Abstract
The aim of the present study was to investigate the 2-year outcome of a cognitive-behavioral training program for the management of depressive symptoms for patients with chronic low back pain (CLBP) and co-existing depressive symptoms compared with the standard rehabilitation. Therefore, a quasi-experimental 3 × 2 × 5 (treatment condition × gender × time) repeated measures design with five assessment points (pre-treatment, post-treatment, 6-, 12-, and 24-month follow-up) was employed among N = 153 patients with CLBP, aged 33–62 years. Patients were consecutively assigned to one of three treatment conditions: patients with no or mild depressive symptoms were treated with the standard rehabilitation (CG) and patients with moderate or severe depressive symptoms were either treated with the standard rehabilitation (CGdepr) or the standard rehabilitation plus cognitive-behavioral management of depressive symptoms (IGdepr). Patients in the IGdepr significantly improved in mental health up to the 6-month follow-up and in anxiety and depressive symptoms up to the 24-month follow-up. Only short- or mid-term improvements were found in the CGdepr. In conclusion, the new cognitive-behavioral training program augmented the long-term rehabilitation success in this highly strained subgroup of patients with CLBP and depressive symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There has been growing evidence that psychological factors, specifically depressive symptoms, play a crucial role in the development of chronic low back pain (CLBP; [1, 2]). Co-morbid depression among patients with chronic musculoskeletal pain was associated with more severe pain, enhanced pain-related disability, and reduced health-related quality of life [3]. Furthermore, it has been suggested that depressive symptoms may interfere with successful rehabilitation in patients with chronic pain [4, 5]. While van der Hulst, Vollenbroek-Hutten, and Ijzerman [6] found no predictive validity of depressive symptoms for rehabilitation success, a lower rehabilitation success was demonstrated in patients with moderate or severe depressive symptoms who underwent orthopedic inpatient rehabilitation of CLBP [7].
Previous research has provided evidence that multidisciplinary approaches integrating cognitive-behavioral components showed more beneficial short-term effects than no-treatment, waiting list control, or solely medically orientated programs in the rehabilitation of CLBP [8–10]. However, no clear evidence for the superior long-term effects of behavioral therapy compared to no-treatment, usual care, or other active treatments was found [11, 12]. It may be assumed that more specific interventions aimed at reducing co-existing psychological impairments could improve rehabilitation success, particularly long-term effects in the rehabilitation of CLBP. Hence, the implementation of cognitive-behavioral interventions specifically targeting depressive symptoms seems to be indicated (see [1, 5]).
Finally, a higher prevalence of low back pain, greater pain-related impairments, and a higher prevalence of psychiatric co-morbidity have been observed among women compared with men [13–15]. Thus, women with CLBP are at high-risk for further development of chronic pain. Likewise, inconclusive findings were found for gender-related differences in the treatment outcomes in CLBP; the various studies have found better outcomes among women [7, 16], better rehabilitation effects in men [17], or no differences [6]. Therefore, more research is needed regarding gender-specific effects in CLBP rehabilitation.
As a final analysis of our 1-year longitudinal study [18], the purpose here was to examine gender-specific long-term effects of an additional cognitive-behavioral training program for the management of depressive symptoms compared with the standard rehabilitation among patients with CLBP and co-existing depressive symptoms during a period of 2 years. Moreover, a third group of patients with no or mild depressive symptoms was treated with the standard rehabilitation, which has been proven to be effective among this subgroup [7]. In our 1-year follow-up, favorable long-term rehabilitation effects were observed for psychological outcome measures [18]. Hence, the results presented here focus on depressive symptoms, anxiety, and mental health.
