Abstract
It is not known whether the results of decompressive surgery to treat the mild and moderate forms of spondylotic cervical myelopathy (CSM) are any better than those of a conservative approach. A 10-year prospective randomised study was performed. The objective of the study was to compare conservative and operative treatments of mild and moderate, non-progressive, or slowly progressive, forms of CSM. Sixty-four patients were randomised into two groups of 32. Group A was treated conservatively while group B was treated surgically. The clinical outcome was evaluated by modified JOA score, timed 10-m walk, score of daily activities recorded by video and evaluated by two observers blinded to the type of therapy, and by subjective assessment by the patients themselves. Seventeen patents died of natural, unrelated causes, during the follow-up. A total of 25 patients in the conservatively and 22 in the surgically treated group were used for the final evaluation. There was no statistically significant difference between both groups in mJOA score, in subjective evaluation by the patients themselves and in evaluation of video-recordings of daily living activities by two observers blinded to treatment mode. There was neither any difference found in the percentage of patients losing the ability to walk nor in the time taken to cover the 10-m track from a standing start. Comparison of conservative and surgical treatment in mild and moderate forms of CSM in a 10-year follow-up has not shown, on average, a significant difference in results. In both groups, patients get better and worse. According to the power analysis it is necessary admit that these results possess the low ability to answer definitely the question which treatment is better for the patients with a mild and moderate non-progressive CSM because of the low number of patients for the final evaluation and for clinically negligible differences between two compared arms. These findings can serve as a worthy odds-on hypothesis which needs the confirmation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The treatment of mild and moderate forms of cervical spondylotic myelopathy (CSM) remains a matter of perennial uncertainty. It appears altogether logical to remove the spondylotic compression of the spinal cord surgically. However, there is not enough data available for surgeons to predict accurately when and for whom operative management is definitely indicated in this subgroup of CSM patients—which represents, incidentally, the majority. Many papers record excellent results with surgery but all of them are retrospective studies without control groups, randomisation or the standard criteria of clinical evaluation, with short follow-up [1–6]. There is still a surprising lack of high-quality series.
In this study, we compare conservative and surgical treatment in a long-term follow-up.
Design of the study
A 10-year follow-up, prospective, randomised and blinded clinical study was performed. A group of patients with non-progressing or very slowly progressing mild and moderate clinical spondylotic cervical myelopathy (mJOA score ≥ 12 points) was randomised into two arms, to be treated surgically or conservatively. The study was approved by local ethical committee.
Population
The study sample consisted of 64 consecutive subjects, drawn from patients referred to the neurological department between 1993 and 1999, with clinical signs and symptoms of spondylotic cervical myelopathy (46 men and 18 women). Both groups consisted of 32 subjects.
The entry profiles of the patients studied are summarised in Table 1. No significant differences between groups were found in any of the parameters followed.
Inclusion criteria:
-
Clinical signs and symptoms of cervical cord dysfunction,
-
Magnetic resonance imaging (MRI) criteria for cervical mono- and multisegmental cord compression and/or myelopathy due to spondylosis (including soft disc herniations—see below) with or without developmentally narrow spinal canal,
-
Age under 75 years,
-
Modified Japanese Orthopaedic Association score ≥12 points,
-
Patient’s consent to surgery.
Exclusion criteria:
-
Decompensated depression,
-
Vascular encephalopathy (dementia, hemiparesis, aphasia),
-
Contraindications to surgery: diabetes mellitus, alcoholism, cardiovascular and lung diseases, blood dyscrasias, significant osteoporosis,
-
Previous surgery on the cervical spine,
-
Inability to engage actively in postoperative rehabilitation,
-
Uncertainty about the presence of significant additional diseases (such as motor neurone disease, multiple sclerosis, progressive polyarthritis).
Clinical evaluation
The clinical grading system proposed by the Japanese Orthopaedic Association, as modified by Benzel (mJOA: maximum 18 points), was utilised to quantify neurological function before enrolment in the study and then at 10 years [7].
