Abstract
When the primary site is unknown in patients with spinal metastases, there can be problems in locating the site of tumor origin. Most previous reports on metastases of unknown origin have not been limited to the spine. The purpose of this study is to assess the usefulness of laboratory analysis, chest, abdominal and pelvic CT and CT-guided biopsy in patients with spinal metastases of unknown origin (SMUO). A retrospective review of the clinical histories of 27 patients with SMUO was done. A total of 43 patients with SMUO were seen at our institution between 2002 and 2007. Of the 43 patients, 27 who underwent all 3 tests (laboratory analysis including M protein and tumor markers, chest, abdominal and pelvic CT and CT-guided biopsy) were included in this study. We retrospectively assessed the diagnostic usefulness of those 3 tests in the 27 patients. In 27 patients, the final diagnosis was obtained in 26 patients. Myeloma was the most common malignancy followed by lung carcinoma. M protein was positive in all 7 patients with myeloma and negative in patients with other malignancies. The level of tumor markers was elevated in 16 of 17 patients with a solid tumor and in all 3 with lymphoma. CA15-3 was elevated in 4 of 27 patients, CA19-9 in 5 of 27 patients, CA125 in 2 of 27 patients, CEA in 6 of 27 patients, SCC in 2 of 27 patients, NSE in 7 of 27 patients, AFP in 1 of 27 patients, PIVKA-II in 1 of 27 patients, TPA in 6 of 27 patients, IAP in 3 of 12 patients, thyroglobulin in 2 of 27 patients, sIL-2R in 3 of 24 patients, and PSA in 5 of 17 male patients. Myeloma, lymphoma and prostate carcinoma had a marker with high sensitivity and specificity (M protein, sIL-2R and PSA). Eleven primary tumor sites (40.7%) were detected (6 lung, 1 prostate, 1 kidney, 1 thyroid, 1 liver, and 1 pancreas) by chest, abdominal and CT scanning. Biopsy led to determination of the final diagnosis in 12 (44.4%) of 27 patients (5 myelomas, 3 lymphomas, 2 prostate carcinomas, 1 renal-cell carcinoma, 1 thyroid carcinoma). In the remaining 15 patients, biopsy did not lead to determination of the final diagnosis, because the histological diagnosis was either an adenocarcinoma or an undifferentiated carcinoma, the tissue sample was not diagnostic. A laboratory analysis limited to specific tumor markers such as PSA and protein electrophoresis is considered to be useful in making a final diagnosis. Chest, abdominal and pelvic CT is considered to be useful for making a final diagnosis in solid tumors, but not for hematologic tumors. A CT-guided biopsy had a low determination rate in the final diagnosis in comparison to a laboratory analysis and CT scanning for solid tumors and it is not considered to be essential for the diagnosis of hematologic tumors.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The skeleton is a common metastatic site for visceral tumors. A metastatic tumor involves the spine more often than any other segment of the bony skeleton. Since most metastases occur after the detection of the primary tumor, the clinical diagnosis of a metastatic tumor of a spinal lesion can often be made from the patients’ history. When the primary site is unknown, however, there are problems in locating the site of tumor origin. Although several articles on metastases of unknown origin have been reported, most of these studies have not been limited to the spine. The purpose of the current study was to assess the diagnostic usefulness of laboratory analysis, chest, abdominal and pelvic CT and CT-guided biopsy in patients with spinal metastases of unknown origin (SMUO).
Materials and methods
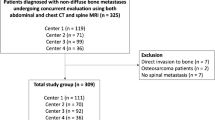
A retrospective review was carried out of 43 consecutive patients with SMUO, who had no history of malignant disease at the time of presentation, treated between 2002 and 2007. This review included patients with hematologic tumors (myeloma and lymphoma), because the therapeutic issues associated with this generally widely metastatic malignancy resemble those of other spinal metastases [13]. Of the 43 patients, 27 fulfilled the following criteria for inclusion in the study. First, a laboratory analysis of blood sample including M protein (protein electrophoresis) and all following markers was performed. The tumor markers consisted of carcinoembryonic antigen (CEA), carbohydrate antigen 15-3 (CA15-3), carbohydrate antigen 19-9 (CA19-9), cancer antigen 125 (CA125), squamous cell carcinoma related antigen (SCC), neuron-specific enolase (NSE), α-fetoprotein (AFP), protein induced by vitamin K absence antagonist-II (PIVKA-II), tissue polypeptide antigen (TPA), immunosuppressive acidic protein (IAP), thyroglobulin and sIL-2R (soluble interleukin-2 receptor). Furthermore, prostate specific antigen (PSA) was added in male patients. (the cutoff values of the markers were as follows: CEA 2.5 ng/ml; CA15-3, 25 U/ml; CA19-9, 37 U/ml; CA125, 35 U/ml; SCC, 1.5 ng/ml; NSE, 10.0 ng/ml; AFP, 10.0 ng/ml, PIVKA-II, 40 m AU/ml; TPA, 70 U/l; IAP, 604 μg/ml; thyroglobulin, 30.0 ng/ml; sIL-2R, 483 U/ml; and PSA, 4.0 ng/ml.) Second, computed tomography (CT) scanning of the chest, abdomen and pelvis was performed to search for the primary visceral tumors. Finally, a CT-guided biopsy of the spinal lesion was performed to determine the histological diagnosis.