Methods
Design and procedure
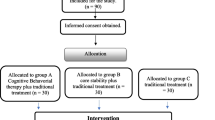
A quasi-experimental trial was conducted with a 3 × 2 × 5 repeated measures design with treatment condition and gender as between-subjects factors and time of assessment as the within-subjects factor. The treatment condition consisted of three groups: the control group comprising patients with no or low depressive symptoms (CG; n = 69), the control group comprising patients with moderate or severe depressive symptoms (CGdepr; n = 40), and the intervention group comprising patients with moderate or severe depressive symptoms (IGdepr; n = 44). All patients participated in the standard rehabilitation program, but patients in the IGdepr were additionally treated with the cognitive-behavioral training program for the management of depressive symptoms. The dependent factor of time consisted of 5 sample points: pre-treatment (t 1), post-treatment (t 2), 6-month follow-up (t 4), 12-month follow-up (t 5), and 24-month follow-up (t 6). Another sample point 3 months post-treatment (t 3) was not included in the analyses. These data were gathered 3 months post-treatment to replicate the results of a pilot study investigating effects of depressive symptoms on rehabilitation success in CLBP rehabilitation [7].
Patients were consecutively referred to the study. During the initial physical consultation, diverse medical and functional data were gathered and patients were informed about the study aims. For the purpose of assignment, depressive symptoms were assessed by the German version of the Center of Epidemiologic Studies-Depression Scale (Allgemeine Depressions-Skala, ADS; [19]). The assignment was conducted by an independent doctoral student at the University of Bremen. Thus, the physicians and nursing staff at both clinics were blinded to the patients’ group assignments (for further details, see [18]).
The study had received full approval of the Institutional Review Board of the University of Bremen.
Participants
A total of N = 153 patients with CLBP for at least 6 months, seeking treatment from two inpatient rehabilitation clinics with orthopedic units, was included in the study (for a detailed description of inclusion and exclusion criteria see Table 1). Data were collected between April 2006 and February 2009.
The sample ranged from 33 to 62 years with a mean age of 50.5 years (SD 6.1), and 45.1% were female. Complete sample characteristics are presented in Table 2. As expected, patients in the CG were significantly less impaired in depressive symptoms, anxiety, and mental health compared to patients in the CGdepr and IGdepr prior to rehabilitation. Furthermore, compared to the CGdepr, patients in the IGdepr showed a significantly greater frequency of taking more than 14 days of sick leave within 3 months prior to inclusion. At the same time, women reported significantly more severe depressive symptoms, anxiety, and mental health, higher frequencies of unemployment and stage of chronicity III, and more pain sites than men.
Treatment
All patients participated in a multidisciplinary standard rehabilitation in orthopedic inpatient units following a bio-psycho-social approach of CLBP, lasting 3 to 4 weeks (for evidence-based health care in CLBP, see [19]). The standard program was comprised of diverse evidence-based treatment modules including four 1-h sessions of cognitive-behavioral pain-management. Additionally, five 1-h sessions of cognitive-behavioral management of depressive symptoms was implemented in the IGdepr. For brevity, essential elements of the cognitive-behavioral programs are summarized below. For a detailed description, see [18].
The cognitive-behavioral pain-management training was aimed at providing a bio-psycho-social concept of chronic pain. Pain-eliciting and pain-exacerbating cognitions, emotions, and behavioral patterns were discussed. Moreover, the participants acquired skills to manage pain and stress to promote self-management competencies and self-efficacy expectations.
The cognitive-behavioral training program for the management of depressive symptoms was aimed at imparting knowledge about the relationship between pain perception and somatic, emotional, cognitive, and behavioral depressive symptoms. The training comprised behavioral activation, cognitive restructuring, and social skills training. Additionally, cognitive and behavioral adaptive coping strategies were acquired.
Outcome measures
Depressive symptoms were assessed by the German version of the CES-D (ADS; [20]). The ADS is a 20-item questionnaire that measures severity of depressive symptoms over the past 2 weeks on a four-point scale (0 = ‘seldom’, 3 = ‘mostly’; response range 0–60). The recommended cut-off score of 24 was applied.