Evaluation of daily activities by video recording
A video recording was made on enrolment in the study and then 10 years later. The recordings consisted of patients showing how they buttoned their shirt, brushed their hair and teeth, how they performed alternate rotation of the hands at maximal speed, how they put their shoes on, walked and ran, and how they went up and down stairs. These were evaluated by two physicians blinded to the type of treatment. The observers assessed the patients’ functional abilities using the following scale of improvement: excellent +3 points, very good +2, slightly better +1, no change 0, and of deterioration: slightly worse −1, much worse −2, poor −3.
Timed 10-m walk
This was measured as the time (in seconds) spent on a 10-m track (“walk as fast as possible, but don’t run”) from a standing start, at 0 and 10 years.
Subjective estimation of the patients themselves
The patients evaluated their own clinical status according to the following semi-quantitative scale: excellent +3 points, very good +2, slightly better +1, no change 0, and of deterioration: slightly worse −1, much worse −2, poor −3.
Statistical methods
Only patients reaching the long-term follow-up point of more than 10 years were included in the analyses; expired patients were only summarised in overall survival curves. Three patients originally recruited in the conservative arm were subsequently treated by surgery and were, therefore, excluded prior to the analyses. The indication for the surgery in all these cases was psychological rather than progression marked by objective clinical symptoms.
Standard robust summary statistics were used to describe primary data: median and 5th–95th percentile range for the description of continuous characteristics of patients, relative frequencies for description of binary characteristics.
The summarizing analysis of overall survival for patients in both groups was worked out by standard Kaplan–Meier approach; statistical analysis of significance of difference in overall survival was tested using log-rank test.
Differences between the groups were analyzed by means of Mann–Whitney U test for continuous variables and by maximum likelihood Chi-square test for binary variables. Agreement between experts evaluating patients’ video records was tested by means of the McNemar test.
Methodology
The power analysis was computed using PS—Power and Sample Size Calculation software [8]. For the computation of detectable differences in percentages using Chi-square test the methodology according to Fleiss [9] was adopted. For the detectable alternative of Mann–Whitney U test the adjustment of results from corresponding t test was applied. If the t test model is valid, and N designates the sample size necessary for the t test to achieve some given power, then the sample size N (Mann–Whitney U test) = N (t test)/A.R.E. yields approximately the same power for the U test. A.R.E. denotes the asymptotic relative efficiency of the U test relative to the t test which is 3/PI = 0.955 [10]. All computations were made using α = 0.05 and 1−β (power) = 0.80.
Results
-
1.
A basic description of the study groups at the time of the final evaluation after 10 months of follow-up is shown in Table 2.
Table 2 Basic description of the study group -
2.
Differences between the pre-study and the post-study mJOA scores are presented in Table 3. There was no statistically significant difference between conservatively and surgically treated groups. The same is true of the subjective evaluation by the patients themselves and in evaluation of video-recordings of daily living activities by two observers blinded to treatment mode. There was neither any difference found in the percentage of patients losing the ability to walk nor in the time taken to cover the 10-m track from a standing start (Table 4).
Table 3 Statistical evaluation of study end-points at the end of the study Table 4 Results of 10-m walk test at the end of the study -
3.
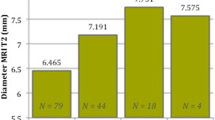
Seventeen patients across the groups studied died of natural causes in the course of the follow-up. None of their deaths was in direct association with the surgery or CSM. Ten patients of the surgery group expired and seven of those treated conservatively. A comparison of the two groups appears in Fig. 1.
-
4.
According to power analysis, the study did not prove any superiority between the study arms and the long-term monitoring confirmed only negligible differences in the outcome of adopted therapeutic strategies. The main added value of the findings is in long-term follow-up, accompanied with methodically and protocol-based monitoring of the patients. Such a long-term study unfortunately suffers from decreased sample size due to events which cannot be expected, including death of patients. Nevertheless, all found differences between the study arms are not only apparently lower than statistically given detectable differences but also most of them are clinically negligible. These findings can serve as worthy data and hypothesis which needs a further confirmation.
Discussion
While surgical intervention in patients with compressive cervical myelopathy appears logical, it should first be clearly shown that such an approach is better than the natural course of the disease or conservative treatment. This holds particularly true for the mild and moderate forms of the complaint, without progression or with very slow progression. Importantly, these represent the majority of patients with CSM.
