pedicle screw length. The percentages of the vulnerable aorta on right and left sides of the spine at all levels were analyzed.
Statistical analysis
The data were analyzed using SPSS 13.0 for Windows (Chicago, IL). A related two-sample test (the Wilcoxon signed-rank test) was performed to determine the differences between the two groups. Significance was defined as a P value <0.05. The percentages of aorta at a potential risk of impingement were calculated on both sides in AIS patients to analyze the risks of the aorta impingement from PS placemen in three scenarios.
Results
The study cohort consisted of 39 female AIS patients: 17 patients with a right-sided thoracolumbar/lumbar curve were assigned to Group R, and 22 patients with a left-sided thoracolumbar/lumbar curve were assigned to Group L. The average age of the patients was 15.2 years (range, 12–18 years) in Group R and 14.9 years (range, 12–18 years) in Group L. No difference in either the ages or the Risser signs was found between the two groups (P > 0.05). In Group R, the Cobb angles of the thoracolumbar/lumbar curves ranged from 41 to 50 , with an average of 43 while in Group L, the Cobb angles of the thoracolumbar/lumbar curves ranged from 42 to 58 with an average of 47.5. The mean corrected height was 162.4 cm (range, 157–168 cm) in Group R, and 161.7 (range, 154–169 cm) in Group L. No significant difference of the corrected heights was noted between two groups (P > 0.05).
CT measurement
A total of 85 vertebrae were measured in Groups R and 110 in Group L; the results are summarized in Table 1. The α increased gradually from T12 through L4 in Group R, increased from T12 through L1, and decreased from L1 through L4 in Group L, which suggested that the aorta moved from the left side of the vertebra to a more anterior position from T12 through L4 in patients with right-sided thoracolumbar/lumbar curves while moved from the right anterolateral side of the vertebrae to the front of vertebral body from L1 through L4 in patients with left-sided thoracolumbar/lumbar curves (Fig. 2).
The LSD constantly increased from T12 through L4 in Group R, increased from T12 through L3, and then decreased from L3 through L4 in Group L. The RSD showed a similar tendency in both groups, increased from T12 through L3, and decreased from L3 through L4 (Fig. 2).
Potential risk of the aorta impingement
The percentages of the aorta at a potential risk of the aorta impingement from PS insertion were demonstrated in Table 2. With the increment of the lengths of the simulated screws, the aorta impingement risks were constantly elevated at all levels in both groups.
The aorta was at a high risk of impingement from left PS placement irrespective of the diameters of the simulated screws in Group R (80–100 % at T12 and 53.3–100 % at L1). In Group L, the aorta was safe when using 35 mm (0 at all levels) PS and at risks of impingement from 45 mm PS placement on the right pedicles (31.8–72.7 %). In all, the risks of the aorta impingement were mainly from left PS in Group R and from right PS in Group L, and the risk of the aorta impingement from PS placement were generally higher in right-sided thoracolumbar/lumbar curves when compared with the left-sided curves.
Discussion
The aorta tends to follow the concavity of the curve [6]. For right thoracic curves, the thoracic aorta shifted to the left side of the curves and was positioned more left laterally and posteriorly to the vertebral body, while for left thoracic curves it moved to the right and was positioned anterior to the vertebral body. Milbrandt et al. [7] ascribed the changes of the relative position of the aorta to vertebral body to the tethering effect of diaphragm. The aorta was caught in place by the surrounding crux of the diaphragm and then forced into the concave side of the curves for it is the shortest distance between the top and the bottom of the chest cavity, as is especially true for the lumbar aorta. In a normal subject, the aorta is not located at the middle front of vertebral body, but at a center-left position to vertebral body in thoracolumbar and lumbar region (12 to 1 o’clock position using a clock analogy) (Fig. 3). In left thoracolumbar/lumbar curves, as vertebra rotates towards the left, the aorta relatively shifts towards the right, and stops at the direct front of vertebral body, further from the posterior entry point. In right curves, as vertebra rotates towards the right, the aorta further shifts towards the left, and goes closer to the left posterior entry point, elevating the risks of the aorta impingement. The subsequent measurement demonstrated that the mean distances between the aorta and the left posterior entry point almost reached 45 mm at all levels in left curves, but less than 35 mm at T12 and L1 levels in left curves. It meant that the aorta had more possibilities of being impinged in right thoracolumbar/lumbar curves than in left curves.