Results
The patients’ characteristics are shown in Table 1. They included 17 men and 10 women with an average age of 62.5 years (range, 30–78 years). Among these 27 patients, the final diagnosis was finally obtained in 26 patients. Myeloma was the most common malignancy followed by lung carcinoma, prostate carcinoma and lymphoma. M protein in serum protein electrophoresis was positive in all 7 patients with myeloma and negative in patients with other malignancies. The level of tumor markers was elevated in 16 of 17 patients with a solid tumor and all 3 with lymphoma. CA15-3 was elevated in 4 of 27 patients, CA19-9 in 5 of 27 patients, CA125 in 2 of 27 patients, CEA in 6 of 27 patients, SCC in 2 of 27 patients, NSE in 7 of 27 patients, AFP in 1 of 27 patients, PIVKA-II in 1 of 27 patients, TPA in 6 of 27 patients, IAP in 3 of 27 patients, thyroglobulin in 2 of 27 patients, sIL-2R in 3 of 24 patients and PSA in 5 of 17 male patients. The sensitivities, specificities, and positive predictive values of M protein and each tumor marker for four main tumors are shown in Table 2. Of those tumors, myeloma, lymphoma and prostate carcinoma had a marker with high sensitivity and specificity (M protein, sIL-2R and PSA). However, no marker with adequate sensitivity was found in lung carcinoma.
Determination rate of final diagnosis in chest, abdominal and pelvic CT and CT-guided biopsy were shown in Table 3. CT of the chest, abdomen and pelvis demonstrated 11 primary tumor sites (40.7%): six patients had carcinoma of the lung; one, the prostate; one, the kidney; one, the thyroid; one, the liver; and one, the pancreas.
Twenty-two (81.5%) of 27 patients had a malignancy histologically confirmed by biopsy of the spinal lesion. The histological diagnoses were eight adenocarcinomas, five myelomas, two prostate carcinomas, three lymphomas, two undifferentiated carcinomas, one each of renal-cell carcinoma, well differentiated thyroid carcinoma. The biopsy findings led to a final diagnosis in 12 (44.4%) of 27 patients: one who had five myelomas, three lymphomas, two prostate carcinomas, one each of renal-cell carcinoma and thyroid carcinoma. In the remaining 15 patients, the biopsy did not lead to determination of the final diagnosis, because the histological diagnosis was either an adenocarcinoma or an undifferentiated carcinoma, or the tissue sample was not diagnostic.
Discussion
About 10% of all cancer patients develop metastases to the spine [3, 5, 6]. Among adults, 60% of spinal metastases are either from breast, lung, or prostate carcinoma. Renal and gastrointestinal malignancies each account for about 5% of spinal metastases, while thyroid carcinomas comprise a lower percentage [1, 2, 4]. In the present series, lung carcinoma was the most common solid tumor followed by prostate carcinoma and there was no case of breast carcinoma. It has been speculated that spinal metastasis is usually found after a diagnosis of breast carcinoma since it has a prolonged prognosis.
It has been reported that a spinal malignancy of unknown origin is often derived not only from solid tumors, but also from hematologic tumors [13]. In this series, myeloma was the most common etiology of SMUO and serologic evaluation for monoclonal gammopathy was very useful in all seven patients with myeloma. Therefore, serum protein electrophoresis should be performed as an initial routine study.
Increased serum levels of sIL-2R have been reported in various hematologic tumors including lymphoma [9, 10, 12]. The serum sIL-2R had high sensitivity and specificity in patients with lymphoma in this series; therefore, sIL-2R was considered useful for the diagnosis of lymphoma in patients with SMUO.
Tumor markers were abnormally elevated in all but one patient with solid tumors in the current study. Although most markers lack adequate specificity to identify the primary lesion, abnormal elevation of serum PSA, AFP and/or PIVKA-II and thyroglobulin have been reported to be considerably specific to prostate, liver and thyroid, respectively [7, 8, 14–17]. In this study, prostate carcinoma was common etiology of SMUO and PSA had high sensitivity and specificity in patients with prostate carcinoma. Furthermore, AFP/PIVKA-II and thyroglobulin were elevated in hepatocellular and thyroid carcinoma, respectively. From the results of the current study, examinations of tumor makers limited to specific tumor markers such as PSA, AFP, PIVKA-II and thyroglobulin is considered to be useful for identifying the site of primary solid tumors.