Convincing information about the natural history of CSM is still lacking, in spite of its prerequisite role in developing a rational plan for treatment and for measurement of effectiveness [11]. Only a few retrospective studies, coming to sometimes controversial conclusions, are available. There is a tendency for CSM patients to progress to severe disability, but it is not known to what degree or how quickly, how many patients in the population might suffer, or what method is suitable for identifying these patients in advance.
Reports from some series refer to a steady progression in all patients [12–16], while another study has reported 67% of patients as exhibiting steady, progressive deterioration [17]. On the other hand, still further retrospective studies have shown that the disability is mild in the majority of cases, and that the prognosis for these mildly affected cases, and even for the more severely disabled, is good [18–20]. The only feature associated with deterioration was age. Retrospective studies, however, are prone to considerable bias. Given the current level of the knowledge, we can merely summarise that the natural history of these forms of CSM is not precisely known, and that there is a tendency to deteriorate, to remain stable or to improve with approximately the same degrees of probability. No reliable prognostic factor is known that enables the determination of the outcome in the individual patient. Almost all existing studies are retrospective and lacking in standard and commonly accepted criteria; they merely provide some plausible hypotheses.
Several critical reviews claim that the surgical treatment of myelopathy, especially of mild and moderate forms, has not clearly shown better results than conservative treatment, and that criteria for the indication and timing of the operation have not been established [21–25]. Surgical treatment is an expensive procedure which, like every major operation, involves its own risks [26–28]. Furthermore, this treatment is associated with the risk of operating on a patient with an irrelevant compression, because of the difficulty in distinguishing other types of myelopathy (multiple sclerosis, motor neurone disease, primary lateral sclerosis, vitamin B12 deficiency, arterio-venous malformations, cervical spinal tumour, syringomyelia or their combination with CSM). In CSM patients, as many as 41% of compressions found by magnetic resonance scanning are clinically asymptomatic [28].
Prospective studies of the surgical approach to this disease are generally lacking. The results of our own randomised prospective study revealed no important difference in outcome for the patients with mild and moderate forms of CSM treated surgically or conservatively over a 36-month period [30, 31]. However, in both groups, part of the patient pool improved and part deteriorated. These results indicate the prognostic factors for good results, different for each group, and have been published elsewhere [31]. The results of this series did not change the conclusions and suggestions appearing here.
In the whole study group, 17 patients expired in the course of the 10 years. They died of natural causes unrelated to the type of treatment. The difference between the groups was not statistically significant.
Conclusions
Comparison of conservative versus surgical treatment in mild and moderate forms of CSM in a 10-year follow-up has not shown, on average, a significant difference in their outcomes. In both groups, patients get better and worse. However, according to the power analysis it is necessary to admit that these results could not answer definitely the question which treatment is better for the patients with mild and moderate non-progressive CSM because of low number of patients for final evaluation and for clinically negligible differences between two compared arms.
References
Nurick S (1972) The pathogenesis of the spinal cord disorder associated with cervical spondylosis. Brain 95:87–100
Kato Y, Iwasaki M, Fuji T et al (1998) Long-term follow-up results of laminectomy for cervical myelopathy caused by ossification of the posterior longitudinal ligament. J Neurosurg 89:217–223
Goto S, Mochizuki M, Watanabe T et al (1993) Long-term follow-up study of anterior surgery for cervical spondylotic myelopathy with special reference to the magnetic resonance imaging findings in 52 cases. Clin Othop Rel Res 291:142–153