Anxiety was measured using the subscale anxiety of the German version of the Hospital Anxiety and Depression Scale (HADS-D), comprising 7 items rated on a four-point scale (0 = ‘not at all’, 3 = ‘mostly’; response range 0–21) with reference to the past 2 weeks [21]. Scores of 11 or higher were evaluated as clinically significant.
To measure mental health, the subscale mental health of the German version of the Short-Form-12 (SF-12) was applied using 6 items with reference to the past 2 weeks [22]. A standard score from 0 to 100 was yielded, with higher scores indicating better health status.
Statistical analyses
Univariate two-way repeated measures analyses of variance (ANOVA) were performed with treatment condition (CG, CGdepr, IGdepr) and gender (male, female) as between-subjects factors and time of assessment (t 1, t 2, t 4, t 5, t 6) as the within-subjects factor. Finally, mean comparisons by Bonferroni were carried out to detect independent and dependent mean differences. A two-tailed significance level test was set at p < 0.05. Moreover, between and within-group effect sizes were calculated using Cohen’s d (cf. [18]). Effect sizes d = 0.20 were considered to be small, d = 0.50 medium, and d = 0.80 high [23].
Results
Dropout and missing values
A total of N = 351 patients with CLBP were approached for the study, 40 patients refused to participate and 114 patients dropped out during follow-up. To orthogonalize the distribution of sample size by gender in each experimental group, 22 male patients with no or low depressive symptoms were excluded at random. A further 22 patients were not factored into analyses due to incomplete data sets in anxiety and depressive symptoms (see Fig. 1). Thus, N = 153 patients were included in the per-protocol (PP) analyses for depressive symptoms and anxiety. For mental health, sample size was further reduced to N = 132 in the PP analyses. Additionally, intention-to-treat (ITT) analyses using the last-observation-looking-forward approach were conducted. The ITT population comprised all participants who agreed to participate in the study (N = 311). Below, only the results of the PP analyses are presented. Supplementary notes are made if the PP and the ITT analyses revealed different results.
Chi-square tests indicated that the treatment groups did not differ in drop-out rates [post-treatment: χ 2 (df = 2) = 1.18, p = ns; 6-month follow-up: χ 2 (df = 2) = 3.88, p = ns; 12-month follow-up: χ 2 (df = 2) = 1.13, p = ns; 24-month follow-up: χ 2 (df = 2) = 2.44, p = ns]. Moreover, the remaining sample of 153 participants and the patients who had dropped out only differed in age and days of sick leave; the drop-out patients were more likely to be over 50 years and to report more than 14 days of sick leave in the 3 months pre-treatment. Likewise, t tests revealed that the drop-out patients were significantly more impaired in mental health, depressive symptoms, and average pain intensity. At the same time, the drop-out patients in the IGdepr and the CGdepr did not differ pre-treatment except for depressive symptoms; patients in the CGdepr were significantly more impaired.
Rehabilitation outcome
As depicted in Table 3, repeated measures ANOVA revealed no significant two-way interactions. However, one-way interactions of treatment condition and time of assessment were obtained for depressive symptoms, anxiety, and mental health. Moreover, a significant interaction of gender and time of assessment was found for mental health.
Treatment condition by time
As presented in Tables 4 and 5, patients in the CGdepr and IGdepr showed reduced depressive symptoms with high effect sizes at post-treatment compared to pre-treatment. This favorable effect in depressive symptoms receded during follow-up in the CGdepr. In contrast, significantly reduced depressive symptoms were found in the IGdepr 6, 12, and 24 months post-treatment with medium to high effect sizes. Moreover, patients in the CGdepr showed significantly higher scores in depressive symptoms compared to patients in the IGdepr at the 6-month follow-up with a medium effect size (p = 0.038, d between = 0.46). At the same time, patients in the CG showed significantly increased depressive symptoms 6 and 24 months post-treatment with small to medium effect sizes. However, the ITT analyses revealed significantly higher scores in depressive symptoms in the CGdepr compared to the IGdepr at the 12- and 24-month follow-up with small effect sizes (t 5: p = 0.047, d between = 0.31; t 6: p = 0.018, d between = 0.37). Moreover, patients in the CG also showed increased depressive symptoms at the 12-month follow-up with a small effect size (p = 0.004, d within = −0.35).