Different relative positions of the aorta to L1 vertebrae. A No spinal deformity. The aorta was at a center-left position to vertebral body. The α angle was 80°, and the distance from the aorta to the left posterior entry point for screw (b) was 41 mm; B left lumbar scoliosis. The aorta was located laterally to the left wall of vertebral body. The α angle was 62°, and the b distance was 36 mm; C right lumbar scoliosis. The aorta was at the middle-front of the vertebral body. The α angle was 94°, and the b distance was 46 mm
Previous studies set different scenarios that simulated screw placement with different lengths and trajectory error angles to analyze the risks of the aorta impingement from PS [13, 14]. We feel that the safety distance may be more important than the angle of trajectory for risks analysis. From a surgical standpoint, surgeons always want to place PS following an ideal trajectory, and when malposition occurred, the trajectory error angles could not be anticipated. Moreover, as the lumbar aorta is located in front of the vertebral body, the ideal trajectory always directly passes the aorta. Ignoring the length of PS, the aorta was always at impingement risks even when the PSs were precisely placed. Actually, the aorta was at impingement risks only when the screw length was larger than the distance between entry points and the aorta (Fig. 2). Therefore, we simulated three scenarios for screw placement based on the screw length and the distance between entry point and aorta without taking trajectory error angle into consideration. The risk analysis showed that the aorta impingement risks were constantly elevated when the diameters of the simulated screws increased especially in right curves. Obviously, the shorter the screw length, the smaller the risk of aorta impingement, and 35 mm PSs seem to carry smaller risks of the aorta impingement at thoracolumbar region when compared with 40 mm PSs. However, the difference of the risks was not significant, and 40 mm PS could provide bigger fixation strength. Moreover, the aorta at thoracolumbar region largely deviated from the ideal trajectory of PS in right curves, and PSs were rarely placed at such a big error angle. Based on these facts, we still recommend using 40 mm at thoracolumbar vertebrae in right curves.
After comparing the risks of impingement between left-sided and right-sided thoracolumbar/lumbar curves, we found that the risks of the aorta impingement were mainly from left PS in right-sided curves and from right PS in left-sided curves. As has been mentioned, with the rotation of vertebrae, the PS entry points at concave side of curves approximate the aorta, thus shortening the safety distance for PS placement (Fig. 4). In addition, the risks of the aorta impingement were generally higher in right-sided curve, especially in T12 and L1 levels (82.4 and 52.9 % using 35 mm PSs while 100 and 88.2 % using 40 mm PSs), which could be ascribed to the more posterior position of the aorta in right-sided curve (Fig. 5). Globally, placing PS carries more risks in right-sided curve than in left-sided curve. Besides, the spinal cord tends to shift to the concave side, which further elevates the risks of neurovascular complication for left PS placement in right-sided thoracolumbar/lumbar curves.
The average course of the aorta relative to the spine in right and left thoracolumbar/lumbar curves. The point was defined by the mean aorta-vertebra angle and the mean left safety distance at each level. The aorta surrounded the left half of the vertebral bodies in right thoracolumbar/lumbar curves while surrounding the right half of the vertebral bodies in the left, and the relative positions of the aorta to vertebral bodies were more posterolateral in right curves when compared with those in the left
Conclusion
The present study illustrated the different migration of the aorta relative to vertebrae in thoracolumbar/lumbar curves with different convexities. In right-sided curve, the risks of the aorta impingement were mainly from left-side PS while mainly from right-side PS in left-sided curves. The aorta was more proximal to the left posterior cortical entry point in right-sided thoracolumbar/lumbar curve than in left-sided curve. Surgeons should be particularly cautious when placing PSs on the concave sides of T12 and L1 vertebrae of right thoracolumbar/lumbar curves.