In the present series, a CT-guided biopsy led to the determination of the final diagnosis in 44.4% patients, especially, in 80.0% of patients with hematologic tumors. However, similar to the findings of previous reports [5, 11], it is not logical to start the search with a needle biopsy in patients with SMUO from the following reasons. First, a biopsy requires an invasive procedure. Second, it is not essential for making a final diagnosis in patients with hematologic tumors, although it does have a high determination rate for the final diagnosis. Third, the determination rate of the final diagnosis in solid tumors is low in comparison to a laboratory analysis and CT scanning.
In conclusion, a laboratory analysis limited to specific tumor markers such as PSA and protein electrophoresis is therefore considered to be useful in making a final diagnosis in such patients. Chest, abdominal and pelvic CT is considered to be useful for making a final diagnosis in solid tumors, but not for hematologic tumors. A CT-guided biopsy had a low determination rate in the final diagnosis in comparison to a laboratory analysis and CT scanning for solid tumors and it is therefore not considered to be essential for the diagnosis of hematologic tumors because a laboratory analysis was found to be an alternative.
References
Aebi M (2003) Spinal metastasis in the elderly. Eur Spine J 12(Suppl. 2):S202–S213. doi:10.1007/s00586-003-0609-9
Bartanusz V, Porchet F (2003) Current strategies in the management of spinal metastatic disease. Swiss Surg 9:55–62. doi:10.1024/1023-9332.9.2.55
Greenlee RT, Murray T, Bolden S, Wingo PA (2000) Cancer statistics, 2000. CA Cancer J Clin 50:7–33. doi:10.3322/canjclin.50.1.7
Groot MT et al (2003) Costs of prostate cancer metastasis to the bone in The Netherlands. Eur Urol 43:226–232. doi:10.1016/S0302-2838(03)00007-1
Katagiri H, Takahashi M, Inagaki J (1999) Determining the primary cancer in patients with skeletal metastasis of unknown origin. Cancer 86:533–537. doi:10.1002/(SICI)1097-0142(19990801)86:3<533::AID-CNCR24>3.0.CO;2-1
Landis SH et al (1999) Global cancer statistics. CA Cancer J Clin 49:33–64. doi:10.3322/canjclin.49.1.8
Motoo Y, Watanabe H, Sawabu N (1996) Sensitivity and specificity of tumor markers in cancer diagnosis. Nippon Rinsho 54(6):1587–1591
Oesterling JE, Fuks Z, Lee CT, Scher HI (1997) Cancer of the genitourinary system. In: Devita VT, Hellman S, Rosenberg SA (eds) Cancer principles and practice of oncology, 5th edn. Lippincott-Raven, Philadelphia, pp 1336–1338
Pizzolo G, Chilosi M, Semenzato G (1987) The soluble interleukin-2 receptor in haematological disorders. Br J Haematol 67:377–380. doi:10.1111/j.1365-2141.1987.tb06156.x
Pui CH (1989) Serum interleukin-2 receptor: clinical and biological implications. Leukemia 3:323–327
Rougraff BT, Kneisl JS, Simon MA (1993) Skeletal metastases of unknown origin. A prospective study of a diagnostic strategy. J Bone Jt Surg Am 75:1276–1281
Rubin LA, Nelson DL (1990) The soluble interleukin-2 receptor: biology, function, and clinical application. Ann Intern Med 113:619–627
Schiff D, O’Neill BP, Suman VJ (1997) Spinal epidural metastasis as the initial manifestation of malignancy. Clinical features and diagnostic approach. Neurology 49:452–456
Spencer CA, Wang CC (1995) Thyroglobulin measurement: techniques, clinical benefits and pitfalls. Endocrinol Metab Clin North Am 24:841–863
Van Herle AJ, Uller RP (1975) Elevated serum thyroglobulin: a marker of metastases in differentiated thyroid carcinomas. J Clin Invest 56:272–277. doi:10.1172/JCI108090
Whitley RJ, Ain KB (2004) Thyroglobulin: a specific serum marker for the management of thyroid carcinoma. Clin Lab Med 24(1):29–47
Yuen MF, Lai CL (2005) Serological markers of liver cancer. Best Pract Res Clin Gastroenterol 19:91–99. doi:10.1016/j.bpg.2004.10.003
Acknowledgments
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Iizuka, Y., Iizuka, H., Tsutsumi, S. et al. Diagnosis of a previously unidentified primary site in patients with spinal metastasis: diagnostic usefulness of laboratory analysis, CT scanning and CT-guided biopsy. Eur Spine J 18, 1431–1435 (2009). https://doi.org/10.1007/s00586-009-1061-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-009-1061-2