As depicted in Tables 4 and 5, all patients showed significantly reduced anxiety immediately after rehabilitation with a medium effect size in the CG and large effect sizes in the CGdepr and the IGdepr. Patients in the CGdepr additionally showed reduced anxiety scores 12 months after rehabilitation with a small effect size. However, no significant effect was observed 6 or 24 months post-treatment in the CGdepr. In contrast, anxiety was significantly decreased at all follow-up sample points in the IGdepr with small to medium effect sizes. Furthermore, patients in the CGdepr scored significantly higher on anxiety compared to patients in the IGdepr 6 and 24 months post-treatment with medium effect sizes (t 4: p = 0.004, d between = 0.64; t 6: p = 0.033, d between = 0.47). During follow-up, no significant effects in anxiety were found in the CG. However, the ITT analyses revealed no significant between-group effect in anxiety at the 24-month follow-up.
Immediately after rehabilitation, all treatment groups benefited from the rehabilitation in mental health with medium to high effect sizes (see Tables 4, 5). However, patients in the CGdepr showed no significant change in mental health during follow-up, while patients in the IGdepr still showed significantly increased mental health scores 6 months after rehabilitation with a medium effect size. Unexpectedly, patients in the IGdepr scored significantly lower on mental health immediately after rehabilitation compared to patients in the CGdepr with a high effect size (p < 0.001, d between = 0.92). This effect receded at the 6-month follow-up. In the CG, improved mental health scores were observed at the 6-month follow-up, while no significant effects in mental health were found 12 and 24 months after rehabilitation. However, in the ITT analyses, significantly improved mental health was observed up to the 24-month follow-up in the IGdepr with small effect sizes (t 5: p = 0.019, d within = −0.33; t 6: p = 0.002, d within = −0.45), while beneficial effects in mental health receded at the 24-month follow-up in the CGdepr (t 5: p = 0.044, d within = −0.29). At the same time, the ITT analyses showed no significant between-group effect immediately after rehabilitation, but significantly improved mental health in the IGdepr compared to the CGdepr at the 6-month follow-up with a small effect size (t 4: p = 0.011, d between = −0.43). In the CG, beneficial effects in mental health receded at the 6-month follow-up in the ITT analyses.
Gender by time
Both genders showed significantly enhanced mental health scores post-treatment (see Table 6). During follow-up, no beneficial rehabilitation effects were found in men, while women showed significantly improved mental health scores up to the 12-month follow-up. Nevertheless, no significant difference in mental health was observed 24 months post-treatment in women. Furthermore, females were significantly more impaired in mental health compared to males pre-treatment with a medium effect size (p < 0.001, d between = 0.75). In contrast, no gender-related differences were shown during follow-up. However, ITT analyses revealed significantly increased mental health up to the 24-month follow-up with a small effect size in women (p = 0.005, d within = −0.34).