References
Halm H, Niemeyer T, Link T, Liljenqvist U (2000) Segmental pedicle screw instrumentation in idiopathic thoracolumbar and lumbar scoliosis. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 9(3):191–197
Suk SI, Kim WJ, Lee SM, Kim JH, Chung ER (2001) Thoracic pedicle screw fixation in spinal deformities: are they really safe? Spine 26(18):2049–2057
Hicks JM, Singla A, Shen FH, Arlet V (2010) Complications of pedicle screw fixation in scoliosis surgery: a systematic review. Spine 35(11):E465–E470. doi:10.1097/BRS.0b013e3181d1021a
Qiu Y, Wang S, Wang B, Yu Y, Zhu F, Zhu Z (2008) Incidence and risk factors of neurological deficits of surgical correction for scoliosis: analysis of 1373 cases at one Chinese institution. Spine 33(5):519–526. doi:10.1097/BRS.0b013e3181657d93
Moore KL (2010) The thoracic and abdominal aorta. In: Moore KL (ed) Clinically Oriented Anatomy. Williams and Wilkins, Baltimore, pp 167–313
Sucato DJ, Duchene C (2003) The position of the aorta relative to the spine: a comparison of patients with and without idiopathic scoliosis. J bone jt surg Am 85-A(8):1461–1469
Milbrandt TA, Sucato DJ (2007) The position of the aorta relative to the spine in patients with left thoracic scoliosis: a comparison with normal patients. Spine 32(12):E348–E353. doi:10.1097/BRS.0b013e318059aeda
Wang W, Zhu Z, Zhu F, Wang B, Chu WC, Cheng JC, Qiu Y (2008) The changes of relative position of the thoracic aorta after anterior or posterior instrumentation of type I Lenke curve in adolescent idiopathic thoracic scoliosis. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 17(8):1019–1026. doi:10.1007/s00586-008-0691-0
Qiu Y, He YX, Wang B, Zhu F, Wang WJ (2007) The anatomical relationship between the aorta and the thoracic vertebral bodies and its importance in the placement of the screw in thoracoscopic correction of scoliosis. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society 16(9):1367–1372. doi:10.1007/s00586-007-0338-6
Zhu F, Chen WJ, Wang WJ, Wang B, Zhu ZZ, Zhu B, Qiu Y (2011) Migration of thoracic aorta after the anterior correction of thoracic idiopathic scoliosis without parietal pleura closure. J spinal disord tech 24(6):390–396. doi:10.1097/BSD.0b013e3182019f1a
Bjure J, Grimby G, Nachemson A (1968) Correction of body height in predicting spirometric values in scoliotic patients. Scand J Clin Lab Invest 21(2):191–192
Krismer M, Bauer R, Sterzinger W (1992) Scoliosis correction by Cotrel-Dubousset instrumentation. The effect of derotation and three dimensional correction. Spine 17(8 Suppl):S263–S269
Takeshita K, Maruyama T, Ono T, Ogihara S, Chikuda H, Shoda N, Nakao Y, Matsudaira K, Seichi A, Nakamura K (2010) New parameters to represent the position of the aorta relative to the spine for pedicle screw placement. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 19(5):815–820. doi:10.1007/s00586-010-1298-9
Takeshita K, Maruyama T, Sugita S, Oshima Y, Morii J, Chikuda H, Ono T, Nakamura K (2011) Is a right pedicle screw always away from the aorta in scoliosis? Spine 36(23):E1519–E1524. doi:10.1097/BRS.0b013e31820f8e6b
Acknowledge
This work was supported by the Natural Science Foundation of Jiangsu Province, China (BK2009001). No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
J. Qiao and F. Zhu contributed equally to this work.
Rights and permissions
About this article
Cite this article
Qiao, J., Zhu, F., Xu, L. et al. Comparison of the aorta impingement risks between thoracolumbar/lumbar curves with different convexities in adolescent idiopathic scoliosis: a computed tomography study. Eur Spine J 21, 2043–2049 (2012). https://doi.org/10.1007/s00586-012-2315-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-012-2315-y