Hirai O, Kondo A, Aoyama I et al (1991) Anterior decompression surgery of aged patients with cervical myelopathy. No Shinkei Geka 19:1017–1023
Singh A, Choi D, Crockard A (2009) Use of walking data in assessing operative results for cervical spondylotic myelopathy: long-term follow-up and comparison with controls. Spine 34(12):1296–1300
Matsumoto M, Chiba K, Ishikawa M et al (2001) Relationships between outcomes of conservative treatment and magnetic resonance imaging findings in patients with mild cervical myelopathy caused by soft disc herniations. Spine 26:1592–1598
Benzel EC, Lancon J, Kesterson L et al (1991) Cervical laminectomy and dentate ligament section for cervical spondylotic myelopathy. J Spin Disord 4:286–295
Dupont WD, Plummer WD (1997) PS power and sample size program available for free on the Internet. Controlled Clin Trials 18:274
Fleiss JL (1981) Statistical methods for rates and proportions, 2nd edn. John Wiley, NewYork, pp 38–46
Lehmann EL (1975) Nonparametrics. Statistical methods based on ranks. Holden-Day, San Francisco
LaRocca H (1988) Cervical spondylotic myelopathy: natural history. Spine 13:854–855
Clarke E, Robinson PK (1956) Cervical myelopathy: a complication of cervical spondylosis. Brain 79:483–510
Epstein JA, Janin Y, Carras R et al (1982) A comparative study of the treatment of the cervical spondylotic myelopathy. Experience with 50 cases treated by means of extensive laminectomy, foraminotomy, and excision of osteophytes during the past 10 years. Acta Neurochir 61:89–104
Montgomery DM, Brower RS (1992) Cervical spondylotic myelopathy. Clinical syndrome and natural history. Orthop Clin North Am 23:487–493
Sadasivan KK, Reddy RP, Albright JA (1993) The natural history of cervical spondylotic myelopathy. Yale J Biol Med 66:235–242
Symon L, Lavender P (1967) The surgical treatment of cervical spondylotic myelopathy. Neurology 17(2):117–127
Nurick S (1972) The pathogenesis of the spinal cord disorder associated with cervical spondylosis. Brain 95:87–100
Shimomura T, Sumi M, Nishida K et al (2007) Prognostic factors for deterioration of patients with cervical spondylotic myelopathy after nonsurgical treatment. Spine 32:2474–2479
Lees F, Turner JWA (1963) Natural history and prognosis of cervical spondylosis. Br Med J 2:1607–1610
Utley D, Monro P (1989) Neurosurgery for cervical spondylosis. Br J Hosp Med 42:62–70
Rowland LP (1992) Surgical treatment of cervical spondylotic myelopathy. Time for a controlled trial. Neurology 42:5–13
Law MD, Bernhardt M, White AA (1994) Cervical spondylotic myelopathy: a review of surgical indications and decisions making. Yale J Biol Med 66:165–177
Braakman R (1994) Management of cervical spondylotic myelopathy and radiculopathy. J Neurol Neurosurg Psychiatry 57:257–263
Ebersold MJ, Pare MC, Quast CM (1995) Surgical treatment for cervical spondylitic myelopathy. J Neurosurg 82:745–751
Yonebobu K, Hosono N, Iwasaki M et al (1991) Neurologic complications of surgery for cervical spondylotic myelopathy. Spine 16:1277–1282
Gok B, Sciubba DM, McLoughlin GS et al (2008) Revision surgery for cervical spondylotic myelopathy: surgical results and outcome. Neurosurgery 63:292–298
Xu BS, Zhang ZL, Le Huec JC et al (2009) Long-term follow-up results and radiographic findings of anterior surgery with Cloward trephination for cervical spondylotic myelopathy. Spinal Disord Tech 22:105–113
Okamoto A, Shinomiya K, Furuya K et al (1991) Postoperative magnetic resonance in patients with cervical myelopathy. Spine 39:263–267
Kadanka Z, Bednarik J, Vohanka S et al (2000) Conservative treatment versus surgery in spondylotic cervical myelopathy: a prospective randomised study. Eur Spine 9:538–544
Kadanka Z, Mares M, Bednarik J et al (2002) Approaches to spondylotic cervical myelopathy: conservative vs surgical results in a three-year follow-up study. Spine 27:2205–2211
Kadaňka Z, Mareš M, Bednařík J et al (2005) Predictive factors for mild forms of spondylotic cervical myelopathy treated conservatively or surgically. Eur J Neurol 12(1):16–24
Acknowledgments
The study was supported by the Czech Ministry of Education Research Plan No.: MSM 0021622404.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kadaňka, Z., Bednařík, J., Novotný, O. et al. Cervical spondylotic myelopathy: conservative versus surgical treatment after 10 years. Eur Spine J 20, 1533–1538 (2011). https://doi.org/10.1007/s00586-011-1811-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-011-1811-9