Discussion and conclusion
Discussion
In this study of the long-term rehabilitation effects of a supplemental cognitive-behavioral training program for the management of depressive symptoms compared with the standard rehabilitation among patients with CLBP and co-existing depressive symptoms during a period of 2 years, results showed that mid- (6-month follow-up) and long-term effects (12- and 24-month follow-up) were considerably affected by treatment condition. While no mid- or long-term effects were observed in depressive symptoms and mental health in the CGdepr, a favorable effect in anxiety 12 months post-treatment relapsed at the 24-month follow-up. Accordingly, mid-term improvements in depressive symptoms regressed at the 12-month follow-up in Pfingsten, Hildebrandt, Leibing, Franz, and Saur [24], who applied an intense cognitive-behavioral treatment. Moreover, the present results confirmed prior findings suggesting that the effects of a standard rehabilitation were not persistent in this subgroup at high-risk [7]. At the same time, results are in agreement with a recent systematic review of the Cochrane Back Group concluding that multidisciplinary rehabilitation programs integrating cognitive-behavioral modules provide no conclusive evidence for superior mid- and long-term beneficial effects on pain and depression compared to usual care [11]. Therefore, not implementing specific treatments for psychological co-morbid impairments seems to be inefficient. However, patients in the IGdepr showed persistent improvements in depressive symptoms and anxiety up to the 24-month follow-up with small to medium effect sizes and in mental health up to the 6-month follow-up with a medium effect size. Notably, the mean depressive symptoms were clinically significant prior to rehabilitation in the IGdepr (M = 24.0), while subclinical mean depressive symptoms were found at the 24-month follow-up (M = 20.7). Most important, patients in the CGdepr were more impaired in depressive symptoms and anxiety compared to patients in the IGdepr at the 6-month follow-up with small to medium effect sizes. At the 24-month follow-up, patients in the IGdepr still showed reduced anxiety compared to patients in the CGdepr with a small effect size. However, this between-group effect in anxiety at the 24-month follow-up marginally failed statistical significance in the ITT analysis. However, further superior effects in the IGdepr compared to the CGdepr were indicated by the ITT analyses in depressive symptoms (12- and 24-month follow-up) and mental health (6-month follow-up). Moreover, the ITT analysis supported persistent favorable effects on mental health up to the 24-month follow-up in the IGdepr. Taken together, the standard rehabilitation combined with the management of depressive symptoms has proved to be more effective in the long-term compared to the standard rehabilitation. It may be assumed that the newly developed cognitive-behavioral training program for the management of depressive symptoms augmented the rehabilitation success in these patients with CLBP and co-existing depressive symptoms. In a study of individualized cognitive-behavioral therapy with twenty-five 1-h sessions, Glombiewski, Hartwich-Tersek, and Rief [12] concluded that reducing pain-related depressive symptoms might be a crucial therapeutic mechanism in the cognitive-behavioral treatment of CLBP.
However, for the slight long-term regression effects in the IGdepr, after-care programs might be suggested. Considerable long-term effects have been reported in studies implementing six booster sessions (90 min/session) over a period of 1 year after rehabilitation [16]. In contrast, Mangels, Schwarz, Worringen, Holme, and Rief [25] found no benefits of seven telephone-based booster sessions (20 min/session) over a period of 1 year, but concluded that this after-care program might not have been sufficiently intense. Therefore, more research is needed to determine whether there are any beneficial effects of intense after-care programs.
The present results suggested that patients in the CG did not show mid- or long-term improvements in anxiety and mental health. Unexpectedly, patients in the CG showed no significant effect immediately after rehabilitation and significantly increased scores at the 6- and 24-month follow-up in depressive symptoms. This unfavorable finding might be associated with the common accelerated development of chronic pain. Nonetheless, it can be concluded that the standard rehabilitation did not meet the needs of this subgroup, although they only showed subclinical levels of depressive symptoms prior to rehabilitation. Sullivan, Adams, Tripp, and Stanish [5] concluded that an early detection and treatment of depressive symptoms in patients with CLBP might be indicated to prevent the transition to severe chronic pain. Hence, low-intensity modules of cognitive-behavioral management of depressive symptoms might be indicated for this subgroup to prevent the aggravation of depressive symptoms and further development of chronic pain. Linton and Nordin [26] demonstrated that a preventive cognitive-behavioral group intervention improved long-term effects in the primary care of low back pain. In the same vein, Glombiewski et al. [12] also concluded that their intense and specific cognitive-behavioral therapy could provide beneficial effects in patients with less psychological co-morbidity. However, the potential beneficial effects of a preventive training program for the management of depressive symptoms need to be investigated in future studies.
No clear evidence for gender-specific differences in treatment outcome was found in the present study, which is in line with the results found by van der Hulst et al. [6]. Women showed beneficial rehabilitation effects up to the 12-month follow-up in mental health, while men did not show significant improvement during follow-up. Nonetheless, no significant improvement in mental health could be found 24 months post-treatment in both genders. However, ITT analysis revealed significantly enhanced mental health at the 24-month follow-up in women. Nonetheless, due to significantly improved baseline mental health scores in women compared to men, no valid conclusions may be drawn based on the present findings.
Limitations
First, the current results need to be interpreted carefully due to the non-randomized procedure. Because a quasi-experimental design was applied, the effects of confounding variables could not be entirely controlled. However, no significant differences between patients in the IGdepr and patients in the CGdepr in the psychological and pain-related variables were found at the pre-assessment except for days of sick leave. Second, the patients who dropped out were significantly more impaired in several pain-related and psychological variables compared to those who were included in this study. However, the drop-out patients in the IGdepr and the CGdepr did not differ at baseline except for depressive symptoms with the drop-out patients in the CGdepr being more impaired. Thus, taking into account that the remaining patients in the CGdepr benefited immediately from the standard treatment, superior long-term effects in the IGdepr might be attributed to the supplemental training for the management of depressive symptoms. This assumption was supported by the results of the ITT analyses widely confirming the results of the PP analyses, but further pointing to more persistent beneficial effects in depressive symptoms and mental health. Nevertheless, in line with recent recommendations of the Cochrane Back Review Group [11], the cost-effectiveness of our newly developed training should be demonstrated in future studies to justify the implementation of this treatment module in multidisciplinary orthopedic inpatient rehabilitation.
Conclusion
In summary, supplemental cognitive-behavioral management of depressive symptoms enhanced long-term rehabilitation success in patients with CLBP and co-existing depressive symptoms. The new training program seemed to reduce important psychological risk factors by addressing the specific psychological needs of this subgroup that had aggravating chronic pain. Therefore, this study suggests favorable effects of psychological treatment elements specifically targeting depressive symptoms in orthopedic inpatient rehabilitation. Our approach was unique and novel, given that comparable treatment modules have not been implemented or evaluated to date in orthopedic inpatient rehabilitation of CLBP.
References
Linton SJ (2000) A review of psychological risk factors in back and neck pain. Spine 25:1148–1156
Pincus T, Burton AK, Vogel S, Field AP (2002) A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine 27:E109–E120
Bair MJ, Wu J, Damush TM, Sutherland JM, Kroenke K (2008) Association of depression and anxiety alone and in combination with chronic musculoskeletal pain in primary care patients. Psychosom Med 70:890–897
Rush AJ, Polatin P, Gatchel RJ (2000) Depression and chronic low back pain: establishing priorities in treatment. Spine 25:2566–2571
Sullivan MJL, Adams H, Tripp D, Stanish WD (2008) Stage of chronicity and treatment response in patients with musculoskeletal injuries and concurrent symptoms of depression. Pain 135:151–159
van der Hulst M, Vollenbroek-Hutten MMR, Ijzerman MJ (2005) A systematic review of sociodemographic, physical, and psychological predictors of multidisciplinary rehabilitation or, back school treatment outcome in patients with chronic low back pain. Spine 30:813–825
Mohr B, Gräf T, Forster M, Krohn-Grimberghe B, Kurzeja R, Mantel F, Thomsen M, Hampel P (2008) Der Einfluss von Depressivität und Geschlecht auf den Rehabilitationserfolg bei chronischem Rückenschmerz: eine Pilotstudie [Influence of depressive symptoms and gender in chronic low back pain rehabilitation outcome: a pilot study]. Rehabilitation 47:284–298
Guzmán J, Esmail R, Karjalainen K, Malmivaara A, Irvin E, Bombardier C (2001) Multidisciplinary rehabilitation for chronic low back pain: systematic review. BMJ 322:1511–1516
Morley S, Ecclestone C, Williams A (1999) Systematic review and meta-analysis of randomized controlled trials of cognitive behavior therapy and behavior therapy for chronic pain in adults, excluding headache. Pain 80:1–13
Scascighini L, Toma V, Dober-Spielmann S, Sprott H (2008) Multidisciplinary treatment for chronic pain: a systematic review of interventions and outcomes. Rheumatology 47:670–678
Henschke N, Ostelo RWJG, van Tulder MW, Vlaeyen JWS, Morley S, Assendelft WJJ, Main CJ (2010) Behavioral treatment for chronic low-back pain. Cochrane Database Syst Rev (7):Art. No.: CD002014. doi:10.1002/14651858.CD002014.pub3
van Middelkoop M, Rubinstein SM, Kuijpers T, Verhagen AP, Ostelo R, Koes B, van Tulder MW (2010) A systematic review on the effectiveness of physical and rehabilitation interventions for chronic non-specific low back pain. Eur Spine J 20:19–39
Bingefors K, Isacson D (2004) Epidemiology, co-morbidity, and impact on health-related quality of life of self-reported headache and musculoskeletal pain: a gender perspective. Eur J Pain 8:435–450
Rollman GB, Lautenbacher S (2001) Sex differences in musculoskeletal pain. Clin J Pain 17:20–24
Unruh AM (1996) Gender variations in clinical pain experience. Pain 65:123–167
Jensen IB, Bergström G, Ljungquist T, Bodin L (2005) A 3-year follow-up of a multidisciplinary rehabilitation program for back and neck pain. Pain 115:273–283
McGeary DD, Mayer TG, Gatchel RJ, Anagnostis C, Proctor TJ (2003) Gender-related differences in treatment outcomes for patients with musculoskeletal disorders. Spine J 3:197–203
Hampel P, Graef T, Krohn-Grimberghe B, Tlach L (2009) Effects of gender and cognitive-behavioral management of depressive symptoms on rehabilitation outcome among inpatient orthopedic patients with chronic low back pain: a 1 year longitudinal study. Eur Spine J 18:1867–1880
van Tulder MW, Koes B, Malmvaara A (2006) Outcome of non-invasive treatment modalities on back pain: an evidence-based review. Eur Spine J 15:S64–S81
Hautzinger M, Bailer M (1993) Allgemeine Depressions-Skala (ADS). Die deutsche Version des CES-D. Manual [German version of the CES-D]. Beltz, Weinheim
Herrmann-Lingen C, Buss U, Snaith RP (2005) HADS-D Hospital Anxiety and Depression Scale-Deutsche Version [HADS-D Hospital Anxiety and Depression Scale-German version], 2nd edn. Huber, Bern
Bullinger M, Kirchberger I (1998) SF-36 Fragebogen zum Gesundheitszustand. SF-12 Kurzversion des SF-36 [SF-12. German short version of the SF-36]. Hogrefe, Göttingen
Cohen J (1977) Statistical power for the behavioral sciences. Academic Press, New York
Pfingsten M, Hildebrandt J, Leibing E, Franz C, Saur P (1997) Effectiveness of a multimodal treatment program for chronic low-back pain. Pain 73:77–85
Mangels M, Schwarz S, Worringen U, Holme M, Rief W (2009) Evaluation of a behavioral-medical inpatient rehabilitation treatment including booster sessions: a randomized controlled study. Clin J Pain 25:356–364
Linton SJ, Nordin EN (2006) A 5-year follow-up evaluation of the health and economic consequences of an early cognitive behavioral intervention for back pain: a randomized, controlled trial. Spine 31:853–888
Acknowledgments
The study was sponsored by the German Pension Insurance Company, Oldenburg-Bremen.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tlach, L., Hampel, P. Long-term effects of a cognitive-behavioral training program for the management of depressive symptoms among patients in orthopedic inpatient rehabilitation of chronic low back pain: a 2-year follow-up. Eur Spine J 20, 2143–2151 (2011). https://doi.org/10.1007/s00586-011-1810-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-011-1810-x